Abstract
Aims/hypothesis
The aim of this study was to estimate the long-term health and economic consequences of improved risk factor control in German adults with type 2 diabetes.
Methods
We used the UK Prospective Diabetes Study Outcomes Model 2 to project the patient-level health outcomes and healthcare costs of people with type 2 diabetes in Germany over 5, 10 and 30 years. We parameterised the model using the best available data on population characteristics, healthcare costs and health-related quality of life from German studies. The modelled scenarios were: (1) a permanent reduction of HbA1c by 5.5 mmol/mol (0.5%), of systolic BP (SBP) by 10 mmHg, or of LDL-cholesterol by 0.26 mmol/l in all patients, and (2) achievement of guideline care recommendations for HbA1c (≤53 mmol/mol [7%]), SBP (≤140 mmHg) or LDL-cholesterol (≤2.6 mmol/l) in patients who do not meet the recommendations. We calculated nationwide estimates using age- and sex-specific quality-adjusted life year (QALY) and cost estimates, type 2 diabetes prevalence and population size.
Results
Over 10 years, a permanent reduction of HbA1c by 5.5 mmol/mol (0.5%), SBP by 10 mmHg or LDL-cholesterol by 0.26 mmol/l led to per-person savings in healthcare expenditures of €121, €238 and €34, and 0.01, 0.02 and 0.015 QALYs gained, respectively. Achieving guideline care recommendations for HbA1c, SBP or LDL-cholesterol could reduce healthcare expenditure by €451, €507 and €327 and gained 0.03, 0.05 and 0.06 additional QALYs in individuals who did not meet the recommendations. Nationally, achieving guideline care recommendations for HbA1c, SBP and LDL-cholesterol could reduce healthcare costs by over €1.9 billion.
Conclusions/interpretation
Sustained improvements in HbA1c, SBP and LDL-cholesterol control among diabetes patients in Germany can lead to substantial health benefits and reduce healthcare expenditures.
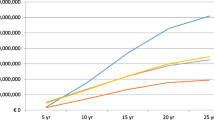
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.

Introduction
As of 2010, over 7% of the German adult population had a type 2 diabetes diagnosis [1], and its prevalence is expected to increase substantially over the next two decades [2]. The costs for routine diabetes management, care for diabetes complications, the time required for self-management and diabetes-associated productivity losses place a substantial economic and health burden on patients, healthcare systems and societies [3,4,5,6]. Previous studies have shown that lifestyle and pharmaceutical interventions aiming at better risk factor control are effective in delaying and preventing subsequent complications and death [7,8,9]. Despite this robust evidence, achievement of guideline-recommended risk factor levels remains sub-optimal globally [10]. In Germany, national surveys have suggested that approximately one-third of patients with type 2 diabetes failed to achieve the guideline-recommended targets for HbA1c and BP, and over 70% did not achieve the guideline care recommendation for LDL-cholesterol [11, 12].
Quantifying the net health and economic burden of poor risk factor control is challenging. Due to the slow progression of type 2 diabetes, the benefits of improved risk factor control accumulate over years or even decades [7, 13, 14], while implementation of interventions to improve risk factor control usually requires considerable up-front investment. Evaluating the long-term value of improved risk factor control is therefore crucial for decision-making given scarce resources in healthcare systems. Computer simulation models that predict long-term health outcomes of people with type 2 diabetes depending on their risk profiles have been established as useful tools that can help to fill this knowledge gap [15]. Previous studies from the US and UK that employed a modelling approach indicated that better risk factor control can lead to substantial reductions in healthcare costs and prolongation of quality-adjusted life expectancy among patients with type 2 diabetes [16,17,18]. However, as the underlying characteristics of patients and healthcare systems differ between countries, the results of these studies are highly context-specific, and the health and economic implications of improved risk factor control in Germany are unknown.
The objective of this study was to estimate the long-term per-person and nationwide health benefits and cost savings that could be achieved through improved control of HbA1c, systolic Blood pressure and LDL-Cholesterol (ABC control) in German adults with type 2 diabetes using a simulation modelling approach.
Methods
Overall study design
For the simulations, we used the UK Prospective Diabetes Study Outcome Model 2 (UKPDS-OM2), which can predict the development of diabetes-related complications, and estimates long-term patient-level health and economic outcomes [19]. We parameterised the model using patient characteristics from a large population-based German cohort study and utility decrements and healthcare expenditures associated with diabetes complications estimated from German survey and claims data [3, 4]. We simulated the mean per-person long-term health and economic consequences of two hypothetical improvement scenarios in ABC control for people with type 2 diabetes in Germany over 5, 10 and 30 years from a healthcare system perspective for the reference year 2022. To obtain estimates at the population level for Germany, we calculated person-level results stratified by age and sex, and combined them with the estimated number of adults with type 2 diabetes by age and sex in Germany.
Intervention scenarios of improved ABC control
In the first scenario, we shifted the entire population distribution of ABC levels to the left (i.e. risk reduction). In the second scenario, we only shifted ABC levels of individuals whose levels would otherwise exceed the thresholds of guideline care recommendations. For each scenario, we estimated the health and economic effects of improved control in HbA1c, systolic blood pressure (SBP) or LDL-cholesterol separately. In addition, we simulated a ‘combined’ intervention for each scenario, in which all three risk factors were targeted simultaneuosly.
The improvements of ABC control in all the scenarios were assumed to be permanent over the respective simulation time horizon.
