Abstract
Aims/hypothesis
Non-diabetic hyperglycaemia is usually not considered at all or is viewed as a binary risk category in isolation from other factors when quantifying cardiovascular risk. We argue that hyperglycaemia should be considered as a continuous risk factor and only in the context of other vascular risk factors. To examine the potential impact of hyperglycaemia on cardiovascular disease (CVD) risk, we calculated the absolute CVD risk in groups defined by different levels of HbA1c and other CVD risk factors.
Methods
We used data on 10,144 men and women from the European Prospective Investigation of Cancer-Norfolk cohort to calculate CVD rates across levels of HbA1c in groups characterised by different levels of traditional risk factors.
Results
We found significant differences in CVD rates across levels of HbA1c in groups defined by different levels of the other risk factors. CVD rates for non-diabetic individuals with an HbA1c of <5.5% increased from 0.6 (95% CI 0.3–1.2) to 29.6 (95% CI 14.8–59.1) per 1,000 person-years when traditional CVD risk factors were added sequentially to the lowest risk reference group. In most cases, non-diabetic individuals with an HbA1c of <5.5% and high values for all other CVD risk factors had substantially higher absolute CVD rates than those with an HbA1c of 6.0% to 6.4% but with no other raised CVD risk factors (29.6 [95% CI 14.8–59.1] and 2.5 [95% CI 0.4–18.1], respectively). A history of diabetes significantly increased CVD risk over the non-diabetic hyperglycaemia range. Comparisons of CVD rates across tertiles of total cholesterol:HDL-cholesterol ratio or mean systolic blood pressure in groups characterised by different levels of other risk factors showed similar findings.
Conclusions/interpretation
In people with non-diabetic hyperglycaemia, cardiovascular risk is highly dependent on the presence of other CVD risk factors. Attention should be given not to whether an individual has ‘pre-diabetes’, ‘hypertension’ or ‘hypercholesterolaemia’, but to an integrated assessment of CVD risk, based on the combination of risk factors present and potential benefits of treatment.
Similar content being viewed by others
Introduction
Observational studies have shown a continuous association between traditional cardiovascular risk factors such as cholesterol [1] and blood pressure [2], and risk of cardiovascular disease (CVD). Randomised controlled trials have confirmed that treatment with lipid-lowering medication reduces the risk of ischaemic heart disease and stroke, regardless of pre-treatment blood cholesterol levels or other characteristics of the study participants [3]. Similarly, trials of blood pressure-lowering drugs have shown that relative risk reductions are comparable at different pre-treatment levels of blood pressure [4, 5]. This suggests that substantial benefits could be achieved from modifying these risk factors at any starting level in individuals whose absolute CVD risk is high for whatever aetiological reason [6]. The concept of treating individuals with a disease diagnosed by a threshold of one single risk factor, e.g. hypertension or hypercholesterolaemia, has thus been challenged [6, 7]. An approach using multivariate risk assessment tools to estimate absolute CVD risk, and consideration of the costs and benefits of treatment based on this value has been advocated in many countries [7, 8].
Glycaemia is an important risk factor for CVD, not only among people with diabetes, but across the whole spectrum of glucose levels. Observational studies show a consistent and continuous relationship between glycaemia and CVD risk, even below diagnostic thresholds for diabetes. HbA1c has been shown to predict CVD and all-cause and cardiovascular mortality rates independently of known cardiovascular risk factors [9, 10]. The effects of treatment to lower blood glucose among people with diabetes are broadly compatible with the observational evidence [11–15]. However, it is unclear whether lowering blood glucose in those with non-diabetic hyperglycaemia will reduce CVD risk [16–18]. Despite the strong evidence of linearity between glucose levels and cardiovascular risk among non-diabetic individuals [9], most authorities have persisted in treating non-diabetic hyperglycaemia as a category usually defined as impaired fasting glucose, impaired glucose tolerance or ‘pre-diabetes’. In the assessment of cardiovascular risk in populations, non-diabetic hyperglycaemia is either not considered at all or is dealt with independently from other cardiovascular risk factors with people being categorised as either having ‘pre-diabetes’ or not. To integrate non-diabetic hyperglycaemia with other risk factors for the assessment and management of cardiovascular risk, we calculated relative and absolute CVD risk in groups defined by different levels of CVD risk factors, including HbA1c, in a large population-based cohort: the European Prospective Investigation of Cancer-Norfolk (EPIC-Norfolk).
