Abstract
Aims/hypothesis
Ceramide lipids have a role in the development of insulin resistance, diabetes and risk of cardiovascular disease. Here we investigated four ceramides and their ratios to find the best predictors of incident diabetes.
Methods
A validated mass-spectrometric method was applied to measure Cer(d18:1/16:0), Cer(d18:1/18:0), Cer(d18:1/24:0) and Cer(d18:1/24:1) from serum or plasma samples. These ceramides were analysed in a population-based risk factor study (FINRISK 2002, n = 8045), in a cohort of participants undergoing elective coronary angiography for suspected stable angina pectoris (Western Norway Coronary Angiography Cohort [WECAC], n = 3344) and in an intervention trial investigating improved methods of lifestyle modification for individuals at high risk of the metabolic syndrome (Prevent Metabolic Syndrome [PrevMetSyn], n = 371). Diabetes risk score models were developed to estimate the 10 year risk of incident diabetes.
Results
Analysis in FINRISK 2002 showed that the Cer(d18:1/18:0)/Cer(d18:1/16:0) ceramide ratio was predictive of incident diabetes (HR per SD 2.23, 95% CI 2.05, 2.42), and remained significant after adjustment for several risk factors, including BMI, fasting glucose and HbA1c (HR 1.34, 95% CI 1.14, 1.57). The finding was validated in the WECAC study (unadjusted HR 1.81, 95% CI 1.53, 2.14; adjusted HR 1.39, 95% CI 1.16, 1.66). In the intervention trial, the ceramide ratio and diabetes risk scores significantly decreased in individuals who had 5% or more weight loss.
Conclusions/interpretation
The Cer(d18:1/18:0)/Cer(d18:1/16:0) ratio is an independent predictive biomarker for incident diabetes, and may be modulated by lifestyle intervention.
Similar content being viewed by others
Avoid common mistakes on your manuscript.

Introduction
Type 2 diabetes is a serious progressive metabolic disorder in which the body becomes resistant to insulin and gradually loses the capacity to produce it in sufficient amounts. Worldwide, an estimated 422 million adults were afflicted by diabetes in 2014, and the global age-standardised prevalence has doubled since 1980, now being 8.5% in the adult population [1]. Type 2 diabetes can lead to severe complications, including kidney, retinal and neural damage, and accelerated cardiovascular disease resulting in myocardial infarctions or strokes [2].
According to WHO guidelines, type 2 diabetes is diagnosed if: (1) the fasting plasma glucose level is 7 mmol/l or higher; (2) the 2 h plasma glucose level is 11.1 mmol/l or higher during a glucose tolerance test; or (3) the HbA1c level is 47.5 mmol/mol (6.5%) or higher [1]. Prediabetes is an intermediate state of hyperglycaemia with glycaemic variables above normal but below the type 2 diabetes threshold; however, the exact diagnostic criteria of prediabetes are not uniform across various international professional organisations [3]. Importantly, lifestyle interventions affecting diet, weight management and physical activity significantly decrease the risk of conversion from the prediabetic state to type 2 diabetes [3]. Thus, identifying individuals at greatest risk and motivating them to lifestyle changes are highly important in the prevention of type 2 diabetes and its complications.
Ceramides are sphingolipids that have a crucial role in the development of type 2 diabetes and other cardiometabolic disorders. Several studies have investigated the role and mechanisms underlying the contribution of ceramides to the development of insulin resistance in various tissues [4, 5]. Moreover, it was recently demonstrated in both mice and humans that concentrations of plasma dihydroceramides, ceramide precursor molecules, are already elevated years before the onset of type 2 diabetes [6]. We previously described the value of three ceramides [Cer(d18:1/16:0), Cer(d18:1/18:0), Cer(d18:1/24:1)] and their ratios to Cer(d18:1/24:0) in predicting cardiovascular risk, especially cardiovascular death, in both secondary and primary prevention cardiovascular studies [7, 8]. Prior results suggest that one of these ceramides, Cer(d18:1/18:0), was also able to predict the risk of future type 2 diabetes [6]. The aim of the present study was to investigate how these cardiovascular disease-associated ceramides predict incident type 2 diabetes and are modulated by lifestyle intervention.
