Abstract
Aims/hypothesis
People with type 2 diabetes are at increased risk of developing obstructive sleep apnoea. However, it is not known whether people with type 1 diabetes are also at an increased risk of obstructive sleep apnoea. This study aimed to examine whether people with type 1 diabetes are at increased risk of incident obstructive sleep apnoea compared with a matched cohort without type 1 diabetes.
Methods
We used a UK primary care database, The Health Improvement Network (THIN), to perform a retrospective cohort study between January 1995 and January 2018 comparing sleep apnoea incidence between patients with type 1 diabetes (exposed) and without type 1 diabetes (unexposed) (matched for age, sex, BMI and general practice). The outcome was incidence of obstructive sleep apnoea. Baseline covariates and characteristics were assessed at the start of the study based on the most recent value recorded prior to the index date. The Cox proportional hazards regression model was used to estimate unadjusted and adjusted hazard ratios, based on a complete-case analysis.
Results
In total, 34,147 exposed and 129,500 matched unexposed patients were included. The median follow-up time was 5.43 years ((IQR 2.19–10.11), and the mean BMI was 25.82 kg/m2 (SD 4.33). The adjusted HR for incident obstructive sleep apnoea in patients with type 1 diabetes vs those without type 1 diabetes was 1.53 (95% CI 1.25, 1.86; p<0.001). Predictors of incident obstructive sleep apnoea in patients with type 1 diabetes were older age, male sex, obesity, being prescribed antihypertensive or lipid-lowering drugs, atrial fibrillation and depression.
Conclusions/interpretation
Individuals with type 1 diabetes are at increased risk of obstructive sleep apnoea compared with people without diabetes. Clinicians should suspect obstructive sleep apnoea in patients with type 1 diabetes if they are old, have obesity, are male, have atrial fibrillation or depression, or if they are taking lipid-lowering or antihypertensive drugs.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.

Introduction
Obstructive sleep apnoea is common, affecting 10% of women and 20% of men in high-income countries [1]. Obstructive sleep apnoea is characterised by repeated complete upper airway obstruction (apnoea) or partial upper airway obstruction (hypopnoea), leading to recurrent episodes of oxygen desaturation and resaturation, as well as cyclical changes in heart rate, blood pressure and sympathetic activity, and disruption of sleep architecture [2, 3]. Obstructive sleep apnoea has been found to be associated with an increased risk of road traffic accidents, reduced workplace productivity, type 2 diabetes, insulin resistance, hypertension, CVD, reduced quality of life, and increased mortality risk [4,5,6,7,8,9,10,11].
Obstructive sleep apnoea is a well-established risk factor for the development of type 2 diabetes [12]. More recently, our group has shown that patients with type 2 diabetes are also at increased risk of developing obstructive sleep apnoea, suggesting that the relationship between obstructive sleep apnoea and type 2 diabetes is bi-directional [13]. We have also demonstrated previously that obstructive sleep apnoea in people with type 2 diabetes is associated with increased oxidative stress, nitrosative stress, poly-ADP ribose polymerase activation and endothelial dysfunction in cross-sectional studies [14, 15], and is associated with diabetes-related micro- and macrovascular complications in cohort studies [16,17,18]. However, little is known about obstructive sleep apnoea in patients with type 1 diabetes. It is important to ascertain whether people with type 1 diabetes are at increased risk of obstructive sleep apnoea given the significant above-mentioned comorbidities associated with obstructive sleep apnoea [15,16,17, 19, 20].
It is plausible that patients with type 1 diabetes may be at increased risk of obstructive sleep apnoea due to the increasing prevalence of obesity and insulin resistance in patients with type 1 diabetes and the high prevalence of autonomic neuropathy, which may contribute to obstructive sleep apnoea pathogenesis by affecting upper airways control [21,22,23,24]. Several small cross-sectional studies reported a high prevalence of obstructive sleep apnoea in patients with type 1 diabetes (10–46%) [25,26,27,28]. Other studies have shown a higher prevalence of sleep disruption and obstructive sleep apnoea in paediatric patients with type 1 diabetes compared with controls, that experimental sleep restriction reduced insulin sensitivity in type 1 diabetes, and that sleep apnoea and sleep disruption were associated with worse glycaemic control [29,30,31,32,33]. However, the direction of these associations is not clear, and hence longitudinal studies are needed.