Methods
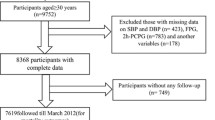
We used data from EPIC-Norfolk, which is a population-based prospective study of men and women aged 40 to 79 years residing in the Norfolk region of the UK. Details of the study have been described elsewhere [19]. Briefly, between 1993 and 1997, 77,630 individuals were invited from general practice to participate in the study. Of these, 25,639 (33%) consented and attended a baseline health assessment. Participants completed questionnaires about their personal and family history of disease, medication and lifestyle factors including smoking habits (current, ex- and non-smokers). They were asked whether a physician had ever told them that they had any of the conditions in a list including diabetes, heart attack and stroke. Additionally, baseline diabetes status was ascertained by: (1) self-report of diabetes medication; (2) diabetes medication brought to the baseline examination; (3) participants indicating modification of their diet in the past year because of diabetes mellitus; or (4) participants indicating adherence to a diabetic diet. Anthropometric and blood pressure measurements and non-fasting blood samples were also taken. We excluded individuals who had CVD at baseline (n = 1,106) and those with missing values for one or more traditional CVD risk factors (n = 2,662). As funding for HbA1c only became available in 1995, around half of all participants had information on this measure at baseline. HbA1c was measured in fresh EDTA blood samples using high-performance liquid chromatography (Diamat Automated Glycated Hemoglobin Analyzer; Bio-Rad Laboratories, Hemel Hempstead, UK), which was standardised to DCCT criteria. [20] We excluded participants without data on HbA1c (n = 11,727), leaving 10,144 individuals for our analyses. During the study period, general practitioners of participants whose test results were abnormal (HbA1c ≥ 7.0%) were notified so that they could assume responsibility for confirming diagnosis and arranging treatment. In the present study, participants were identified as having diabetes if they: (1) reported physician-diagnosed diabetes, diet modification due to diabetes or diabetes medication, or brought diabetes medication to the baseline health assessment; and/or (2) had an HbA1c of ≥6.5% at baseline [21, 22]. We used values of continuous risk factors such as HbA1c, blood pressure and blood lipids measured at baseline for all analyses.
The Norfolk area is slightly healthier than the general UK population, with a standardised mortality ratio of 93 (source: registration data, 2008, from Office for National Statistics, London, UK; www.statistics.gov.uk/StatBase/ssdataset.asp?vlnk=9876&Pos=1&ColRank=1&Rank=272, accessed 15 February 2010). However, the EPIC-Norfolk cohort is similar to a nationally representative sample with regard to anthropometric indices, blood pressure and serum lipids [19].
We followed up participants who were free from CVD at the time of recruitment until development of a first CVD event or death. We report results for follow-up to 30 April 2007, a median of 10.1 years (interquartile range 9.6–10.8). Incident CVD was defined as a composite of fatal or non-fatal CVD, including hospitalisation for coronary heart disease and stroke, or death from coronary heart disease, stroke peripheral vascular disease. Vital status for all EPIC-Norfolk participants was obtained via death certification at the Office for National Statistics. Participants admitted to a hospital were identified by their National Health Service number. Hospitals were linked to the East Norfolk Health Authority database, which identifies all hospital contacts throughout England and Wales for Norfolk residents. Follow-up data were 95% complete for hospital records and over 99% complete for death. Previous validation studies in this prospective cohort indicated high specificity of such case ascertainment [23].
Baseline characteristics were summarised separately for men and women, with and without a first cardiovascular event, using percentages, means and medians. We tested for differences between groups using χ2 tests for categorical variables and t tests or Kruskal–Wallis tests for normally or non-normally distributed continuous variables.
We calculated CVD event rates by dividing the number of CVD events by person-years of follow-up. Follow-up was defined as the period from the date of the first health assessment to the first event date (date of hospitalisation or date of death) or 30 April 2007. We used Cox proportional hazards regression to calculate the age-adjusted relative risk of developing a first CVD event in groups defined by different levels of systolic BP, total cholesterol, HDL-cholesterol, total cholesterol:HDL-cholesterol ratio (TC:HDL ratio) and HbA1c. Cut-off points for these risk factors were chosen on the basis of clinically meaningful values in line with national and international guidelines [21, 24–26]. Proportional hazards assumptions were evaluated using Kaplan–Meier survival curves for categorical variables, none of which violated the assumptions.
