Abstract
Aims/hypothesis
Soluble CD163 (sCD163) was recently identified as a strong risk marker for developing type 2 diabetes. We hypothesised that sCD163 independently associates with insulin resistance.
Methods
This cross-sectional study includes 234 participants: 96 with type 2 diabetes, 34 with impaired glucose tolerance (IGT) and 104 with normal glucose tolerance (NGT), matched for sex and BMI. Glucose-lowering medication was paused for 1 week before plasma samples were obtained for determination of sCD163 and other inflammatory and metabolic variables. Insulin resistance was estimated by homeostasis model assessment of insulin resistance (HOMA-IR).
Results
Concentrations of sCD163 were 1.95 mg/l (0.63–6.97) in individuals with type 2 diabetes, 1.64 mg/l (0.58–4.19) in those with IGT, and 1.48 mg/l (0.48–4.11) (median [range]) in those with NGT (p < 0.0001). In univariate analyses, sCD163 correlated significantly with HOMA-IR (R = 0.44), insulin (R = 0.41), glucose (R = 0.30), triacylglycerol (R = 0.29) and HDL-cholesterol (R = −0.34) (all p < 0.0001). All but glucose remained significant when adjusting for age, sex, BMI and glycaemic group. In univariate regression analyses, HOMA-IR was associated with sCD163, C-reactive protein (CRP), TNF-α and IL-6 (all p ≤ 0.0001). An increase of 50% in sCD163 resulted in an estimated increase in HOMA-IR of 36% (95% CI 26, 48; p < 0.0001). In multiple linear regression analyses, sCD163 (p = 0.001) and CRP (p = 0.01) remained independent predictors of HOMA-IR, whereas TNF-α and IL-6 did not.
Conclusions/interpretation
Macrophage-specific sCD163 was strongly associated with insulin resistance independently of TNF-α and other predictors. Moreover, sCD163 was associated with well-known variables of the metabolic syndrome.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic systemic inflammation plays an important role in the development of obesity-related insulin resistance. Insulin resistance is associated with increased concentrations of inflammatory markers such as C-reactive protein (CRP) [1]; and it has been established that adipose tissue, rather than just functioning as a storage depot for excess lipid energy, is an active endocrine organ that releases a number of hormones and adipokines [2]. Furthermore, recent studies have shown that adipose tissue in obese individuals is inflamed and infiltrated by macrophages that secrete proinflammatory cytokines such as TNF-α and IL-6 [3]. These cytokines promote insulin resistance and are thought to be directly involved in the development of obesity-related disease [4–6].
TNF-α is expressed as a membrane-bound protein in the macrophages and other immune cells [7]. TNF-α is cleaved into a soluble form and released from the cell surface by proteolytic action of the metalloproteinase TNF-α-converting enzyme (TACE/ADAM17) [8]. Recently it has been shown that TACE is also responsible for the shedding of macrophage-specific soluble CD163 (sCD163) [9]. Plasma sCD163 is regarded as a longer duration circulating marker of TNF-α, and concentrations of sCD163 are increased in obese [10, 11] and type 2 diabetic patients [12], consistent with macrophage accumulation in the adipose tissue. Zanni et al., in a study which was published while this manuscript was under review, reported a strong association between sCD163 and insulin resistance in obese individuals and normal-weight controls [11]. Furthermore, we have recently shown that baseline increased sCD163 is a strong risk factor for developing type 2 diabetes during the subsequent 18 years in the general population [13].
The primary objective of the present study was to evaluate the association between sCD163 and insulin resistance in well-defined groups of individuals with type 2 diabetes, impaired glucose tolerance (IGT) and normal glucose tolerance (NGT). A secondary objective was to compare sCD163 as an independent predictor of insulin resistance with TNF-α, CRP and IL-6.
Methods
The local Ethics Committee of Copenhagen and Frederiksberg approved the study (01-141/04), and informed consent was obtained from all participants.
