Abstract
Aims/hypothesis
Type 1 diabetes is a T cell-mediated autoimmune disease with a clinically silent prodrome, during which prediction and treatment of disease are theoretically possible. Using retrospective analysis, spontaneous disease in the non-obese diabetic (NOD) mouse has been correlated with islet-specific glucose-6-phosphatase catalytic subunit-related protein (IGRP)-reactive CD8+ T cells in the peripheral blood. In this study, we determined prospectively whether IGRP-reactive T cells in peripheral blood could predict disease occurrence. Since recurrent autoimmunity is an important contributor to transplant failure, we also determined whether failure of islet grafts (syngeneic and allogeneic) could be predicted by the presence of circulating autoreactive T cells.
Materials and methods
Peripheral blood samples were taken weekly from female NOD mice between the ages of 8 and 30 weeks and from NOD mice transplanted with NODscid islets. Peripheral blood cells and islet grafts were analysed for the presence of IGRP-reactive CD8+ T cells by flow cytometry.
Results
Prospective analysis of peripheral blood IGRP-reactive T cells in the prediabetic period predicted disease development with a sensitivity of 100% and a specificity of 60%, resulting in positive and negative predictive values of 85 and 100%, respectively. Significant proportions of IGRP-reactive T cells were found in the grafts, but not in peripheral blood of NOD mice undergoing syngeneic and allogeneic rejection.
Conclusions/interpretation
The occurrence of spontaneous diabetes can be predicted prospectively by measuring peripheral blood autoreactive T cells. Rejection of syngeneic or allogeneic islets is associated with large populations of autoreactive CD8+ T cells within islets, suggesting that immunodominant autoreactive T cells during the prediabetic period are also responsible for autoimmune graft rejection.
Similar content being viewed by others
Introduction
In spontaneous immune-mediated diabetes, pancreatic islet beta cells are selectively targeted and destroyed by autoreactive T cells. The initiation and propagation of disease are a consequence of the combined actions of self-reactive CD4+ and CD8+ T cells, with increasing evidence pointing to an important role for CD8+ cytotoxic T lymphocytes (CTL) in the destruction of beta cells, both in humans and in the non-obese diabetic (NOD) mouse model of the disease [1]. In the NOD mouse, three CTL specificities with in vivo pathogenicity have been identified. These CTL recognise peptide sequences from the insulin B chain15 – 23 (G9C8 clone) [2], islet-specific glucose-6-phosphatase catalytic subunit-related protein (IGRP206 – 214; 8.3 clone) [3] and dystrophia myotonica kinase (AI4 clone) [4]. Together, these CTL populations constitute a large proportion (up to 60%) of the CD8+ T cells within the pancreatic islets of prediabetic NOD mice [4, 5].
The clinical onset of human type 1 diabetes is generally preceded by an asymptomatic phase during which islet beta cell mass decreases. This phase represents a window of opportunity for disease prediction and testing of potential therapeutic interventions. After tracking IGRP206 – 214-reactive T cells with MHC class I tetramers in the peripheral blood of prediabetic NOD mice and using a retrospective analysis, we have previously shown that disease outcome could be predicted on the basis of the frequency of circulating IGRP206 – 214-reactive CD8+ T cells [5]. Our study demonstrated that mice that subsequently went on to develop diabetes had a significantly higher proportion of IGRP206 – 214-reactive T cells in the peripheral blood many weeks prior to disease onset than mice that remained diabetes-free. Prospective validation of these previously established prediction criteria would make such an approach more valuable in disease prediction.
In addition to prediction of spontaneous disease, the ability to predict rejection of beta cell grafts would be useful for monitoring islet transplant recipients. Beta cell replacement by islet transplantation has shown promise as therapy for individuals with type 1 diabetes [6], and with the advent of the Edmonton protocol [7], the clinical feasibility of islet transplantation has been realised [8]. The mechanisms underlying graft failure are not fully known, but probably involve both alloimmune rejection of the graft, autoimmune destruction of beta cells and primary graft non-function [9]. At present, assessment of islet graft health following islet transplantation is difficult, and surrogate measures such as C-peptide production and insulin requirements are commonly used for monitoring graft health and survival [8]. The ability to directly assess the activity of beta-cell-reactive T cells could provide an elegant and sensitive means of determining the level of ongoing autoimmune-mediated beta cell damage within transplanted tissue.
