Abstract
Aims/hypothesis
Secreted by adipocytes, adiponectin is a hormone that acts as an antidiabetic and anti-atherogenic adipokine. We recently cloned the genes encoding two adiponectin receptors (ADIPOR1 and ADIPOR2). The aim of this study was to examine whether ADIPOR1 and/or ADIPOR2 play a major role in genetic susceptibility to insulin resistance or type 2 diabetes in the Japanese population.
Methods
By direct sequencing and a search of public databases, we identified single nucleotide polymorphisms (SNPs) in ADIPOR1 and ADIPOR2, and investigated whether these SNPs are associated with insulin resistance and type 2 diabetes in the Japanese population.
Results
The linkage disequilibrium (LD) in the chromosomal region of ADIPOR1 was almost completely preserved, whereas the LD in ADIPOR2 was less well preserved. None of the SNPs in ADIPOR1 or ADIPOR2 were significantly associated with insulin resistance or type 2 diabetes. No differences in ADIPOR1 or ADIPOR2 haplotype frequencies were observed between type 2 diabetic and non-diabetic subjects.
Conclusions/interpretation
Genetic variations in ADIPOR1 or ADIPOR2 are unlikely to lead to a common genetic predisposition to insulin resistance or type 2 diabetes in the Japanese population.
Similar content being viewed by others
Introduction
Adiponectin (also known as the 30-kDa adipocyte complement-related protein, or Acrp30) [1–4] is a hormone secreted by adipocytes that acts as an antidiabetic adipokine [5–9]. Levels of adiponectin in the blood are decreased in subjects with obesity, insulin resistance or type 2 diabetes [10, 11]. In animal models, decreased plasma adiponectin is causally involved in insulin resistance and glucose intolerance [6–9]. In humans, polymorphisms in the gene encoding adiponectin have been shown to be associated with insulin resistance and type 2 diabetes [12–14].
We recently cloned cDNAs encoding adiponectin receptors 1 and 2 (ADIPOR1 and ADIPOR2) [15]. These receptors mediate increases in the AMP kinase [16] and peroxisome proliferator-activated receptor-α ligand activities [17] of adiponectin [15], and are likely to mediate the insulin-sensitising actions of adiponectin. Therefore, ADIPOR1 and ADIPOR2 may be viewed as plausible candidate genes for susceptibility to insulin resistance and type 2 diabetes.
The aim of this study was to investigate whether single nucleotide polymorphisms (SNPs) in ADIPOR1 and ADIPOR2 influence insulin resistance and susceptibility to type 2 diabetes in the Japanese population.
Subjects and methods
Subjects
The inclusion criteria for the diabetic and non-diabetic subjects enrolled in this study have been described previously [13]. Diabetes was diagnosed according to the criteria of the World Health Organization [18]. All subjects enrolled in this study were of full Japanese ancestry. SNPs in ADIPOR1 and ADIPOR2 were genotyped in 192 diabetic and 192 non-diabetic subjects. The clinical characteristics of the subjects are described in Table 1 of the electronic supplementary material (ESM). Written informed consent was obtained from the subjects, and the study was approved by the Ethics Committee of the University of Tokyo.
Biological measurements
Insulin resistance and beta cell function were assessed using homeostasis model assessment (HOMA). The HOMA of insulin resistance (HOMA-IR) was calculated as fasting insulin (μU/ml)×glucose (mmol/l)/22.5, as described elsewhere [19]. Data are expressed as means±SEM. Since the use of insulin therapy or oral hypoglycaemic agents in subjects with type 2 diabetes is likely to interfere with insulin levels, the correlations between SNPs and insulin resistance were only assessed in non-diabetic subjects.
