Abstract
Aims/hypothesis
Mortality has declined in people with type 1 diabetes in recent decades. We examined how the pattern of decline differs by country, age and sex, and how mortality trends in type 1 diabetes relate to trends in general population mortality.
Methods
We assembled aggregate data on all-cause mortality during the period 2000–2016 in people with type 1 diabetes aged 0–79 years from Australia, Denmark, Latvia, Scotland, Spain (Catalonia) and the USA (Kaiser Permanente Northwest). Data were obtained from administrative sources, health insurance records and registries. All-cause mortality rates in people with type 1 diabetes, and standardised mortality ratios (SMRs) comparing type 1 diabetes with the non-diabetic population, were modelled using Poisson regression, with age and calendar time as quantitative variables, describing the effects using restricted cubic splines with six knots for age and calendar time. Mortality rates were standardised to the age distribution of the aggregate population with type 1 diabetes.
Results
All six data sources showed a decline in age- and sex-standardised all-cause mortality rates in people with type 1 diabetes from 2000 to 2016 (or a subset thereof), with annual changes in mortality rates ranging from −2.1% (95% CI −2.8%, −1.3%) to −5.8% (95% CI −6.5%, −5.1%). All-cause mortality was higher for male individuals and for older individuals, but the rate of decline in mortality was generally unaffected by sex or age. SMR was higher in female individuals than male individuals, and appeared to peak at ages 40–70 years. SMR declined over time in Denmark, Scotland and Spain, while remaining stable in the other three data sources.
Conclusions/interpretation
All-cause mortality in people with type 1 diabetes has declined in recent years in most included populations, but improvements in mortality relative to the non-diabetic population are less consistent.
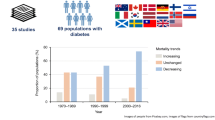
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.

Introduction
The overall age-standardised mortality in general populations, primarily from cardiovascular disease [1, 2], has been decreasing since the 1970s. In line with this, mortality in type 1 diabetes has also declined, primarily because of better diabetes care and prevention of complications [3,4,5,6,7,8,9]. However, most of the studies on mortality trends in type 1 diabetes focus on children and young adults [6, 9, 10], and there are few studies assessing mortality trends in type 1 diabetes across a broader age range [3,4,5, 7, 8]. Deaths in younger individuals with type 1 diabetes are rare, and are predominantly caused by acute complications. Secular mortality trends in middle-aged and older adults, for whom chronic complications dominate the causes of death [11, 12], and among whom the vast majority of deaths in type 1 diabetes occur, may differ markedly from those in younger adults. One earlier study reported the trends in cumulative mortality by calendar period of diagnosis in people with early and late onset of type 1 diabetes [13], but studies of age-specific trends in all-cause mortality in type 1 diabetes are scarce [4].
People with type 1 diabetes have a significantly higher risk of all-cause mortality than do people without diabetes [3, 8,9,10, 14,15,16]. However, it is not clear how this excess risk of all-cause death in people with type 1 diabetes has changed over time, and whether this has varied by sex, age or country.
Large observational studies with long follow-up times are needed to monitor these trends and to understand whether improvements in treatment have not only reduced all-cause mortality rates but have also narrowed the mortality gap between those with type 1 diabetes and the general population. Elucidating these mortality trends can help identify sub-populations in need of targeted intervention. Therefore, the aim of this study was to assess the trends in the absolute all-cause mortality rates among people with type 1 diabetes and trends in excess mortality in type 1 diabetes relative to those without diabetes in six countries, and to investigate whether the changes in both absolute and relative mortality rates over time varied by country, age and sex.
Methods
Data sources
This study used aggregate data on all-cause mortality in people with type 1 diabetes from an international diabetes consortium database, which has assembled longitudinal data on diabetes incidence and all-cause mortality from 24 predominantly administrative data sources in 21 countries or sub-national regions [17]. Of these datasets, seven included mortality data specifically for type 1 diabetes. After excluding data from Israel, which only had data for people with type 1 diabetes aged <50 years, we included data on people with type 1 diabetes aged 0–79 years from Australia, Denmark, Latvia, Scotland, Spain (Catalonia) and the USA (Kaiser Permanente Northwest [KPNW]) in the current analysis. Each data source provided aggregate data for each calendar year on population size, counts of prevalent and incident type 1 diabetes, death counts and person-years in people with type 1 diabetes and in people without diabetes, by sex and 5-year age-group (<20, 20–24, 25–29, …, 70–74, 75–79 years) from 2000 to 2016 (or a subset of this time period) (Table 1). This study was approved by the Human Ethics Committee of Alfred Health, Melbourne, Australia.