Therefore, we performed a cohort study with the primary aim of assessing whether patients with type 1 diabetes are at increased risk of developing incident obstructive sleep apnoea compared with matched controls without diabetes. A secondary aim was to identify predictors of incident obstructive sleep apnoea in the patients with type 1 diabetes.
Methods
Study design
We used a UK primary care database, The Health Improvement Network (THIN), to perform a retrospective cohort study between January 1995 and January 2018 comparing sleep apnoea incidence between patients with type 1 diabetes (exposed) and without type 1 diabetes (unexposed) (matched for age, sex, BMI and general practice).
Data source
The datasets for this study were extracted from The Health Improvement Network (THIN) database, which is a nationally representative electronic primary care database of more than 15 million patients from 787 practices in the UK [18]. This database contains anonymised medical records and is generalisable to the UK population. The data include coded demographic details, symptoms and diagnoses, all prescribed drugs, and the results of diagnostic tests [34, 35]. The database has previously been used in multiple studies of type 1 diabetes or sleep apnoea [13, 36].
Study population
To ensure that the data extracted were of good quality, we included patients from practices after at least one year of acceptable mortality reporting. Acceptable mortality reporting is important for epidemiological studies as under-reporting may result in attempted follow-up of participants who are actually dead. In contrast, over-reporting of mortality may result in reporting deaths in a specific period for people who actually died before the reporting dates [37]. Patients were only included from these practices if they have been registered with that practice for at least 1 year, to ensure completeness of the data.
In this study, we compared the HR of incident obstructive sleep apnoea in all age groups in patients with type 1 diabetes (exposed) vs matched patients without a diagnosis of type 1 diabetes (controls/unexposed).
Type 1 diabetes diagnosis was ascertained by the presence of any clinical (Read) code consistent with type 1 diabetes (https://digital.nhs.uk/article/1104/Read-Codes) in the absence of any record of type 2 diabetes or type 2 diabetes medications (except metformin) throughout the study period. The control (unexposed) cohort had no codes relating to any type of diabetes throughout the study period. Each exposed patient was matched to a maximum of four controls by age ± 3 years, sex, BMI ± 3 kg/m2 and general practitioner. Exposed and control patients were eligible for inclusion in the study if they had no diagnosis of obstructive sleep apnoea at or prior to the index date.
The index date for the exposed group was the later of the type 1 diabetes diagnosis date or 12 months after joining the general practitioner. The controls were assigned the same index date that was given to their corresponding exposed patient with type 1 diabetes.
The outcome measure (obstructive sleep apnoea) was also defined based on clinical (Read) codes (see electronic supplementary material [ESM] Table 1; https://digital.nhs.uk/article/1104/Read-Codes). The cohort was followed-up until the earliest of the following: developing obstructive sleep apnoea, death, leaving the practice, the practice ceasing to contribute to this primary care database, or the study end date.
Ethics
Data were obtained from IQVIA Medical Research Data UK, incorporating data from The Health Improvement Network, which is a registered trademark of Cegedim in the UK and other countries. Reference made to The Health Improvement Network database is intended to be descriptive of the data asset licensed by IQVIA. This work uses de-identified data provided by patients as a part of their routine primary care. This study was approved by the Scientific Review Committee (SRC) on 3rd December 2019 (SRC reference number 19THIN085).
Statistical analysis
The baseline characteristics were summarised for those exposed and unexposed using appropriate descriptive statistics. Baseline covariates and characteristics were assessed at the start of the study. Baseline measures were the most recent value recorded prior to the index date. Continuous variables were reported as means (SD), and categorical variables were reported as the number of individuals (percentage). Crude HR and adjusted HR and their corresponding 95% CIs for incident obstructive sleep apnoea in the exposed vs unexposed groups were calculated using Cox proportional hazards regression. The Cox regression model was adjusted for several covariates including age, sex, BMI category, Townsend deprivation quintile, smoking status, drinking status, CVD, hypertension and atrial fibrillation. Bioplausibility and previous literature were used to identify covariates that were included in the multivariable model [13]. We performed a post hoc Cox regression analysis by including variables from the type 1 diabetes predictor analysis (adding atrial fibrillation, antihypertensive and lipid-lowering drugs to the Cox model). The proportional hazards assumption was tested using a log−log plot and Schoenfeld residuals test. Due to the presence of missing data for key covariates (BMI categories, Townsend deprivation quintile, smoking status, drinking status), we performed the analysis using complete-case analysis. We also performed a sensitivity analysis using multiple imputation analysis to adjust for the bias of missing data, and the results of the imputed analysis are presented in ESM Table 2.