Methods
FINRISK 2002 study population
The FINRISK survey has been performed every 5 years since 1972 mainly to monitor trends in cardiovascular risk factors in the Finnish population [9]. The FINRISK 2002 study is a stratified random sample of the population aged 25–74 years from specific geographical areas of Finland. The survey included participants from North Karelia and Northern Savo in eastern Finland, the Turku and Loimaa regions in south-western Finland, the cities of Helsinki and Vantaa in the capital region, the provinces of Northern Ostrobothnia and Kainuu in north-western Finland and the province of Lapland in northern Finland. Sampling was stratified by sex, region and 10 year age groups so that each stratum contained 250 participants. In North Karelia, Lapland and the cities of Helsinki and Vantaa, the strata of 65–74-year-old men and women were also sampled, each with 250 participants. The original population sample was thus 13,500 (minus 64 who had died or moved away between sampling and the survey); the overall participation rate was 65.5%, including a questionnaire and a health examination during which blood samples were drawn. The study protocol was approved by the Coordinating Ethics Committee of the Helsinki and Uusimaa Hospital District and all participants gave written informed consent.
Serum samples from 8121 participants were available for the present study, and pregnant women (n = 46) as well as those with missing clinical variables (n = 30) were excluded from the data. This left 8045 participants, of whom 445 had prevalent type 2 diabetes and 593 developed incident type 2 diabetes during the follow-up. The participants were advised to fast for 4 h or longer and to avoid heavy meals earlier in the day. Serum was separated and stored at −70°C. Some analytes, such as conventional lipids, were measured immediately. The detailed methods have previously been described [9]. The authors had full access to the data used in this study. The participants were followed up until 31 December 2014, i.e. for 13 years. Only participants who had permanently moved abroad (<1%) before the disease event or 31 December 2014 were lost to follow-up. Prevalent diseases were defined as those that had developed prior to or at the baseline examination date, and incident events were those occurring thereafter. Individuals with incident diabetes during follow-up were identified by record linkage of the FINRISK 2002 data with the countrywide electronic health registers on the basis of the personal ID-code, unique to every permanent resident of Finland. Registers included the Causes-of-Death Register, Hospital Discharge Register and Drug Reimbursement Registers. This procedure has previously been described in detail [10].
All 45–74-year-old individuals were invited further to participate in a 2 h glucose tolerance test. In addition, HbA1c was measured in participants of all ages in North Karelia, the capital region and the Turku/Loimaa regions. Both fasting glucose and HbA1c measurements were available for 2119 participants; this population is referred to here as the FINRISK 2002 substudy.
Western Norway coronary angiography cohort study population
Citrate plasma samples were obtained from the Western Norway Coronary Angiography Cohort (WECAC), which consists of 5209 adults who underwent coronary angiography at Haukeland University Hospital, Bergen, or Stavanger University Hospital, Stavanger, in Norway between January 2000 and April 2004 [11]. The study was carried out according to the Declaration of Helsinki and approved by the Regional Committee for Medical and Health Research Ethics and the Norwegian Data Inspectorate. The primary aim of WECAC was to study various prognostic biomarkers of cardiovascular endpoints. WECAC includes 3090 participants who were randomised to participate in the Western Norway B vitamin Intervention Trial (WENBIT; ClinicalTrials.gov number NCT00354081) to investigate the effect of B vitamin supplementation on mortality and cardiovascular events [12]. The trial did not find an effect of treatment with folic acid/vitamin B12 or B6 on cardiovascular events or total mortality [12].
Altogether, 4634 baseline samples were analysed, and only participants examined because of suspected stable angina pectoris were considered for the current investigation (n = 3927). Those individuals with missing ceramide or clinical data were excluded (n = 69). Moreover, we excluded participants with any of the following: a self-reported diagnosis of diabetes mellitus (type 1 or type 2) at baseline (n = 442), fasting plasma glucose ≥7.0 mmol/l (n = 45) or non-fasting plasma glucose ≥11.1 mmol/l (n = 27). Using these criteria, a total of 3344 eligible individuals were included in the final analyses. Individuals with incident diabetes during the follow-up were identified from the Norwegian prescription database, hospital discharge diagnosis and WENBIT trial follow-up, as previously described in detail [13]. Because information on incident diabetes was collected through 31 December 2009, i.e. before the HbA1c criterion was implemented in the diagnosis of diabetes [14], the diagnosis of type 2 diabetes was based only on glucose levels. We performed additional analyses after excluding participants with HbA1c ≥ 47.5 mmol/mol (6.5%) at baseline (n = 2352). The median follow-up time for incident diabetes in the WECAC cohort was 7.6 years.
