Abstract
Regulation of glycaemia represents a fundamental biological principle, and its failure underlies Type 2 diabetes. The complex aetiology of Type 2 diabetes, which probably involves a medley of molecular mechanisms, requires dissection out of diabetes-associated subphenotypes, such as the non-obese with increased liver fat or the obese with low plasma adiponectin. The concepts of the hyperbolic relationship of insulin secretion and insulin sensitivity with glucose allostasis help us to establish the pathophysiological framework within which such mechanisms must operate. The translation of burgeoning new basic science findings into a physiological and clinical context calls for novel and imaginative clinical experimental tools. For the purpose of this review, four molecules (adiponectin [APM1], stearoyl CoA desaturase-1 [SCD1], insulin receptor substrate-1 [IRS1], peroxisome proliferator-activated receptor-γ [PPARG]), each with a plausible role in the disease process, have been selected to illustrate the use of such techniques in humans. These include procedures as diverse as isotope dilution for turnover studies (e.g. glycerol turnover as a proxy for lipolysis), conventional and modified clamp procedures, association studies of functionally relevant single nucleotide polymorphisms in candidate genes (e.g. IRS-1 and PPARγ), multivariate correlational analyses (as with plasma adiponectin), magnetic resonance spectroscopy to quantify intra-tissue lipid deposition and regional fat distribution, and gas chromatography to determine fatty acid patterns in selected lipid fractions as proxy for intrahepatic enzyme activity. A concerted effort by scientists from many disciplines (genetics and cell biology, physiology and epidemiology) will be required to bridge the growing gap between basic scientific concepts of biological modifiers of glycaemia and concepts that are truly relevant for human Type 2 diabetes.
Similar content being viewed by others
Introduction
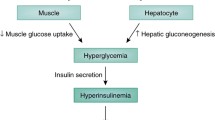
The regulation of glucose levels is a fundamental biological process that becomes deranged in diabetes mellitus, a condition that affects millions of people around the world [1] and, via its associated complications, imposes enormous strain on health care systems [2]. Some 90% of affected individuals have Type 2 diabetes mellitus, and within this category no more than 10% can be accounted for by monogenic forms such as maturity-onset diabetes of the young [3], by mitochondrial diabetes [4], or by late-onset autoimmune diabetes [5]. The common form of Type 2 diabetes is, in itself, likely to represent a melting pot of disease entities that differ in terms of aetiology and pathogenesis. By definition, whatever the primary aetiology, all of these mechanisms culminate in the inability to regulate hyperglycaemia.
Traditionally, little effort has been made to distinguish between one person with Type 2 diabetes and another, except perhaps for the distinction between the lean and the obese. Our knowledge about the pathogenesis of this condition has, however, advanced to a stage where pathophysiological substratification into categories such as beta cell dysfunction, increased endogenous glucose production or impaired insulin-stimulated glycogen storage has become possible. Having said this, such characterisation is virtually impossible after the onset of overt hyperglycaemia and associated metabolic derangements, because hyperglycaemia can, in itself, induce all of these abnormalities. Nevertheless, an understanding of the molecular mechanisms underlying the loss of normoglycaemia will form the essential basis for our ultimate success in predicting, preventing and treating Type 2 diabetes. This requires us to have a clear idea about the general principles of control of glycaemia in humans, especially in the pre-diabetic state.
This review will identify the principal physiological constraints within which any mechanism affecting glycaemia must operate. The aim will be to provide a framework within which the flow of new knowledge from disciplines ranging from genetics and cell biology to physiology and epidemiology can be channelled into the identification of molecules truly relevant for human Type 2 diabetes. Within this framework each and every advance in basic science will need to be scrutinised carefully before its relevance for human disease can be accepted.
The hyperbolic law of glycaemia
Normoglycaemia is maintained by the balanced interplay between insulin action and insulin secretion. This prevents not only the development of hyperglycaemia (Type 2 diabetes) but also of hypoglycaemia. In humans with normal glucose tolerance, a decrease in insulin action is accompanied by up-regulation of insulin secretion (and vice versa). Figure 1 illustrates the curvilinear relationship between beta cell function and insulin sensitivity in subjects with normal glucose tolerance. It is thought to indicate beta cell compensation for insulin resistance [4, 5, 6, 7]. Mathematically, this relationship is best approximated by a hyperbolic function, with the product of beta cell function and insulin sensitivity being constant. This constant has been named the “disposition index” [7] and can be interpreted as a measure of the ability of the beta cells to compensate for insulin resistance. Deviation from the “hyperbola”, such as in the subjects with impaired glucose tolerance and Type 2 diabetes in Figure 1, occurs when beta cell function is inadequately low for a given degree of insulin sensitivity, i.e. with a decreasing disposition index.
“The hyperbolic law of glycaemia”. In subjects with NGT a quasi-hyperbolic relationship exists between beta cell function (estimated from the OGTT [85]) and insulin sensitivity (estimated from the OGTT [86]). With deteriorating glucose tolerance (IGT and Type 2 diabetes), deviation from this hyperbola occurs. In other words, as long as a decrease in insulin sensitivity over time (as a result of weight gain, for example) is accompanied by a compensatory increase in beta cell function, glucose tolerance is maintained. However, if in response to decreasing insulin sensitivity beta cell function remains unchanged or even decreases, glucose tolerance deteriorates. Grey squares, NGT (n=483); white circles, IGT (n=71); black diamonds, Type 2 diabetes (n=65)
While the hyperbola elegantly captures many previous observations, the physiological signal that stimulates this compensatory increase in beta cell function in response to decreasing insulin action remains unexplained, especially in subjects with perfectly normal glucose tolerance. Glucose is the pre-eminent insulin secretagogue, and if this were important as the signal linking insulin resistance to beta cell compensation, insulin secretion would probably not fully compensate for worsening insulin resistance, since this would remove the stimulus for the compensation. We therefore hypothesised that despite appropriate beta cell compensation (reflected by a constant disposition index), glycaemia, i.e. fasting or 2-hour glucose, would increase as insulin action decreases. This is in sharp contrast to what was widely believed, namely that the compensatory increase in beta cell function would keep glycaemia (glucose tolerance) constant. We used a mathematical separation of changes in disposition index and changes along the hyperbola, with disposition index remaining constant, to analyse cross-sectional, longitudinal and prospective data of Pima Indians and Caucasians with normal glucose tolerance [8]. When everything else is kept constant, especially the disposition index (i.e. appropriateness of beta cell compensation), a higher beta cell demand due to reduced insulin action was positively associated with glycaemia. Figure 2a shows the same inverse relationship as in Figure 1, just on a log-transformed scale and in a cohort of Pima Indians in whom beta cell function was truly measured by an intravenous glucose tolerance test. Introducing glycaemia on the z axis for the same set of data (Fig. 2b) illustrates an increase in glycaemia along the hyperbola which might not have been expected. We also studied a large cohort of subjects longitudinally (time of follow-up: 5–6 years) and made them “travel” exactly along the curve by mathematically accounting for any deviation from the curve. Interestingly enough, with increasing beta cell demand over time, i.e. upon travelling up and left, glycaemia also increased; in the extreme groups this increase was almost 0.6 mmol/l for fasting glucose and 2.2 mmol/l for 2-hour plasma glucose. Vice versa, with decreasing beta cell demand, i.e. upon travelling down and right, glycaemia decreased. Finally, the prospective analysis showed that for any given disposition index, subjects with initially higher beta cell demand were more likely to become “diabetic” than those with lower beta cell demand [8]. These results clearly demonstrate that despite normal beta cell compensation, glycaemia increases when insulin resistance is present. In other words, even with unlimited beta cell reserves, it is unhealthy to become insulin resistant.