We postulated that an increase in the prevalence of circulating IGRP-reactive CD8+ T cells occurs not only during the development of spontaneous diabetes, but also as islet grafts are destroyed, allowing for prediction of both spontaneous diabetes and islet graft failure. In the present study, we sought to validate our criteria for prospective prediction of diabetes in the NOD mouse, with a view to stratifying mice a priori into control and treatment arms for testing efficacy of preventive interventions. We also sought to determine whether recurrent diabetes and graft failure following islet transplantation were predictable based on the presence of IGRP206 – 214-reactive T cells in the peripheral blood.
Materials and methods
Mice NODltj, NODscid, BALB/C and C57BL/6 mice were purchased from The Jackson Laboratories (Bar Harbor, ME, USA) and maintained in a specific pathogen-free animal facility. Animal experiments were performed in accordance with the guidelines of the Animal Care Committee, University of British Columbia. Mice were considered diabetic following two consecutive blood glucose measurements of >17 mmol/l. Diabetic mice were maintained with 0.5 U/day of Humulin NPH (Eli Lilly Canada, Toronto, ON, Canada) or with LinBit insulin implants (LinShin Canada, Toronto, ON, Canada).
Blood collection and tetramer staining
Beginning at 8 weeks of age, blood (130 μl) was sampled weekly from the femoral vein into heparinised capillary tubes. Blood was processed, stained and analysed by flow cytometry as previously described [5]. Briefly, erythrocytes were lysed and the remaining cells were stained with Kd-NRP-V7 or Kd-TUM (control) tetramers for 60 min, followed by fluorescein–isothiocyanate-conjugated anti-CD8 (clone YTS 169.4; Cedarlane Laboratories, Hornby, ON, Canada) and PerCP-conjugated anti-B220 (clone RA3-6B2; Pharmingen, San Diego, CA, USA). Tetramer-positive cells are expressed as the percentage of CD8+ B220− cells, minus the percentage of Kd-TUM tetramer-positive cells (<0.05%).
Transplantation
Islets were isolated from 8- to 12-week-old mice by perfusion of the common bile duct with collagenase (type XI; Sigma-Aldrich, Oakville, ON, Canada), followed by density gradient centrifugation. A total of 550 islets were transplanted under the kidney capsule of diabetic NOD recipients. In order to assess the composition of the transplanted islets following graft failure, grafts were removed within a margin of renal tissue, and a single-cell suspension was generated by mechanical dissociation, followed by incubation in 2 ml of Cell Dissociation Buffer (Gibco-BRL, Invitrogen, Burlington, ON, Canada) for 8 min at 37°C. Cells were then stained and analysed as described above.
Results
Prospective prediction of spontaneous diabetes
Beginning at 8 weeks of age, 32 prediabetic female NOD mice were monitored weekly for the presence of IGRP206 – 214-reactive CD8+ T cells using Kd-NRP-V7 MHC class I tetramers. NRP-V7 is a high-avidity peptide mimotope of IGRP206 – 214 that allows for highly sensitive detection of IGRP206 – 214-reactive CD8+ T cells [10]. The proportion of NRP-V7-positive CD8+ T cells over the course of 30 weeks is shown for representative mice in Fig. 1a–h, with averaged data shown in Fig. 1i. Based on previous findings, the following criteria were used for prediction of disease development: (1) any single weekly blood sample with >0.50% Kd-NRP-V7 tetramer+ CD8+ B220− (minus control value); or (2) a value >0.75% following cumulative summation of the weekly percentage of Kd-NRP-V7 tetramer+ CD8+ B220− (minus control value) cells between 8 and 15 weeks of age.