Prevent metabolic syndrome study
The Prevent Metabolic Syndrome (PrevMetSyn) trial is a population-based randomised study that consists of either overweight or obese individuals [15]. All procedures of the study comply with the Declaration of Helsinki (World Medical Association 2013). All study participants gave written informed consent, and the study was approved by the Ethics Committee of the Hospital District of Northern Ostrobothnia, Oulu, Finland (decision number 29/2012). The study is registered at ClinicalTrials.gov with the identifier NCT01959763.
The sample was collected using the address and information system of the Finnish Population Register Center. Invitation letters were sent to people aged 20–60 years living in the city of Oulu. Eligibility criteria were: (1) a BMI of 27–35 kg/m2; (2) access to the Internet; (3) no health-related restrictions for losing weight (such as pregnancy); and (4) no other ongoing treatment for obesity. Volunteers were invited to a screening visit at the enrolment site at the Oulu University Hospital. After the screening, the participants were randomised and started the lifestyle intervention; they attended follow-up visits after the first and second years of the intervention.
Blood samples were drawn during the screening and study visits at the research laboratory of the Oulu University Hospital. Blood pressure, waist circumference, height and weight were also measured. All the procedures have been described in detail and approved by the Ethics Committee of the Hospital District of Northern Ostrobothnia, Oulu, Finland. Samples from 375 participants were analysed, and four were excluded due to missing ceramide or clinical data, leaving 371 individuals for the analyses.
Analysis of ceramides
The analysis of ceramides from serum samples has previously been described in detail [8, 16]. In brief, ceramide quantification was performed using a validated high-throughput mass spectrometry approach [16]. Serum or plasma samples (10 μl) were spiked with 2H (deuterium [D])-labelled internal standards, D7-Cer(d18:1/16:0), D7-Cer(d18:1/18:0), D7-Cer(d18:1/24:0) and D7-Cer(d18:1/24:1), and extracted in isopropanol:ethyl acetate (8:2, vol./vol.) using a Hamilton MICROLAB STAR robot (Hamilton Robotics, Kista, Sweden). The levels of Cer(d18:1/16:0), Cer(d18:1/18:0), Cer(d18:1/24:0) and Cer(d18:1/24:1) were quantified on a QTRAP6500 (AB SCIEX, Concord, ON, Canada) mass spectrometer equipped with an Eksigent 100-XL ultra-HPLC system (AB SCIEX). The individual ceramides were quantified in multiple-reaction-monitoring mode. Quantification was assessed through calibration line samples comprising of known amounts of synthetic Cer(d18:1/16:0), Cer(d18:1/18:0), Cer(d18:1/24:0) and Cer(d18:1/24:1) and corresponding 2H-labelled standards. The peak area ratios of each ceramide to its corresponding 2H-labelled form were calculated, plotted against the added ceramide concentration and fitted by linear regression analysis. Final ceramide concentrations were presented in μmol/l.
Statistical methods
The baseline characteristics are described using medians (interquartile range) for continuous variables, and numbers (percentages) for categorical variables. Cox proportional hazard regression analyses were used to determine associations of the ceramide ratios with incident diabetes, after excluding individuals with prevalent diabetes. Full models were adjusted for the following risk factors: age, BMI, HDL-cholesterol (HDL-C), C-reactive protein (CRP), current smoking status, lipid-lowering treatment and systolic blood pressure (in FINRISK, 15 mmHg was added for participants on antihypertensive medication). In addition, WECAC was adjusted by sex, and FINRISK 2002 by waist circumference, eastern location in Finland, family history of diabetes (first-degree relatives), physical activity (binary variable for physical activity during free time) and socioeconomic status, defined as educational level (low, medium, high). Some models were additionally adjusted for glucose and HbA1c. In WECAC, the vitamin B intervention arms, alone or in combination with the investigated ceramide ratio, did not show an interaction with the development of diabetes in Cox regression models, but the intervention arms were used as a stratifying variable. In FINRISK 2002, the models were stratified by sex. All continuous covariates, including baseline age and ceramide level, were log e -transformed, and their effects are expressed per SD of the transformed variable. Individuals were excluded from the analyses if data relating to any of the variables was missing.