Population-level shift of ABC
We simulated the effects of a population-wide shift of the HbA1c distribution by 5.5 mmol/mol (0.5%) [20], of the SBP distribution by 10 mmHg [21], and of the LDL-cholesterol distribution by 0.26 mmol/l [22]. This change in risk factor levels was irrespective of whether the original level was below or above the guideline-recommended threshold. The chosen effect size for the change in risk factors corresponds to around 20–50% of the standard deviations for the risk factors. These simulated intervention effects are higher than the effects resulting from lifestyle interventions [23], but lower than the effects resulting from intense pharmaceutical treatment [24,25,26], and therefore represent realistic changes of what could be achieved across the treatment cascade.
ABC guideline care recommendations
In this scenario, we only targeted individuals with ABC levels above the recommended thresholds mentioned in German or international guidelines. Acknowledging that the thresholds differ between countries and change over time and due to personalisation will not be applicable for each patient, we programmatically set them in this study to HbA1c ≤53 mmol/mol (7%) for glycaemic control, SBP ≤140 mmHg for blood pressure management and LDL-cholesterol ≤2.6 mmol/l for lipid management. Individuals with risk factors above the threshold were set to the threshold level. For example, if the HbA1c level of a person was 65 mmol/mol (8.1%) (above the guideline threshold), it was set to 53 mmol/mol (7%), whereas a person with an HbA1c of 49.7 mmol/mol (6.7%) (below the guideline threshold) was assumed to be unaffected by the intervention.
Cost associated with changes in risk factor control
There are multiple ways of improving ABC control. These include intensified medication, better self-management, lifestyle changes or population-level intervention. All of these interventions come at a certain cost [27]. However, this study only aims to quantify the hypothetical population impact of improved ABC control independently of the measure used to achieve this improvement. Therefore, we disregarded the potential costs that any intervention would entail. Thus, the results of this study must always be considered in the context of the one-off or continuous cost of the intervention needed to improve ABC control.
Simulation model
General information on the UKPDS-OM2
The UKPDS-OM2 is a patient-level microsimulation tool for modelling the progression of type 2 diabetes and estimating lifetime health outcomes of people with type 2 diabetes [19]. It was developed based on 89,760 patient-years of data from the UK Prospective Diabetes Study, a randomised controlled trial evaluating treatment regimens with different intensities of blood glucose and BP control, performed among newly diagnosed type 2 diabetes patients between 1977 and 1991 in the UK, and a 10-year post-trial monitoring observational study. Details on the development and validation of the model have been described in detail elsewhere [19, 28] and are briefly summarised here.
Risk equations in the UKPDS-OM2 were developed via proportional hazards survival models for first occurrence of eight diabetes complications (myocardial infarction, ischaemic heart disease, stroke, congestive heart failure, amputation, renal failure, blindness and foot ulcer), three additional second events (myocardial infarction, stroke, amputation) and mortality [19]. The probability of death and experiencing one or more complications is calculated for each patient at an annual cycle. As the model is parameterised with the respective utility decrements and healthcare expenditures associated with each complication, it predicts total accumulated healthcare costs and (quality-adjusted) life expectancy [28].
In a previous study, we tested the performance of the epidemiological risk equations in the UKPDS-OM2 by predicting mortality and cardiovascular events in a population-based German sample of people with type 2 diabetes. The results suggested that the risk equations overestimate mortality but predict cardiovascular events well over a 10-year time horizon, and that, despite some limitations, the model may be suitable for applications in German populations [29].
Model parameterisation with type 2 diabetes patient characteristics
To parameterise the model with patient characteristics that represent the mean German population with type 2 diabetes, we used data from participants with known type 2 diabetes (n=146) from the KORA-S4 study, a population-based cross-sectional survey and examination study of 4261 participants that was performed between 1999 and 2001 in the city of Augsburg and two surrounding counties in southern Germany. The study collected demographic and behavioural characteristics (age, sex, duration of diabetes, weight, height, smoking), biological risk factors (HDL-cholesterol, LDL-cholesterol, HbA1c, SBP, heart rate, white blood cell count, haemoglobin level and eGFR), and the occurrence of diabetes-related pre-existing events (ischaemic heart disease, heart failure, myocardial infarction, stroke, amputation, blindness, renal failure, ulcer) and the time that had passed since their occurrence, and some additional conditions (peripheral vascular disease, atrial fibrillation, albuminuria). We assumed that all patients were white and of European descent. We further adjusted the mean HbA1c, SBP and LDL-cholesterol levels in this sample for observed improvements that occurred between the years 2000 and 2014 [11]. To avoid instability in our simulations, we generated a synthetic population of 1000 patients based on the KORA-S4 sample using the R package ‘Synthpop’ that draws on the underlying empirical risk factor distributions (see electronic supplementary material [ESM] Appendix A for further details). This synthetic population was used to populate the model.
Model parameterisation with healthcare expenditures estimates
We used published estimates of total healthcare expenditures (including inpatient and outpatient care, pharmaceuticals, rehabilitation, and non-medical aids and remedies) associated with incident complications in patients with type 2 diabetes [3]. The study reported age- and sex-specific estimates of annual healthcare expenditures from the perspective of the German statutory health insurance system for the year of the event and in subsequent years in people with type 2 diabetes for all eight complications simulated in the UKPDS-OM2 (for further details, see ESM Appendix B and ESM Table 1). Costs are expressed in 2022 euros using official inflation data from the Statistisches Bundesamt (Federal Statistical Office) [30].
