Abstract
Aims/hypothesis
Retinal vascular leakage is an early pathological feature in diabetic retinopathy and can lead to macular oedema and loss of vision. Previously we have shown that plasminogen kringle 5 (K5), an angiogenic inhibitor, inhibits retinal neovascularisation in the rat model of oxygen-induced retinopathy (OIR). The purpose of this study was to examine the effect of K5 on vascular leakage in the retina.
Methods
Neonatal rats were exposed to hyperoxia to induce OIR. Diabetes was induced in adult rats by injecting streptozotocin. Vascular permeability was measured by Evans blue method. Expression of vascular endothelial growth factor (VEGF) was evaluated using immunohistochemistry and western blot analysis.
Results
Rats with OIR and diabetes showed abnormal vascular hyperpermeability in the retina and iris. Intravitreal injection of K5, reduced vascular permeability in both animal models, but did not affect permeability in normal rats. K5 reduced vascular permeability at doses substantially lower than that required for inhibition of retinal neovascularisation. The K5-induced reduction in vascular permeability correlated with its down-regulation of VEGF expression in the retina. Moreover, K5 inhibited IGF-1-induced hyperpermeability, which is known to arise through up-regulation of endogenous VEGF expression. However, K5 had no effect on the hyperpermeability induced by injection of exogenous VEGF.
Conclusions/interpretation
Very low doses of K5 reduce pathological vascular leakage in the retina. K5 thus has therapeutic potential in the treatment of diabetic macular oedema. This effect can be ascribed, at least in part, to the down-regulation of endogenous VEGF expression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Breakdown of the blood-retinal barrier is a common pathological change in many ocular diseases such as diabetic retinopathy [1, 2, 3]. In the early stage of diabetic retinopathy, an increase of retinal vascular permeability precedes the appearance of clinical retinopathy [4, 5]. Retinal vascular leakage often leads to macular oedema, which is the single greatest cause of vision loss in diabetes [6]. Increased retinal vascular permeability caused by the breakdown of the blood-retinal barrier has been shown to occur in patients with diabetes and in streptozotocin (STZ)-induced diabetic animal models [4, 5, 7]. An increase in microvascular permeability is also thought to be a crucial step in angiogenesis associated with tumours [8]. The exact mechanism underlying the breakdown of the blood-retinal barrier and the pathological increase of retinal vascular permeability is mostly unclear, and there is no effective treatment for macular oedema secondary to vascular hyperpermeability.
Vascular endothelial growth factor (VEGF) is a major angiogenic and mitogenic factor, playing a crucial role in normal and pathological angiogenesis [9, 10]. Based on its ability to induce vascular hyperpermeability, VEGF is also referred to as the vascular permeability factor [9, 11] and is one of the main mediators of retinal vascular hyperpermeability [12, 13]. The up-regulated expression of VEGF or its receptors is associated with increased vascular hyperpermeability in the retina of STZ-induced diabetes [7].
Plasminogen kringle 5 (K5) is a proteolytic fragment of plasminogen with a potent anti-angiogenic activity [14, 15]. Our previous studies showed that K5 prevents the development and arrests the progression of retinal neovascularisation in a rat model of oxygen-induced retinopathy (OIR) [16, 17]. Moreover, K5 down-regulates endogenous VEGF and up-regulates an endogenous angiogenic inhibitor, pigment epithelium-derived factor in vivo and in vitro [16]. Based on the close relationship between retinal vascular permeability and VEGF and the ability of K5 to regulate the expression of VEGF, we hypothesised that K5 prevents the breakdown of the blood-retinal barrier and decreases retinal vascular leakage in ischaemia-induced retinal diseases. To determine the effect of K5 on pathological vascular leakage and explore its possible mechanisms of action we used OIR and STZ-diabetic models.
Materials and methods
Animals
Brown Norway rats were purchased from Harlan Sprague-Dawley (Indianapolis, Ind., USA). The project was approved by the Institutional Animal Care and Use Committee of the Medical University of South Carolina and the University of Oklahoma Health Science Center. Care, use, and treatment of all animals in this study were in strict agreement with the Association for Research in Vision and Ophthalmology statement for the Use of Animals in Ophthalmic and Vision Research, as well as the Medical University of South Carolina’s guidelines on the Care and Use of Laboratory Animals. The principles of laboratory animal care were followed and national laws on this issue were complied with.