For prediction, Cox regression models were constructed based on FINRISK 2002 to predict the 10 year absolute risk of incident diabetes, using tenfold crossvalidation to prevent overoptimism. The increase in C-statistic resulting from the addition of the Cer(d18:1/18:0)/Cer(d18:1/16:0) ratio into the model was evaluated using the method of Antolini et al [17] for correlated C-statistics. Calibration of the models was estimated using the Hosmer–Lemeshow test. For validation, the regression coefficients from FINRISK 2002 were used to predict the 7 year risk in the WECAC study. In this validation, the baseline hazard was recalibrated in the WECAC study. The diabetes risk scores were derived directly from the models developed in FINRISK 2002.
In the PrevMetSyn study, the data were log2-transformed and paired t tests were performed to calculate the significance of changes at 1 or 2 years relative to baseline. Software package R version 3.4.3 [18] was used for all statistical analyses. A value of p < 0.05 was considered statistically significant, and all tests were two-sided.
Results
Stearic acid (18:0) ceramide shows the strongest association with incident diabetes
Four ceramides, Cer(d18:1/16:0), Cer(d18:1/18:0), Cer(d18:1/24:0) and Cer(d18:1/24:1), were analysed in the FINRISK 2002 population study (n = 8045; see electronic supplementary material [ESM] Table 1). In unadjusted Cox regression models, all ceramides and ceramide ratios were significantly associated with future type 2 diabetes, and several of these remained significant after adjusting for other diabetes-associated variables (ESM Table 2). However, in an analysis of the substudy with fasting glucose and HbA1c data available (ESM Table 3), adjusting additionally for these variables the highest significant HRs were observed for Cer(d18:1/18:0) and Cer(d18:1/18:0)/Cer(d18:1/24:0) (ESM Table 2).
Among the ceramides, Cer(d18:1/18:0)/Cer(d18:1/16:0) ratio is the best predictor of incident diabetes
As distinct ceramides have specific roles in different cardiometabolic disorders, ceramide ratios may appear to be better predictors than individual ceramide concentrations [7]. To this end, we investigated the ratios of Cer(d18:1/18:0) to the other ceramides, and observed that the most significant predictor in univariate and multivariable analyses was the Cer(d18:1/18:0)/Cer(d18:1/16:0) ratio (Table 1). The HR for this ceramide ratio was more significant than for several traditional risk markers including cholesterol measurements (total cholesterol, LDL-cholesterol and HDL-C), triacylglycerols (TGs), CRP and systolic blood pressure, while glucose and HbA1c were stronger predictors of incident type 2 diabetes, which is expected as they form the diagnostic definition of the disease (ESM Table 4).
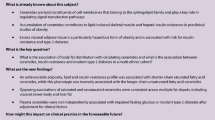
The Cer(d18:1/18:0)/Cer(d18:1/16:0) ratio was elevated in individuals with prevalent diabetes or with incident diabetes compared with individuals who remained free of type 2 diabetes during the follow-up (Fig. 1a). Furthermore, this ratio was elevated by lipid-lowering treatment (Fig. 1b). This ratio, followed by Cer(d18:1/18:0), was the ceramide variable that correlated most significantly with BMI, waist circumference, insulin, glucose and HbA1c (Fig. 1c). Of note, Cer(d18:1/16:0) was not statistically significantly associated to any of these variables. There was no difference in the ratio between men and women (p = 0.55).
Cer(d18:1/18:0)/Cer(d18:1/16:0) ratio in individuals (a) without type 2 diabetes (T2D), or with incident T2D or prevalent T2D, and (b) in individuals receiving and not receiving lipid-lowering treatment. The Wilcoxon rank-sum t test p values were <2.2 × 10−16 for the following two-group comparisons: incident T2D vs no T2D; prevalent T2D vs no T2D; and lipid treatment vs no lipid treatment. (c) Correlation (Spearman) of ceramides and Cer(d18:1/18:0)/Cer(d18:1/16:0) ratio to various variables. Waist, waist circumference
Validation of the diabetes-associated ceramide ratio in individuals with suspected stable angina pectoris
The predictive value of the Cer(d18:1/18:0)/Cer(d18:1/16:0) ratio was validated in the WECAC study (n = 3344; ESM Table 5). In WECAC as well, the Cer(d18:1/18:0)/Cer(d18:1/16:0) ratio showed the strongest association with incident type 2 diabetes (Table 2). The Cox regression results for other clinical measurements were similar to those for the FINRISK 2002 study, i.e. CRP was significant primarily in unadjusted models, HDL-C and TGs were the only significant measurements from the lipid panel, and glucose showed the highest univariate and multivariable HRs (ESM Table 6). In addition to excluding the participants with self-reported diabetes and high glucose levels, we also analysed the WECAC study after excluding all individuals with HbA1c ≥ 47.5 mmol/mol (6.5%) at baseline. The results remained consistent, although the HRs decreased for all the investigated variables (Table 2, ESM Table 6).