Model parameterisation with utility decrement estimates
Estimates on health utility decrements associated with type 2 diabetes and diabetes-related complications in Germany were taken from the KORA Health Questionnaire 2016, in which health utility was assessed using the EuroQol five-dimension questionnaire (EQ-5D-5L) in a sample of 8951 participants [4]. Since the utility decrements for ‘amputation’ and ‘renal failure’ were not estimated in this study, values for these two variables were taken from international studies [31, 32] (see ESM Appendix C and ESM Tables 2 and 3 for details).
Model details
Simulations were run over 5, 10 and 30 years; 30 years is assumed to approximate a population lifetime horizon. Healthcare expenditures and quality-adjusted life years (QALYs) were discounted by 3.5% per year. The number of internal loops (Monte-Carlo trials, related to first-order uncertainty; a sufficient number of loops can reduce the random variation of predicted outcomes in each internal loop) was set to 10,000, and the number of bootstrap samples was set to 100 (related to second order uncertainty; each bootstrap run will use a different set of model equation parameters from the 5000 sets of model equation parameters in OM2) to generate sufficiently precise confidence intervals around predicted outcomes.
Outcomes
Costs and quality-adjusted life years
The cumulative healthcare costs and cumulative QALYs over simulation years were estimated.
Individual-level perspective
In the analysis of scenario with a population-level shift of the ABC distribution, we estimated mean per-person health and cost outcomes. In the analysis of the ABC guideline care recommendation scenario, we estimated mean per-person health and cost outcomes only for those above the recommended guideline threshold. We also generated mean per-person estimates representative for the German population by adjusting for the age and sex distribution of type 2 diabetes patients in Germany.
National healthcare system perspective
We extrapolated the modelled per-person effects to the whole German population with type 2 diabetes. Given that the patient characteristics from the KORA-S4 sample may not be fully representative of people with type 2 diabetes in the overall German population with type 2 diabetes, and that health outcomes are largely determined by age and sex, we multiplied the age- and sex-specific per-person effects (presented in ESM Appendix D) by the age- and sex-specific numbers of people with type 2 diabetes in Germany [1, 33]. Methodological details are given in ESM Appendix E.
For the guideline care scenario, we multiplied the age- and sex-specific per-person effects for those above the guideline care recommendation thresholds (presented in ESM Appendix D) by the age- and sex-specific numbers of people with type 2 diabetes in Germany and the age- and sex-specific proportions of people with type 2 diabetes whose ABC levels exceed recommended thresholds (age- and sex-specific prevalence is presented in ESM Table 9). We took these proportion data from our KORA-S4 sample, as the proportions of people with type 2 diabetes whose ABC levels exceed recommended thresholds in KORA lie in the middle of the reported proportions for other studies [10,11,12].
Maximum intervention costs at a given willingness-to-pay threshold
Based on the individual-level results for QALY gains and cost savings, we calculated the maximum costs for an intervention achieving the modelled risk factor improvements under which this intervention would be cost-effective over a lifetime, given a willingness-to-pay threshold of €50,000/QALY gained. We divided this number by the mean simulated life expectancy to annualise the maximum per-person expenditures.
Sensitivity analyses
Several sensitivity analyses were performed to determine the relative importance of model parameters. We varied discount rates (0%, 5%), the number of internal loops (5000, 20,000), cost estimates and utility decrements (half of the original values, twice the original values).
Results
Sample characteristics
The baseline characteristics of participants with type 2 diabetes in the original KORA-S4 sample and the derived synthetic population are presented in Table 1. The mean age in the sample population was 62 years, the mean duration of diabetes was 9 years, the mean HbA1c levels was 50.8 mmol/mol (6.8%), the mean SBP was 126 mmHg and the mean LDL-cholesterol was 2.93 mmol/l. The derived synthetic population had very similar characteristics.
Per-person cost savings and QALY gains
Differences in total healthcare costs and QALYs between the intervention scenarios and the control scenario without any risk factor improvements are driven by reduced event rates of complications in the group with improved ABC control. For example, a reduction of systolic BP of 10 mmHg over a time horizon of 10 years reduced the cumulative incidence of stroke from 5% to 4.4%. The differences in cumulative event rates of the eight modelled complications between reference and treatment groups over the various simulation time horizons are reported in ESM Appendix F. Improved HbA1c control mainly had an impact on microvascular outcomes (foot ulcer, blindness or amputation), whereas the effect of improvements in LDL-cholesterol was mostly limited to cardiovascular events (stroke, myocardial infarction and ischaemic heart disease).
Table 2 shows the per-person total healthcare expenditure, QALYs and remaining life years for the reference group, and the incremental healthcare expenditures (cost savings; negative cost savings represent an increase in healthcare expenditures), QALYs and life expectancies between the reference group and each intervention group. The simulated mean per-person estimates are based on the characteristics of type 2 diabetes patients in the KORA-S4 sample.