a. Hyperbolic relationship (here linearised by log transformation) between the acute insulin response (AIR) from the IVGTT and insulin action (M) from the hyperinsulinaemic-euglycaemic clamp (413 Pima Indians with normal glucose tolerance). r=−0.28; p=0.0001 b. Superimposition of the 2-hour plasma glucose concentration in the cohort (qualitative representation from data in Stumvoll et al. [8]). In the x-y plain the linear least square regression line of the correlation between log M and log AIR of Figure 1a is shown again. The dotted line illustrates how glycaemia increases when M decreases, even if AIR increases (i.e. the projection of the regression line onto the mesh has a significant slope). The grey shaded area represents the 95% confidence band of the least square regression line. EMBS, effective metabolic body size
The concept of glucose allostasis
In 1988, Sterling and Eyer expanded the general concept of homeostasis [9] by introducing the term “allostasis” as an essential component of maintaining health in response to stress [10]. McEwen and others applied the concept of allostasis to help explain adaptive neuroendocrine responses to chronic stress, which ensure day-to-day survival but take a cumulative toll on the individual’s health [11, 12, 13].
Based on our observations and the presented concepts, we propose to make an analogous distinction between homeostasis and allostasis in the context of glucose metabolism. The widely used term, glucose homeostasis, describes a system that is essential for life and becomes operative when an acute and transient stressor (e.g. an oral glucose load) is introduced. In sequence, glucose levels rise, insulin secretion increases, glucose disposal is stimulated, and finally, glucose levels return to where they started. A chronic glucotoxic state is prevented. When the stressor is chronic, however, (i.e. insulin resistance due to obesity) beta cell function improves and insulin secretion increases, but this usually fails to bring glucose concentration back to where it was before insulin resistance was introduced. This increment may be minute, but over time it accumulates and takes its toll. Such a situation fulfils the original criteria for the term allostasis. Thus, with chronic insulin resistance, the regulatory process becomes allostatic while continuing to maintain homeostatic regulation during the next acute challenge. It appears that this higher glycaemia (among other signals like non-esterified fatty acids, sympathetic nerve activity or glucagon-like peptide-1) is necessary to keep the beta cell continuously informed that insulin resistance is present.
Though not appreciated in such terms, an allostatic increase in glycaemia despite normal beta cell regulation has been previously documented. In a longitudinal study in 60 children going through insulin resistance of puberty (from Tanner I to Tanner III), fasting glucose increased by an average of 0.2 mmol/l with each stage, a difference that was statistically significant [14]. It can be safely assumed that beta cell compensation at that age is as good as it gets. Thus, despite perfect compensation, the glucoregulatory system is not designed to maintain perfectly constant glycaemia as implied by the term glucose homeostasis. It follows logically that any mechanism that induces insulin resistance has the potential to lead ultimately to Type 2 diabetes.
Interindividual variability
Figure 1 teaches us one other important lesson. The variability along both axes is remarkable. Within one group, say the IGT group, the two-dimensional variability is so great that there is a large degree of overlap with the Type 2 diabetes group and the NGT group. Moreover, in contrast to what the hyperbola might suggest at any given degree of insulin sensitivity, beta cell function can vary enormously. It seems that a high number versus a low number ultimately determines whether an individual becomes diabetic or remains NGT. Thus, the obvious question is what endows one person with poor beta cell function and another person with good beta cell function? A similar notion can be obtained from Figure 3, which depicts the inverse, slightly curvilinear relationship between obesity and insulin sensitivity. Even within the NGT cohort the variability of insulin sensitivity at any given BMI is remarkable. Here, the analogous question is what makes one person develop insulin resistance in the presence of obesity while another does not?
Inverse, curvilinear relationship between obesity (quantitated by BMI) and insulin sensitivity (in arbitrary units [86]) across different stages of glucose tolerance. Grey squares, NGT (n=483); white circles, IGT (n=71); black diamonds, Type 2 diabetes (n=65)
A significant portion of this variability is accounted for by factors such as measurement error (due to the limited reproducibility of the in vivo procedure, for example) or incompleteness of the artificial experimental condition to quantify every biologically important nuance of the parameter of interest. For example, how precisely can a euglycaemic-hyperinsulinaemic clamp at insulin concentrations of ~400 pmol/l assess insulin sensitivity of glucose uptake at say 100 pmol/l, or insulin sensitivity of the vessel wall to vasodilate? The answer is probably not at all, and as with any experiment, the data obtained by such an in vivo procedure are only valid under the defined experimental conditions unless proven otherwise. In any case, measurement technique and understanding of the disease mechanism are inseparable.
A good example to show that the two go hand in hand is the issue of fat distribution. It has been well established that measuring the absolute or relative fat mass is insufficient to capture fat-related associations. With the advances of molecular tools (for expression studies, for example) and imaging techniques (CT scanning) it has become clear that regional differences have to be taken into consideration. Visceral adipose tissue is metabolically more detrimental than subcutaneous adipose tissue [15]. Further advancements in imaging techniques (magnetic resonance spectroscopy) shed light on the metabolic importance of fat (usually small quantities in absolute terms) at atypical sites such as intrahepatic [16] or intramyocellular lipids [17]. Thus, developing and advancing measurement techniques to the best possible level, and controlling for the measured parameter (either by matching or mathematically) should progressively reduce interindividual variability and help us to understand why one person develops diabetes and another does not. This concept must be taken all the way to the molecular level by comparing the genetic make up of one individual with that of another. Theoretically, measurement of as many relevant parameters as possible, including those that can be influenced (e.g. physical fitness due to regular exercise) and those that cannot be influenced (genetic factors), should permit near-perfect assessment of disease risk.