Prediction of incident diabetes and score
Cox regression models were constructed to predict the 10 year risk of incident diabetes in the FINRISK 2002 study and validated in the WECAC study for 7 year risk. For validation, regression coefficients from the FINRISK 2002 study were used, but due to the different nature and follow-up time of the study, baseline hazard was recalibrated for the WECAC study. In addition to age, sex and BMI, the variables selected for these models were those that showed significant HRs (ESM Table 4) and were available for all participants in the FINRISK 2002 study. Furthermore, in FINRISK 2002 we compared the results with risk factors currently used in diabetes risk scores. In all models, the addition of Cer(d18:1/18:0)/Cer(d18:1/16:0) statistically significantly increased the C-statistic in both the FINRISK 2002 and WECAC studies (Table 3). Most of the models also showed adequate calibration in both studies. In the WECAC study with an HbA1c cut-off, the C-statistic also showed an increase but were not statistically significant (ESM Table 7). The highest C-statistics were obtained when the ceramide ratio was added on top of age, BMI, sex and TGs (C-statistic 0.824 in FINRISK 2002 and 0.736 in WECAC) or traditional risk factors (C-statistic 0.828 in FINRISK) (Table 3). These two models had equally good predictive value in FINRISK 2002 (p = 0.40 for the difference in C-statistics).
Two diabetes scores (dScores) were constructed for Cer(d18:1/18:0)/Cer(d18:1/16:0) that could be used to predict the onset of diabetes, using also BMI and age with or without TG. For scoring, the regression models developed in the FINRISK 2002 for the 10 year risk were used, and individuals were divided into three groups based on the predicted risk. For both scores in FINRISK 2002, approximately 60% of the population had a low risk of 1.5% for developing incident diabetes in 10 years, whereas for the individuals in the high risk group the risk was on average 25%, i.e. 17-fold the low-risk group (Table 4). The scores were validated in the WECAC cohort, where roughly half of the population belonged to the low-risk group (2.4% and 1.7% developed incident diabetes, for dScore1 and dScore2, respectively), while the highest risk individuals had an average 17% risk of developing incident diabetes (Table 4).
Weight loss reduces the ceramide ratio
The effect of nutritional intervention and resulting weight loss on the ceramide ratio was investigated in the PrevMetSyn dietary intervention study (n = 371; ESM Table 8). The ceramide ratio was significantly reduced in individuals with weight loss of 5% or more, and the result was more significant after 2 years (Fig. 2, ESM Fig. 1) than 1 year. Glucose showed a similar trend, whereas for insulin the changes between participants with either weight loss or weight gain were stronger. Interestingly, HbA1c and CRP did not show trends according to change in weight. The diabetes scores were significantly reduced in individuals with a weight loss of 2% or more.
Change in ceramide ratio and other variables in individuals with different weight changes, resulting from dietary intervention, after (a) 1 or (b) 2 years. The bars represent the mean relative change (%) between time points. Black bars, weight loss >5%; white bars, weight loss 2–5%; light grey bars, weight loss 0–2%; dark grey bars, weight gain 0–2%; horizontally hatched bars, weight gain >2%. *p < 0.05, **p < 0.01, ***p < 0.001. Individual data points are shown in ESM Fig. 1. The calculations for dScores are presented in Table 4
Discussion
In this study, it has been shown for the first time that the Cer(d18:1/18:0)/Cer(d18:1/16:0) ratio is an independent marker for risk of incident diabetes. Moreover, this ratio was decreased in individuals with a weight loss of 5% or more, which is in line with dietary intervention studies showing that even a weight loss of a few kilograms is sufficient to lower the risk of developing diabetes [19]. New diabetes scores have been proposed to improve the prediction of incident diabetes.