To examine the combined effect of cardiovascular risk factors, we started by calculating the CVD event rate in the lowest risk reference group of non-smoking non-diabetic women aged ≤55 years and with systolic BP of ≤140 mmHg and a TC:HDL ratio of ≤4.5 (the mean value in this population). We then calculated CVD rates for groups characterised by the sequential addition of risk factors (non-modifiable followed by modifiable) to the reference group, i.e. by adding age >55 years, male sex, TC:HDL ratio >4.5, systolic BP >140 mmHg, smoking and diabetes. CVD rates for these groups were calculated for different levels of HbA1c (<5.5%, 5.5–5.9% and 6.0–6.4%). We did not include total cholesterol in this stage of analysis as it was not significantly associated with CVD risk in this study population. We evaluated the difference in cardiovascular event rates across groups using the logrank test for trend. We carried out sensitivity analyses, examining different cut-off points for age and different components of cholesterol. We also explored the effect of adding risk factors in a different order, i.e. adding age and sex after the modifiable risk factors.
We also compared CVD rates across tertiles of TC:HDL ratio (<3.7, 3.7–5.0 and >5.0) or mean systolic blood pressure (<126, 126–140 and >140 mmHg) in groups characterised by different levels of other risk factors.
Results
Baseline characteristics of the study population by CVD outcome and sex are shown in Table 1. The mean age (SD) at baseline was 57.3 (9.6) years and 4,429 (44%) of the population were men. Individuals who developed CVD were older than those who did not. They were more likely to be men, from a lower social class and to have diabetes than those who did not develop CVD. People who developed CVD also had higher levels of systolic BP, BMI, total cholesterol, TC:HDL ratio and HbA1c, and lower HDL-cholesterol values at baseline.
Relative risk of CVD
Figure 1a–d shows the age-adjusted relative risk of developing a first CVD event by different levels of each risk factor. The risk of CVD increased by 9% for each year of age (HR 1.09 [95% CI 1.09–1.10]). Individuals aged >70 years had 15 times the CVD risk of those aged <50 years. Men had around a twofold higher risk of CVD than women. Smoking conferred an 82% increase in CVD risk (HR 1.82 [95% CI 1.52–2.18]). Total cholesterol was not significantly associated with risk of CVD in any of its strata. CVD risk increased with each decreasing stratum of HDL-cholesterol. A more than twofold increase in CVD risk was seen in individuals with HDL-cholesterol of <1.0 mmol/l compared with those with HDL-cholesterol of ≥1.5 mmol/l. Risk of CVD increased across each increasing stratum of TC:HDL ratio. Among the lipid measures, TC:HDL ratio had the strongest association with CVD risk (χ2 for trend: 752.4, 732.3 and 658.6 for TC:HDL ratio, HDL-cholesterol and total cholesterol, respectively). Increasing levels of systolic BP and HbA1c were significantly associated with an increased risk of CVD. Thus, individuals with systolic BP of 140 to 159 mmHg and ≥160 mmHg had a 30% and 70% higher CVD risk, respectively, than those with systolic BP of <130 mmHg. Each 1% increase in HbA1c was associated with a 27% increase in CVD risk (HR 1.27 [95% CI 1.21–1.33]). Individuals with an HbA1c of ≥6.5% were more than twice as likely to develop CVD than those with an HbA1c of <5.5%.
Absolute risk of CVD by levels of HbA1c and other risk factors
There were 966 CVD events during 980,003 person-years of observation. The overall CVD rate was 9.86 (95% CI 9.25–10.50) per 1,000 person-years. CVD rates in individuals with HbA1c <5.5%, 5.5 to 5.9% and 6.0 to 6.4% and in those with diabetes were 7.04 (95% CI 6.42–7.72), 12.36 (11.00–13.89), 16.50 (13.67–19.91) and 28.94 (24.24–34.56) per 1,000 person-years, respectively (χ2 for trend: 265.5, p < 0.001).