The percentage of NRP-V7 tetramer+ CD8+ cells in the peripheral blood of NOD mice that were predicted (a–d, g, h) and not predicted (e, f) to develop diabetes. Representative examples for each group are shown (a–d, predicted, and subsequent diabetes; e, f, not predicted, and no diabetes; g, h, predicted, but no diabetes). For each animal, the weekly proportion of circulating Kd-NRP-V7 tetramer+ CD8+ B220− cells (filled circles) and relative blood glucose (dashed line) are shown. Normoglycaemia was defined as a level 6 mmol/l and significant hyperglycaemia as 25 mmol/l. Glucose normalisation following hyperglycaemia was the result of insulin treatment. For reference, the dashed line representing glycaemia is at a level of 0.50% Kd-NRP-V7 tetramer positivity for normoglycaemia (prediction criterion 1). Arrows represent the point at which an animal reached 0.75% cumulative Kd-NRP-V7 tetramer positivity (prediction criterion 2). i The averaged (±SEM) frequency of Kd-NRP-V7 tetramer+ CD8+ cells is shown for the three groups: (1) animals that were predicted to and did actually develop diabetes (circle, solid line); (2) animals that were predicted to develop diabetes but remained non-diabetic (triangle, dashed line); and (3) animals that were not predicted to develop diabetes and subsequently remained disease-free (square, solid line)
Over the course of 30 weeks, 22 of 32 mice developed diabetes (incidence = 69%). Of the mice that went on to develop diabetes, all were predicted to do so based on one or both criteria above (Fig. 1, Table 1). Of the ten mice that remained diabetes-free, four had been identified as pre-diabetic based on the prediction criteria, resulting in a prediction test sensitivity and specificity of 100 and 60%, respectively. Of 26 mice predicted to develop diabetes on the basis of satisfying either criterion, 22 actually did develop diabetes, resulting in a positive predictive value (PPV) of 85%. All mice that were not predicted to develop diabetes (6/6) remained diabetes-free for the duration of the study period (negative predictive value [NPV] = 100%). Diabetes outcome using the outlined prediction criteria is shown in Fig. 2. Table 1 shows the predictive values for diabetes development using a variety of different criteria.
Diabetes-free survival for NOD mice predicted to develop diabetes (circles) and for those predicted to remain diabetes-free (squares). The data demonstrate what the control diabetic (untreated) and non-diabetic groups would look like if the outlined prediction criteria were used to establish treatment groups a priori
Prediction of recurrent autoimmune diabetes following islet transplantation
Peripheral blood of prediabetic female NOD mice was monitored weekly, beginning at 8 weeks of age, for the presence of IGRP-reactive CD8+ T cells using Kd-NRP-V7 tetramers. As mice became diabetic, they were maintained with exogenous insulin. Four to six weeks following the onset of diabetes, insulin was discontinued and pancreatic islets derived from NODscid donors were transplanted under the kidney capsule of diabetic mice. Following transplantation, peripheral blood was again monitored for the presence of IGRP-reactive CD8+ T cells at 24 h and then each 48 h thereafter. Islet grafts were removed at various time points post-transplantation to determine the number of IGRP-reactive CD8+ T cells within the graft itself.
As described previously, large populations of IGRP-reactive CD8+ T cells were observed in the peripheral blood prior to diabetes onset, with a dramatic decline in number following the onset of hyperglycaemia [5]. One week prior to transplantation (4 to 6 weeks following the onset of hyperglycaemia), the number of IGRP-reactive CD8+ T cells in the peripheral blood was much lower than in pre-diabetic animals, ranging from 0.03 to 0.09% (Fig. 3). Following islet transplantation, no significant increase in the number of IGRP-reactive CD8+ T cells was seen in the peripheral blood on days 1, 3, 5, 7 or 9 post-transplantation (Fig. 3a–f,i). Immediately prior to graft failure, there was a slight tendency for the number of autoreactive CD8+ T cells to increase (Fig. 3i); however these increases were small and inconsistently observed.