Assessment of diabetes status
Diabetes status was determined on the basis of clinical diagnosis by healthcare professionals or based on ICD-10 codes (http://apps.who.int/classifications/icd10/browse/2016/en) in the data from Australia, Latvia, Scotland and Spain (Catalonia), and using algorithms incorporating clinical diagnosis, linkage to medication or reimbursement registries and measurement of blood glucose or HbA1c in Denmark and the USA (KPNW) data sources (Table 1 and electronic supplementary material [ESM] Table 1). Further, people were classified as having type 1 diabetes based on the ICD codes recorded in the database (Latvia, Spain [Catalonia] and the USA [KPNW] [18]) and criteria based on age at diagnosis or prescription history in addition to a diagnostic code of type 1 diabetes (Australia [19], Denmark [8] and Scotland [9]) (ESM Table 1).
Outcome
Death in people with diabetes was determined by linkage to the death registries within each respective country or region. Sex- and age-specific numbers of deaths from any cause for the general population were obtained from the General Records of Incidence of Mortality (Australia), Statistics Denmark’s databank (Denmark), the National Records of Scotland’s mortality database (Scotland) and the Human Mortality Database (Latvia). For Spain (Catalonia) and the USA (KPNW), death in people without diabetes was determined by linkage to death registries.
Quality of the included data sources
We assessed the quality of the included data and the risk of bias using a modified Newcastle−Ottawa scale [20] (details in ESM Methods). This modified scale included items that assess representativeness of the study population, the method of assessing diabetes status, whether gestational diabetes could be excluded, sample size at each time point, the method of assessing outcomes, and the number of data points (years) reported.
Statistical analysis
We modelled mortality rates using age and calendar time as quantitative variables, scored as the midpoint of each age group (5 years) and calendar time interval (1 year). We used Poisson likelihood for multiplicative models, with death as the outcome and log person-years as offset. For the data source from Latvia, which did not have data on person-years in people with type 1 diabetes, we computed person-years in each year as the number of people with prevalent type 1 diabetes at the beginning of each year, plus half the number of people with incident type 1 diabetes in that year, minus half the number of deaths occurring in people with type 1 diabetes in that year. This computation assumes that new diabetes cases and deaths are uniformly distributed over each year. The numbers of deaths and person-years in people without diabetes reflect the population without any form of diabetes (Australia), or the population without type 1 or type 2 diabetes (other five data sources). We fitted age–period–cohort models [21] using cubic splines for the effects. Knots for the splines were placed at evenly spaced quantiles of the marginal distribution of the event times for each of the three variables in the model (age, period [calendar time] and cohort [period minus age]). Specifically, there were six knots for age, one knot per 4 years of period and four knots for cohort. For each data source and sex, we plotted the estimated mortality rates by age for a select set of dates 4 years apart, spanning the observation period, as well as mortality rates by period for five selected ages (40, 50, 60, 70 and 80 years). The estimated rates from the age–period–cohort models were used to calculate the age-standardised mortality rates using direct standardisation (using a type 1 diabetes population assembled from pooling the six data sources). We also fitted a set of age–period models with smooth age effects but a linear effect of calendar time for each data source, providing an overall summary of the annual changes in mortality rates for total people with type 1 diabetes and for male and female individuals separately. 95% CIs were computed as Wald CIs (back-transformed from log rates ±1.96 SE) [22]. We classified the mortality trend as ‘increasing’ if the point estimate of annual change was positive and the 95% CI excluded zero. Conversely, a trend was defined as ‘decreasing’ if the annual change was negative and its 95% CI excluded zero. When the 95% CI of the annual change included zero, we classified the trend as ‘unchanged’ (i.e. the change was not statistically significant).