Figure 2 shows the effect on absolute CVD risk (incidence of a first CVD event) of successively adding risk factors in individuals with different HbA1c levels. Across all subgroups defined by the presence or absence of traditional cardiovascular risk factors, increasing values of HbA1c were associated with increasing CVD risk. At each level of HbA1c, CVD rates increased when another risk factor was successively added (p < 0.05 for all levels of HbA1c). The lowest CVD rate was observed in non-smoking non-diabetic women aged ≤55 years with systolic BP ≤140 mmHg, a TC:HDL ratio of ≤4.5 (reference group) and HbA1c <5.5% (CVD rate 0.6 [95% CI 0.3–1.2] per 1,000 person-years). The CVD rate was as high as 29.6 (95% CI 14.8–59.1) per 1,000 person-years in non-diabetic male smokers with the same level of HbA1c but aged >55 years and with systolic BP >140 mmHg and a TC:HDL ratio of >4.5. In most cases, individuals with a low HbA1c level and high values for all other CVD risk factors had a much higher absolute CVD risk than those with a high HbA1c level but with no other raised CVD risk factors. For example, male non-smokers with HbA1c < 5.5%, systolic BP >140 mmHg and a TC:HDL ratio of >4.5 had a higher rate of CVD than individuals with HbA1c of 6.0 to 6.4%, but normal levels of other risk factors (CVD rate 29.6 [95% CI 14.8–59.1] and 2.5 [95% CI 0.4–18.1], respectively). Diabetes considerably increased the risk of CVD over the non-diabetic hyperglycaemia range.
Absolute rates of cardiovascular events over 10 years by HbA1c levels in individuals with different levels of other CVD risk factors in EPIC-Norfolk (n = 10,144). Reference represents a non-smoking, non-diabetic woman aged ≤55 years with TC:HDL ratio of ≤4.5 and a mean systolic BP (SBP) of ≤140 mmHg. In other groups, risk factors were added sequentially, i.e. age >55 years, male sex, TC:HDL ratio >4.5, SBP >140 mmHg, current cigarette smoking and diabetes. *p < 0.05 for difference in CVD rates between different levels of HbA1c. White bars, HbA1c <5.5%; hatched bars, HbA1c 5.5–5.9%; grey bars, HbA1c 6.0–6.4%
The main findings were not significantly altered by changing the order in which risk factors were added, changing the age cut-off point from 55 to 60 years or using HDL-cholesterol instead of TC:HDL ratio.
Comparisons of CVD rates across tertiles of TC:HDL ratio or mean systolic BP in groups characterised by different levels of other risk factors showed similar findings to those for HbA1c (Figs 3 and 4).
Absolute rates of cardiovascular events over 10 years by tertiles of TC:HDL ratio in individuals with different levels of other CVD risk factors in EPIC-Norfolk (n = 10,144). Reference represents a non-smoking, non-diabetic woman aged ≤55 years with a mean systolic BP (SBP) of ≤140 mmHg and HbA1c <6.0%. In other groups, risk factors were added sequentially, i.e. age >55 years, male sex, systolic BP of >140 mmHg, HbA1c of >6.0%, diabetes and current cigarette smoking. *p < 0.05 for difference in CVD rates across tertiles of TC:HDL ratio. White bars, TC:HDL ratio <3.7; hatched bars, TC:HDL ratio 3.7–5.0; grey bars, TC:HDL ratio >5.0. The values 1,171 and 160 are the point estimates of CVD rates in each subgroup
Absolute rates of cardiovascular events over 10 years by tertiles of mean systolic BP in individuals with different levels of other CVD risk factors in EPIC-Norfolk (n = 10,144). Reference represents a non-smoking, non-diabetic woman aged ≤55 years with TC:HDL ratio of ≤4.5 and HbA1c <6.0%. In other groups, risk factors were added sequentially, i.e. age >55 years, male sex, TC:HDL ratio of >4.5, HbA1c >6.0%, diabetes and current cigarette smoking. *p < 0.05 for difference in CVD rates across tertiles of mean systolic BP. White bars, systolic BP <126 mmHg; hatched bars, systolic BP 126–140 mmHg; grey bars, systolic BP >140 mmHg
Discussion
Summary of findings
We have documented the combined effect of risk factors, including HbA1c in the non-diabetic range, on risk of developing CVD. Our findings reinforce the view that calculation of cardiovascular risk should integrate hyperglycaemia as a continuous risk factor. Decisions on treatment for primary prevention of CVD should not be based on threshold levels of individual risk factors, including glycaemia, but mainly on the estimation of absolute CVD risk and on the costs and benefits of treatments that target individual risk factors as well as combinations of treatments. Our findings suggest that aiming for moderate reductions in several risk factors may be more effective than large reductions in one risk factor, even before consideration of the fewer side effects associated with lower doses of treatment.