Several sensitivity analyses were performed by limiting the analysis to patients younger than 60 years old; those younger than 60 years old and diagnosed with diabetes before the age of 40 years; and patients less than 40 years old. In addition, a secondary analysis limited to adult patients (age ≥ 18 years old) was performed. Additional subgroup analysis compared the incidence of obstructive sleep apnoea among patients with or without type 1 diabetes stratified by age, sex, BMI, Townsend deprivation quintile and comorbid conditions (CVD, hypertension, atrial fibrillation, anxiety and depression). All analyses included the exposed cohort with their corresponding controls.
Further analysis (using multiple imputation) limited to exposed participants with type 1 diabetes was performed to identify obstructive sleep apnoea risk factors (predictors) in patients with type 1 diabetes. The predictors were based on baseline variables.
All analyses were performed in Stata IC version 15 (StataCorp, USA). Two-sided p values were obtained, and p value <0.05 was considered statistically significant.
Results
Baseline characteristics
We identified 34,147 patients with type 1 diabetes without a diagnosis of obstructive sleep apnoea who were eligible for inclusion in the study. These were matched to 129,500 patients without diabetes or obstructive sleep apnoea. The baseline characteristics are summarised in Table 1. The study population was young, with slightly more men than women, and a low prevalence of obesity. The study population were mostly white people of European extraction, with poor glycaemic control and a relatively low number with prescriptions of CVD medications. All these features are consistent with what is expected in a type 1 diabetes population.
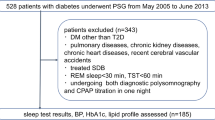
Type 1 diabetes and incident obstructive sleep apnoea
By the end of the study, obstructive sleep apnoea had been diagnosed in 219 (0.64%) of the patients with type 1 diabetes, and 531 (0.41%) of the controls, over a median follow-up duration of 5.43 years (IQR 2.19–10.11). The median diabetes duration in patients with type 1 diabetes who were diagnosed with obstructive sleep apnoea was 19.36 years (IQR 7.42–28.11), which was approximately double the duration for patients with type 1 diabetes without obstructive sleep apnoea (median 10.47, IQR 2.56–21.17).
A total of 19,689 patients with type 1 diabetes without a diagnosis of obstructive sleep apnoea and 77,604 patients without diabetes or obstructive sleep apnoea were included in the complete-case analysis. The incidence rates were 11.62 and 7.46 per 10,000 person-years for the exposed participants and controls, respectively. Evaluation of the incidence rate for obstructive sleep apnoea over time showed a consistent higher annual rate in patients with type 1 diabetes since 2002 (ESM Fig. 1). After adjusting for baseline age, sex, BMI category, Townsend quintile, smoking status and drinking status, the adjusted HR for obstructive sleep apnoea in the exposed vs control group was 1.51 (95% CI 1.24, 1.83; p< 0.001) (Table 2). Further adjustments for CVD, hypertension and atrial fibrillation at baseline did not change the findings (adjusted HR 1.53; 95% CI 1.25, 1.86; p<0.001) (Table 2). This association remained significant after multiple imputation of missing data (HR 1.68; 95% CI 1.43, 1.97; p< 0.001) (ESM Table 2). The adjusted HR decreased to 1.24 (95% CI 1.00, 1.54; p=0.05) after performing a post hoc analysis by adding baseline depression and use of lipid-lowering and antihypertensive drugs to the above-mentioned baseline covariates in the complete-case analysis model. The Cox proportional hazards assumption was examined using a log–log plot and Schoenfeld residuals test, and there were no violations.
Sensitivity analysis
Limiting the analysis to people younger than 60 years old or patients younger than 60 years old who were diagnosed with type 1 diabetes before the age of 40 years, along with their respective controls, did not change the results of the main analysis (Table 2). Limiting the analysis to patients younger than 40 years of age attenuated the association between type 1 diabetes and obstructive sleep apnoea (Table 2). This attenuation is not surprising given that older age is a risk factor for obstructive sleep apnoea.