IGRP-reactive CD8+ T cells do not appear in the peripheral blood prior to graft failure, but predominate in islet grafts. Peripheral blood was sampled and analysed for the presence of Kd-NRP-V7 tetramer+ CD8+ cells beginning at least 4 weeks prior to transplantation (n = 8). a The percentage of Kd-NRP-V7 tetramer+ CD8+ cells in the peripheral blood of female diabetic NOD mice that had been maintained on exogenous insulin for approximately 4 weeks (pre-transplant). b–f NODscid islets (n = 550) were then transplanted under the kidney capsule and the proportion of circulating Kd-NRP-V7 tetramer+ CD8+ cells was measured on pretransplant (a) and on post-transplant days 1 (b), 3 (c), 5 (d), 7 (e) and 9 (f). One representative experiment is shown (mean values see i). Numbers (top-right quadrants) indicate the percentage of CD8+ B220− tetramer+ cells. g, h Two examples of islet grafts that were analysed from day 6 post-transplantation, one (g) taken from a mouse that was normoglycaemic, the other (h) representing a graft taken on the day of graft failure. Numbers (top-right quadrants) indicate the percentage of CD8+ B220− tetramer+ cells. i Average percentages of Kd-NRP-V7 tetramer+ CD8+ cells determined in the peripheral blood pretransplantation (−1 week, n = 8) and post-transplantation (day [d]1, n = 8; d3, n = 4; d5, n = 7; d7, n = 4; d8, n = 1; d9, n = 3) and found (j) to have infiltrated the islet grafts (n = 10). The data shown are the percentage Kd-NRP-V7 tetramer+ CD8+ B220− (minus control) ±SEM
Following graft failure, islet grafts were removed from the kidney capsule and examined, and a significant proportion of IGRP-reactive CD8+ T cells was detected in the graft. The majority of grafts were removed on the first or second day following graft failure (ranging from day 6 to 9 post-transplantation; Table 2). Up to 51% of the CD8+ cells within the islet graft were IGRP-reactive as indicated by bright Kd-NRP-V7 tetramer staining (Fig. 3g,h), a proportion significantly higher than the islet infiltration that is seen during spontaneous disease [4, 5]. The amount of IGRP-reactive CD8+ T cells within the grafts ranged from 9.8 to 51.5%, with a mean of 21.7% (Fig. 3j, Table 2). The grafts of animals that never attained normoglycaemia following transplantation were indistinguishable from those of animals that did, containing comparable numbers of IGRP-reactive CD8+ T cells within the graft (Table 2).
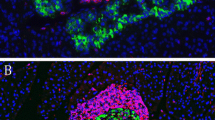
Expansion of IGRP-reactive T cells in islet allografts
An increase of IGRP-reactive CD8+ T cells was also seen when islets from BALB/C (H-2d) mice, matched for MHC class I but not class II, were used as donors (Fig. 4a,b; Table 2). As many as 14.3% of CD8+ T cells (mean = 6.8%) infiltrating allografts of BALB/C islets in diabetic NOD recipients were IGRP206 – 214-reactive. Interestingly, even when completely (MHC class I and II) mismatched (C57BL/6, H-2b) mice were used as donors, a significant infiltration of the graft with IGRP-reactive CD8+ T cells was still observed (Fig. 4c,d; Table 2). IGRP206 – 214-reactive cells comprised up to 14% (mean = 5.8%) of all CD8+ T cells in grafts of C57BL/6 islets in diabetic NOD recipients at the time of graft rejection.
IGRP-reactive CD8+ T cells proliferate in response to BALB/C (H-2d) and C57BL/6 (H-2b) islet grafts. Islets from BALB/C (n = 6) (a, b) or C57BL/6 mice (n = 4) (c, d) were transplanted under the kidney capsule of diabetic female NOD mice. Islet grafts were removed and assessed for the proportion of IGRP-reactive CD8+ T cells. Representative experiments are shown (a, c), with the mean (±SEM) percentage (b, d) of tetramer-positive cells for all of the grafts analysed. Numbers (top-right quadrants) indicate the percentage of CD8+ B220− tetramer+ cells
Discussion
Based on previously established prediction criteria [5], we were able to prospectively identify prediabetic mice 6.5 ± 3.6 weeks prior to onset of hyperglycaemia by quantifying IGRP206 – 214-reactive CD8+ T cells in peripheral blood. The varying and unpredictable incidence of diabetes in this animal model has thus far limited effective testing of preventative therapies in prediabetic NOD mice. Given the high positive predictive value (85%) of this methodology, these criteria could be used to assign animals to treatment and control groups when assessing treatment or prevention protocols in NOD mice, knowing with confidence that the large majority of predicted mice will develop diabetes. Use of this predictive test prior to initiation of a therapeutic intervention could greatly increase the power of a prevention trial to assess the efficacy of that intervention. Although only a few MHC class I epitopes have been identified in human type 1 diabetes [11, 12], and tetramer staining of circulating beta-cell-reactive CD8+ cells in diabetic humans has been limited [13], this approach may have even greater potential in human prevention trials, where the cost of such trials is increased by the relatively low prevalence (50% 5-year incidence) of disease in cohorts [14].