Comparisons with previous studies
We confirm previous studies showing that there is a common pattern of association between risk factors such as systolic BP, HDL-cholesterol, TC:HDL ratio and HbA1c and CVD risk without any obvious risk thresholds across a wide range of levels. A meta-analysis of 61 prospective studies showed that total cholesterol, HDL-cholesterol and TC:HDL ratio were continuously associated with death from ischaemic heart disease at all ages and blood pressure levels, and with stroke mortality rates in middle-aged individuals [1]. Another meta-analysis by the same authors found that blood pressure was strongly associated with risk of stroke and death from ischaemic heart disease throughout middle and old age, without any evidence of a threshold [2]. The authors reported a constant proportional change in CVD risk for a given change in each risk factor, a finding similar to our own findings. Previous studies using data from the EPIC-Norfolk cohort reported an independent association of HbA1c with risk of CVD events, and with all-cause and CVD-specific death [9, 27]. We have now demonstrated differences in absolute CVD rates across HbA1c levels (both in non-diabetic and diabetic ranges) in individuals with different levels of other CVD risk factors. Jackson et al. have also shown the effect on absolute CVD risk of sequentially adding risk factors in individuals with different levels of blood pressure and total cholesterol [7]. However, they used the Framingham risk equations to calculate modelled CVD risk [7]. Here, we have demonstrated the combined effects of risk factors including HbA1c on actual CVD rates in a representative British population.
Uncertainties about the beneficial effects of lowering blood glucose on CVD risk
Evidence from prospective observational studies shows a continuous relationship between HbA1c and CVD. Data from intervention studies are broadly consistent with the observational data in people with established diabetes. A meta-analysis of the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial, Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified Release Controlled Evaluation (ADVANCE) trial, Veterans Affairs Diabetes Trial (VADT) and UK Prospective Diabetes Study (UKPDS) suggests that tight glycaemic control may reduce CVD risk among patients with diabetes [15]. However, it remains unclear whether interventions used to lower blood glucose in individuals with non-diabetic hyperglycaemia will reduce CVD risk. Clinical trials primarily designed to prevent diabetes in people with impaired glucose tolerance by lifestyle modification [16, 17] and pharmacological intervention [17, 18] did not have adequate power to detect a beneficial effect on cardiovascular risk. Recently, the Nateglinide and Valsartan in Impaired Glucose Tolerance Outcomes Research (NAVIGATOR) trial , which was the first clinical trial devised to investigate the effect of lowering blood glucose on the risk of cardiovascular events as a primary outcome in people with non-diabetic hyperglycaemia, showed no reduction in cardiovascular events over 6 years [28]. However, while a small reduction in plasma glucose levels was observed, 2-h post-challenge glucose was elevated in the intervention compared with the control groups. It is likely that the benefit of glucose-lowering therapy is modest compared with interventions targeting other risk factors [29]. The lower-than-expected CVD rates in the intervention and control groups in the ACCORD trial, ADVANCE trial and VADT highlight the importance of an integrated approach to the assessment and treatment of all CVD risk factors, not only hyperglycaemia [29].
The importance of absolute CVD risk estimation
The combined effect of risk factors on absolute risk of CVD emphasises the importance of using multivariate risk prediction tools. Previous studies have shown that a small effect of an individual risk factor on CVD risk could be magnified in the presence of other risk factors. In other words, an individual with mildly abnormal levels of several risk factors often has a greater absolute CVD risk than someone with a raised level of one risk factor [7, 30]. Neaton and Wentworth showed that absolute CVD risk can vary up to 20-fold in people with the same levels of traditional CVD risk factors such as cholesterol and blood pressure [31]. Our study supports this finding by demonstrating that non-diabetic individuals with a ‘low’ HbA1c level and high values for all other CVD risk factors had a markedly higher absolute CVD risk than those with a ‘high’ HbA1c level but with no other raised CVD risk factors.
Compared with multifactorial CVD risk assessment, major CVD risk factors such as blood pressure or blood lipid levels are, individually, poorer predictors of CVD risk and of the benefits of treatment in individuals with and without existing CVD [6, 8]. The same is demonstrably true for non-diabetic hyperglycaemia. This suggests that clinicians should treat patients based mainly on absolute CVD risk, rather than treating them according to the presence of hypertension, hypercholesterolaemia or pre-diabetes.