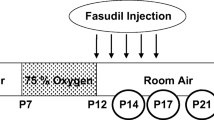
OIR and intravitreal injection of K5
OIR was induced as described previously [18] with some modifications. Pigmented Brown Norway rats were used as they are more susceptible to OIR [19]. At postnatal day (P) seven, 40 rats in the experimental group were exposed to hyperoxia (75% O2) for 5 days (P7-P12) and then returned to normoxia (room air) to induce retinopathy. Another 40 rats in the control group were kept at constant normoxia under a normal diet and a 12-h light and dark cycle. At each time point (P12, P14, P16, P18, P22, P30 and P36), vascular permeability was measured in the retina and iris of experimental and control groups.
Recombinant K5 was expressed and purified as described previously [17]. K5 was injected into the vitreous of the right eye (3 µl per eye) of the anaesthetised rats through the pars plana using a glass capillary. The left eye received the same volume of sterile PBS. After injection, the animals were kept in normoxia until they were analysed.
Measurement of vascular permeability
Vascular permeability was quantified by measuring albumin leakage from blood vessels into the retina and iris using Evans blue in accordance with a documented protocol [20] with minor modifications. Evans blue dye (Sigma, St Louis, Mo., USA) was dissolved in normal saline (30 mg/ml), sonicated for 5 min and filtered through a 0.45-µm filter (Millipore, Bedford, Mass., USA). The rats were anaesthetised, and Evans blue (30 mg/kg) was injected over 10 s through the femoral vein using a glass capillary under microscopic inspection. Evans blue binds non-covalently to plasma albumin in the blood stream [21]. Immediately after Evans blue infusion, the rats turned blue, confirming uptake and distribution of the dye. The rats were kept on a warm pad for 2 h to ensure the complete circulation of the dye. Then the chest cavity was opened and the rats were perfused via the left ventricle with 1% paraformaldehyde in citrate buffer (pH=4.2), which was pre-warmed to 37°C to prevent vasoconstriction. The perfusion lasted 2 min under the physiological pressure of 120 mmHg to clear the dye from the vessel. Immediately after perfusion, the eyes were enucleated and the retina and iris were carefully dissected under an operating microscope. Evans blue dye was extracted by incubating each sample in 150 µl formamide (Sigma) for 18 h at 70°C. The extract was centrifuged (Rotor type: TLA 100.3, Beckman Coulter, Fullerton, Calif., USA) at 70 000 rpm for 20 min at 4°C. Absorbance was measured using 100 µl of the supernatant at 620 nm. The concentration of Evans blue in the extracts was calculated from a standard curve of Evans blue in formamide and normalised by the total protein concentration in each sample. Results were expressed in micrograms of Evans blue per milligrams of total protein content.
Induction of experimental diabetes and intravitreal injection of K5
Eight Brown Norway rats (6 weeks old) were used in the experiment. Diabetes was induced after an overnight fast with an intraperitoneal injection of STZ (60 mg/kg in 10 mmol/l of citrate buffer, pH 4.5) into anaesthetised rats. Control rats were injected with citrate buffer alone. Serum glucose concentrations were checked every 2 days, and only animals with concentrations above 20 mmol/l were considered diabetic. Two weeks after the injection of STZ, K5 was injected into the vitreous of the right eye. The left eye received the same volume of sterile PBS as the control eye. Two days later vascular permeability was measured using the Evans blue method.
Evaluation of effect of K5 on hyperpermeability induced by VEGF and IGF-1
Sixteen 7-week-old Brown Norway rats were used in this experiment. VEGF (Pepro Tech, Rocky Hill, N.J., USA) was diluted to 0.03 µg/µl in PBS and sterilised. Purified IGF-1 was provided by Dr. Rosenzweig at the Department of Pharmacology, Medical University of South Carolina and was diluted to a concentration of 1.6 ng/µl and sterilised. The VEGF + K5 mixture contained 0.03 µg/µl VEGF and 0.3 µg/µl K5. The IGF-1 + K5 mixture contained 1.6 ng/µl IGF-1 and 0.3 µg/µl K5. Two groups of animals received an intravitreal injection of 3 µl VEGF or IGF-1 solution into the right eye and PBS into the left eye. The other two groups received 3 µl of the VEGF + K5 or IGF-1 + K5 solutions to the right eye and VEGF or IGF-1 alone to the left eye. Six hours after the injection, the vascular permeability in the retina and iris was measured as described above.