Genetic factors in control of glycaemia
The most compelling evidence for a genetic component of Type 2 diabetes is the excess concordance rate in monozygotic versus dizygotic twins. The heritability of abnormal glucose tolerance has been estimated as about 60% [18, 19]. Moreover, excess concordance rates in monozygotic versus dizygotic twins also suggest a contribution of genetic factors to insulin resistance and beta cell dysfunction [20]. There can be no doubt, therefore, that in the control of glycaemia and in the pathogenesis of Type 2 diabetes, genetic factors play a role. But what exactly is meant by genetic factors?
Approximately 35 000 genes, organised in 46 chromosomes, encode for an even greater number of proteins (due to alternate splicing and post-translational modification, for example), which regulate the structure and function of the human organism. What makes humans different from one another—not only in terms of eye colour but also in terms of disease susceptibility—is the presence or absence of genetic polymorphisms such as single nucleotide polymorphisms (SNPs). An SNP with biological significance is expected to alter the function (when located in an exon) or the expression (when located in the promotor region or in an intron) of the resulting protein. This could lead to a decrease or increase in activity of an enzyme, to altered signal transmission for signalling proteins, or to modified expression of dependent genes in the case of a transcription factor.
Among the 3 billion base pairs of the human genome there is a common site of variation every 300 base pairs. The crucial question is which of these SNPs accounts for the fact that one person develops diabetes, say with a given degree of obesity, while another does not? The enormous heterogeneity of the diabetic phenotype has impeded the identification of significant SNPs, and very few genetic variants have been identified to account for even a minor proportion of common Type 2 diabetes. The most widely used experimental techniques for dissecting complex traits in general are the candidate gene approach and genome-wide random mapping (linkage analysis).
The candidate gene approach targets naturally occuring variants in genes that encode for proteins critical for insulin secretion, insulin action or obesity. The variants or polymorphisms in these genes are subsequently examined for significant association with Type 2 diabetes. Ideally, evidence should also be available from in vitro experiments, demonstrating functional significance of a variant, such as impaired binding of a docking protein, altered catalytic activity, or reduced expression as a result of an amino acid exchange or of a promoter polymorphism in a transcription factor binding site. Classical historical examples include the insulin receptor as a candidate gene for insulin resistance and the beta-cell-specific potassium channel KIR6.2 as a candidate gene for beta cell dysfunction. More recent candidates (IRS1 and PPARG) will be discussed below.
The genome-wide random mapping approach, in contrast, is not based on assumptions about the biological involvement of any gene product. It locates genes through their genomic position alone and is based on the following rationale: family members who share a specific phenotype (e.g. Type 2 diabetes) will also share chromosomal regions surrounding the gene, which contribute to that phenotype in excess of what is expected by chance alone [21]. Allele sharing is assessed after typing several hundred polymorphic chromosomal markers across the genome. The first (and to date only) successful example of a positionally cloned “common Type 2 diabetes gene” is CAPN10 in the NIDDM1 region of chromosome 2 [22, 23]. This gene encodes for calpain-10, a cysteine protease that is ubiquitously expressed [24]. Although an association with insulin-stimulated glucose disposal was reported in Pima Indians [25], the biological role of this protein in the control of glycaemia is far from understood.
Successful identification of genes through association with Type 2 diabetes is, however, only the beginning. To take full advantage of a “diabetes gene” for prevention and therapy it is necessary to understand the mechanism by which it modifies disease risk or progression. This is the interface between basic and clinical science. The basic scientist develops the biological concept, according to which the gene or protein in question might affect relevant pathways. For example, peroxisome proliferator-activated receptor-γ (PPARγ) interferes with development of obesity and insulin resistance by regulating transcription of genes important in adipogenic differentiation and lipid metabolism. Can this concept become relevant for humans? The clinical scientist’s task is to devise an experimental approach to test a plausible hypothesis, for example whether variability in transcriptional activity of PPARγ affects the risk of developing obesity in humans. The presence of the Pro12Ala polymorphism, leading to proline–alanine exchange, alters transcriptional activity in vitro. Comparing carriers and non-carriers of this polymorphism provides one opportunity to test the above hypothesis.
In the following section I shall present human data obtained in vivo to illustrate the potential role of four proteins that have been implicated in pathways or mechanisms related to insulin secretion or insulin sensitivity and thus to control of glycaemia. This will serve as a platform to describe different clinical experimental approaches to questions such as those discussed above.
Selected molecules involved in control of glycaemia
Adiponectin (APM1)
The striking association between insulin resistance and obesity justifies the study of factors originating from adipose tissue that have insulin-sensitising or -desensitising effects. Conceivably, greater release of an insulin desensitising factor for a given fat mass should make an individual more insulin-resistant. Adipose tissue releases not only fatty acids but also peptide hormones (adipocytokines or adipokines) with distant sites of action, making it an endocrine organ. While the role of leptin appears to be most prominent in the context of lipoatrophy [26], and that of TNF-α is confined to rodents, or in humans is only detectable at a local but probably not systemic (i.e. circulating) level, the role of adiponectin as an endogenous insulin sensitiser is progressively emerging.
With a concentration of around 5 µg/ml in human plasma, adiponectin represents one of the most abundant circulating proteins. In cases of obesity, plasma adiponectin levels are significantly decreased [27, 28], and after weight reduction, levels increase [29]. Moreover, two independent nested case-control studies, one in Pima Indians and one in a German cohort, demonstrated that high plasma adiponectin concentrations predicted lower risk of developing Type 2 diabetes in the future, independently of any known covariate [30, 31].
In rodent models of insulin resistance, intravenous administration of recombinant adiponectin restored normal insulin sensitivity, and transgenic elevation of circulating adiponectin resulted in improved insulin sensitivity [32, 33]. In humans, plasma adiponectin concentrations are negatively associated with obesity (Fig. 4a). On the other hand, plasma adiponectin concentrations are positively correlated with insulin sensitivity independently of measures of body fatness [27, 34] (Fig. 4a), which is compatible with a direct insulin-sensitising effect of this adipokine. Animal data have also suggested that this may occur primarily in the liver [35], although effects on muscle have been reported [32]. In the Pima Indians, higher plasma adiponectin concentrations were associated with greater insulin suppression of endogenous glucose production independently of age, sex, percentage body fat and insulin-stimulated glucose disposal [36]. Consistent with the suggestion of an effect on the liver, high plasma HDL cholesterol concentrations (an indicator of hepatic insulin sensitivity) were independently correlated with high plasma adiponectin concentrations in non-diabetic humans [34].