Strengths and limitations
In this large prospective cohort with robust ascertainment of CVD events, we have shown that different levels of CVD risk factors, including HbA1c, confer different risks of CVD events. Due to the small number of individuals and CVD events in some groups, we did not find a significant difference in CVD rates across HbA1c levels in all of the subgroups of individuals. Using hospital linkage data for ascertainment of CVD outcomes might lead to misclassification of non-fatal CVD events, as not all non-fatal CVD cases lead to hospital admission. However, this method captures the non-fatal events of most clinical importance, and previous validation studies in this cohort have indicated high specificity of such case ascertainment [23]. We used values of HbA1c, blood pressure and blood lipids measured at baseline rather than ‘usual levels’ for our analysis. It is therefore possible that regression dilution might have led to underestimation of the association between these risk factors and CVD. The EPIC-Norfolk study sample was similar to the UK population in terms of anthropometry, blood pressure and serum lipids. However, given the 33% participation rate in this study, it is possible that attendees might have been more health-conscious and more likely to seek existing preventive services than non-attendees. Furthermore, our research question required around half of the study participants to be excluded due to a lack of HbA1c data, and those included in this analysis were healthier than those excluded (according to their risk factor profiles). We might therefore have underestimated the population incidence of cardiovascular events. However, this is likely to have a limited influence on our main finding that cardiovascular risk in non-diabetic hyperglycaemia is largely reliant on the presence of other risk factors.
Conclusions
Cardiovascular risk has a linear and continuous association with many CVD risk factors, including HbA1c. This suggests that attention should focus less on whether an individual has pre-diabetes, hypertension or hypercholesterolaemia, and more on an integrated consideration of absolute CVD risk. Management of cardiovascular risk should be based upon quantitative assessment of CVD risk and treatment benefits, taking into account differential effects, costs and side effects of treatments for each risk factor.
Abbreviations
- ACCORD:
-
Action to Control Cardiovascular Risk in Diabetes
- ADVANCE:
-
Action in Diabetes and Vascular Disease: Preterax and Diamicron Modified Release Controlled Evaluation
- CVD:
-
Cardiovascular disease
- EPIC-Norfolk:
-
European Prospective Investigation of Cancer-Norfolk
- TC:HDL ratio:
-
Total cholesterol:HDL-cholesterol ratio
- VADT:
-
Veterans Affairs Diabetes Trial
References
Lewington S, Whitlock G, Clarke R et al (2007) Blood cholesterol and vascular mortality by age, sex, and blood pressure: a meta-analysis of individual data from 61 prospective studies with 55,000 vascular deaths. Lancet 370:1829–1839
Lewington S, Clarke R, Qizilbash N, Peto R, Collins R (2002) Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 360:1903–1913
Baigent C, Keech A, Kearney PM et al (2005) Efficacy and safety of cholesterol-lowering treatment: prospective meta-analysis of data from 90, 056 participants in 14 randomised trials of statins. Lancet 366:1267–1278
Yusuf S, Sleight P, Pogue J, Bosch J, Davies R, Dagenais G (2000) Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. The Heart Outcomes Prevention Evaluation Study Investigators. N Engl J Med 342:145–153
PROGRESS Collaborative Group (2001) Randomised trial of a perindopril-based blood-pressure-lowering regimen among 6,105 individuals with previous stroke or transient ischaemic attack. Lancet 358:1033–1041
Law MR, Wald NJ (2002) Risk factor thresholds: their existence under scrutiny. BMJ 324:1570–1576
Jackson R, Lawes CM, Bennett DA, Milne RJ, Rodgers A (2005) Treatment with drugs to lower blood pressure and blood cholesterol based on an individual’s absolute cardiovascular risk. Lancet 365:434–441
Jackson R (2008) Cardiovascular risk prediction: are we there yet? Heart 94:1–3
Khaw KT, Wareham N, Bingham S, Luben R, Welch A, Day N (2004) Association of hemoglobin A1c with cardiovascular disease and mortality in adults: the European prospective investigation into cancer in Norfolk. Ann Intern Med 141:413–420