Sustained population-wide decreases of HbA1c by 5.5 mmol/mol (0.5%) (mean 50.8 mmol/mol [6.8%] vs 45.3 mmol/mol [6.3%]), of SBP by 10 mmHg (mean SBP of 126 mmHg vs 116 mmHg) and of LDL-cholesterol by 0.26 mmol/l (mean 2.96 mmol/l vs 2.70 mmol/l) over 10 years led to gains in QALYs of 0.01 (95% CI 0.007, 0.013), 0.02 (0.014, 0.023) and 0.015 (0.011, 0.018), respectively, and healthcare cost savings of €121 (€83, €182), €238 (€154, €307) and €34 (€29, €115) per person, respectively. Achieving guideline care recommendations for HbA1c, SBP and LDL-cholesterol over 10 years resulted in QALYs gained of 0.03 (0.02, 0.04), 0.05 (0.03, 0.06) and 0.06 (0.05, 0.08), respectively, and decreased healthcare costs by €451 (€344, €676), €507 (€349, €922) and €327 (€230, €515), respectively, per person with ABC levels above the recommended threshold. Generally, QALY gains and healthcare savings were substantially smaller for the 5-year time horizon and substantially larger for the 30-year time horizon, with the exception that healthcare cost savings were smaller and negative for LDL-cholesterol control over the 30-year time horizon, i.e. the costs increased.
Simultaneously decreasing HbA1c by 5.5 mmol/mol (0.5%), SBP by 10 mmHg and LDL-cholesterol level by 0.26 mmol/l (‘Combined population-wide reduction’ in Table 2) led to a per-person QALY gain of 0.012 (0.010, 0.014) over 5 years, of 0.04 (0.04, 0.05) over 10 years and of 0.15 (0.14, 0.17) over 30 years (lifetime), and reduced per-person healthcare costs by €254 (€202, €294), €422 (€339, €514) and €438 (€190, €589), respectively. Achieving guideline care recommendations for HbA1c, SBP and LDL-cholesterol resulted in QALY gains of 0.02 (0.018, 0.024), 0.07 (0.06, 0.08) and 0.25 (0.22, 0.29) over 5, 10 and 30 years, respectively, and healthcare cost savings of €400 (€316, €477), €581 (€462, €776) and €451 (€170, €695) per person for people with at least one value above the ABC thresholds.
ESM Table 10 shows the per-person estimates after adjusting for the age and sex distribution of patients with type 2 diabetes in Germany. The per-person QALY and life years gained for the German population are very similar to those in Table 2; per-person cost savings are slightly higher than the estimates from the KORA-S4 sample over the 5-year time horizon, and slightly lower compared with those from the KORA-S4 sample over the 30-year time horizon.
Cost savings and QALY gains from a national healthcare system perspective
The nationwide cost savings and QALY gains resulting from improved ABC control from a national healthcare system perspective are shown in Table 3. Over a 10-year period, sustaining a population-wide reduction of HbA1c by 5.5 mmol/mol (0.5%), of SBP by 10 mmHg and of LDL-cholesterol by 0.26 mmol/l would result in 54,381, 98,753 and 78,535 QALYs gained, respectively, and €543 million, €1047 million and €60 million cost savings, respectively, for people with type 2 diabetes in Germany; achieving recommended levels of HbA1c, SBP and LDL-cholesterol for every patient with type 2 diabetes in Germany would lead to 43,358, 45,418 and 185,381 QALYs gained, respectively, and reduce healthcare expenditures by €681 million, €457 million and €921 million, respectively.
Shifting the ABC risk factor distribution simultaneously for all type 2 diabetes patients in Germany would gain 210,333 QALYs and reduce healthcare costs by over €1.8 billion within the national healthcare system over 10 years. Achieving recommended levels of ABC control for everyone with levels above the threshold would lead to a decrease of over €1.9 billion in healthcare expenditure, and an increase of 268,783 QALYs.
Maximum per-person annual intervention costs at a willingness-to-pay threshold of €50,000 per QALY
To be cost-effective at a willingness-to-pay threshold of €50,000 per QALY gained over a lifetime perspective, we found that the annual cost for a hypothetical intervention to achieve guideline care recommendations for HbA1c, SBP or LDL-cholesterol should not exceed €549, €760 or €958, respectively (Table 4).
Sensitivity analyses
The Tornado plots in ESM Appendix G show the results of a one-way sensitivity analysis of simulated outcomes. Assumptions regarding the costs associated with complications, utility decrements for complications and the chosen discount rates had a bigger impact on the outcomes than the chosen number of loops.
Discussion
Summary of results
To the best of our knowledge, this is the first study to use an established, validated simulation model to predict long-term health and economic consequences of improved ABC control in German adults with type 2 diabetes. Our study showed that simultaneously achieving the recommended levels for HbA1c, SBP or LDL-cholesterol control for all people with type 2 diabetes in Germany would gain approximately 270,000 QALYs and save over €1.9 billion in healthcare costs over the next 10 years. The expected health benefits would be substantially greater over longer time horizons.
The two modelled scenarios – population-level shift of ABC and achievement of ABC guideline care recommendations – may be achieved by various evidence-based intervention strategies. A population-level shift of the risk factor distribution to the left may most likely be reached through a ‘population-level’ approach. An example for this is a national salt reduction intervention that would reduce salt intake in the entire population [34, 35] or the use of drugs for primary prevention [36]. In contrast, a scenario that only targets individuals who do not achieve guideline-recommended risk factor levels may be reached through a ‘high-risk screen and treat’ approach that involves pharmaceutical treatment, for example [34, 37, 38].
The magnitude of the healthcare cost savings and QALY gains at the national level are often greater for the scenarios in which the ABC distribution was shifted, even though individual-level effects were larger for the achievement of guideline care recommendations. This is because the achievement of guideline care recommendation scenarios only affected a proportion of patients—those with risk factor levels above the thresholds. For example, over 10 years, the healthcare cost savings per person were €238 for a 10 mmHg shift in the SBP distribution and €507 per person who achieved guideline-recommended levels for those whose SBP levels were above the threshold of 140 mmHg at baseline. As only 20% of the population had SBP levels above 140 mmHg, the national-level cost savings for the distribution shift were much larger (€1047 million) than those for achieving recommended levels of SBP (€457 million). This highlights the importance of complementing clinical disease management with population-based intervention strategies [34].