Assessment of VEGF expression
VEGF western blot analysis was done as described previously [16]. Immunohistochemistry was carried out as described previously [22]. Briefly, retinal sections were incubated with 1 to 100 dilution of the anti-VEGF antibody (Santa Cruz Biotechnology, Santa Cruz, Calif., USA). After extensive washes, the sections were incubated with biotin-labelled monoclonal anti-rabbit antibody (Vector Laboratories, Burlingame, Calif., USA) and developed using the ABC method (Vector Laboratories), with 3.3′ diaminobenzidine (0.025% in 0.05 mol/l Tris, pH 7.4, containing 0.03% hydrogen peroxide) as a chromogen.
Statistical analysis
Statistical analysis used the Student’s t test. The paired t test was used for comparing eyes from the same animal, while the unpaired test was used to compare different animals. ANOVA was used in the factorial test. Statistical difference was considered significant at a p value of less than 0.05.
Results
Time-course of vascular permeability change in OIR rats
In normal rats kept under constant normoxia, vascular permeability did not change in the retina and iris from P12 to P22 (p>0.1, n=4 to 7) (Fig. 1a, b). Permeability in the retina was lower than in the iris, reflecting a normal blood-retinal barrier.
Time course of vascular permeability changes in a rat model of OIR. Rats were exposed to 75% O2 from P7 to P12 and then returned to normoxia. Age-matched rats kept in constant normoxia were used as controls. Vascular permeability in the retina (a) and iris (b) was measured at P12, P14, P16, P18, P22, P30 and P36. The Evans blue in the tissues was normalised by total protein concentration and expressed as µg of dye per mg of protein in the tissue (means ± SD, n=4 to 7). Values statistically different from the control values are indicated by *. OIR, oxygen-induced retinopathy
In OIR rats exposed to hyperoxia from P7 to P12, retinal vascular permeability was increased at P12, the first day after they were returned to normoxia. The increase was 3.2 times higher than in the control rats matched for age (p<0.001, n=4). Retinal vascular permeability reached a peak at P16, 4 days after the animals were returned to normoxia (8.7-fold over the controls, p<0.001, n=7). From P18 to P22, the permeability declined gradually, but remained higher than the normal levels (7.6- and 4.23-fold over the respective controls, p<0.001, n=4). Vascular permeability in the retina declined to the normal level after P30 (Fig. 1a).
In the iris of the OIR rats, permeability started to increase at P14 (1.87-fold over the controls, p<0.001) and peaked at P18 (2.41-fold, p<0.001). Thereafter, it remained higher than in the controls for the duration of the experimental period (Fig. 1b).
Effect of K5 on vascular hyperpermeability in OIR rats
After the intravitreal injection at P14 vascular permeability was measured at P15, P16, P18 and P22. At P15, retinal vascular permeability in eyes treated with K5 decreased to 52% of that in eyes injected with PBS (paired t test, p<0.01, n=4) (Fig. 2a). The fluorescein angiography showed that K5 had no detectable effect on retinal neovascularisation at this early stage and this dose (data not shown), suggesting that the reduction of vascular permeability through K5 occurs before its action on retinal neovascularisation. The strongest effect of K5 was seen 2 days after the injection (P16), with retinal vascular permeability in K5-treated eyes decreasing to 24.6% of the PBS control values (paired t test, p<0.001, n=4). Four and eight days after the K5 injection, retinal vascular permeability returned to the control range (p>0.05, n=4) (Fig. 2a).
Dose- and time-dependent effects of K5 on vascular hyperpermeability in OIR rats. At P14 (a, b) the right eye received an intravitreal injection of K5 (1 µg per eye). The left eye received PBS as the control eye. Vascular permeability was measured 1, 2, 4 and 8 days after the injection. The Evans blue leakage was normalised by total protein concentration and expressed as percentage of the respective control. Rats with OIR received (c, d) an intravitreal injection of 1, 0.3, or 0.1 µg K5 per eye at P14. Permeability was measured at P16. Effects are shown as follows: retina (a, c), iris: (c, b). Values are expressed as means ± SD (n=4). K5 plasminogen kringle 5, OIR oxygen-induced retinopathy
In the iris K5 significantly reduced vascular permeability only at 2 days after the injection (65.4% of the controls, p<0.01) (Fig. 2b).