Screening and selection of SNPs in ADIPOR1 and ADIPOR2
To establish an SNP map encompassing ADIPOR1 and ADIPOR2, SNPs were identified by direct sequencing and a search of public databases. All eight exons in ADIPOR1 and all nine exons in ADIPOR2, plus 50–100 bases of the 5′ and 3′ intronic regions flanking the exons, were amplified and directly sequenced in 30 type 2 diabetic subjects. The conditions and the sequences of the primers used in the PCR are described in Table 2 of the ESM. The SNPs were identified based on the sequences reported in the GenBank database (http://www.ncbi.nih.gov/index.html), which contains ADIPOR1 (accession number NT_004671) and ADIPOR2 (accession number NT_009759). From the public database, 14 SNPs in ADIPOR1 (rs6666089, rs10920534, rs12039275, rs12733285, rs1539355, rs2275738, rs2275737, rs2275735, rs1342387, rs3737884, rs2275736, rs11581, rs1043268, rs1043280) and 29 SNPs in ADIPOR2 (rs2058033, rs6489322, rs12579507, rs11061935, rs7975600, rs10773982, rs11829703, rs12810020, rs11061947, rs11612383, rs11612726, rs9888418, rs7976827, rs12582624, rs10848566, rs7297509, rs12818963, rs10848569, rs11061974, rs2068485, rs7974924, rs12831353, rs12828908, rs10848571, rs7974422, rs2286385, rs730032, rs12342, rs1044471) were selected and validated in 30 type 2 diabetic subjects. From the database, we chose SNPs with a minor allele frequency higher than 10%; we excluded those SNPs for which information on allele frequency was not presented. In total, 25 SNPs in ADIPOR1 and 41 SNPs in ADIPOR2 were identified. Minor allele frequency was determined and Hardy–Weinberg equilibrium was assessed. We eliminated SNPs that deviated from Hardy–Weinberg equilibrium or that had a minor allele frequency lower than 10% from further study. In total, 14 SNPs in ADIPOR1 and 24 SNPs in ADIPOR2 were analysed, resulting in an average SNP density of one SNP per 1.2 kb in ADIPOR1 and one SNP per 3.9 kb in ADIPOR2.
Genotyping of SNPs used in the association study
We genotyped the SNPs in ADIPOR1 and ADIPOR2 in type 2 diabetic subjects and non-diabetic subjects using direct sequencing. PCR was performed under standard conditions. Sequencing reactions were performed using the BigDye terminator kit (Applied Biosystems, Foster City, CA, USA), and the products were resolved using an ABI 3700 automated DNA sequencer (Applied Biosystems). The results were integrated using a Sequencher (Gene Codes Corporation, Ann Arbor, MI, USA), and individual SNPs were manually genotyped. Ambiguous base assignments were eliminated from further analysis.
Statistical analysis
The proportions of genotypes or alleles between subjects with or without type 2 diabetes were compared using a chi square (χ 2) test. The differences between subjects with different SNP genotypes were statistically tested using an ANOVA. A Bonferroni adjustment was used to avoid type 1 errors caused by multiple testing. The level of significance for SNPs in ADIPOR1 and ADIPOR2 was 0.001 (0.05 divided by 38, the total number of SNPs for which the association between SNPs and type 2 diabetes was investigated in the present study). We further genotyped SNP15 in ADIPOR2, which showed a tendency towards an association with HOMA (p=0.04), in a second panel to test reproducibility. The statistical analyses, except for those for haplotype estimation, were performed using JUMP for Windows, version 4.00 (SAS Institute, Cary, NC, USA).
Haplotype analysis
Tagged SNPs were selected for haplotype analysis using HaploBlockFinder software (http://www.cgi.uc.edu/cgi-bin/kzhang/haploBlockFinder.cgi, last accessed in April 2005). The tagged SNPs consisted of a minimal set of SNPs that were uniquely distinguishable from at least 90% of the common haplotypes. After selecting the tagged SNPs, the frequency of each haplotype was estimated and differences in haplotype frequencies between non-diabetic and diabetic subjects were assessed using a piece of software based on the Expectation Maximisation algorithm (SNPAlyze; Dynacom, Tokyo, Japan). The differences in the haplotype frequencies were then analysed using the chi square test and the permutation test.