Subjects
The original study had a cross-sectional, case–control design and included patients with type 2 diabetes and healthy individuals matched for age, sex and BMI [14]. Participants were recruited by advertising in a local newspaper in the communities of Copenhagen and Frederiksberg, Denmark, and information on the diagnosis of type 2 diabetes was based on oral information from each participant. A standard OGTT was performed and WHO diagnostic criteria were used to verify participants’ glycaemic status [15]. The present study also included individuals with IGT. In all, 234 participants were included: 96 with type 2 diabetes, 34 with IGT and 104 with NGT. Baseline characteristics are shown in Table 1.
Exclusion criteria were recent or ongoing infection, immune inflammatory disease, history of malignant disease, or treatment with anti-inflammatory drugs or insulin.
Study design
All participants’ medication was paused for 24 h prior to the examination day, and in patients with type 2 diabetes oral glucose-lowering medication was paused for 1 week. After an overnight fast, participants arrived at the laboratory between 08:00 and 10:00 hours. Blood samples were drawn from an antecubital vein to measure sCD163 and other markers of inflammation (CRP, TNF-α, IL-6) and metabolic variables (HbA1c, glucose, insulin, triacylglycerol, total cholesterol, and HDL- and LDL-cholesterol). An OGTT was conducted as previously described [14].
Laboratory assessments
Plasma levels of HbA1c, glucose, insulin, triacylglycerol and total, HDL- and LDL-cholesterol were measured using standard clinical biochemical methods. Plasma CRP was measured using Tinaquant CRPLX (Roche Diagnostics, Mannheim, Germany). Plasma concentrations of TNF-α and IL-6 were measured by ELISA (R&D Systems, Minneapolis, MN, USA).
We determined serum concentrations of sCD163 in duplicate samples that had been frozen for up to 7 years at −20 °C by use of an in-house sandwich ELISA on a BEP-2000 ELISA analyser (Dade Behring, Marburg, Germany) [16]. In each run, we co-analysed control samples and serum calibrator with concentrations traceable to purified CD163. The inter-assay imprecision in the current study (seven runs) was 6.6% CV at concentrations of 1.52 mg/l, and 8.6% CV at 3.76 mg/l. The limit of detection was 6.25 μg/l. Soluble CD163 is robust to thawing, and stability has been rigorously verified for at least 7 months at −20°C [16]. Postprandial levels of sCD163 (4 h after a meal) did not differ significantly from fasting levels in healthy individuals (data not shown).
Insulin resistance
Insulin resistance was estimated from fasting plasma insulin and glucose concentrations using HOMA of insulin resistance (HOMA-IR) [17]. The HOMA model, version 2, from 1996, was used [18].
Statistical analyses
Baseline glycaemic group comparisons were made using the one-way ANOVA test (normally distributed data), Kruskal–Wallis test (non-normal data) or χ2 test (for sex; Table 1).
The relationship between the different metabolic variables and sCD163 was investigated using simple linear regression and multiple linear regression on a log–log scale where appropriate. Two multivariate models were considered: model 1, which included sex and glycaemic group; and model 2, which also included age and BMI (Table 2). In order to determine whether the association between the metabolic variables and sCD163 differed between sexes and glycaemic groups, we included interaction terms between sCD163, sex and glycaemic group. The appropriateness of the multiple linear models to describe the data was established by inspecting plots of the standardised residuals against the fitted values and the different covariates.
The relationship between HOMA-IR and the different inflammatory markers was also investigated using simple linear regression and multiple linear regression. Two multivariate models were considered: model 3, which included all four inflammatory markers as explanatory variables; and model 4, which also included sex, glycaemic group, age, BMI and concentrations of triacylglycerol and HDL-cholesterol (Table 3). Model validation was performed as for the metabolic variables.
We compared the value of CRP and sCD163 in predicting HOMA-IR by testing the hypothesis of equal width of the prediction intervals for HOMA-IR based on CRP and sCD163, respectively. This was done using Pitman's test and was repeated in the analysis, where adjustment for sex, glycaemic group, age, BMI and concentrations of triacylglycerol and HDL-cholesterol was made.