Selvin E, Marinopoulos S, Berkenblit G et al (2004) Meta-analysis: glycosylated hemoglobin and cardiovascular disease in diabetes mellitus. Ann Intern Med 141:421–431
No authors listed (1998) Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group. Lancet 352:837–853
Patel A, MacMahon S, Chalmers J et al (2008) Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med 358:2560–2572
Gerstein HC, Miller ME, Byington RP et al (2008) Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med 358:2545–2559
Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA (2008) 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med 359:1577–1589
Turnbull FM, Abraira C, Anderson RJ et al (2009) Intensive glucose control and macrovascular outcomes in type 2 diabetes. Diabetologia 52:2288–2298
Tuomilehto J, Lindstrom J, Eriksson JG et al (2001) Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 344:1343–1350
Knowler WC, Barrett-Connor E, Fowler SE et al (2002) Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 346:393–403
Gerstein HC, Yusuf S, Bosch J et al (2006) Effect of rosiglitazone on the frequency of diabetes in patients with impaired glucose tolerance or impaired fasting glucose: a randomised controlled trial. Lancet 368:1096–1105
Day N, Oakes S, Luben R et al (1999) EPIC-Norfolk: study design and characteristics of the cohort. European Prospective Investigation of Cancer. Br J Cancer 80(Suppl 1):95–103
Little RR, Rohlfing CL, Wiedmeyer HM, Myers GL, Sacks DB, Goldstein DE (2001) The national glycohemoglobin standardization program: a five-year progress report. Clin Chem 47:1985–1992
Nathan DM, Balkau B, Bonora E et al (2009) International Expert Committee report on the role of the A1C assay in the diagnosis of diabetes. Diabetes Care 32:1327–1334
American Diabetes Association (2010) Diagnosis and classification of diabetes mellitus. Diabetes Care 33(Suppl 1):S62–S69
Boekholdt SM, Peters RJ, Day NE et al (2004) Macrophage migration inhibitory factor and the risk of myocardial infarction or death due to coronary artery disease in adults without prior myocardial infarction or stroke: the EPIC-Norfolk Prospective Population study. Am J Med 117:390–397
National Cholesterol Education Program Expert Panel (2002) Third report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 106:3143–3421
Chobanian AV, Bakris GL, Black HR et al (2003) The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 289:2560–2572
Joint British Societies (2005) JBS 2: Joint British societies’ guidelines on prevention of cardiovascular disease in clinical practice. Heart 91(Suppl 5):v1–v52
Khaw KT, Wareham N, Luben R et al (2001) Glycated haemoglobin, diabetes, and mortality in men in Norfolk cohort of European prospective investigation of cancer and nutrition (EPIC-Norfolk). BMJ 322:15–18
NAVIGATOR Study Group (2010) Effect of nateglinide on the incidence of diabetes and cardiovascular events. N Engl J Med 362:1463–1476
Skyler JS, Bergenstal R, Bonow RO et al (2009) Intensive glycemic control and the prevention of cardiovascular events: implications of the ACCORD, ADVANCE, and VA diabetes trials: a position statement of the American Diabetes Association and a scientific statement of the American College of Cardiology Foundation and the American Heart Association. Circulation 119:351–357
Anderson KM, Odell PM, Wilson PW, Kannel WB (1991) Cardiovascular disease risk profiles. Am Heart J 121:293–298
Neaton JD, Wentworth D (1992) Serum cholesterol, blood pressure, cigarette smoking, and death from coronary heart disease. Overall findings and differences by age for 316, 099 white men. Multiple Risk Factor Intervention Trial Research Group. Arch Intern Med 152:56–64
Acknowledgements
Funding support was provided by the Medical Research Council (grant G950223), Cancer Research UK (grant C8648A3883) and European Union (Europe Against Cancer Programme number 6438). P. Chamnan is supported by a Royal Thai Government scholarship. S. J. Griffin receives support from the National Institute for Health Research (NIHR) Programme Grant funding scheme (RP-PG-0606-1259). We gratefully acknowledge the contributions of the EPIC-Norfolk participants and the EPIC-Norfolk team.
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chamnan, P., Simmons, R.K., Jackson, R. et al. Non-diabetic hyperglycaemia and cardiovascular risk: moving beyond categorisation to individual interpretation of absolute risk. Diabetologia 54, 291–299 (2011). https://doi.org/10.1007/s00125-010-1914-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-010-1914-6