Standardised mortality ratios (SMRs) were calculated by modelling the mortality rates in the entire population stratified by diabetes status, i.e. people with type 1 diabetes and people without diabetes [23]. An SMR of 1 indicates an equivalent mortality risk to the age- and sex-matched population without diabetes. A decline in SMR by calendar time implies that mortality rates among people with diabetes declined faster than among people without. The SMR was modelled in a similar way to the mortality rates, using Poisson likelihood for multiplicative models with observed number of deaths as outcomes and the log of expected number of deaths as the offset. As for mortality rates, we fitted models with a linear effect of calendar time for each data source, providing an overall summary of the annual changes in SMRs separately for each data source.
Stata software version 15.1 (Stata Corporation, College Station, TX, USA) was used for data management, and R software version 3.6.3 (R Foundation for Statistical Computing, Vienna, Austria) was used for statistical analyses and graphics.
Results
Table 1 shows details for the six included data sources. All were from high-income countries: four European populations (Denmark, Latvia, Scotland and Spain), Australia and the USA. Four studies included national data, one study included regional data from Spain (Catalonia), and another study included data from a US regional health insurance database (KPNW) (Table 1). Quality scores for the data sources ranged from 5 to 9, with a median of 7 (IQR 6–8) (ESM Table 2).
There were 18,105 deaths (11,355 deaths in male individuals and 6750 in female individuals) during 1.55 million person-years of follow-up in 179,514 individuals with type 1 diabetes aged 0–79 years (Table 1, ESM Table 3). Overall, the ratio of male to female individuals with type 1 diabetes was 1.28 in the six included data sources, and the crude all-cause mortality rate was 11.7 (95% CI 11.5, 11.9) per 1000 person-years for all individuals with type 1 diabetes. The crude mortality rate was 13.2 (95% CI 12.9, 13.4) per 1000 person-years in male individuals, and 9.9 (95% CI 9.6, 10.1) per 1000 person-years in female individuals (ESM Fig. 1).
Trends in all-cause mortality rates among people with type 1 diabetes
The age- and sex-standardised all-cause mortality rate for each calendar year was highest in Latvia and lowest in Spain (Fig. 1, ESM Table 4). All six data sources showed a decline in the age- and sex-standardised all-cause mortality rates in people with type 1 diabetes over the whole study period, with annual estimated changes in mortality rates ranging from −2.1% (95% CI −2.8%, −1.3%) in Australia to −5.8% (95% CI −6.5%, −5.1%) in Denmark (Figs. 1 and 2a, ESM Table 5). In Latvia, the mortality remained relatively stable from approximately 2009 to 2016 (Fig. 1, ESM Table 4). Sex-specific mortality trends analysis showed that, over the whole study period, mortality declined in all male populations and in four female populations (Fig. 2c, ESM Fig. 2, ESM Table 5). Among Latvian female individuals, mortality fell for the first few years, and then rose until the end of the reporting period (2016), with an annual estimated change in mortality rates of −2.1% (95% CI −4.5%, 0.3%); among Spanish female individuals, the annual change in mortality rates was −3.3% (95% CI −7.5%, 1.1%).
Age- and sex-standardised all-cause mortality rates in people with type 1 diabetes by calendar year. Standardisation is based on annual age-specific mortality rates from age–period–cohort models fitted separately for each data source and sex. The standard population was derived from the pooled study population with type 1 diabetes within the six data sources, with equal weights for male and female individuals. Shaded areas represent 95% CIs around mortality trends. The y-axis is plotted on a natural logarithmic scale. aData are from Catalonia, Spain
Annual estimated change in all-cause mortality rates in type 1 diabetes (a, c) and annual estimated change in SMR in type 1 diabetes relative to those without diabetes (b, d), in all individuals (a, b) and in male and female individuals separately (c, d). Data in (a, b) are ordered according to the magnitude of annual change in all-cause mortality rates in people with type 1 diabetes. Blue lines, male; red lines, female. Error bars indicate 95% CIs. aData are from Catalonia, Spain. SMR, standardised mortality ratio
Trends in all-cause mortality rates in people with type 1 diabetes by age
ESM Figs. 3–8 present the age-specific and calendar time-specific all-cause mortality rates by sex for each data source. In general, all-cause mortality was higher for male individuals and for older individuals (ESM Figs. 2–8), but the rate of decline in mortality was generally unaffected by sex or age. An age by time interaction of mortality rates (estimated annual change in mortality by age) in each data source is shown in ESM Fig. 9. All-cause mortality rates decreased over time across ages in all data sources, except Latvia. Reductions in mortality rates over time appeared to be greater in people at older ages than younger ages for Australia and Denmark, and were similar across ages for the remainder.