Results
The baseline characteristics of the study participants are shown in Table 1.
Plasma sCD163 is increased in IGT and type 2 diabetes
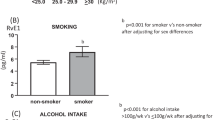
Concentrations of sCD163 were 1.95 mg/l (0.63–6.97) in individuals with type 2 diabetes, 1.64 mg/l (0.58–4.19) in those with IGT, and 1.48 mg/l (0.48–4.11; median [range]) in those with NGT (p < 0.0001; Table 1). Concentrations of sCD163 were comparable in men and women in the entire study population (1.72 mg/l [0.48–6.97] vs. 1.59 mg/l [0.58–5.84]; p = 0.545) and in the different glycaemic groups (all, p > 0.47).
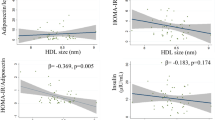
Plasma sCD163 is related to HOMA-IR and other metabolic measures
In univariate linear regression analyses, plasma sCD163 was a significant predictor of HOMA-IR, glucose, insulin, triacylglycerol and HDL-cholesterol (inversely) (all, p < 0.0001), but not of total cholesterol, LDL-cholesterol and HbA1c (Table 2). The association between sCD163 and HOMA-IR did not depend significantly on glycaemic group (p = 0.91).
In multivariate linear regression analysis adjusted for sex and glycaemic group (IGT and type 2 diabetes) (model 1), as well as for age and BMI (model 2), sCD163 was still a significant predictor of HOMA-IR, insulin, triacylglycerol and HDL-cholesterol (inversely; all, p ≤ 0.0017), but not glucose (Table 2). Whereas BMI was determined in all participants, other anthropometric measures such as waist circumference and total fat mass (dual-energy x-ray absorptiometry scans) were determined in most but not all participants. The correlations between sCD163 and the different measures of obesity were quite similar (R = 0.23–0.26; all p ≤ 0.0006). In glycaemic subgroup analyses, the correlations were also comparable, although only for BMI were all correlations statistically significant in all subgroups.
An increase of 50% in sCD163 resulted in an estimated increase in HOMA-IR of 36% (95% CI 26, 48) in the unadjusted model, 28% (95% CI 18, 39) in multivariate model 1 and 19% (95% CI 10, 28) in model 2 (all models, p < 0.0001; Fig. 1).
The relationship between an increase in sCD163 (%) and the corresponding increase in HOMA-IR (%). a Univariate analysis. b Multivariate analyses, model 1; adjusted for sex and glycaemic group. c Multivariate analyses, model 2; adjusted for sex, glycaemic group, age and BMI. Shaded areas correspond to 95% CI
Plasma sCD163 is related to other inflammatory markers
In univariate linear regression analyses, sCD163 was associated with CRP (R = 0.24, p = 0.0002), TNF-α (R = 0.35, p < 0.0001) and IL-6 (R = 0.25, p < 0.0001).
Plasma sCD163 is related to HOMA-IR independently of other inflammatory markers
In univariate linear regression analyses, sCD163, CRP, TNF-α and IL-6 were associated with HOMA-IR (all, p ≤ 0.0001; Table 3).
In multiple linear regression analyses, including all inflammatory markers (model 3) and adjusted for sex, glycaemic group, age, BMI and concentrations of triacylglycerol and HDL-cholesterol (model 4), only sCD163 (p = 0.001) and CRP (p = 0.01) remained significant predictors of HOMA-IR (Table 3).
There was no evidence against the hypothesis of equal value of CRP and sCD163 in predicting HOMA-IR (p = 0.42). This conclusion was not altered when adjusting for sex, glycaemic group, age, BMI and concentrations of triacylglycerol and HDL-cholesterol (p = 0.63).