We performed an additional complete-case analysis limited to adult people (age ≥ 18 years old) with type 1 diabetes (n= 19,493) and their matched controls (n=77,018). The results for the association between type 1 diabetes and obstructive sleep apnoea for the adults were similar to the results for the whole population (ESM Table 3).
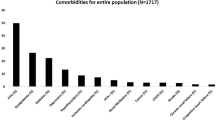
The stratified analysis (Fig. 1) found that patients with type 1 diabetes were more likely to develop obstructive sleep apnoea compared with people without diabetes across age categories, in men and women, in people with normal weight, overweight or obesity, across social deprivation quantiles, and in the presence or absence of comorbidities.
Forest plot showing adjusted HR for obstructive sleep apnoea in patients with type 1 diabetes compared with patients without diabetes in subgroups stratified by age, sex, BMI, Townsend score and comorbidity. The HR was adjusted for age, sex, BMI categories, Townsend quintiles, smoking status and alcohol intake
Predictors of incident obstructive sleep apnoea in patients with type 1 diabetes
Male sex, age, being overweight or obese, use of lipid-lowering medication, use of antihypertensive medication, and a history of atrial fibrillation and depression were associated with increased HR of incident obstructive sleep apnoea (Table 3).
Discussion
We found that patients with type 1 diabetes are at increased risk of obstructive sleep apnoea compared with patients without diabetes. The study also identified a number of predictors of incident obstructive sleep apnoea in patients with type 1 diabetes. As far as we are aware, this is the first study to examine the relationship between obstructive sleep apnoea and type 1 diabetes longitudinally.
The adjusted HRs for incident obstructive sleep apnoea in people with vs without type 1 diabetes reported in this study are similar to those reported in patients with type 2 diabetes in another study by our team that used the current database [13]. This may be surprising considering the lower prevalence of obesity and younger age of patients with type 1 vs type 2 diabetes. This finding suggests that another mechanism may play a role in the development of obstructive sleep apnoea in people with type 1 diabetes. One potential mechanism, which was not directly measured in this study, is the presence of diabetic autonomic neuropathy; this mechanism is indirectly supported in this data by the longer duration of diabetes in patients with obstructive sleep apnoea vs no obstructive sleep apnoea, and the finding that atrial fibrillation was a predictor of incident obstructive sleep apnoea, as diabetic autonomic neuropathy is also associated with longer diabetes duration, atrial fibrillation and CVD [24].
Several previous cross-sectional studies observed that obstructive sleep apnoea is common in patients with type 1 diabetes [25,26,27,28], but the direction of this relationship was not clear. In this study, we found that patients with type 1 diabetes are at increased risk of obstructive sleep apnoea. In addition, cross-sectional studies found that obstructive sleep apnoea in type 1 diabetes was associated with diabetes-related peripheral and autonomic neuropathy, chronic kidney disease and retinopathy [26, 28]. Our group has also reported previously that, in patients with type 2 diabetes, having obstructive sleep apnoea was associated with an increased incidence of micro- and macrovascular complications [18]. In addition, patients with type 1 diabetes are at increased risk of hypoglycaemia, which is important in the context of driving as obstructive sleep apnoea is also associated with an increased risk of road traffic accidents [38]. Hence, clinicians and healthcare professionals caring for patients with type 1 diabetes should be vigilant in terms of suspecting obstructive sleep apnoea in these patients despite the low prevalence of obesity and younger age, particularly patients with factors identified in our analysis as predictive of incident obstructive sleep apnoea. Future work should examine whether patients with type 1 diabetes and obstructive sleep apnoea are at increased risk of vascular complications compared with those with type 1 diabetes only.
We found that depression was an independent predictor for obstructive sleep apnoea in patients with type 1 diabetes. This is consistent with findings from non-diabetes studies. The relationship between obstructive sleep apnoea and mental health disease was examined in a large US retrospective study including over 4 million records (not specifically with diabetes), and found that depression was common in people with obstructive sleep apnoea (22%) [39]. Systematic reviews have also established the relationship between obstructive sleep apnoea and depression [40], and found that obstructive sleep apnoea treatment using continuous positive airway pressure improved depression symptoms [41].
In patients with type 1 diabetes, we also found that baseline atrial fibrillation was a strong obstructive sleep apnoea predictor. People with type 1 diabetes had an increased risk of atrial fibrillation compared with the general population in a Swedish population-based analysis [42]. Sleep disturbance has been linked to atrial fibrillation [43], and up to 85% of people with atrial fibrillation had obstructive sleep apnoea [44,45,46,47].