Trends in SMRs between people with type 1 diabetes and those without diabetes
Trends in SMRs in people with type 1 diabetes relative to people without diabetes are presented in Fig. 2b and ESM Table 5. The annual estimated change in SMR between type 1 diabetes and non-diabetes ranged from −6.3% (95% CI −8.8%, −3.8%) in Spain to 1.1% (95% CI −0.4%, 2.5%) in Latvia. Denmark, Scotland and Spain showed declines in SMRs over the whole study period, indicating larger declines in all-cause mortality rates among people with type 1 diabetes compared with those without diabetes. SMRs were stable in the other three data sources. Annual estimated changes in SMRs by sex were similar to those changes for male and female individuals combined (Fig. 2b,d, ESM Fig. 10 and ESM Table 5).
Trends in SMRs in people with type 1 diabetes relative to those without diabetes by age and sex
ESM Figs. 11–16 present the age-specific and calendar time-specific SMR trends by sex for each data source. All-cause mortality rates were two to five times higher in people with type 1 diabetes than those without diabetes (Fig. 3), and were significantly elevated across all ages (ESM Figs. 11–16). For each data source, the SMR was higher in female individuals than male individuals at all ages for most calendar years, except in the USA (KPNW), which showed higher SMRs in older male individuals than older female individuals. In Denmark, SMR fell progressively with increasing age, but in other data sources, SMR rose to a peak at ages between 40 and 70 years old, and then fell. Denmark, Scotland and Spain showed a decrease in SMRs over the study period at all ages in both male and female individuals. Australia showed a decline in SMR among older individuals at ages 70 and 80 years but stable SMRs in younger individuals for both sexes. In Latvian female individuals, SMR initially fell, but then rose after about 2009. SMR was relatively stable across five selected ages in Latvian male individuals and in both sexes for the USA (KPNW).
SMR in people with type 1 diabetes compared with those without diabetes by calendar year. Smoothing is based on a model with SMR constant over age and sex. Shaded areas represent 95% CIs. The y-axis is plotted on a natural logarithmic scale. aData are from Catalonia, Spain. SMR, standardised mortality ratio
Discussion
Using contemporary aggregate data on all-cause mortality in people with type 1 diabetes from six data sources in high-income countries, we obtained four key findings. First, all data sources showed a decline in the age- and sex-standardised all-cause mortality rates in people with type 1 diabetes aged 0–79 years from 2000 to 2016 (or a subset thereof), with an annual estimated change in mortality rates ranging from −2.1% (95% CI −2.8%, −1.3%) to −5.8% (95% CI −6.5%, −5.1%). Furthermore, annual mortality rates declined in most country- and sex-specific populations, although this decline was not statistically significant in the Latvian and Spanish female populations. Second, mortality declined at a wide range of ages for most data sources. Third, the SMR, reflecting excess mortality, fell in half of the six included data sources. Fourth, despite reductions in absolute all-cause mortality rates, and, in some countries, in the SMR, people with type 1 diabetes still had a two to five times higher risk of death compared with those without diabetes.
Our observation of the decline in the age-standardised mortality rates in most populations with type 1 diabetes is consistent with previous studies from these countries for other time periods, with mortality declines among male and female populations with type 1 diabetes being reported in Australia (2000–2011) [4], Denmark (2005–2016) [8] and Scotland (from 2006–2010 to 2011–2015) [7]. Cardiovascular diseases are a major cause of deaths in individuals with type 1 diabetes [11, 12], although other important contributors to excess mortality include renal diseases, cancer and infectious diseases. Decreasing mortality in people with type 1 diabetes may be attributable to the advances in treatment and interventions for type 1 diabetes, as well as improvement in cardiovascular disease prevention with widespread use of statins and anti-hypertensive medications over the last two decades.