Discussion
Obesity-associated insulin resistance is central to the development of type 2 diabetes, but it is not easy to estimate insulin resistance in routine clinical practice. Reliable biomarkers for insulin resistance that can be measured in non-fasting blood samples may therefore prove to be of significant clinical value for early identification of at-risk individuals. Early identification is important, since a substantial part of patients with type 2 diabetes already have diabetic complications at the time of diagnosis [19, 20]. We have previously shown that high levels of sCD163 in the general population carry a large increased risk of later development of type 2 diabetes [13], but whether this is linked to insulin resistance is not known.
In the present study, we have shown for the first time that sCD163 is a strong and independent predictor of insulin resistance (HOMA-IR) in sex- and BMI-matched (mainly overweight/obese) individuals with type 2 diabetes, IGT or NGT. In the unadjusted model, a change of 50% in sCD163 resulted in an estimated change in HOMA-IR of 36%. Importantly, the day-to-day intra-individual biological variation of sCD163 in healthy people is only 9% [21], and a 50% change in sCD163 will therefore be clinically easy to identify.
Normal human adipose tissue is infiltrated with macrophages that increase in number and activation state during obesity [22]. Different phenotypes have been described that do not fit simple categories of pro- or anti-inflammatory macrophages, but are characterised by excretion of inflammatory cytokines such as TNF-α and IL-6 [3, 23, 24]. These cytokines induce insulin resistance in the liver, which in turn stimulates the production of CRP [25]. In this study, sCD163 was a strong independent predictor of HOMA-IR, whereas TNF-α and IL-6 were not. This is interesting, since sCD163 and TNF-α share similar mechanisms of shedding by TACE from activated macrophages [9]. However, sCD163 may predict insulin resistance better due to the almost complete monocyte-macrophage specificity of CD163 and the longer plasma half-life of sCD163 (t ½ = approximately 1 day) [9], which makes it a more robust biomarker than TNF-α (t ½ = 18 min) [26].
Both increased number of macrophages and increased expression of CD163 in adipose tissue macrophages may contribute to the serum levels. CD163 mRNA levels are increased in the adipose tissue of obese individuals [27], although a clear association between mRNA levels and sCD163 has not been described. Furthermore, the source of sCD163 may also include other tissue macrophages and blood monocytes known to have increased CD163 expression in diabetes [28].
Concentrations of sCD163 increased significantly with deteriorating glycaemic status. Furthermore, sCD163 was significantly and independently associated with triacylglycerol and HDL-cholesterol (inversely), which are components included in the definition of the metabolic syndrome [29]. This strong association with the metabolic syndrome was also confirmed in our findings from the general population [13].
In addition to sCD163, CRP was an independent predictor of HOMA-IR. This emphasises that a model employing both sCD163 and CRP in combination with known factors, e.g. BMI or waist:hip ratio, may be superior in predicting insulin resistance [30]. It is possible that CRP to a higher degree reflects vascular inflammation, whereas sCD163 predominantly reflects obesity-related inflammation [31].
The study has some limitations due to the nature of its design. The participants were mainly overweight/obese, and the results may not be applicable to the small subgroup of leaner individuals who develop type 2 diabetes. We used HOMA-IR as a proxy of insulin resistance. Since the gold standard technique—the hyperinsulinaemic–euglycaemic clamp—is a laborious and time-consuming procedure, HOMA-IR has been widely used and acknowledged in large-scale studies as an estimate of insulin resistance. Furthermore, due to the cross-sectional design we cannot make any conclusions regarding cause-and-effect relationships. Such implications would require a design which in a more direct way tests the effect of altering one factor (e.g. insulin sensitivity) on the other factor (CD163). Moreover, we cannot conclude whether a time-dependent relationship between changes in sCD163 and changes in insulin resistance exists. Medications other than oral glucose-lowering agents were only paused for 24 h, and carry-over effects that influence the results may exist. Finally, the age-matching was not perfect, since those with IGT and type 2 diabetes were 6 years older than those with NGT. Age, however, was included in the multiple linear regression analysis and did not prove to be a significant confounder in the study.