The study has limitations. Although the current database includes comprehensive and reliable data, the accuracy of the study depends on the quality of the data recorded by the general practitioners in the primary care clinics. Also, the severity of obstructive sleep apnoea and use of continuous positive airway pressure were not recorded in the current database. It is plausible that clinicians are more likely to look for obstructive sleep apnoea in the exposed vs unexposed cohort due to the presence of type 1 diabetes, and this may result in detection bias. Although we used certain criteria to select type 1 diabetes patients and exclude type 2 diabetes, the criteria do not eliminate the risk of misclassification. However, the study findings were robust despite matching for key variables, and in multiple sensitivity and subgroup analyses including multiple age groups and comorbidities. In this study, we used baseline characteristics to identify obstructive sleep apnoea predictors, and therefore another potential limitation is not accounting for time-varying covariates in the analysis. A further limitation of the analysis is that ethnicity was not included, due to the large proportion of patients for whom ethnicity data was missing. Previous studies also showed similar large missingness for ethnicity data [13, 18, 48].
This study is the first longitudinal study to examine the associations between type 1 diabetes, incident sleep apnoea and sleep apnoea predictors. We used a validated well-established primary care database from the UK. The breadth of the data available allowed us to adjust for a large number of variables and perform sensitivity and subgroup analyses.
In conclusion, compared with people without diabetes, patients with type 1 diabetes are at increased risk of obstructive sleep apnoea. Obesity, male sex, age, depression, atrial fibrillation, and use of lipid-lowering and antihypertensive drugs at baseline were predictors for incident obstructive sleep apnoea in type 1 diabetes. Therefore, clinicians should suspect obstructive sleep apnoea in patients with type 1 diabetes who have the above-mentioned predictors even though people with type 1 diabetes usually have less obesity than type 2 diabetes.
Data availability
THIN data governance does not allow us to share individual patient data. Researchers may apply for individual patient data access at https://www.iqvia.com/contact.
Abbreviations
- THIN:
-
The Health Improvement Network
References
Jordan AS, McSharry DG, Malhotra A (2014) Adult obstructive sleep apnoea. Lancet 383(9918):736–747. https://doi.org/10.1016/S0140-6736(13)60734-5
Altaf QA, Barnett AH, Tahrani AA (2015) Novel therapeutics for type 2 diabetes: insulin resistance. Diabetes Obes Metab 17(4):319–334. https://doi.org/10.1111/dom.12400
Shaw JE, Punjabi NM, Wilding JP, Alberti KGMM, Zimmet PZ (2008) Sleep-disordered breathing and type 2 diabetes: a report from the international diabetes federation taskforce on epidemiology and prevention. Diabetes Res Clin Pract 81(1):2–12. https://doi.org/10.1016/j.diabres.2008.04.025
Tregear S, Reston J, Schoelles K, Phillips B (2009) Obstructive sleep apnea and risk of motor vehicle crash: systematic review and meta-analysis. J Clinical Sleep Med 5(6):573–581
Tesler Waldman L, Parthasarathy S, Villa KF et al (2019) Impact of excessive sleepiness associated with obstructive sleep apnea on work productivity in the United States. Eur Resp J 54(Suppl 63):PA902. https://doi.org/10.1183/13993003.congress-2019.PA902
Punjabi NM, Caffo BS, Goodwin JL et al (2009) Sleep-disordered breathing and mortality: a prospective cohort study. PLoS Med 6(8):e1000132. https://doi.org/10.1371/journal.pmed.1000132
Lindberg E, Theorell-Haglöw J, Svensson M, Gislason T, Berne C, Janson C (2012) Sleep apnea and glucose metabolism: a long-term follow-up in a community-based sample. Chest 142(4):935–942. https://doi.org/10.1378/chest.11-1844