a. Inverse relationship between % body fat and plasma adiponectin concentrations after adjustment for age and sex. r=−0.28; p<0.0001 b. Positive relationship between plasma adiponectin concentrations and insulin sensitivity (µmol·kg−1·min−1·\( {\left[ {{\text{pmol}} \cdot {\text{l}}^{{ - 1}} } \right]}^{{ - 1}} \) , measured by euglycaemic-hyperinsulinaemic clamp) after adjustment for age, sex and % body fat (modified from Tschritter et al. [34]). r=−0.28; p<0.0001
In conclusion, variability in adiponectin release may contribute to the variation in insulin sensitivity for any given degree of adiposity. It is still unclear what influences the variability in adiponectin release independently of the determinants such as age, sex and percentage body fat. Although the data are not convincing, SNPs in the adiponectin (APM1) gene itself, such as the T-G polymorphism in exon 2 [37], or any of the host of proteins involved in the regulation of adiponectin production and degradation, could play a role. Nevertheless, the emerging role of adiponectin as an endogenous insulin sensitiser might lead to novel therapeutic modalities for Type 2 diabetes, conceivably also in a preventive context. Although recent observations of exophthalmos and increased interscapular fat pads in transgenic mice with elevated circulating adiponectin [33] have somewhat dampened earlier enthusiasm, cloning of the adiponectin receptor [38] might lead the way to safe and effective adiponectin analogues for human use.
Stearoyl-CoA desaturase (SCD1)
Human obesity involves accumulation of excess triglycerides not only at classical sites (subcutaneous, visceral) but also at intramuscular and intrahepatic locations. More so than intramyocellular lipids, intrahepatic lipids are associated with insulin resistance [16]. A step crucial for hepatic VLDL and triglyceride synthesis is the enzyme stearoyl-CoA desaturase-1 (SCD1), which catalyses the conversion of saturated fatty acids (palmitate and stearate) to monounsaturated fatty acids (palmitoleic and oleate). Ob/ob mice are characterised not only by excessive whole-body adiposity (as a result of hyperphagia) but also by a markedly increased hepatic triglyceride content. Interestingly, transgenic reduction of SCD1 activity almost completely prevented hepatic triglyceride accumulation in ob/ob mice [39].
We sought to develop a method to probe SCD1 activity non-invasively in humans in vivo. Oleate incorporated into secretory VLDL is the product of stearate desaturated by SCD1. The oleate:stearate ratio in VLDL particles, the main secretory triglyceride originating in the liver, should therefore semiquantitavely reflect intrahepatic SCD1 activity. Since plasma triglycerides are the predominant content of VLDL particles, we measured the oleate:stearate ratio in fatty acids contained in plasma triglycerides. Stearate (18:0) and oleate (18:1 ω9) relative to total fatty acids in plasma triglycerides were determined in 98 healthy individuals using gas chromatography and flame ionisation detection.
We found the oleate:stearate ratio in plasma triglycerides to be higher in women than in men (p=0.04), to be negatively correlated with age (r =−0.20, p=0.04) and to be positively correlated with percentage body fat (r=0.20, p=0.047). Interestingly, the oleate:stearate ratio in plasma triglycerides was inversely correlated with insulin sensitivity determined by hyperinsulinaemic-euglycaemic clamp (r=−0.27, p=0.008) (Fig. 5). This relationship remained significant (p=0.01) after adjustment for percentage body fat, age, sex, waist-to-hip ratio and plasma adiponectin concentrations.
SCD1 activity is regulated by nutritional factors (stimulated by saturated fatty acids and caloric oversupply, inhibited by polyunsaturated fatty acids) and probably genetic factors. Figure 6 shows an example where despite increased whole-body adiposity (subject A, Fig. 6a), intrahepatic lipids were reduced (subject A, Fig. 6c) compared with those in a control subject (subject B, Fig. 6b, d). Figure 6e suggests that the decreased liver fat content is causally related to the greater insulin sensitivity. It has been previously observed that the intrahepatic fat content is highly correlated with insulin suppression of endogenous glucose production [16]. It is thus possible that human insulin resistance and Type 2 diabetes due to caloric oversupply are mediated, at least partially, by the intrinsic activity of SCD1 and accumulation of intracellular, i.e. intrahepatic lipids. Hypothetically, down-regulated SCD1 activity in subject A may protect against insulin resistance despite caloric overload, and may help to explain the variability shown in Figure 3.
Comparison between an obese subject with low intrahepatic lipids (subject A) and a less obese subject with increased intrahepatic lipids (subject B). a, b. Magnetic resonance image with volume of interest for spectroscopic measurement. c, d. Magnetic resonance spectroscopy of intrahepatic lipids (quantitated against the water peak). Despite 20-fold magnification there is no detectable lipid peak (CH2)n in subject A. e. Placement of the two subjects (A and B) into the inverse linear relationship between liver fat and insulin sensitivity. Despite a greater % body fat, subject A is more insulin-sensitive. The position in the figure suggests that this may be related to the very intrahepatic lipids. r=−0.65; p=0.01
Insulin receptor substrate-1 (IRS1, Gly972Arg polymorphism)
IRS-1 is a classical insulin signalling molecule and therefore a prime candidate gene for insulin resistance. The Gly972Arg polymorphism in IRS-1 therefore represented a prime candidate for genetic causes of impaired insulin signalling. Over the years, however, conflicting data have accumulated [40, 41, 42, 43, 44, 45, 46] and this polymorphism has not held up to expectations as an insulin resistance gene. More recently, it was shown that insulin-secreting cells overexpressing the IRS-1 Gly972Arg variant had decreased sulphonylurea and glucose-stimulated insulin secretion compared with cells overexpressing the wild-type IRS-1 [47]. Moreover, cell apoptosis in isolated human islets obtained from organ donors heterozygous for Arg972 was increased two-fold compared with that of wild-type IRS-1 carriers [48], and the mature to immature insulin-containing granules were unfavourably affected by this polymorphism [49]. It was consequently suggested that this polymorphism might represent a genetic variant unifying insulin resistance and beta cell dysfunction.
We studied subjects with and without the polymorphism using a modified hyperglycaemic clamp method [50]. This consisted of a sequential and additive combination of square-wave hyperglycaemia (at 10 mmol/l glucose concentration), glucagon-like peptide-1 and arginine. To increase statistical power, we also analysed OGTTs of 212 subjects (31 with and 181 without the mutation), using a number of validated indices to estimate beta cell function from insulin (and C-peptide) concentrations obtained during an OGTT. During the modified hyperglycaemic clamp insulin secretion rates were significantly lower in Gly/Arg than in Gly/Gly during first-phase secretion and after maximal stimulation with arginine. During second-phase insulin secretion the differences reached statistical significance, while during the GLP-1 phases they were not significant. Several validated indices of beta cell function from the OGTT were significantly lower in X/Arg than in Gly/Gly (p values 0.002–0.05). Insulin sensitivity as determined by the euglycaemic-hyperinsulinaemic clamp was not different [48]. The most striking difference in absolute terms was seen during maximal stimulation with glucose plus GLP-1 plus arginine (5340±639 vs 9075±722 pmol/min), compatible with the finding of reduced mature granules in beta cells of arginine carriers [49]. Although no association with impaired beta cell function was observed in an older Dutch cohort [51], it is possible that the Gly972Arg polymorphism in IRS1 contributes to the variation in insulin secretion in people with normal glucose tolerance.