Achieving recommended levels for ABC control would reduce the healthcare expenditures of adults with diabetes by around €289 million annually (€1443 million saved over 5 years). In relative terms, this would reduce annual healthcare expenditures for patients with diabetes in Germany by approximately 1% [39].
Results in light of the existing literature
Using the original model parameters from the UKPDS-OM2, Hayes et al reported that a decrease of 1.5% (16.4 mmol/mol) in HbA1c led to an increase of 0.35 life years over lifetime [19]. This effect is larger compared with that observed in our study (0.04 life years with a 0.5% [5.5 mmol/mol] reduction in HbA1c), even after taking into account the intervention intensity. However, in their analysis, the study population had a worse baseline mean HbA1c level of 8.2% (66.1 mmol/mol), compared with our 6.8% (50.8 mmol/mol), and the mean age of their study sample at baseline was 53 years (62 years in our study), which resulted in an expected life expectancy of 19.5 years in their study, almost twice as high as that in ours (11 years [Table 2]) [40].
The effects of improved ABC control on QALYs were also estimated using observed trial data. In the original UKPDS trial, a mean decrease in HbA1c of 0.9% (9.8 mmol/mol) (from 7.9% [62.8 mmol/mol] to 7% [53.0 mmol/mol]) resulted in 0.08 QALYs gained over a time horizon of 10 years, and a mean decrease in SBP of 10 mmHg resulted in 0.1 QALYs gained [21, 41]. In comparison, in our study, 11 mmol/mol (1.0%) decrease in HbA1c sustained over 10 years resulted in 0.02 QALYs gained, and a sustained decrease of SBP by 10 mmHg (from 154 to 144 mmHg) resulted in 0.02 QALYs gained (Table 2 and ESM Table 14). Therefore, our modelled QALYs gained were smaller compared with the UKPDS trial and predicted model scenarios in other populations.
Other previous modelling studies also reported higher QALY gains and cost savings from treatment scenarios that improve ABC control than those found in our study. A study by Palmer et al using the CORE Diabetes Model suggested that a decrease in HbA1c of 0.9% (9.8 mmol/mol) would lead to gains of 0.81 QALYs and healthcare expenditure savings of US$10,800 per person over their lifetime from a US private payer perspective [16]. These differences may partially be explained by differences in the characteristics of the baseline population, the costs associated with treatment of diabetes and its complications, and the risk equations used to describe the epidemiological relationship between risk factor control and complications. In this context, it should be highlighted that, in contrast to this study [16] and other previous modelling studies, the performance of the risk equations used in our model was tested previously in the population of interest, showing that the calibration for cardiovascular morbidity and mortality is moderate to good [29]. In addition, the parameters for the costs associated with incident diabetes complications were estimated from claims of the largest German statutory health insurance company using panel regression methods that are less likely to yield biased estimates than models based on cross-sectional data [31].
Results in the context of diabetes care in Germany
As the aim of the analyses was to highlight the long-term health benefits and cost saving potential of improved risk factor control, we did not consider any resources and costs needed to achieve these improvements. However, all real-world risk factor improvement strategies of course come with costs to achieve these improvements. We show that the maximum per-person annual costs for interventions that improve HbA1c control be cost-effective at a willingness-to-pay threshold of €50,000 per QALY gained over a 30-year time horizon range between €190 and €549. In context, the per-person annual costs for metformin, sulfonylurea, sodium–glucose cotransporter 2 (SGLT-2) inhibitors, dipeptidyl peptidase 4 (DPP-4) inhibitors and glucagon-like peptide-1 (GLP-1) antagonists in Germany are approximately €33–99, €31–131, €377–884, €350–511 and €861–1463, respectively [42]. It is important to mention that German guidelines for Health Technology Assessment (HTA) do not endorse the use of cost-effectiveness analyses for reimbursement decisions, and no formal willingness-to-pay threshold for a QALY gained is defined for Germany [43].
Strengths of this study
We used one of the most established type 2 diabetes simulation models [29]. We parameterised the model using the characteristics of a concurrent population-based diabetes cohort and healthcare expenditures and quality of life variables from large real-world and population-based studies from Germany. We further analysed several ABC distribution shift and guideline-based control scenarios, and provide sensitivity analyses to show the robustness of our results.