The averaged data of tetramer positivity (Fig. 1i) indicate that differences between mice that go on to develop diabetes and those that remain diabetes-free are most marked prior to 16 weeks of age. Further analysis of Fig. 1i revealed that those mice predicted to develop diabetes using the original predictive criteria, but which ultimately remained disease-free, would not have been incorrectly predicted had data prior to 16 weeks been used rather than for the entire period to 30 weeks. Therefore, for purposes of testing the efficacy of diabetes prevention or intervention therapies, one could choose to maximise the PPV by requiring that mice achieve one of the stated prediction criteria by 15 weeks of age, thereby excluding those animals that have single readings of >0.50% tetramer positivity after 15 weeks of age. This strategy results in slightly lower sensitivity (91%), but with an increased specificity of 80% and a PPV and NPV of 91 and 80%, respectively. Depending on the sensitivity, specificity or predictive values that best suit a given experimental design, one can choose the appropriate prediction criteria, alone or in combination (Table 1).
These data confirm the importance of IGRP206 – 214-reactive CD8+ T cells for development of spontaneous diabetes in the NOD mouse, and as a powerful determinant of diabetes development. Despite recent data demonstrating that prediabetic NOD mice exhibit unique patterns of CD8+ T cell specificities within pancreatic islet infiltrates at different times throughout the natural history of disease [4], these data indicate that, in mice going on to develop diabetes, the contribution of IGRP-reactive T cells is sufficient to justify using this population alone as a reliable disease predictor. It is possible that quantification of other beta-cell-reactive CD8+ T cell populations in the circulation may also be sufficient or may further enhance the predictive power of this approach.
Recurrent autoimmunity is an important contributor to graft failure in human recipients of islets from partially matched HLA donors, as suggested by studies showing that mismatched grafts subject only to allogeneic rejection experience better outcomes [15, 16]. The ability to predict and prevent recurrent autoimmunity is also relevant if autologous stem cells [17] or regenerated endogenous beta cells [18, 19] are used. However, despite the importance of the IGRP-specific CD8+ T cell subset for islet pathogenicity, prediction of recurrent autoimmune islet graft failure was not possible based on detection of IGRP-reactive CD8+ T cells in the peripheral blood. Instead, large proportions (up to 51%) of IGRP-specific CD8+ T cells were detected in rejected NODscid-derived islet grafts, consistent with recent findings [20]. These data are surprising because IGRP-specific CD8+ T cells constituted a large proportion of the T cells within the graft itself. They are also unexpected because other investigators have shown the presence of insulin-reactive cells in the peripheral blood of human transplant recipients undergoing recurrent autoimmunity [13]. These differences may be due to the epitope that was studied (IGRP in mice vs insulin B10–18 in humans) or may reflect pathophysiological differences between animal models and humans, such as the relatively compressed kinetics of autoimmune rejection in NOD mice. In mice, the rapid development of post-transplant autoimmunity may have precluded detection in peripheral blood, as we were unable to sample cells at all early time points. The differences between the animal model and humans may also reflect the massive immunodominance of IGRP as an islet epitope in mice and the consequently larger pool of IGRP-reactive memory cells that may render peripheral blood trafficking unnecessary.
As mentioned above, during the development of spontaneous diabetes, unique autoreactive CD8+ T cell subsets predominate at different points in time [4]. Our data were generated for single time points, and therefore it remains unclear whether a particular T cell subset predominates throughout the natural history of the spontaneous disease process in a single animal, or whether different T cell specificities predominate at different times. Our findings suggest that the IGRP206 – 214-reactive T cell subset that is probably immunodominant during the spontaneous disease process is also likely to be immunodominant during recurrent autoimmune rejection. If true, this T cell population may be a useful target for testing therapeutic interventions post-transplantation. The IGRP-reactive CD8+ T cell populations recovered from the islet grafts were often of strikingly high fluorescence intensity (as compared with the staining intensity obtained from islet-associated T cells during the earlier stages of spontaneous diabetes), suggesting that these cells represent a high-avidity population that may have been selected from a mixed population of low- and high-avidity T cells during the spontaneous disease process [21].