Despite reductions in all-cause mortality rates in people with type 1 diabetes in most populations studied, the improvement in the excess risk of all-cause death among people with type 1 diabetes relative to the non-diabetic population was less evident, with SMR decreasing in only three of the six data sources over the study period. Previous data from Australia showed that there was a reduction in excess all-cause mortality among both male and female individuals with type 1 diabetes aged 0–75 years between 1997 and 2010 [14]. A recent analysis of the Danish Diabetes Register reported that the SMR declined by approximately 2% per year for both sexes in the entire population with type 1 diabetes between 2005 and 2016 [8]. However, a cohort study from Sweden showed a decreased mortality rate among adults with type 1 diabetes from 1998 to 2014, but they did not find a similar decline in the excess mortality relative to the general population [5].
Similar to other studies [3], absolute mortality rates in people with type 1 diabetes increased with increasing age, while the excess mortality for type 1 diabetes relative to those without diabetes decreased with increasing age. As has been reported previously [9, 16], we found that the SMR associated with type 1 diabetes was higher among female individuals than male individuals across all ages for most calendar years. We also noted that mortality declined over the study period across most ages for both male and female individuals, while SMR declined at all ages examined in only three out of six data sources. Studies of age-specific trends in all-cause mortality rates or excess mortality in people with type 1 diabetes are scarce, and most were restricted to younger individuals with type 1 diabetes [6, 9, 10, 14]. Previous work from our group indicated that age-specific SMRs in people with type 1 diabetes in Australia did not significantly change between 1997–2003 and 2004–2010 [14]. A cohort study of individuals diagnosed with type 1 diabetes before the age of 15 years from Northern Ireland did not find a significant change in either all-cause mortality rates or corresponding SMR associated with type 1 diabetes from 1989 to 2012 [10]. Studies in Uzbekistan (1998–2014) [6] and Scotland (2004–2017) [9] identified mortality reductions in children <15 years and in people aged below 50 years, respectively. However, there was no improvement in excess mortality for individuals with type 1 diabetes under age 50 years in Scotland from 2004 to 2017 [9].
Despite reductions in absolute all-cause mortality rates, and, in some countries, in the SMR, type 1 diabetes still confers a higher excess risk of death compared with individuals without diabetes. Suboptimal glycaemic control and the presence of acute and chronic complications are key contributors to excess risk of death in type 1 diabetes [3, 9, 15]. Even among people with type 1 diabetes who have an HbA1c below the target level of 53 mmol/mol (7.0%), the risk of all-cause mortality is still twice that of the general population [15]. Evidence shows that intensive insulin therapy is associated with a decreased all-cause mortality compared with conventional therapy, with a persistent benefit more than 30 years later [24, 25]. However, data from the USA T1D Exchange Clinic Network showed that there was an increase in mean HbA1c from 62 mmol/mol (7.8%) to 68 mmol/mol (8.4%) between 2010–2012 and 2016–2018 [26]. More recent Scottish data showed that, despite an overall declining trend in HbA1c level from 70 mmol/mol (8.6%) to 68 mmol/mol (8.4%) in people with type 1 diabetes (2012–2016), more than one-third of all those with type 1 diabetes still had poor glycaemic control with an HbA1c> 75 mmol/mol (>9%) in 2016 [27]. Poor glycaemic control in younger people with type 1 diabetes increases the risk of developing complications when they age [25], and increases the risk of death from any cause or from cardiovascular causes [15]. In addition to glycaemic management, data from the Swedish National Diabetes Register suggested a steep increase in the excess risk of all-cause death with decreasing number of cardiovascular risk factors (BP, LDL-cholesterol, smoking and albuminuria) meeting target levels among people with type 1 diabetes [28].
Strengths and weaknesses
A key strength of this work is that we have assembled six large population-based cohorts, with a sizeable number of people with type 1 diabetes and a long study period to enable us to provide estimates of time trends in all-cause mortality rates in six countries, and by sex and age categories. To the best of our knowledge, this work is the only study of this kind, and provides the most recent data on mortality trends in people with type 1 diabetes across a broader age range. Four out of six sources were national diabetes registries, which cover the entire population with type 1 diabetes in those countries.