Limitations of this study
First, the results of this modelling study are potentially limited by the underlying model assumptions. We demonstrated in a previous study that the risk equations used in the UKPDS-OM2 predict cardiovascular events well but over-estimate mortality. However, the performance of the model for the prediction of other outcomes remains unknown [29]. Second, we assumed and simulated sustained risk factor improvements over the lifetime of simulated individuals. This may represent an over-simplification as such sustained improvements may be unrealistic for some individuals in the population due to their specific genetic risk profiles and during critical life stages, e.g. menopausal transition, which is associated with higher LDL-cholesterol [44]. Third, the utility decrements used were taken from a large German cross-sectional study. It has been shown that estimates from cross-sectional studies tend to overestimate true causal effects [31]. Fourth, the characteristics of our population-based diabetes sample from a regional cohort study in southern Germany may not be entirely representative for all patients with type 2 diabetes in Germany. As previous studies indicated that control of diabetes risk factors in patients in southern Germany is better than in the rest of Germany [45], the results may underestimate the true health and economic benefits. In addition, this sample only included 146 patients with type 2 diabetes. Fifth, the mean population levels of HbA1c, SBP and LDL-cholesterol may have further decreased since 2014. If this is the case, we may have slightly overestimated the health benefits, as the given changes in risk factors in people with lower baseline disease risk would mostly translate into lower absolute health benefits. Sixth, a population-wide shift in HbA1c, SBP or LDL-cholesterol may lead to adverse complications such as hypoglycaemia for individuals at the lower end of the HbA1c distribution, but we did not model these potential adverse outcomes. Due to the low proportion of people in these very low ranges, we assume that this would affect our results only marginally. Finally, cost estimates for complications of diabetes and estimates on diabetes prevalence were taken from samples of Germans insured in the statutory health insurance scheme in which approximately 89% of Germans are included. Compared with the statutory health insurance scheme, the per-person cost estimates for treating complications are likely to be higher and the prevalence of type 2 diabetes is likely to be lower in individuals with private health insurance, and thus the estimates for the national healthcare system perspective may be biased in either direction. We again assume that that this would affect our results only marginally.
Conclusion
Both population-level shifts in risk factor distribution and the achievement of guideline care recommendations for patients exceeding recommended risk factor levels can result in substantial health benefits and cost savings. The expected long-term health and economic benefits described in this study may help German decision makers to assess the clinical effects of interventions and their costs from an efficiency perspective. Using an internationally accepted willingness-to-pay threshold, treatment aiming for better adherence to the guideline-recommended HbA1c level, SBP level and LDL-cholesterol level should not cost more than €549, €760 and €958 a year, respectively.
Abbreviations
- ABC:
-
HbA1c, systolic Blood pressure and LDL-Cholesterol
- KORA:
-
Kooperative Gesundheitsforschung in der Region Augsburg/Cooperative Health Research in the Region of Augsburg
- QALY:
-
Quality-adjusted life year
- SBP:
-
Systolic blood pressure
- UKPDS-OM2:
-
UK Prospective Diabetes Study Outcomes Model 2
References
Tamayo T, Brinks R, Hoyer A, Kuss OS, Rathmann W (2016) The prevalence and incidence of diabetes in Germany. Dtsch Arztebl Int 113(11):177–82. https://doi.org/10.3238/arztebl.2016.0177
Tonnies T, Rockl S, Hoyer A et al (2019) Projected number of people with diagnosed type 2 diabetes in Germany in 2040. Diabet Med 36(10):1217–25. https://doi.org/10.1111/dme.13902
Kähm K, Laxy M, Schneider U, Rogowski WH, Lhachimi SK, Holle R (2018) Health care costs associated with incident complications in patients with type 2 diabetes in Germany. Diabetes Care 41(5):971–8. https://doi.org/10.2337/dc17-1763
Laxy M, Becker J, Kähm K et al (2021) Utility decrements associated with diabetes and related complications: estimates from a population-based study in Germany. Value Health 24(2):274–280. https://doi.org/10.1016/j.jval.2020.09.017
Bommer C, Sagalova V, Heesemann E et al (2018) Global economic burden of diabetes in adults: projections from 2015 to 2030. Diabetes Care 41(5):963–70. https://doi.org/10.2337/dc17-1962
Icks A, Haastert B, Arend W et al (2020) Patient time costs due to self-management in diabetes may be as high as direct medical costs: results from the population-based KORA survey FF4 in Germany. Diabetic Med 37(5):895–7. https://doi.org/10.1111/dme.14210
Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA (2008) 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med 359(15):1577–89. https://doi.org/10.1056/NEJMoa0806470
Vijan S, Hayward RA (2003) Treatment of hypertension in type 2 diabetes mellitus: blood pressure goals, choice of agents, and setting priorities in diabetes care. Ann Intern Med 138(7):593–602. https://doi.org/10.7326/0003-4819-138-7-200304010-00018
Nichols GA, Joshua-Gotlib S, Parasuraman S (2013) Independent contribution of A1C, systolic blood pressure, and LDL cholesterol control to risk of cardiovascular disease hospitalizations in type 2 diabetes: an observational cohort study. J Gen Intern Med 28(5):691–7. https://doi.org/10.1007/s11606-012-2320-1