Wang X, Bi Y, Zhang Q, Pan F (2013) Obstructive sleep apnoea and the risk of type 2 diabetes: a meta-analysis of prospective cohort studies. Respirology 18(1):140–146. https://doi.org/10.1111/j.1440-1843.2012.02267.x
Wang X, Ouyang Y, Wang Z, Zhao G, Liu L, Bi Y (2013) Obstructive sleep apnea and risk of cardiovascular disease and all-cause mortality: a meta-analysis of prospective cohort studies. Int J Cardiol 169(3):207–214. https://doi.org/10.1016/j.ijcard.2013.08.088
D'Ambrosio C, Bowman T, Mohsenin V (1999) Quality of life in patients with obstructive sleep apnea: effect of nasal continuous positive airway pressure – a prospective study. Chest 115(1):123–129
Peppard PE, Young T, Palta M, Skatrud J (2000) Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med 342(19):1378–1384. https://doi.org/10.1056/NEJM200005113421901
Tahrani AA (2017) Obstructive sleep apnoea in diabetes: does it matter? Diab Vasc Dis Res 14(5):454–462. https://doi.org/10.1177/1479164117714397
Subramanian A, Adderley NJ, Tracy A et al (2019) Risk of incident obstructive sleep apnea among patients with type 2 diabetes. Diabetes Care 42(5):954–963. https://doi.org/10.2337/dc18-2004
Altaf QA, Ali A, Piya MK, Raymond NT, Tahrani AA (2016) The relationship between obstructive sleep apnea and intra-epidermal nerve fiber density, PARP activation and foot ulceration in patients with type 2 diabetes. J Diabetes Complicat 30(7):1315–1320. https://doi.org/10.1016/j.jdiacomp.2016.05.025
Tahrani AA, Ali A, Raymond NT et al (2012) Obstructive sleep apnea and diabetic neuropathy: a novel association in patients with type 2 diabetes. Am J Respir Crit Care Med 186(5):434–441. https://doi.org/10.1164/rccm.201112-2135OC
Tahrani AA, Ali A, Raymond NT et al (2013) Obstructive sleep apnea and diabetic nephropathy: a cohort study. Diabetes Care 36(11):3718–3725. https://doi.org/10.2337/dc13-0450
Altaf QA, Dodson P, Ali A et al (2017) Obstructive sleep apnea and retinopathy in patients with type 2 diabetes. A longitudinal study. Am J Respir Crit Care Med 196(7):892–900. https://doi.org/10.1164/rccm.201701-0175OC
Adderley NJ, Subramanian A, Toulis K et al (2020) Obstructive sleep apnea, a risk factor for cardiovascular and microvascular disease in patients with type 2 diabetes: findings from a population-based cohort study. Diabetes Care 43(8):1868–1877. https://doi.org/10.2337/dc19-2116
Foster GD, Sanders MH, Millman R et al (2009) Obstructive sleep apnea among obese patients with type 2 diabetes. Diabetes Care 32(6):1017–1022. https://doi.org/10.2337/dc08-1776
Tahrani A, Dodson P, Ali A et al (2013) Obstructive sleep apnoea is associated with sight threatening retinopathy and predicts the development of preproliferative and proliferative retinopathy in patients with type 2 diabetes: a longitudinal analysis. Eur J Ophthalmol 23(3):449–449
Corbin KD, Driscoll KA, Pratley RE et al (2018) Obesity in type 1 diabetes: pathophysiology, clinical impact, and mechanisms. Endocr Rev 39(5):629–663. https://doi.org/10.1210/er.2017-00191
Dempsey JA, Veasey SC, Morgan BJ, O'Donnell CP (2010) Pathophysiology of sleep apnea. Physiol Rev 90(1):47–112. https://doi.org/10.1152/physrev.00043.2008
Rees PJ, Prior JG, Cochrane GM, Clark TJ (1981) Sleep apnoea in diabetic patients with autonomic neuropathy. J R Soc Med 74(3):192–195
Fisher VL, Tahrani AA (2017) Cardiac autonomic neuropathy in patients with diabetes mellitus: current perspectives. Diabetes Metab Syndr Obes 10:419–434. https://doi.org/10.2147/dmso.S129797
Schober AK, Neurath MF, Harsch IA (2011) Prevalence of sleep apnoea in diabetic patients. Clin Respir J 5(3):165–172. https://doi.org/10.1111/j.1752-699X.2010.00216.x
Banghoej AM, Nerild HH, Kristensen PL et al (2017) Obstructive sleep apnoea is frequent in patients with type 1 diabetes. J Diabetes Complicat 31(1):156–161. https://doi.org/10.1016/j.jdiacomp.2016.10.006
Meyer L, Massuyeau M, Canel C et al (2017) Association of sleep apnoea syndrome and autonomic neuropathy in type 1 diabetes. Diabetes Metab 45(2):206–209. https://doi.org/10.1016/j.diabet.2017.10.011