Peroxisome proliferator-activated receptor-γ (PPARG, Pro12Ala polymorphism)
The PPARγ is a transcription factor that belongs to the same family of nuclear receptors as steroid and thyroid hormone receptors [52]. It is activated by certain fatty acids, prostanoids and thiazolidinediones [53, 54, 55, 56] and promotes transcription of numerous target genes [57]. While the isoform PPARγ1 is expressed in most tissues, PPARγ2 is specific for adipose tissue, where it plays a key role in regulating adipogenic differentiation [58]. The PPARG gene is located on chromosome 3 [59], and the specific isoforms are a result of alternative mRNA splicing. The highly prevalent Pro12Ala polymorphism in PPARγ2 is the result of a CCA to GCA missense mutation in codon 12 of exon B of the PPARG gene. This exon encodes the N-terminal residue that defines the adipocyte-specific PPARγ2 isoform. The Pro12Ala polymorphism in PPARγ2 was first identified in 1997 [60] and studied as a plausible obesity candidate variant.
When16 candidate gene variants with previously published evidence for association with Type 2 diabetes (or related disorders) were tested using transmission disequilibrium testing (a powerful variant of association studies) in 333 Scandinavian parent–offspring trios with abnormal glucose tolerance, only the Pro12Ala polymorphism in the PPARγ2 gene was found to be significant [61]. An additional meta-analysis demonstrated a signficant risk reduction of 21% and a population-attributable risk of approximately 25% [61]. In other words, if the entire population carried the Ala allele, the prevalence for Type 2 diabetes would be 25% lower. In a recent prospective analysis (n>1000) from the Nurses’ Health Study, carriers of the Ala variant had 27% reduced risk of Type 2 diabetes compared with carriers of the Pro/Pro genotype [62]. This underlines the importance of alleles with weak individual effect but high population prevalence, such as the Pro/Pro wild type of PPARγ (75% prevalence in Caucasians).
The mechanism by which the Ala allele of the polymorphism protects from Type 2 diabetes probably involves improved insulin sensitivity [63, 64, 65]. It is worth noting that the heterozygous PPARγ knockout mouse is also more insulin-resistant. In subgroups with obesity, the difference in insulin sensitivity is more pronounced [66, 67], suggesting an interaction of the polymorphism with factors originating from adipose tissue. Most investigators observed lower fasting insulin concentrations in carriers of the Ala allele [64, 68, 69]. While this observation is generally compatible with the suggestion of greater insulin sensitivity, it could also indicate greater insulin clearance.
In a recent series of analyses from our laboratory we therefore addressed the question of whether carriers of the Pro12Ala polymorphism have greater insulin clearance than wild-type controls. We used insulin concentrations during the steady state of a standard euglycaemic-hyperinsulinaemic clamp produced by a constant insulin infusion based on kg body weight. We also used C-peptide:insulin ratio and insulin concentrations adjusted for C-peptide concentrations during an OGTT and a hyperglycaemic clamp, taking advantage of endogenous hyperinsulinaemia.
In all three datasets insulin clearance was significantly greater in carriers of the Ala allele compared with that in controls (Fig. 7a). Such differences in insulin clearance may be secondary to differences in (mainly hepatic) insulin sensitivity. The liver-specific mouse knockout model of the insulin receptor, a model of primary hepatic insulin resistance, is characterised by extreme hyperinsulinaemia as a result not only of hypersecretion but also of reduced or absent insulin clearance [70]. Interestingly, in Pima Indians insulin suppression of glucose production was 40% more efficient in carriers of the Ala allele, while insulin-stimulated glucose uptake was not different [68]. Collectively, these findings suggest that greater hepatic insulin sensitivity is pivotal for the mechanism of this polymorphism.
a. Insulin clearance (estimated from the molar ratio of C-peptide:insulin during an OGTT in subjects with and without the Pro12Ala polymorphism in PPARγ2; p=0.01) b. Suppression of NEFAs during a euglycaemic-hyperinsulinaemic clamp in subjects with and without the Pro12Ala polymorphism in PPARγ2 (modified from Tschritter et al. [83]); p=0.03
Since PPARγ2 is exclusively expressed in adipose tissue, a primary mechanism in this tissue with an immediate impact on hepatic insulin sensitivity and insulin clearance can be invoked. Increased NEFA delivery to the liver could induce hepatic insulin resistance and decreased insulin clearance [71]. In vitro, NEFAs reduced insulin binding, degradation and action [72]. In vivo, elevation of NEFAs substantially decreased insulin clearance [73, 74]. Moreover, human obesity, a condition characterised by excessive NEFA turnover [75], is usually associated with reduced insulin clearance [76, 77, 78]. Finally, in dogs [79, 80, 81] and in humans [82], insulin-induced suppression of endogenous glucose production is prevented by experimental elevation of NEFA. It is therefore highly possible that the greater insulin clearance in carriers of the Ala allele mirrors reduced portal NEFA availability. Our observation of significantly lower insulin-suppressed NEFA concentrations in carriers of the polymorphism [83] (Fig. 7b) suggested that one effect of the Ala allele is the more efficient suppression of lipolysis.
We addressed this issue further using a combination of a three-step hyperinsulinaemic-euglycaemic clamp and isotopic dilution to measure insulin sensitivity of lipolysis in subjects with and without the polymorphism. Glycerol labelled with a stable isotope (d5) was infused, and the systemic rate of appearance of glycerol was used as an index for whole body lipolysis. We found greater sensitivity to suppression of lipolysis by insulin in carriers of the Ala12 allele (Fig. 8a), translating into a lower insuln EC50 (Fig. 8b), which confirmed our earlier findings based on NEFA concentrations alone [69] (Fig. 8).
a. Suppression of the glycerol production rate (as index of whole-body lipolysis) determined by dilution of glycerol labelled with a stable isotope during a three-step euglycaemic-hyperinsulinaemic clamp in subjects with and without the Pro12Ala polymorphism in PPARγ2. White circles: Pro/Pro, wild-type; black circles: Pro/Ala, heterozygous; black triangles: Ala/Ala, homozygous. b. Resulting insulin EC50 in the same dataset. Carriers of the Ala allele suppress lipolysis at significantly lower insulin concentrations (modified from Stumvoll et al. [69]); p=0.001
Nevertheless, our results are also compatible with an alternative hypothesis. Although PPARγ is mainly expressed in adipose tissue, a direct effect of this polymorphism on hepatic insulin binding, action, internalisation and degradation cannot be excluded. In such a scenario, the Ala allele would primarily cause enhanced hepatic insulin clearance. That this could impact on insulin sensitivity and glucose tolerance derives support from a very recent report. Carcinoembryogenic-antigen-related cell adhesion molecule-1 (CEACAM1) is a protein with a key role in hepatic internalisation and degradation of receptor-bound insulin. Mutation of a functional serine residue resulted in hyperinsulinaemia, insulin resistance and impaired glucose tolerance in mice, while not affecting metabolic insulin signalling [84]. This clearly demonstrated that a primary defect in insulin clearance can trigger the cascade of events leading to Type 2 diabetes. Thus, a mutation that leads to an increase in insulin clearance would secondarily produce an improvement in insulin sensitivity and glucose tolerance.