Stone MA, Charpentier G, Doggen K et al (2013) Quality of care of people with type 2 diabetes in eight European countries: findings from the Guideline Adherence to Enhance Care (GUIDANCE) study. Diabetes Care 36(9):2628–38. https://doi.org/10.2337/dc12-1759
Laxy M, Knoll G, Schunk M, Meisinger C, Huth C, Holle R (2016) Quality of diabetes care in Germany improved from 2000 to 2007 to 2014, but improvements diminished since 2007 evidence from the population-based KORA studies. Plos One 11(10):e0164704. https://doi.org/10.1371/journal.pone.0164704
Du Y, Heidemann C, Rosario AS et al (2015) Changes in diabetes care indicators: findings from German National Health Interview and Examination Surveys 1997–1999 and 2008–2011. BMJ Open Diabetes Research and Care 3(1):e000135. https://doi.org/10.1136/bmjdrc-2015-000135
Gong Q, Zhang P, Wang J et al (2019) Morbidity and mortality after lifestyle intervention for people with impaired glucose tolerance: 30-year results of the Da Qing Diabetes Prevention Outcome Study. Lancet Diabetes Endocrinol 7(6):452–61. https://doi.org/10.1016/S2213-8587(19)30093-2
Diabetes Prevention Program Research Group (2015) Long-term effects of lifestyle intervention or metformin on diabetes development and microvascular complications over 15-year follow-up: the Diabetes Prevention Program Outcomes Study. Lancet Diabetes Endocrinol 3(11):866–75. https://doi.org/10.1016/S2213-8587(15)00291-0
Dadwani RS, Laiteerapong N (2020) Economic simulation modeling in type 2 diabetes. Curr Diabetes Rep 20(7):24. https://doi.org/10.1007/s11892-020-01306-y
Palmer AJ, Roze S, Valentine WJ et al (2004) Impact of changes in HbA1c, lipids and blood pressure on long-term outcomes in type 2 diabetes patients: an analysis using the CORE Diabetes Model. Curr Med Res Opinion 20(sup1):S53–S58. https://doi.org/10.1185/030079903125002611
Keng MJ, Tsiachristas A, Leal J, Gray A, Mihaylova B (2019) Impact of achieving primary care targets in type 2 diabetes on health outcomes and healthcare costs. Diabetes Obes Metab 21(11):2405–12. https://doi.org/10.1111/dom.13821
Valentine W, Palmer A, Nicklasson L, Cobden D, Roze S (2006) Improving life expectancy and decreasing the incidence of complications associated with type 2 diabetes: a modelling study of HbA1c targets. Int J Clin Pract 60(9):1138–45. https://doi.org/10.1111/j.1742-1241.2006.01102.x
Hayes AJ, Leal J, Gray AM, Holman RR, Clarke PM (2013) UKPDS outcomes model 2: a new version of a model to simulate lifetime health outcomes of patients with type 2 diabetes mellitus using data from the 30 year United Kingdom Prospective Diabetes Study: UKPDS 82. Diabetologia 56(9):1925–33. https://doi.org/10.1007/s00125-013-2940-y
Knight K, Badamgarav E, Henning JM et al (2005) A systematic review of diabetes disease management programs. Am J Manag Care 11(4):242–50
UK Prospective Diabetes Study Group (1998) Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ 317(7160):703–13. https://doi.org/10.1136/bmj.317.7160.703
Heart Protection Study Collaborative Group HPSC (2003) MRC/BHF Heart Protection Study of cholesterol-lowering with simvastatin in 5963 people with diabetes: a randomised placebo-controlled trial. Lancet 361(9374):2005–16. https://doi.org/10.1016/S0140-6736(03)13636-7
Chen L, Pei J-H, Kuang J et al (2015) Effect of lifestyle intervention in patients with type 2 diabetes: a meta-analysis. Metabolism 64(2):338–47. https://doi.org/10.1016/j.metabol.2014.10.018
Sherifali D, Nerenberg K, Pullenayegum E, Cheng JE, Gerstein HC (2010) The effect of oral antidiabetic agents on A1C levels: a systematic review and meta-analysis. Diabetes Care 33(8):1859–64. https://doi.org/10.2337/dc09-1727
Hodkinson A, Tsimpida D, Kontopantelis E, Rutter MK, Mamas MA, Panagioti M (2022) Comparative effectiveness of statins on non-high density lipoprotein cholesterol in people with diabetes and at risk of cardiovascular disease: systematic review and network meta-analysis. BMJ 376:e067731. https://doi.org/10.1136/bmj-2021-067731
Canoy D, Copland E, Nazarzadeh M et al (2022) Antihypertensive drug effects on long-term blood pressure: an individual-level data meta-analysis of randomised clinical trials. Heart 108(16):1281–9. https://doi.org/10.1136/heartjnl-2021-320171
Siegel KR, Ali MK, Zhou X et al (2020) Cost-effectiveness of interventions to manage diabetes: has the evidence changed since 2008? Diabetes Care 43(7):1557–92. https://doi.org/10.2337/dci20-0017
Clarke PM, Gray AM, Briggs A et al (2004) A model to estimate the lifetime health outcomes of patients with type 2 diabetes: the United Kingdom Prospective Diabetes Study (UKPDS) Outcomes Model (UKPDS no. 68). Diabetologia 47(10):1747–59. https://doi.org/10.1007/s00125-004-1527-z
Laxy M, Schoning VM, Kurz C et al (2019) Performance of the UKPDS Outcomes Model 2 for predicting death and cardiovascular events in patients with type 2 diabetes mellitus from a German population-based cohort. Pharmacoeconomics 37(12):1485–94. https://doi.org/10.1007/s40273-019-00822-4
Statistisches Bundesamt Office. Consumer price indices for Germany, Annual Report 2022. Available from: https://www.destatis.de/DE/Themen/Wirtschaft/Preise/Verbraucherpreisindex/Publikationen/Downloads-Verbraucherpreise/verbraucherpreisindex-jahresbericht-pdf-5611104.pdf?__blob=publicationFile. Accessed 17 Jan 2023 [article in German]
Alva M, Gray A, Mihaylova B, Clarke P (2014) The effect of diabetes complications on health-related quality of life: the importance of longitudinal data to address patient heterogeneity. Health Econ 23(4):487–500. https://doi.org/10.1002/hec.2930
Lung TW, Hayes AJ, Hayen A, Farmer A, Clarke PM (2011) A meta-analysis of health state valuations for people with diabetes: explaining the variation across methods and implications for economic evaluation. Qual Life Res 20(10):1669–78. https://doi.org/10.1007/s11136-011-9902-y