Manin G, Pons A, Baltzinger P et al (2015) Obstructive sleep apnoea in people with type 1 diabetes: prevalence and association with micro- and macrovascular complications. Diabet Med 32:90–96. https://doi.org/10.1111/dme.12582
Matyka KA, Crawford C, Wiggs L, Dunger DB, Stores G (2000) Alterations in sleep physiology in young children with insulin-dependent diabetes mellitus: relationship to nocturnal hypoglycemia. J Pediatr 137(2):233–238. https://doi.org/10.1067/mpd.2000.107186
Denic-Roberts H, Costacou T, Orchard TJ (2016) Subjective sleep disturbances and glycemic control in adults with long-standing type 1 diabetes: the Pittsburgh’s epidemiology of diabetes complications study. Diabetes Res Clin Pract 119:1–12. https://doi.org/10.1016/j.diabres.2016.06.013
Villa MP, Multari G, Montesano M et al (2000) Sleep apnoea in children with diabetes mellitus: effect of glycaemic control. Diabetologia 43(6):696–702. https://doi.org/10.1007/s001250051365
Perfect MM, Beebe D, Levine-Donnerstein D, Frye SS, Bluez GP, Quan SF (2016) The development of a clinically relevant sleep modification protocol for youth with type 1 diabetes. Clin Pract Pediatr Psychol 4(2):227–240. https://doi.org/10.1037/cpp0000145
Donga E, van Dijk M, van Dijk JG et al (2010) Partial sleep restriction decreases insulin sensitivity in type 1 diabetes. Diabetes Care 33(7):1573–1577. https://doi.org/10.2337/dc09-2317
Blak B, Thompson M, Dattani H, Bourke A (2011) Generalisability of the health improvement network (THIN) database: demographics, chronic disease prevalence and mortality rates. Inform Prim Care 19(4):251–255. https://doi.org/10.14236/jhi.v19i4.820
Gibson JE (2009) Using data from primary care to investigate the epidemiology of motor vehicle crashes. Doctoral dissertation, University of Nottingham. http://eprints.nottingham.ac.uk/10871/
Weber DR, Haynes K, Leonard MB, Willi SM, Denburg MR (2015) Type 1 diabetes is associated with an increased risk of fracture across the life span: a population-based cohort study using the health improvement network (THIN). Diabetes Care 38(10):1913–1920. https://doi.org/10.2337/dc15-0783
Maguire A, Blak BT, Thompson M (2009) The importance of defining periods of complete mortality reporting for research using automated data from primary care. Pharmacoepidemiol Drug Saf 18(1):76–83. https://doi.org/10.1002/pds.1688
Graveling AJ, Frier BM (2015) Driving and diabetes: problems, licensing restrictions and recommendations for safe driving. Clin Diabetes Endocrinol 1(1):8. https://doi.org/10.1186/s40842-015-0007-3
Sharafkhaneh A, Giray N, Richardson P, Young T, Hirshkowitz M (2005) Association of psychiatric disorders and sleep apnea in a large cohort. Sleep 28(11):1405–1411. https://doi.org/10.1093/sleep/28.11.1405
Gupta MA, Simpson FC (2015) Obstructive sleep apnea and psychiatric disorders: a systematic review. J Clin Sleep Med 11(2):165–175. https://doi.org/10.5664/jcsm.4466
Gupta MA, Simpson FC, Lyons DCA (2016) The effect of treating obstructive sleep apnea with positive airway pressure on depression and other subjective symptoms: a systematic review and meta-analysis. Sleep Med Rev 28:55–68. https://doi.org/10.1016/j.smrv.2015.07.002
Dahlqvist S, Rosengren A, Gudbjornsdottir S et al (2017) Risk of atrial fibrillation in people with type 1 diabetes compared with matched controls from the general population: a prospective case-control study. Lancet Diabetes Endocrinol 5(10):799–807. https://doi.org/10.1016/s2213-8587(17)30262-0
Christensen MA, Dixit S, Dewland TA et al (2018) Sleep characteristics that predict atrial fibrillation. Heart Rhythm 15(9):1289–1295. https://doi.org/10.1016/j.hrthm.2018.05.008
Holmqvist F, Guan N, Zhu Z et al (2015) Impact of obstructive sleep apnea and continuous positive airway pressure therapy on outcomes in patients with atrial fibrillation – results from the outcomes registry for better informed treatment of atrial fibrillation (ORBIT-AF). Am Heart J 169(5):647–654. https://doi.org/10.1016/j.ahj.2014.12.024