Several potential limitations of our study should be considered. First, misclassification of diabetes type cannot be ruled out. Algorithms based on clinical criteria, medication use and laboratory measurements are commonly used in administrative databases and diabetes registries to assign diabetes type. However, the absence of some laboratory data from the database, such as autoantibody or C-peptide levels, may lead to misclassification of diabetes type. The use of algorithms to classify type 1 diabetes based on age at diagnosis in some data sources may exclude those with older-onset type 1 diabetes [29], which means that the mortality rates in type 1 diabetes may be underestimated. However, within each data source, the same approach was used to classify diabetes type across time periods, therefore mortality trends are less likely to be affected by the potential misclassification of older-onset type 1 diabetes. Second, we did not have access to individual clinical data. Therefore, we could not determine whether mortality trends in people with type 1 diabetes were due to changes in glycaemic control, changes in other risk factors, or differences in the prevalence of acute or chronic diabetes-related complications over time. Moreover, improved survival over time will increase diabetes duration, an important risk factor for mortality, which may have attenuated improvements in age-specific mortality rates. We did not have access to data on age at diagnosis of type 1 diabetes or diabetes duration, and thus could not examine the relationship of mortality with duration of diabetes. As data were not available for risk factors in people with and without diabetes, we were not able to investigate possible explanations for the excess risk of mortality among people with type 1 diabetes. Third, the sample size was variable between the six data sources, with a relatively small number of people with type 1 diabetes in the data sources from Spain (Catalonia), the USA (KPNW) and Latvia. Fourth, the six data sources only represent high-income countries; therefore, our results may not be generalisable to middle- and low-income countries where patterns of mortality trends in people with type 1 diabetes remain uncertain. Fifth, we did not have data on ethnicity, socioeconomic status or population immigration. Finally, our data are limited in terms of the time period covered by some data sources.
Conclusions
This is the first multicountry analysis of six large contemporary population-based studies, and shows that all-cause mortality in people with type 1 diabetes has declined in recent years in most studied populations. However, excess mortality relative to the population without diabetes remains high in people with type 1 diabetes. Considering the increasing incidence of type 1 diabetes observed in younger populations in recent years [8, 30, 31], it is critical to continuously improve the multidimensional management of type 1 diabetes, particularly among younger populations.
Data availability
Aggregate data may be available upon reasonable request to the corresponding author. There might be limitations on what the data can be used for, subject to approval from the data custodians.
Abbreviations
- KPNW:
-
Kaiser Permanente Northwest
- SMR:
-
Standardised mortality ratio
References
Capewell S, Morrison CE, McMurray JJ (1999) Contribution of modern cardiovascular treatment and risk factor changes to the decline in coronary heart disease mortality in Scotland between 1975 and 1994. Heart 81(4):380–386. https://doi.org/10.1136/hrt.81.4.380
Ford ES, Ajani UA, Croft JB et al (2007) Explaining the decrease in U.S. deaths from coronary disease, 1980-2000. N Engl J Med 356(23):2388–2398. https://doi.org/10.1056/NEJMsa053935
Jorgensen ME, Almdal TP, Carstensen B (2013) Time trends in mortality rates in type 1 diabetes from 2002 to 2011. Diabetologia 56(11):2401–2404. https://doi.org/10.1007/s00125-013-3025-7
Harding JL, Shaw JE, Peeters A, Davidson S, Magliano DJ (2016) Age-specific trends from 2000-2011 in all-cause and cause-specific mortality in type 1 and type 2 diabetes: a cohort study of more than one million people. Diabetes Care 39(6):1018–1026. https://doi.org/10.2337/dc15-2308