The paucity of IGRP-reactive T cells in the peripheral blood during recurrent autoimmunity also suggests that memory IGRP-reactive CD8+ T cells migrate to the transplantation site and proliferate in situ, bypassing the requirement for priming in local lymph nodes and subsequent trafficking through the peripheral blood. In support of this hypothesis, CD8+ T cells recovered from islet grafts were found to be CD62Llow, CD69med and CD44high (data not shown), suggesting an activated memory phenotype [22]. Alternatively, primed T cells may travel in the circulation, but do so in sufficiently small frequencies, very quickly or at different time points, such that we were unable to detect them.
The proliferation of IGRP206 – 214-reactive CD8+ T cells in islet grafts from BALB/C donors, despite the MHC class II mismatch, could be explained by the presentation of this epitope by H2-Kd MHC class I molecules on BALB/C beta cells with subsequent recognition by this CD8+ T cell subset. It is therefore plausible that in this partial mismatch islet allograft, autoreactive CD8+ T cells contribute to graft rejection, and indeed the same may be true in human islet allografts in type 1 diabetes, in which donor and recipient are matched at an HLA-class I allele. More surprising is our finding that expansion of IGRP206 – 214-reactive CD8+ also occurs in islet allografts derived from C57BL/6 donors, which are mismatched at both MHC class I and II loci. This finding suggests either that some T cell proliferation occurs via bystander activation of resident T cells [23] within the islet graft following transplantation, or that IGRP-reactive T cells proliferate following presentation of donor (C57BL/6) beta cell antigen by recipient (NOD) antigen-presenting cells that have invaded the graft. The latter possibility would point to a role for the direct pathway of graft antigen presentation in proliferation of autoreactive T cells.
Our inability to predict impending islet graft failure in syngeneic models via the expansion of autoreactive CD8+ T cells in the peripheral circulation was disappointing, but encouraging results have been shown in humans with the use of the insulin B10–18 epitope [13]. The recent description of other immunodominant HLA class I beta cell epitopes may also improve the peripheral blood detection of autoreactive cells in humans prior to islet graft rejection. Detection of autoreactive T cells in the circulation may be simpler in humans, where rejection is slower and recurrent autoimmunity is only part of the equation. The dissimilarity in findings also highlights possible important differences between the NOD mouse model and human disease. Interestingly, Han and colleagues were able to predict graft rejection following transplant of islet allografts based on an increase in granzyme B mRNA levels in peripheral blood (a marker of cytotoxic CD8+ T lymphocyte and natural killer cell activity), along with other clinical correlates. This suggests that other blood-based predictive tests may be feasible in humans [24].
Abbreviations
- CTL:
-
cytotoxic T lymphocytes
- IGRP:
-
islet-specific glucose-6-phosphatase catalytic subunit-related protein
- NOD:
-
non-obese diabetic
- NPV:
-
negative predictive value
- PPV:
-
positive predictive value
References
Liblau RS, Wong FS, Mars LT, Santamaria P (2002) Autoreactive CD8 T cells in organ-specific autoimmunity. Emerging targets for therapeutic intervention. Immunity 17:1–6
Wong FS, Karttunen J, Dumont C et al (1999) Identification of an MHC class I-restricted autoantigen in type 1 diabetes by screening an organ-specific cDNA library. Nat Med 5:1026–1031
Lieberman SM, Evans AM, Han B et al (2003) Identification of the beta cell antigen targeted by a prevalent population of pathogenic CD8+T cells in autoimmune diabetes. Proc Natl Acad Sci USA 100:8384–8388
Lieberman SM, Takaki T, Han B, Santamaria P, Serreze DV, DiLorenzo TP (2004) Individual nonobese diabetic mice exhibit unique patterns of CD8+T cell reactivity to three islet antigens, including the newly identified widely expressed dystrophia myotonica kinase. J Immunol 173:6727–6734