Stevenson IH, Teichtahl H, Cunnington D, Ciavarella S, Gordon I, Kalman JM (2008) Prevalence of sleep disordered breathing in paroxysmal and persistent atrial fibrillation patients with normal left ventricular function. Eur Heart J 29(13):1662–1669. https://doi.org/10.1093/eurheartj/ehn214
Gami AS, Pressman G, Caples SM et al (2004) Association of atrial fibrillation and obstructive sleep apnea. Circulation 110:364–367. https://doi.org/10.1161/01.CIR.0000136587.68725.8E
Abumuamar AM, Dorian P, Newman D, Shapiro CM (2018) The prevalence of obstructive sleep apnea in patients with atrial fibrillation. Clin Cardiol 41(5):601–607. https://doi.org/10.1002/clc.22933
Iqbal G, Johnson MRD, Szczepura A, Gumber A, Wilson S, Dunn JA (2012) Ethnicity data collection in the UK: the healthcare professional's perspective. Divers Equality Health Care 9(4):281–290
Harding S, Greenwood R, Aldington S et al (2003) Grading and disease management in national screening for diabetic retinopathy in England and Wales. Diabet Med 20(12):965–971. https://doi.org/10.1111/j.1464-5491.2003.01077.x
Data availability
THIN data governance does not allow us to share individual patient data. Researchers may apply for individual patient data access at https://www.iqvia.com/contact.
Funding
Ziyad Alshehri was supported by a PhD scholarship from Taibah University through the Saudi Arabian Cultural Bureau in London.
Authors’ relationships and activities
AAT reports grants from Novo Nordisk, personal fees from Novo Nordisk, non-financial support from Novo Nordisk, personal fees from Eli Lilly, non-financial support from Eli Lilly, personal fees from Janssen, personal fees from AstraZeneca, non-financial support from AstraZeneca, non-financial support from Impeto Medical, non-financial support from ResMed, non-financial support from Aptiva, personal fees from Boehringer Ingelheim, non-financial support from Boehringer Ingelheim, personal fees from BMS, non-financial support from BMS, personal fees from Napp, non-financial support from Napp, personal fees from MSD, non-financial support from MSD, personal fees from Nestlé, personal fees from Gilead, grants from Sanofi, and personal fees from Sanofi outside the submitted work. AAT is currently an employee of Novo Nordisk. This work was performed before becoming a Novo Nordisk employee, and Novo Nordisk had no role in this project. KN has been awarded research grants from the NIHR, the UKRI/MRC, the Kennedy Trust for Rheumatology Research, Health Data Research UK, the Wellcome Trust, the European Regional Development Fund, the Institute for Global Innovation, Boehringer Ingelheim, Action Against Macular Degeneration Charity, Midlands Neuroscience Teaching and Development Funds, the South Asian Health Foundation, Vifor Pharma, the College of Police and CSL Behring (all payments were made to his academic institution); he also received consulting fees from Boehringer Ingelheim, Sanofi, Cegedim and MSD, and holds a leadership/fiduciary role with NICST, a charity, and OpenClinical, a social enterprise.
Contribution statement
ZA, CJR, PK, KN and AAT were responsible for the concept and design of the study. AS, NJA, KMG and KN contributed to data acquisition. ZA, AS, NJA, MAK, CJR, PK, KN, AAT contributed to the analysis and interpretation of data. ZA, CJR, PK and AAT drafted the manuscript. All authors revised the manuscript critically and approved the final version. ZA, AS, AAT and KN had full access to all the data in the study, and take responsibility for the integrity of the data and the accuracy of the data analysis.
Funding
Ziyad Alshehri was supported by a PhD scholarship from Taibah University through the Saudi Arabian Cultural Bureau in London.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(PDF 720 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Alshehri, Z., Subramanian, A., Adderley, N.J. et al. Risk of incident obstructive sleep apnoea in patients with type 1 diabetes: a population-based retrospective cohort study. Diabetologia 65, 1353–1363 (2022). https://doi.org/10.1007/s00125-022-05714-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-022-05714-5