In conclusion, the diabetes-protective effect of the Ala allele in PPARγ is probably secondary to the association with greater insulin sensitivity. This in turn is probably secondary to decreased release of NEFAs and possibly other factors from (perhaps mainly visceral) adipose tissue, and may operate through greater hepatic insulin sensitivity and insulin clearance [87].
Summary and conclusions
Unravelling the pathogenesis of Type 2 diabetes requires continued efforts to understand the mechanisms relevant for the control of glycaemia, from the molecular to the epidemiological level. Translation of the ever-growing basic scientific findings into a physiological and clinical context calls for novel and imaginative clinical experimental tools. The scope of such techniques encompasses procedures as diverse as isotope dilution for turnover studies (such as glycerol turnover as proxy for lipolysis) in addition to conventional clamp procedures, association studies of functionally relevant SNPs in candidate genes (such as IRS-1 and PPARγ), intelligent multivariate correlational approaches (such as with plasma adiponectin), magnetic resonance spectroscopy to quantify intra-tissue lipid deposition in addition to regional fat distribution, and advanced analytical biochemistry to determine fatty acid patterns in selected lipid fractions as proxy for enzymatic activity. Whenever human cohorts are studied, it is crucial to control for possible confounders of the variable under investigation based on a profound insight into human physiology. This can range from simple control for age or sex to taking into account differences in fat distribution or even genetic background. Future generations of scientists from all backgrounds and disciplines will need to make an honest effort to bridge the growing gap between basic scientific concepts and their relevance for human disease in prediction, prevention, diagnosis and therapy.
Abbreviations
- PPAR:
-
peroxisome proliferator-activated receptor
- SCD:
-
stearoyl-CoA desaturase
- SNP:
-
single nucleotide polymorphism
References
Fajans SS, Bell GI, Polonsky KS (2001) Molecular mechanisms and clinical pathophysiology of maturity-onset diabetes of the young. N Engl J Med 345:971–980
Maassen JA, Kadowaki T (1996) Maternally inherited diabetes and deafness: a new diabetes subtype. Diabetologia 39:375–382
Pozzilli P, Di Mario U (2001) Autoimmune diabetes not requiring insulin at diagnosis (latent autoimmune diabetes of the adult): definition, characterization, and potential prevention. Diabetes Care 24:1460–1467
Bergman RN, Phillips LS, Cobelli C (1981) Physiologic evaluation of factors controlling glucose tolerance in man: measurement of insulin sensitivity and beta-cell glucose sensitivity from the response to intravenous glucose. J Clin Invest 68:1456–1467
Bergman RN, Ader M, Huecking K et al. (2002) Accurate assessment of beta-cell function: the hyperbolic correction. Diabetes 51 [Suppl 1]:S212–S220
Kahn SE, Prigeon RL, McCulloch DK et al. (1993) Quantification of the relationship between insulin sensitivity and beta-cell function in human subjects. Evidence for a hyperbolic function. Diabetes 42:1663–1672
Bergman RN (1989) Lilly lecture 1989. Toward physiological understanding of glucose tolerance. Minimal-model approach. Diabetes 38:1512–1527
Stumvoll M, Tataranni PA, Stefan N et al. (2003) Glucose allostasis. Diabetes 52:903–909
Cannon WB (1929) Organization for physiological homeostasis. Physiol Rev 9:399–431
Sterling P, Eyer J (1988) Allostasis: a new paradigm to explain arousal pathology. In: Fisher S, Reason J (eds) Handbook of life stress, cognition and health. Wiley, New York, pp 629–649
McEwen BS (1998) Protective and damaging effects of stress mediators. N Engl J Med 338:171–179
Seeman TE, McEwen BS, Rowe JW et al. (2001) Allostatic load as a marker of cumulative biological risk: MacArthur studies of successful aging. Proc Natl Acad Sci USA 98:4770–4775
Goldstein DS, McEwen B (2002) Allostasis, homeostats, and the nature of stress. Stress 5:55–58
Goran MI, Gower BA (2001) Longitudinal study on pubertal insulin resistance. Diabetes 50:2444–2450
Montague CT, O’Rahilly S (2000) The perils of portliness: causes and consequences of visceral adiposity. Diabetes 49:883–888
Seppala-Lindroos A, Vehkavaara S, Hakkinen AM et al. (2002) Fat accumulation in the liver is associated with defects in insulin suppression of glucose production and serum free fatty acids independent of obesity in normal men. J Clin Endocrinol Metab 87:3023–3028
Thamer C, Machann J, Bachmann O et al. (2003) Intramyocellular lipids: anthropometric determinants and relationships with maximal aerobic capacity and insulin sensitivity. J Clin Endocrinol Metab 88:1785–1791
Medici F, Hawa M, Pyke DA et al. (1999) Concordance rate for type II diabetes mellitus in monozygotic twins: actuarial analysis. Diabetologia 42:146–150
Poulsen P, Kyvik KO, Vaag A et al. (1999) Heritability of type II (non-insulin-dependent) diabetes mellitus and abnormal glucose tolerance—a population-based twin study. Diabetologia 42:139–145
Lehtovirta M, Kaprio J, Forsblom C et al. (2000) Insulin sensitivity and insulin secretion in monozygotic and dizygotic twins. Diabetologia 43:285–293
Lander ES, Schork NJ (1994) Genetic dissection of complex traits. Science 265:2037–2048
Hanis CL, Boerwinkle E, Chakraborty R et al. (1996) A genome-wide search for human non-insulin-dependent (Type 2) diabetes genes reveals a major susceptibility locus on chromosome 2. Nat Genet 13:161–166
Permutt AM, Bernal-Mizrachi E, Inoue H (2000) Calpain 10: the first positional cloning of a gene for Type 2 diabetes. J Clin Invest 106:819–821
Ma H, Fukiage C, Kim YH et al. (2001) Characterization and expression of calpain 10. A novel ubiquitous calpain with nuclear localization. J Biol Chem 276:28525–28531
Baier LJ, Permana PA, Yang X et al. (2000) A calpain-10 gene polymorphism is associated with reduced muscle mRNA levels and insulin resistance. J Clin Invest 106:R69–R73