Rawshani A, Rawshani A, Franzen S et al (2017) Mortality and cardiovascular disease in type 1 and type 2 diabetes. N Engl J Med 376(15):1407–1418. https://doi.org/10.1056/NEJMoa1608664
Rakhimova GN, Alimova NU, Ryaboshtan A, Waldman B, Ogle GD, Ismailov SI (2018) Epidemiological data of type 1 diabetes mellitus in children in Uzbekistan, 1998-2014. Pediatr Diabetes 19(1):158–165. https://doi.org/10.1111/pedi.12495
Campbell RAS, Colhoun HM, Kennon B et al (2020) Socio-economic status and mortality in people with type 1 diabetes in Scotland 2006-2015: a retrospective cohort study. Diabet Med 37(12):2081–2088. https://doi.org/10.1111/dme.14239
Carstensen B, Ronn PF, Jorgensen ME (2020) Prevalence, incidence and mortality of type 1 and type 2 diabetes in Denmark 1996-2016. BMJ Open Diabetes Res Care 8(1):e001071. https://doi.org/10.1136/bmjdrc-2019-001071
O'Reilly JE, Blackbourn LAK, Caparrotta TM et al (2020) Time trends in deaths before age 50 years in people with type 1 diabetes: a nationwide analysis from Scotland 2004-2017. Diabetologia 63(8):1626–1636. https://doi.org/10.1007/s00125-020-05173-w
Morgan E, Black CR, Abid N, Cardwell CR, McCance DR, Patterson CC (2018) Mortality in type 1 diabetes diagnosed in childhood in Northern Ireland during 1989-2012: a population-based cohort study. Pediatr Diabetes 19(1):166–170. https://doi.org/10.1111/pedi.12539
Livingstone SJ, Levin D, Looker HC et al (2015) Estimated life expectancy in a Scottish cohort with type 1 diabetes, 2008-2010. JAMA 313(1):37–44. https://doi.org/10.1001/jama.2014.16425
Huo L, Harding JL, Peeters A, Shaw JE, Magliano DJ (2016) Life expectancy of type 1 diabetic patients during 1997-2010: a national Australian registry-based cohort study. Diabetologia 59(6):1177–1185. https://doi.org/10.1007/s00125-015-3857-4
Harjutsalo V, Forsblom C, Groop PH (2011) Time trends in mortality in patients with type 1 diabetes: nationwide population based cohort study. BMJ 343:d5364. https://doi.org/10.1136/bmj.d5364
Harding JL, Shaw JE, Peeters A, Guiver T, Davidson S, Magliano DJ (2014) Mortality trends among people with type 1 and type 2 diabetes in Australia: 1997-2010. Diabetes Care 37(9):2579–2586. https://doi.org/10.2337/dc14-0096
Lind M, Svensson AM, Kosiborod M et al (2014) Glycemic control and excess mortality in type 1 diabetes. N Engl J Med 371(21):1972–1982. https://doi.org/10.1056/NEJMoa1408214
Huxley RR, Peters SA, Mishra GD, Woodward M (2015) Risk of all-cause mortality and vascular events in women versus men with type 1 diabetes: a systematic review and meta-analysis. Lancet Diabetes Endocrinol 3(3):198–206. https://doi.org/10.1016/S2213-8587(14)70248-7
Magliano DJ, Chen L, Islam RM et al (2021) Trends in the incidence of diagnosed diabetes: a multicountry analysis of aggregate data from 22 million diagnoses in high-income and middle-income settings. Lancet Diabetes Endocrinol 9(4):203–211. https://doi.org/10.1016/S2213-8587(20)30402-2
Schroeder EB, Donahoo WT, Goodrich GK, Raebel MA (2018) Validation of an algorithm for identifying type 1 diabetes in adults based on electronic health record data. Pharmacoepidemiol Drug Saf 27(10):1053–1059. https://doi.org/10.1002/pds.4377
Sacre JW, Harding JL, Shaw JE, Magliano DJ (2021) Declining mortality in older people with type 2 diabetes masks rising excess risks at younger ages: a population-based study of all-cause and cause-specific mortality over 13 years. Int J Epidemiol 50(4):1362–1372. https://doi.org/10.1093/ije/dyaa270
Wells G, Shea B, O’Connell D et al (2014) The Newcastle–Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Available from http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 11 Apr 2019
Carstensen B (2007) Age–period–cohort models for the Lexis diagram. Stat Med 26(15):3018–3045. https://doi.org/10.1002/sim.2764
Carstensen B (2021) Epidemiology with R. Oxford University Press, Oxford
Keiding N (1987) The method of expected number of deaths, 1786–1886–1986. Int Stat Rev 55(1):1–20
Diabetes Control and Complications Trial Research Group, Nathan DM, Genuth S et al (1993) The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 329(14):977–986. https://doi.org/10.1056/NEJM199309303291401
Orchard TJ, Nathan DM, Zinman B et al (2015) Association between 7 years of intensive treatment of type 1 diabetes and long-term mortality. JAMA 313(1):45–53. https://doi.org/10.1001/jama.2014.16107