Results
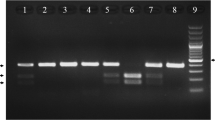
We identified a total of 25 SNPs in ADIPOR1 (Fig. 1a) and 41 SNPs in ADIPOR2 (Fig. 1b). All of the SNPs that were identified had genotype frequencies that were in Hardy–Weinberg equilibrium in non-diabetic and type 2 diabetic subjects (p>0.05). Among these, SNPs with a minor allele frequency higher than 10% were investigated for linkage disequilibrium (LD) in ADIPOR1 and ADIPOR2, and then association with type 2 diabetes and insulin resistance was evaluated. We estimated the degree of LD between pairs of SNPs using an absolute value of D′ (|D′|). For ADIPOR1, the LD extended over 20 kb of the chromosomal region and covered one haplotype block (Fig. 2a). In contrast, the LD in the chromosomal region was less preserved for ADIPOR2 and was split into three haplotype blocks (Fig. 2b). No differences were observed between the diabetic and non-diabetic subjects in terms of the distribution of the genotypes or alleles of the SNPs in ADIPOR1 (Table 1) and ADIPOR2 (Table 2). Only one nominal association was found; this was between SNP15 in ADIPOR2 and HOMA-IR (11/12/22: 1.27±0.05/1.35±0.08/1.81±0.21, p=0.04) (see Tables 3 and 4 of the ESM). When a Bonferroni adjustment was performed (adopted to avoid type 1 errors caused by multiple testing; threshold of significance, p=0.001), no association was found between HOMA-IR and SNP15 in ADIPOR2. Moreover, when SNP15 in ADIPOR2 was further genotyped in 384 additional type 2 diabetic subjects and 384 additional non-diabetic subjects (second panel) to avoid type 2 errors, no significant differences were observed in the HOMA results when compared according to SNP15 genotype (11/12/22: 1.66±0.09/1.62±0.07/1.67±0.13, p=0.91). There were no differences in clinical parameters, such as sex, age, BMI, HbA1c and fasting glucose, between the genotypes of any of the SNPs investigated in the present study (data not shown). We then performed a haplotype analysis, which may be a more sensitive method for detecting associations than the assessment of individual SNPs. First, the haplotype blocks in ADIPOR1 and ADIPOR2 were determined. The tagged SNPs that represented more than 90% of the haplotypes in each block were then selected, and the difference in the frequency of each haplotype between the type 2 diabetic subjects and the non-diabetic subjects was analysed. As shown in Table 3, none of the haplotypes in ADIPOR1 or ADIPOR2 were associated with type 2 diabetes.
Genomic structure of ADIPOR1 (a) and ADIPOR2 (b) and the locations of the SNPs genotyped in the present study. Exons are shown as boxes, and introns and flanking sequences as lines connecting the boxes. Coding sequences are represented as closed boxes, and untranslated regions as open boxes. The SNPs are numbered in order of appearance from the 5′ to 3′ ends of the genes
Discussion
After constructing a dense map of SNPs in ADIPOR1 and ADIPOR2 and performing haplotype analysis, no evidence of a major role for ADIPOR1 or ADIPOR2 in susceptibility to type 2 diabetes or insulin resistance was found in a Japanese population. Our results may reflect a type 2 error (false-negative result), but this is unlikely. First, SNP densities of one SNP every 1.2 kb in ADIPOR1 and one SNP every 3.9 kb in ADIPOR2 were used for the association study. The distance between each SNP was short, and the LD between them was fully analysed. We estimated that more than 90% of the haplotypes in ADIPOR1 and ADIPOR2 were covered. Second, the sample size used in the present study had an 80% power to detect the effect of a polymorphism, conferring an odds ratio of 2.0 at a significance level of 5% (assuming an allele frequency of 40% in the control population). However, it cannot be excluded that SNPs in ADIPOR1 and/or ADIPOR2 had a minor effect on susceptibility to type 2 diabetes.
Consistent with our results for ADPOR1, an American study recently reported that SNPs in ADIPOR1 were not associated with type 2 diabetes in Caucasians or African Americans [20]. However, they reported that the level of expression of ADIPOR1 in lymphocytes from type 2 diabetic subjects was reduced compared with that in lymphocytes from non-diabetic subjects, implicating ADIPOR1 in the pathogenesis of type 2 diabetes. Further analysis is needed to clarify the role played by ADIPOR2 in susceptibility to type 2 diabetes in different ethnic groups.
In summary, the genetic variations in ADIPOR1 or ADIPOR2 investigated in the present study were not associated with insulin resistance or type 2 diabetes. However, further studies using denser SNPs and larger samples may be required to conclusively determine that genetic variations in ADIPOR1 or ADIPOR2 are not major genetic determinants of the development of type 2 diabetes or insulin resistance.