Oral EA, Simha V, Ruiz E et al. (2002) Leptin-replacement therapy for lipodystrophy. N Engl J Med 346:570–578
Weyer C, Funahashi T, Tanaka S et al. (2001) Hypoadiponectinemia in obesity and Type 2 diabetes: close association with insulin resistance and hyperinsulinemia. J Clin Endocrinol Metab 86:1930–1935
Takahashi M, Arita Y, Yamagata K et al. (2000) Genomic structure and mutations in adipose-specific gene, adiponectin. Int J Obes Relat Metab Disord 24:861–868
Yang WS, Lee WJ, Funahashi T et al. (2001) Weight reduction increases plasma levels of an adipose-derived anti-inflammatory protein, adiponectin. J Clin Endocrinol Metab 86:3815–3819
Lindsay RS, Funahashi T, Hanson RL et al. (2002) Adiponectin and development of Type 2 diabetes in the Pima Indian population. Lancet 360:57–58
Spranger J, Kroke A, Mohlig M et al. (2003) Adiponectin and protection against Type 2 diabetes mellitus. Lancet 361:226–228
Yamauchi T, Kamon J, Waki H et al. (2001) The fat-derived hormone adiponectin reverses insulin resistance associated with both lipoatrophy and obesity. Nat Med 7:941–946
Combs TP, Pajvani UB, Berg AH et al. (2004) A transgenic mouse with a deletion in the collagenous domain of adiponectin displays elevated circulating adiponectin and improved insulin sensitivity. Endocrinology 145:367–383
Tschritter O, Fritsche A, Thamer C et al. (2003) Plasma adiponectin concentrations predict insulin sensitivity of both glucose and lipid metabolism. Diabetes 52:239–243
Combs TP, Berg AH, Obici S et al. (2001) Endogenous glucose production is inhibited by the adipose-derived protein Acrp30. J Clin Invest 108:1875–1881
Stefan N, Stumvoll M, Vozarova B et al. (2003) Plasma adiponectin and endogenous glucose production in humans. Diabetes Care 26:3315–3319
Stumvoll M, Tschritter O, Fritsche A et al. (2002) Association of the T-G polymorphism in adiponectin (exon 2) with obesity and insulin sensitivity. Interaction with family history of diabetes. Diabetes 51:37–42
Yamauchi T, Kamon J, Ito Y et al. (2003) Cloning of adiponectin receptors that mediate antidiabetic metabolic effects. Nature 423:762–769
Cohen P, Miyazaki M, Socci ND et al. (2002) Role for stearoyl-CoA desaturase-1 in leptin-mediated weight loss. Science 297:240–243
Zhang Y, Wat N, Stratton IM et al. (1996) UKPDS 19: heterogeneity in NIDDM: separate contributions of IRS-1 and beta 3-adrenergic-receptor mutations to insulin resistance and obesity respectively with no evidence for glycogen synthase gene mutations. UK Prospective Diabetes Study. Diabetologia 39:1505–1511
Koch M, Rett K, Volk A et al. (1999) Amino acid polymorphism Gly 972 Arg in IRS-1 is not associated to lower clamp-derived insulin sensitivity in young healthy first degree relatives of patients with Type 2 diabetes. Exp Clin Endocrinol Diabetes 107:318–322
Hager J, Zouali H, Velho G et al. (1993) Insulin receptor substrate (IRS-1) gene polymorphisms in French NIDDM families. Lancet 342:1430–1430
Imai Y, Philippe N, Sesti G et al. (1997) Expression of variant forms of insulin receptor substrate-1 identified in patients with noninsulin-dependent diabetes mellitus. J Clin Endocrinol Metab 82:4201–4207
Ura S, Araki E, Kishikawa H et al. (1996) Molecular scanning of the insulin receptor substrate-1 (IRS-1) gene in Japanese patients with NIDDM: identification of five novel polymorphisms. Diabetologia 39:600–608
Almind K, Bjorbaek C, Vestergaard H et al. (1993) Aminoacid polymorphisms of insulin receptor substrate-1 in non-insulin-dependent diabetes mellitus. Lancet 342:828–832
Laakso M, Malkki M, Kekalainen P et al. (1994) Insulin receptor substrate-1 variants in non-insulin-dependent diabetes. J Clin Invest 94:1141–1146
Porzio O, Federici M, Hribal ML et al. (1999) The Gly972→Arg amino acid polymorphism in IRS-1 impairs insulin secretion in pancreatic beta cells. J Clin Invest 104:357–364
Stumvoll M, Fritsche A, Volk A et al. (2001) The Gly972Arg polymorphism in the insulin receptor substrate-1 gene contributes to the variation in insulin secretion in normal glucose tolerant humans. Diabetes 50:882–885
Marchetti P, Lupi R, Federici M et al. (2002) Insulin secretory function is impaired in isolated human islets carrying the Gly(972)→Arg IRS-1 polymorphism. Diabetes 51:1419–1424
Fritsche A, Stefan N, Hardt E et al. (2000) A novel hyperglycemic clamp for characterization of islet function in humans: assessment of three different secretagogues, maximal insulin response and reproducibility. Eur J Clin Invest 30:411–418
’t Hart LM, Nijpels G, Dekker JM et al. (2002) Variations in insulin secretion in carriers of gene variants in IRS-1 and -2. Diabetes 51:884–887
Desvergne B, Wahli W (1999) Peroxisome proliferator-activated receptors: nuclear control of metabolism. Endocr Rev 20:649–688
Stumvoll M, Haring HU (2002) Glitazones: clinical effects and molecular mechanisms. Ann Med 34:217–224
Olefsky JM (2000) Treatment of insulin resistance with peroxisome proliferator-activated receptor gamma agonists. J Clin Invest 106:467–472
Schoonjans K, Auwerx J (2000) Thiazolidinediones: an update. Lancet 355:1008–1010
Saltiel AR, Olefsky JM (1996) Thiazolidinediones in the treatment of insulin resistance and type II diabetes. Diabetes 45:1661–1669
Spiegelman BM (1998) PPAR-gamma: adipogenic regulator and thiazolidinedione receptor. Diabetes 47:507–514
Auwerx J (1999) PPARgamma, the ultimate thrifty gene. Diabetologia 42:1033–1049
Beamer BA, Negri C, Yen CJ et al. (1997) Chromosomal localization and partial genomic structure of the human peroxisome proliferator activated receptor-gamma (hPPAR gamma) gene. Biochem Biophys Res Commun 233:756–759
Yen CJ, Beamer BA, Negri C et al. (1997) Molecular scanning of the human peroxisome proliferator activated receptor gamma (hPPAR gamma) gene in diabetic Caucasians: identification of a Pro12Ala PPAR gamma 2 missense mutation. Biochem Biophys Res Commun 241:270–274