Trudeau JD, Kelly-Smith C, Verchere CB et al (2003) Prediction of spontaneous autoimmune diabetes in NOD mice by quantification of autoreactive T cells in peripheral blood. J Clin Invest 111:217–223
Weir GC, Bonner-Weir S (1997) Scientific and political impediments to successful islet transplantation. Diabetes 46:1247–1256
Shapiro AM, Lakey JR, Ryan EA et al (2000) Islet transplantation in seven patients with type 1 diabetes mellitus using a glucocorticoid-free immunosuppressive regimen. N Engl J Med 343:230–238
Ryan EA, Paty BW, Senior PA et al (2005) Five-year follow-up after clinical islet transplantation. Diabetes 54:2060–2069
Coulombe M, Gill RG (2004) The immunobiology of pancreatic islet transplantation. Adv Exp Med Biol 552:154–169
Amrani A, Serra P, Yamanouchi J et al (2001) Expansion of the antigenic repertoire of a single T cell receptor upon T cell activation. J Immunol 167:655–666
Lieberman SM, DiLorenzo TP (2003) A comprehensive guide to antibody and T-cell responses in type 1 diabetes. Tissue Antigens 62:359–377
Panagiotopoulos C, Trudeau JD, Tan R (2004) T-cell epitopes in type 1 diabetes. Curr Diab Rep 4:87–94
Pinkse GG, Tysma OH, Bergen CA et al (2005) Autoreactive CD8 T cells associated with beta cell destruction in type 1 diabetes. Proc Natl Acad Sci USA 102:18425–18430
Diabetes Prevention Trial-Type 1 Diabetes Study Group (2002) Effects of insulin in relatives of patients with type 1 diabetes mellitus. N Engl J Med 346:1685–1691
Hering BJ (1996) Insulin independence following islet transplantation in man a comparison of different recipient categories. Intern Islet Transpl Registry 6:5–19
Roep BO (2003) The role of T-cells in the pathogenesis of type 1 diabetes: from cause to cure. Diabetologia 46:305–321
Peck AB, Cornelius JG, Chaudhari M, Shatz D, Ramiya VK (2002) Use of in vitro-generated, stem cell-derived islets to cure type 1 diabetes: how close are we? Ann N Y Acad Sci 958:59–68
Ryu S, Kodama S, Ryu K, Schoenfeld DA, Faustman DL (2001) Reversal of established autoimmune diabetes by restoration of endogenous beta cell function. J Clin Invest 108:63–72
Kodama S, Kuhtreiber W, Fujimura S, Dale EA, Faustman DL (2003) Islet regeneration during the reversal of autoimmune diabetes in NOD mice. Science 302:1223–1227
Wong CP, Li L, Frelinger JA, Tisch R (2006) Early autoimmune destruction of islet grafts is associated with a restricted repertoire of IGRP-specific CD8+T cells in diabetic nonobese diabetic mice. J Immunol 176:1637–1644
Han B, Serra P, Yamanouchi J et al (2005) Developmental control of CD8 T cell-avidity maturation in autoimmune diabetes. J Clin Invest 115:1879–1887
Sprent J, Surh CD (2002) T cell memory. Annu Rev Immunol 20:551–579
Horwitz MS, Bradley LM, Harbertson J, Krahl T, Lee J, Sarvetnick N (1998) Diabetes induced by Coxsackie virus: initiation by bystander damage and not molecular mimicry. Nat Med 4:781–785
Han D, Xu X, Baidal D et al (2004) Assessment of cytotoxic lymphocyte gene expression in the peripheral blood of human islet allograft recipients: elevation precedes clinical evidence of rejection. Diabetes 53:2281–2290
Acknowledgements
J. D. Trudeau was supported by a studentship from the Michael Smith Foundation for Health Research (MSFHR). This work was supported by grants from the Canadian Institutes of Health Research to R. Tan (no. 19839) and C. B. Verchere (no. 64427), the Canadian Diabetes Association (to R. Tan) and a Childhood Diabetes Research Unit infrastructure award from the MSFHR. R. Tan and B. Verchere are MSFHR Senior Scholars.
Duality of interest
There is no duality of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Trudeau, J.D., Chandler, T., Soukhatcheva, G. et al. Prospective prediction of spontaneous but not recurrent autoimmune diabetes in the non-obese diabetic mouse. Diabetologia 50, 1015–1023 (2007). https://doi.org/10.1007/s00125-007-0600-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-007-0600-9