These d18:1 ceramides have been extensively investigated in plasma, skeletal muscle, liver and adipose tissue in human and animal studies, but this is the first study to show that the Cer(d18:1/18:0)/Cer(d18:1/16:0) ratio stands out as a superior ceramide biomarker for the onset of incident diabetes. This raises the question of why this ratio in particular offers the best predictive ability. One answer comes from our analyses showing that among the ceramides Cer(d18:1/18:0) was the most, and Cer(d18:1/16:0) the least, significantly correlated ceramide with BMI, fasting glucose, insulin and HbA1c, which are all important factors predisposing an individual to the onset of diabetes. Thus, the very different associations of these two ceramides with the development of insulin resistance may explain the predictive power of this ratio. However, Cer(d18:1/18:0)/Cer(d18:1/16:0) also predicts incident diabetes independently of glucose and HbA1c.
The important role of Cer(d18:1/18:0) in the development of insulin resistance has been demonstrated in several studies. In the Australian Diabetes, Obesity and Lifestyle Study (AusDiab), both plasma Cer(d18:1/18:0) and its precursor Cer(d18:0/18:0) showed strong associations with type 2 diabetes and prediabetes [20]. It has been documented in another human study that insulin sensitivity inversely correlates especially with plasma Cer(d18:1/18:0) [21], and this was also the most upregulated ceramide in plasma in genetically obese (ob/ob) mice [22].
Insulin resistance in skeletal muscle plays a major role in the development of type 2 diabetes [23], and there are mixed results for the Cer(d18:1/18:0) and Cer(d18:1/16:0) ceramides in the literature, although most studies support the importance of Cer(d18:1/18:0) in the development of insulin resistance in muscle. In a study investigating insulin resistance in humans, it was shown that, in muscle, Cer(d18:1/18:0) was the only lipid elevated by insulin resistance independently of obesity, and in plasma, Cer(d18:1/18:0), together with its precursor Cer(d18:0/18:0), was associated with both insulin resistance and obesity [24]. The same study also demonstrated that there was a positive correlation between plasma and muscle concentrations of Cer(d18:1/18:0), and this lipid correlated positively with visceral and liver fat and inversely with metabolic flexibility, which was determined by the change in respiratory quotient at rest and after insulin stimulation [24]. Another study supports these findings by showing that the concentration of Cer(d18:1/18:0) was significantly higher in type 2 diabetic individuals than athletes, and it was positively associated with BMI and inversely associated with insulin sensitivity [25]. However, there is a study demonstrating that Cer(d18:1/16:0) is more strongly increased than Cer(d18:1/18:0) in the muscle of obese individuals [26].
The results in adipose tissue are more controversial than those observed in muscle. Elevated expression of ceramide synthase 6, responsible for the synthesis of Cer(d18:1/16:0), has been demonstrated in adipose tissue in obese humans, together with increased concentrations of Cer(d18:1/16:0) and Cer(d18:1/18:0) [27]. CerS6-deficient mice, and also models with specific knockout in brown adipose tissue and liver, are protected from diet-induced obesity and glucose intolerance [27]. However, contradictory results were obtained in another study showing that obesity leads to the degradation of ceramides in the adipose tissue of obese (ob/ob) mice [22]. The accumulation of ceramides in adipose tissue in obesity was again supported by a mouse study which showed that both Cer(d18:1/16:0) and Cer(d18:1/18:0) were already elevated in adipose tissue after 1 week on a high-fat diet [28]. In this study, it was also reported that the high-fat diet induced in particular an elevation of Cer(d18:1/18:0) in muscle, and in liver Cer(d18:1/18:0) was elevated after 16 weeks, but not as much as Cer(d18:1/20:0) or Cer(d18:1/22:0) [28].
Taken together, these studies suggest that the observed increase of especially Cer(d18:1/18:0) in obese and insulin-resistant individuals is a result of the regulation and synthesis of ceramides in several different organs. Numerous studies have investigated the mechanisms by which ceramides affect insulin sensitivity, and there are several pathways that induce ceramide synthesis, such as saturated fatty acids and activation of inflammatory pathways triggered by Toll-like receptor 4 (TLR4) recognition of the saturated fatty acids [4]. Furthermore, the insulin sensitiser adiponectin and endoplasmic reticulum stress modulate ceramide metabolism [4]. The accumulated ceramides then inhibit insulin signalling by decreasing the activity of Akt (also known as protein kinase B) via protein phosphatase 2A or atypical protein kinase C [5]. However, further studies are needed to understand why stearic acid-containing ceramides in particular are strongly associated with the development of obesity and insulin resistance.