Abbreviations
- LD:
-
linkage disequilibrium
- ESM:
-
electronic supplementary material
- HOMA:
-
homeostasis model assessment
- SNP:
-
single nucleotide polymorphism
References
Scherer PE, Williams S, Fogliano M et al (1995) Novel serum protein similar to C1q, produced exclusively in adipocytes. J Biol Chem 270:26746–26749
Hu E, Liang P, Spiegelman BM (1996) AdipoQ is a novel adipose-specific gene dysregulated in obesity. J Biol Chem 271:10697–10703
Maeda K, Okubo K, Shimomura I et al (1996) cDNA cloning and expression of a novel adipose specific collagen-like factor, apM1 (AdiPose most abundant gene transcript 1). Biochem Biophys Res Commun 221:286–296
Nakano Y, Tobe T, Choi-Miura NH et al (1996) Isolation and characterization of GBP28, a novel gelatin-binding protein purified from human plasma. J Biochem (Tokyo) 120:802–812
Fruebis J, Fruebis J, Tsao TS et al (2001) Proteolytic cleavage product of 30-kDa adipocyte complement-related protein increases fatty acid oxidation in muscle and causes weight loss in mice. Proc Natl Acad Sci U S A 98:2005–2010
Yamauchi T, Kamon J, Waki H et al (2001) The fat-derived hormone adiponectin reverses insulin resistance associated with both lipoatrophy and obesity. Nature Med 7:941–946
Berg AH, Combs TP, Du X et al (2001) The adipocyte-secreted protein Acrp30 enhances hepatic insulin action. Nat Med 7:947–953
Kubota N, Kubota N, Terauchi Y et al (2002) Disruption of adiponectin causes insulin resistance and neointimal formation. J Biol Chem 277:25863–25866
Maeda N, Maeda N, Shimomura I et al (2002) Diet-induced insulin resistance in mice lacking adiponectin/ACRP30. Nat Med 8:731–737
Arita Y, Kihara S, Ouchi N et al (1999) Paradoxical decrease of an adipose-specific protein, adiponectin, in obesity. Biochem Biophys Res Commun 257:79–83
Hotta K, Funahashi T, Arita Y et al (2000) Plasma concentrations of a novel, adipose-specific protein, adiponectin, in type 2 diabetic patients. Arterioscler Thromb Vasc Biol 20:1595–1599
Hara K, Boutin P, Mori Y et al (2002) Genetic variation in the gene encoding adiponectin is associated with increased risk of type 2 diabetes in the Japanese population. Diabetes 51:536–540
Vasseur F, Helbecque N, Dina C et al (2002) Single-nucleotide polymorphism haplotypes in the both proximal promoter and exon 3 of the APM1 gene modulate adipocyte-secreted adiponectin hormone levels and contribute to the genetic risk for type 2 diabetes in French Caucasians. Hum Mol Genet 11:2607–2614
Menzaghi C, Ercolino T, Di Paola R et al (2002) A haplotype at the adiponectin locus is associated with obesity and other features of the insulin resistance syndrome. Diabetes 51:2306–2312
Yamauchi T, Kamon J, Ito Y et al (2003) Cloning of adiponectin receptors that mediate antidiabetic metabolic effects. Nature 423:762–769
Yamauchi T, Yamauchi T, Kamon J et al (2002) Adiponectin stimulates glucose utilization and fatty-acid oxidation by activating AMP-activated protein kinase. Nat Med 8:1288–1295
Yamauchi T, Kamon J, Waki H et al (2003) Globular adiponectin protected ob/ob mice from diabetes and apoE deficient mice from atherosclerosis. J Biol Chem 278:2461–2468
Alberti KG, Zimmet PZ (1998) Definition, diagnosis and classification of diabetes mellitus and its complications: part 1. Diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet Med 15:539–553
Matthews DR, Hosker JP, Rudenski AS et al (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
Wang H, Zhang H, Jia Y et al (2004) Adiponectin receptor 1 gene (ADIPOR1) as a candidate for type 2 diabetes and insulin resistance. Diabetes 53:2132–2136
Acknowledgements
K. Hara and M. Horikoshi contributed equally to this study. This work was supported by a grant-in-aid (to T. Kadowaki) from the Organization for Pharmaceutical Safety and Research (Tokyo, Japan), and a grant-in-aid (to R. Nagai) for The 21st Century Center of Excellence Program from the Ministry of Education, Culture, Science, Sports and Technology of Japan. We thank Y. Okada for technical assistance.
Author information
Authors and Affiliations
Corresponding author
Electronic Supplementary Material
Rights and permissions
About this article
Cite this article
Hara, K., Horikoshi, M., Kitazato, H. et al. Absence of an association between the polymorphisms in the genes encoding adiponectin receptors and type 2 diabetes. Diabetologia 48, 1307–1314 (2005). https://doi.org/10.1007/s00125-005-1806-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-005-1806-3