Klüsener S, Grigoriev P, Scholz RD, Jdanov DA (2018) Adjusting inter-censal population estimates for Germany 1987–2011: approaches and impact on demographic indicators. Comp Popul Stud 43:31–64. https://doi.org/10.12765/CPoS-2018-05en
Rose G (1981) Strategy of prevention: lessons from cardiovascular disease. Br Med J (Clin Res ed) 282(6279):1847. https://doi.org/10.1136/bmj.282.6279.1847
Hyseni L, Elliot-Green A, Lloyd-Williams F et al (2017) Systematic review of dietary salt reduction policies: evidence for an effectiveness hierarchy? PloS one 12(5):e0177535. https://doi.org/10.1371/journal.pone.0177535
Bibbins-Domingo K, Grossman DC, Curry SJ et al (2016) Statin use for the primary prevention of cardiovascular disease in adults: US Preventive Services Task Force recommendation statement. Jama 316(19):1997–2007. https://doi.org/10.1001/jama.2016.15450
American Diabetes Association AD (2021) 9. Pharmacologic approaches to glycemic treatment: standards of medical care in diabetes-2021. Diabetes care 44(Suppl 1):S111–S124. https://doi.org/10.2337/dc21-S009
American Diabetes Association (2019) 10. Cardiovascular disease and risk management: standards of medical care in diabetes-2019. Diabetes care 42(Suppl 1):S103–S123. https://doi.org/10.2337/dc19-S010
Müller N, Heller T, Freitag MH et al (2015) Healthcare utilization of people with type 2 diabetes in Germany: an analysis based on health insurance data. Diabet Med 32(7):951–7. https://doi.org/10.1111/dme.12747
Clarke P, Gray A, Holman R (2002) Estimating utility values for health states of type 2 diabetic patients using the EQ-5D (UKPDS 62). Med Decis Making 22(4):340–9. https://doi.org/10.1177/027298902400448902
Clarke PM, Gray AM, Briggs A et al (2005) Cost-utility analyses of intensive blood glucose and tight blood pressure control in type 2 diabetes (UKPDS 72). Diabetologia 48(5):868–77. https://doi.org/10.1007/s00125-005-1717-3
Niedersachsen A. Arzneimittelinformationen & Beratungsangebot der AOK Niedersachsen. Antidiabetika [Internet]. 2023 02. Available from: https://www.aok.de/gp/wirtschaftliche-verordnung/aktuelle-arzneimittelinformationen-der-aok-niedersachsen/orale-antidiabetika. Accessed 1 Feb 2023 [article in German]
Gerber-Grote A, Sandmann FG, Zhou M et al (2014) Decision making in Germany: is health economic evaluation as a supporting tool a sleeping beauty? Zeitschrift Für Evidenz, Fortbildung Und Qualität Im Gesundheitswesen 108(7):390–6. https://doi.org/10.1016/j.zefq.2014.06.018
Carr MC, Kim KH, Zambon A et al (2000) Changes in LDL density across the menopausal transition. J Investig Med Off Publ Am Fed Clin Res 48(4):245–50
Tamayo T, Claessen H, Ruckert IM et al (2014) Treatment pattern of type 2 diabetes differs in two German regions and with patients’ socioeconomic position. PLoS One 9(6):e99773. https://doi.org/10.1371/journal.pone.0099773
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Acknowledgements
Data collection in the KORA study was performed in cooperation with the University Hospital of Augsburg. An abstract of this paper was submitted to the EUHEA (European Health Economics Association) Conference 2022 ‘Health Economics for Sustainable Welfare Systems’ (Oslo, Norway), and was presented orally by Min Fan.
Data availability
The data are subject to national data protection laws, and restrictions were imposed by the Ethics Committee of the Bavarian Medical Association to ensure data privacy of the study participants; therefore, data cannot be made freely available in a public repository. Data are third-party and belong to the KORA research platform, but may be accessed for specific research projects through individual project agreements. Interested researchers can request data from KORA via the online tool (https://www.helmholtz-munich.de/en/epi/cohort/kora). Interested researchers, who agree to the general terms and conditions of the KORA data user agreement, can therefore access the data of KORA in the same way that we did.
Funding
Parts of this work were funded by iPDM-GO (Integrated Personalised Diabetes Management), for which we received funding from the European Institute for Innovation and Technology (EIT) through its Knowledge and Innovation Community EIT Health. The EIT is a body of the European Union that receives support from the European Union’s Horizon 2020 research and innovation programme. The KORA study was initiated and financed by the Helmholtz Zentrum München/German Research Center for Environmental Health, which is funded by the German Bundesministerium für Bildung und Forschung and the State of Bavaria. Open Access funding enabled and organised by Projekt DEAL.
Authors’ relationships and activities
The authors declare that there are no relationships or activities that might bias, or be perceived to bias, their work.
Contribution statement
MF analysed and interpreted the data and drafted the manuscript. ML conceptualised and designed the study, interpreted the data, and contributed to acquisition of the data and drafting the article. A-JS and KE-F contributed to the drafting of the article and revised it critically for important intellectual content. AP made contributions to the acquisition of the data, and critically reviewed the manuscript. All authors gave final approval of the version to be published. MF and ML are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of this data analysis.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Fan, M., Stephan, AJ., Emmert-Fees, K. et al. Health and economic impact of improved glucose, blood pressure and lipid control among German adults with type 2 diabetes: a modelling study. Diabetologia 66, 1693–1704 (2023). https://doi.org/10.1007/s00125-023-05950-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-023-05950-3