The strength of our study was that the results were derived from a large population-based study and validated in another large cohort of individuals with suspected stable angina pectoris, and both studies had long follow-up times. Despite the apparent differences between these studies, the results were consistent, which supports the robustness of our observations. Another strength was that, using the ceramide ratio and other laboratory measurements, we were able to obtain a better prediction than with the traditional risk factors, such as BMI, physical activity and family history of diabetes. However, a limitation of our study was that we did not have available all the risk factors of the current diabetes risk calculators, such as history of blood glucose levels, gestational diabetes and blood pressure medication, or nutritional data, and therefore we could not compare the developed models explicitly with current risk calculators. However, it is noteworthy that the ceramide ratio also improved the model consisting of several established risk factors, including BMI, waist circumference, family history, blood pressure and physical activity. Another limitation was the slight difference in the follow-up times of the two cohorts, and that the study participants were not fasting, which may especially affect TG levels.
It has recently been suggested that the investigated ceramides should be adopted into clinical practice for cardiovascular risk prediction [29], and it is therefore a tempting idea that the same molecules, although in a different ratio, could also be used to predict risk of diabetes. An interesting topic for further investigation is whether these ceramides could predict the cardiovascular complications of diabetes. Another interesting area for study is the predictive value of the Cer(d18:1/18:0)/Cer(d18:1/16:0) ratio for gestational diabetes, and, as the ceramide ratio was elevated in individuals on statin treatment, to explore whether this ratio could serve as a biomarker for statin-induced diabetes.
Data availability
The FINRISK study will consider any reasonable application for scientific collaboration submitted through the National Institute for Health and Welfare biobank. Other datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CRP:
-
C-reactive protein
- dScore:
-
Diabetes score
- HDL-C:
-
HDL-cholesterol
- PrevMetSyn:
-
Prevent Metabolic Syndrome (trial)
- TG:
-
Triacylglycerol
- WECAC:
-
Western Norway Coronary Angiography Cohort
References
World Health Organization (2016) Global report on diabetes. World Health Organization, Geneva
Forbes JM, Cooper ME (2013) Mechanisms of diabetic complications. Physiol Rev 93:137–188
Bansal N (2015) Prediabetes diagnosis and treatment: a review. World J Diabetes 6:296–303
Chavez JA, Summers SA (2012) A ceramide-centric view of insulin resistance. Cell Metab 15:585–594
Markgraf DF, Al-Hasani H, Lehr S (2016) Lipidomics–reshaping the analysis and perception of type 2 diabetes. Int J Mol Sci 17:E1841
Wigger L, Cruciani-Guglielmacci C, Nicolas A et al (2017) Plasma dihydroceramides are diabetes susceptibility biomarker candidates in mice and humans. Cell Rep 18:2269–2279
Laaksonen R, Ekroos K, Sysi-Aho M et al (2016) Plasma ceramides predict cardiovascular death in patients with stable coronary artery disease and acute coronary syndromes beyond LDL-cholesterol. Eur Heart J 37:1967–1976
Havulinna AS, Sysi-Aho M, Hilvo M et al (2016) Circulating ceramides predict cardiovascular outcomes in the population-based FINRISK 2002 cohort. Arterioscler Thromb Vasc Biol 36:2424–2430
Borodulin K, Vartiainen E, Peltonen M et al (2015) Forty-year trends in cardiovascular risk factors in Finland. Eur J Pub Health 25:539–546
Salomaa V, Havulinna A, Saarela O et al (2010) Thirty-one novel biomarkers as predictors for clinically incident diabetes. PLoS One 5:e10100
Tveitevag Svingen GF, Ueland PM, Pedersen EKR et al (2013) Plasma dimethylglycine and risk of incident acute myocardial infarction in patients with stable angina pectoris. Arterioscler Thromb Vasc Biol 33:2041–2048
Ebbing M, Bleie Ø, Ueland PM et al (2008) Mortality and cardiovascular events in patients treated with homocysteine-lowering B vitamins after coronary angiography. JAMA 300:795–804
Rebnord EW, Strand E, Midttun Ø et al (2017) The kynurenine:tryptophan ratio as a predictor of incident type 2 diabetes mellitus in individuals with coronary artery disease. Diabetologia 60:1712–1721
World Health Organization (2011) Use of glycated haemoglobin (HbA1c) in the diagnosis of diabetes mellitus. www.who.int/diabetes/publications/report-hba1c_2011.pdf. Accessed 20 October 2017