Altshuler D, Hirschhorn JN, Klannemark M et al. (2000) The common PPARγ Pro12Ala polymorphism is associated with decreased risk of Type 2 diabetes. Nat Genet 26:76–80
Memisoglu A, Hu FB, Hankinson SE et al. (2003) Interaction between a peroxisome proliferator-activated receptor {gamma} gene polymorphism and dietary fat intake in relation to body mass. Hum Mol Genet 12:2923–2929
Ek J, Andersen G, Urhammer SA et al. (2001) Studies of the Pro12Ala polymorphism of the peroxisome proliferator-activated receptor-γ2 (PPAR-γ2) gene in relation to insulin sensitivity among glucose tolerant Caucasians. Diabetologia 44:1170–1176
Deeb SS, Fajas L, Nemoto M et al. (1998) A Pro12Ala substitution in PPARγ2 associated with decreased receptor activity, lower body mass index and improved insulin sensitivity. Nat Genet 20:284–287
Jacob S, Stumvoll M, Becker R et al. (2000) The PPARgamma2 polymorphism Pro12Ala is associated with better insulin sensitivity in the offspring of Type 2 diabetic patients. Horm Metab Res 32:413–416
Hara K, Okada T, Tobe K et al. (2000) The Pro12Ala polymorphism in PPAR gamma2 may confer resistance to Type 2 diabetes. Biochem Biophys Res Commun 271:212–216
Koch M, Rett K, Maerker E et al. (1999) The PPARgamma2 amino acid polymorphism Pro 12 Ala is prevalent in offspring of Type II diabetic patients and is associated to increased insulin sensitivity in a subgroup of obese subjects. Diabetologia 42:758–762
Muller YL, Bogardus C, Beamer BA et al. (2003) A functional variant in the peroxisome proliferator-activated receptor gamma2 promoter is associated with predictors of obesity and Type 2 diabetes in Pima Indians. Diabetes 52:1864–1871
Stumvoll M, Wahl HG, Löblein K et al. (2001) The Pro12Ala polymorphism in the peroxisome proliferator activated receptor γ2 gene is associated with increased antilipolytic insulin sensitivity. Diabetes 50:876–881
Boden G, Chen X, Capulong E et al. (2001) Effects of free fatty acids on gluconeogenesis and autoregulation of glucose production in Type 2 diabetes. Diabetes 50:810–816
Boden G (1997) Role of fatty acids in the pathogenesis of insulin resistance and NIDDM. Diabetes 46:3–10
Duckworth WC, Bennett RG, Hamel FG (1998) Insulin degradation: progress and potential. Endocr Rev 19:608–624
Douglas JA, Erdos MR, Watanabe RM et al. (2001) The peroxisome proliferator-activated receptor-gamma2 Pro12A1a variant: association with Type 2 diabetes and trait differences. Diabetes 50:886–890
Ferrannini E, Wahren J, Faber OK et al. (1983) Splanchnic and renal metabolism of insulin in human subjects: a dose-response study. Am J Physiol 244:E517–E527
Campbell PJ, Carlson MG, Nurjhan N (1994) Fat metabolism in human obesity. Am J Physiol 266:E600–E605
Iozzo P, Beck-Nielsen H, Laakso M et al. (1999) Independent influence of age on basal insulin secretion in nondiabetic humans. European Group for the Study of Insulin Resistance. J Clin Endocrinol Metab 84: 863–868
Jones CN, Pei D, Staris P et al. (1997) Alterations in the glucose-stimulated insulin secretory dose-response curve and in insulin clearance in nondiabetic insulin-resistant individuals. J Clin Endocrinol Metab 82:1834–1838
Luan J, Browne PO, Harding AH et al. (2001) Evidence for gene-nutrient interaction at the PPARgamma locus. Diabetes 50:686–689
Mori H, Ikegami H, Kawaguchi Y et al. (2001) The Pro12 -->Ala substitution in PPAR-gamma is associated with resistance to development of diabetes in the general population: possible involvement in impairment of insulin secretion in individuals with Type 2 diabetes. Diabetes 50:891–894
Bergman RN (2000) Non-esterified fatty acids and the liver: why is insulin secreted into the portal vein? Diabetologia 43:946–952
Michael MD, Kulkarni RN, Postic C et al. (2000) Loss of insulin signaling in hepatocytes leads to severe insulin resistance and progressive hepatic dysfunction. Mol Cell 6:87–97
Chen X, Iqbal N, Boden G (1999) The effects of free fatty acids on gluconeogenesis and glycogenolysis in normal subjects. J Clin Invest 103:365–372
Tschritter O, Fritsche A, Stefan N et al. (2003) Increased insulin clearance in peroxisome proliferator-activated receptor gamma2 Pro12Ala. Metabolism 52:778–783
Poy MN, Yang Y, Rezaei K et al. (2002) CEACAM1 regulates insulin clearance in liver. Nat Genet 30:270–276
Stumvoll M, Mitrakou A, Pimenta W et al. (2000) Use of the oral glucose tolerance test to assess insulin release and insulin sensitivity. Diabetes Care 23:295–301
Matsuda A, DeFronzo R (1999) Insulin sensitivity indices obtained from oral glucose tolerance testing. Diabetes Care 22:1462–1470
Stumvoll M, Häring H (2002) The Pro12Ala polymorphism in the peroxisome proliferator-activated receptor γ. Diabetes 51:2341–2347
Acknowledgements
I wish to thank the many volunteers who participated in our studies. I gratefully acknowledge the teaching, patience and continuous support of my mentors and their co-workers: John Gerich, University of Rochester, N.Y., USA, who raised my interest in clinical research; Hans Häring, University of Tübingen, Germany, who provided a wonderful platform for most of my studies; Bo Bogardus, National Institutes of Health, Phoenix, Ariz., USA, who put the idea, though not the word, of glucose allostasis in my mind. I also thank Bruce McEwen, The Rockefeller University, New York, N.Y., USA, for his discussions on the allostasis concept, and Hans-Günther Wahl for meticulously establishing the technique of measuring fatty acid patterns in Tübingen. This review was in large parts presented as the Minkowski Lecture at the 2003 IDF Meeting in Paris, at which time the author was still affiliated with the University of Tübingen, Department of Medicine.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Stumvoll, M. Control of glycaemia: from molecules to men. Minkowski Lecture 2003. Diabetologia 47, 770–781 (2004). https://doi.org/10.1007/s00125-004-1400-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-004-1400-0