Foster NC, Beck RW, Miller KM et al (2019) State of type 1 diabetes management and outcomes from the T1D exchange in 2016-2018. Diabetes Technol Ther 21(2):66–72. https://doi.org/10.1089/dia.2018.0384
Mair C, Wulaningsih W, Jeyam A et al (2019) Glycaemic control trends in people with type 1 diabetes in Scotland 2004-2016. Diabetologia 62(8):1375–1384. https://doi.org/10.1007/s00125-019-4900-7
Rawshani A, Rawshani A, Franzen S et al (2017) Range of risk factor levels: control, mortality, and cardiovascular outcomes in type 1 diabetes mellitus. Circulation 135(16):1522–1531. https://doi.org/10.1161/CIRCULATIONAHA.116.025961
Stene LC (2016) Gaps in life expectancy for people with type 1 diabetes. Diabetologia 59(6):1150–1152. https://doi.org/10.1007/s00125-016-3943-2
Luk AOY, Ke C, Lau ESH et al (2020) Secular trends in incidence of type 1 and type 2 diabetes in Hong Kong: a retrospective cohort study. PLoS Med 17(2):e1003052. https://doi.org/10.1371/journal.pmed.1003052
Mayer-Davis EJ, Lawrence JM, Dabelea D et al (2017) Incidence trends of type 1 and type 2 diabetes among youths, 2002-2012. N Engl J Med 376(15):1419–1429. https://doi.org/10.1056/NEJMoa1610187
Acknowledgements
We thank the people with diabetes, health service staff and organisations involved in providing data and setting up, maintaining and overseeing collation of data for people with diabetes in Scotland. Scottish data linkage and provision were provided by the Information Services Division of NHS National Services Scotland. We acknowledge the work by those at Diabetes Australia and the Australian Institute of Health and Welfare for supplying the Australian data. We acknowledge all data custodians providing aggregate data to this study.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. The study was funded by the Centers for Disease Control and Prevention, USA and a Diabetes Australia Research Program grant. The funder of the study (the Centers for Disease Control and Prevention) was part of the study group, and contributed to study design, data interpretation and editing of the report. The findings and conclusions in this report are those of the authors, and do not necessarily represent the official position of the Centers for Disease Control and Prevention. This work was partly supported by the Victoria State Government Operational Infrastructure Support Program, which did not play a role in study design/conduct, analysis/interpretation of data, or manuscript preparation. Data for Scotland were submitted on behalf of the Scottish Diabetes Research Network epidemiology group; this network is supported by NHS Research Scotland. PLDR is supported by a grant from the South-Eastern Norway Regional Health Authority. JIM is supported by an Australian Government Research Training Program Scholarship and Monash Graduate Excellence Scholarship. JES is supported by a National Health and Medical Research Council Investigator Grant.
Author information
Authors and Affiliations
Contributions
The authors declare that there are no relationships or activities that might bias, or be perceived to bias, their work.
Contribution statement
DJM, EWG, MEP and JES conceived the study and made contacts with contributing centres. DJM and LC oversaw the practical gathering of data from the centres. LC was responsible for the database. PLDR, LC, AS and DJM designed and undertook the statistical analysis. PLDR and LC wrote the manuscript. All other authors curated data from centres into the standardised form. All authors contributed to data interpretation and critical evaluation, and editing of the report, and approved the final submitted version of the manuscript. PLDR, LC, AS and DJM verified the data and had access to raw data (aggregate). PLDR, LC, AS and DJM are guarantors of data and analysis integrity. JES and DJM had final responsibility for the decision to submit for publication.
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(PDF 1.27 mb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ruiz, P.L.D., Chen, L., Morton, J.I. et al. Mortality trends in type 1 diabetes: a multicountry analysis of six population-based cohorts. Diabetologia 65, 964–972 (2022). https://doi.org/10.1007/s00125-022-05659-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-022-05659-9