Karppinen P, Oinas-Kukkonen H, Alahäivälä T et al (2016) Persuasive user experiences of a health behavior change support system: a 12-month study for prevention of metabolic syndrome. Int J Med Inform 96:51–61
Kauhanen D, Sysi-Aho M, Koistinen KM, Laaksonen R, Sinisalo J, Ekroos K (2016) Development and validation of a high-throughput LC-MS/MS assay for routine measurement of molecular ceramides. Anal Bioanal Chem 408:3475–3483
Antolini L, Nam B-H, D’Agostino RB (2004) Inference on correlated discrimination measures in survival analysis: a nonparametric approach. Commun Stat Theory Methods 33:2117–2135
Core Team R (2017) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna
Lindström J, Louheranta A, Mannelin M et al (2003) The Finnish diabetes prevention study (DPS): lifestyle intervention and 3-year results on diet and physical activity. Diabetes Care 26:3230–3236
Meikle PJ, Wong G, Barlow CK et al (2013) Plasma lipid profiling shows similar associations with prediabetes and type 2 diabetes. PLoS One 8:e74341
Haus JM, Kashyap SR, Kasumov T et al (2009) Plasma ceramides are elevated in obese subjects with type 2 diabetes and correlate with the severity of insulin resistance. Diabetes 58:337–343
Samad F, Hester KD, Yang G, Hannun YA, Bielawski J (2006) Altered adipose and plasma sphingolipid metabolism in obesity: a potential mechanism for cardiovascular and metabolic risk. Diabetes 55:2579–2587
DeFronzo RA, Tripathy D (2009) Skeletal muscle insulin resistance is the primary defect in type 2 diabetes. Diabetes Care 32(Suppl 2):S157–S163
Tonks KT, Coster AC, Christopher MJ et al (2016) Skeletal muscle and plasma lipidomic signatures of insulin resistance and overweight/obesity in humans. Obesity (Silver Spring) 24:908–916
Bergman BC, Brozinick JT, Strauss A et al (2016) Muscle sphingolipids during rest and exercise: a C18:0 signature for insulin resistance in humans. Diabetologia 59:785–798
Adams JM, Pratipanawatr T, Berria R et al (2004) Ceramide content is increased in skeletal muscle from obese insulin-resistant humans. Diabetes 53:25–31
Turpin SM, Nicholls HT, Willmes DM et al (2014) Obesity-induced CerS6-dependent C16:0 ceramide production promotes weight gain and glucose intolerance. Cell Metab 20:678–686
Turner N, Kowalski GM, Leslie SJ et al (2013) Distinct patterns of tissue-specific lipid accumulation during the induction of insulin resistance in mice by high-fat feeding. Diabetologia 56:1638–1648
Nicholls M (2017) Plasma ceramides and cardiac risk. Eur Heart J 38:1359–1360
D’Agostino RB, Vasan RS, Pencina MJ et al (2008) General cardiovascular risk profile for use in primary care: the Framingham heart study. Circulation 117:743–753
Contribution statement
RL, VS and ON were responsible for the conception and design of the whole study. The conception, design and data acquisition of the studies were carried out by VS, ASH, TL and PJ (FINRISK 2002); ON, ERP, GST and KM (WECAC); and MJS, TS and A-MT (PrevMetSyn). DK undertook the design of the laboratory analyses and acquisition of the ceramide data. MH was responsible for statistical analyses, data interpretation and drafting of the first version of the manuscript. All authors have revised the manuscript critically for important intellectual content and accepted the manuscript version to be published. MH and RL are responsible for the integrity of the work as a whole.
Funding
VS was supported by the Finnish Foundation for Cardiovascular Research. The PrevMetSyn study was supported by grants from the Ministry of Social Affairs and Health (decisions 083/THL/TE/2012 and 201310185), Finland, the Academy of Finland (decision 1114784), the Juho Vainio Foundation, the Sigrid Jusélius Foundation, the Diabetes Research Foundation, the Finnish Foundation for Cardiovascular Research and the City of Oulu, Finland.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Zora Biosciences Oy holds patents for the diagnostic use of ceramides for cardiovascular risk determination. MH and DK are employees, and RL is an employee and shareholder, of Zora Biosciences Oy. VS participated in a congress trip sponsored by Novo Nordisk.
Electronic supplementary material
ESM
(PDF 506 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Hilvo, M., Salonurmi, T., Havulinna, A.S. et al. Ceramide stearic to palmitic acid ratio predicts incident diabetes. Diabetologia 61, 1424–1434 (2018). https://doi.org/10.1007/s00125-018-4590-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-018-4590-6