In conclusion, macrophage-specific sCD163 is strongly and independently associated with HOMA-IR and other relevant metabolic variables of the metabolic syndrome. Plasma sCD163 seems to be a better predictor of insulin resistance than TNF-α and IL-6. Plasma sCD163 should be further evaluated as a simple and reliable measure of insulin resistance.
Abbreviations
- CRP:
-
C-reactive protein
- HOMA-IR:
-
HOMA of insulin resistance
- IGT:
-
Impaired glucose tolerance
- NGT:
-
Normal glucose tolerance
- sCD163:
-
Soluble CD163
- TACE:
-
TNF-α-converting enzyme
References
Chen J, Wildman RP, Hamm LL et al (2004) Association between inflammation and insulin resistance in U.S. nondiabetic adults: results from the Third National Health and Nutrition Examination Survey. Diabetes Care 27:2960–2965
Kershaw EE, Flier JS (2004) Adipose tissue as an endocrine organ. J Clin Endocrinol Metab 89:2548–2556
Zeyda M, Stulnig TM (2007) Adipose tissue macrophages. Immunol Lett 112:61–67
Plomgaard P, Bouzakri K, Krogh-Madsen R, Mittendorfer B, Zierath JR, Pedersen BK (2005) Tumor necrosis factor-alpha induces skeletal muscle insulin resistance in healthy human subjects via inhibition of Akt substrate 160 phosphorylation. Diabetes 54:2939–2945
Rieusset J, Bouzakri K, Chevillotte E et al (2004) Suppressor of cytokine signaling 3 expression and insulin resistance in skeletal muscle of obese and type 2 diabetic patients. Diabetes 53:2232–2241
Popa C, Netea MG, van Riel PL, van der Meer JW, Stalenhoef AF (2007) The role of TNF-alpha in chronic inflammatory conditions, intermediary metabolism, and cardiovascular risk. J Lipid Res 48:751–762
Camussi G, Albano E, Tetta C, Bussolino F (1991) The molecular action of tumor necrosis factor-alpha. Eur J Biochem 202:3–14
Black RA, Rauch CT, Kozlosky CJ et al (1997) A metalloproteinase disintegrin that releases tumour-necrosis factor-alpha from cells. Nature 385:729–733
Etzerodt A, Maniecki MB, Moller K, Moller HJ, Moestrup SK (2010) Tumor necrosis factor alpha-converting enzyme (TACE/ADAM17) mediates ectodomain shedding of the scavenger receptor CD163. J Leukoc Biol 88:1201–1205
Axelsson J, Moller HJ, Witasp A et al (2006) Changes in fat mass correlate with changes in soluble sCD163, a marker of mature macrophages, in patients with CKD. Am J Kidney Dis 48:916–925
Zanni MV, Burdo TH, Makimura H, Williams KC, Grinspoon SK (2011) Relationship between monocyte/macrophage activation marker soluble CD163 and insulin resistance in obese and normal-weight subjects. Clin Endocrinol (Oxf). doi:10.1111/j.1365-2265.2011.04284.x
Levy AP, Purushothaman KR, Levy NS et al (2007) Downregulation of the hemoglobin scavenger receptor in individuals with diabetes and the Hp 2–2 genotype: implications for the response to intraplaque hemorrhage and plaque vulnerability. Circ Res 101:106–110
Moller HJ, Frikke-Schmidt R, Moestrup SK, Nordestgaard BG, Tybjaerg-Hansen A (2011) Serum soluble CD163 predicts risk of type 2 diabetes in the general population. Clin Chem 57:291–297
Krabbe KS, Nielsen AR, Krogh-Madsen R et al (2007) Brain-derived neurotrophic factor (BDNF) and type 2 diabetes. Diabetologia 50:431–438
Alberti KG, Zimmet PZ (1998) Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med 15:539–553
Moller HJ, Hald K, Moestrup SK (2002) Characterization of an enzyme-linked immunosorbent assay for soluble CD163. Scand J Clin Lab Invest 62:293–299
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
Levy JC, Matthews DR, Hermans MP (1998) Correct homeostasis model assessment (HOMA) evaluation uses the computer program. Diabetes Care 21:2191–2192
UK Prospective Diabetes Study (UKPDS) Group (1998) Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 352:837–853
Ginsberg HN, Zhang YL, Hernandez-Ono A (2006) Metabolic syndrome: focus on dyslipidemia. Obesity (Silver Spring) 14(Suppl 1):41S–49S
Moller HJ, Petersen PH, Rejnmark L, Moestrup SK (2003) Biological variation of soluble CD163. Scand J Clin Lab Invest 63:15–21
Morris DL, Singer K, Lumeng CN (2011) Adipose tissue macrophages: phenotypic plasticity and diversity in lean and obese states. Curr Opin Clin Nutr Metab Care 14:341–346
Bourlier V, Zakaroff-Girard A, Miranville A et al (2008) Remodeling phenotype of human subcutaneous adipose tissue macrophages. Circulation 117:806–815
Zeyda M, Farmer D, Todoric J et al (2007) Human adipose tissue macrophages are of an anti-inflammatory phenotype but capable of excessive pro-inflammatory mediator production. Int J Obes (Lond) 31:1420–1428
Meshkani R, Adeli K (2009) Hepatic insulin resistance, metabolic syndrome and cardiovascular disease. Clin Biochem 42:1331–1346
Oliver JC, Bland LA, Oettinger CW et al (1993) Cytokine kinetics in an in vitro whole blood model following an endotoxin challenge. Lymphokine Cytokine Res 12:115–120
Shakeri-Manesch S, Zeyda M, Huber J, Ludvik B, Prager G, Stulnig TM (2009) Diminished upregulation of visceral adipose heme oxygenase-1 correlates with waist-to-hip ratio and insulin resistance. Int J Obes (Lond) 33:1257–1264
Sporrer D, Weber M, Wanninger J et al (2009) Adiponectin downregulates CD163 whose cellular and soluble forms are elevated in obesity. Eur J Clin Invest 39:671–679
Alberti KG, Eckel RH, Grundy SM et al (2009) Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 120:1640–1645
Goldfine AB, Gerwien RW, Kolberg JA et al (2011) Biomarkers in fasting serum to estimate glucose tolerance, insulin sensitivity, and insulin secretion. Clin Chem 57:326–337
Inoue N (2006) Vascular C-reactive protein in the pathogenesis of coronary artery disease: role of vascular inflammation and oxidative stress. Cardiovasc Hematol Disord Drug Targets 6:227–231
Acknowledgments
K. Bank Petersen is acknowledged for excellent technical assistance.
Funding
This work was supported by the Danish Council for Strategic Research (TRAIN 10-092797).
Duality of interest
H. J. Møller and Aarhus University have received royalties from IQ Products, Groningen, the Netherlands. Aarhus University has filed a patent application, with H. J. Møller as co-inventor, for the use of sCD163 as a prognostic biomarker.
Contribution statement
CPF, SN, BKP and HJM contributed to the conception and design of the study. TP, LPS, ARN, CPF, BMB and HJM analysed the data. TP, LPS, BMB and HJM were responsible for drafting the article. ARN, CPF, SN and BKP revised the manuscript. All authors approved the final version.
Author information
Authors and Affiliations
Corresponding author
Additional information
T. Parkner and L. P. Sørensen are joint first authors.
Rights and permissions
About this article
Cite this article
Parkner, T., Sørensen, L.P., Nielsen, A.R. et al. Soluble CD163: a biomarker linking macrophages and insulin resistance. Diabetologia 55, 1856–1862 (2012). https://doi.org/10.1007/s00125-012-2533-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-012-2533-1