Dose-dependent effects of K5 on vascular permeability in OIR rats
Two days after the K5 injection (0.1, 0.3 and 1 µg per eye), vascular permeability was decreased in a dose-dependent manner in the retina and iris (Fig. 2). K5 at a dose of 1 and 0.3 µg per eye reduced vascular permeability in the retina and iris in comparison to the eye injected with PBS (p<0.01, n=4) (Fig. 2c, d).
Effect of K5 on vascular permeability in normal rats
K5 was injected into the right eyes of normal rats (1 µg per eye) at P14. The results showed that K5 did not reduce permeability in the retina and iris of normal rats, when compared to the PBS control rats, although it did reduce vascular permeability in rats with OIR (Fig. 3, p>0.05, n=4).
Effect of K5 on vascular permeability in normal and OIR rats. Normal rats (P14) maintained under normoxia and OIR rats received the same dose of K5 (1 µg per eye) in the right eye and PBS in the left eye. Vascular permeability in the retina (a) and iris (b) was measured at P16 and normalised by total protein concentrations (means ± SD, n=4). OIR oxygen-induced retinopathy, K5 plasminogen kringle 5
Effect of K5 on vascular leakage in diabetic rats
Vascular permeability in the retina and iris was significantly higher in rats with STZ-induced diabetes than in age-matched normal rats (Fig. 4). Two days after the injection of K5 (1 µg per eye), the eyes injected with K5 showed less vascular permeability in the retina and iris than the PBS-injected eyes in STZ-diabetic rats (p<0.01, n=4) (Fig. 4). K5 decreased permeability to the level of normal rats. In contrast, the same dose of K5 did not affect vascular permeability in age-matched normal adult rats (p>0.05, n=4) (Fig. 4).
K5-mediated decrease of vascular leakage possibly caused by down-regulation of endogenous VEGF
Immunohistochemistry using an anti-VEGF antibody showed that rats with OIR have a substantially increased VEGF signal in the retina (Fig. 5). Intravitreal injection of 0.3 and 1.0 µg per eye of K5 resulted in an apparent VEGF signal in the retina 2 days after the injection, compared to PBS-injected retina of OIR rats. The inner retina showed greater changes than the outer retina (Fig. 5c, d). The effect of K5 on VEGF expression was semi-quantified by western blot analysis using the anti-VEGF antibody. The results showed that K5 decreased VEGF concentrations in a dose-dependent manner in the retina of OIR rats (Fig. 5e). The dose-dependent effect on VEGF expression correlated with the K5-induced reduction of vascular permeability.
K5-mediated down-regulation of VEGF expression in the retina of OIR rats. Immunohistochemistry using an anti-VEGF antibody showed that K5 (1 µg per eye) decreases VEGF expression in the retina of OIR rats, compared with expression after PBS injection. The figure shows the retina of normal rats (a), rats with OIR after PBS injection (b); rats with OIR after injection of 0.3 µg per eye of K5 (c), and (d) rats with OIR after injection of 1 µg per eye K5. Each image is a representative from three rats. Rats with OIR received (e) an intravitreal injection of K5 (1, 0.3 or 0.1 µg per eye) at P14. Retinal VEGF concentrations were assessed by western blot analysis at P16. The same membrane was stripped and reblotted with the anti-β-actin antibody. K5, plasminogen kringle 5, VEGF, vascular endothelial growth factor, OIR, oxygen-induced retinopathy
To further confirm that K5 affects vascular permeability through the down-regulation of endogenous VEGF, we assessed its effect on (i) hyperpermeability induced by injection of exogenous VEGF, and (ii) on hyperpermeability induced by IGF-1, which is known to induce endogenous VEGF expression. The injection of VEGF increased vascular permeability 2.2-fold in the retina and 1.2-fold in the iris, compared with PBS controls (p<0.01, Fig. 6a, b). Vascular permeability in the retina and iris of eyes injected with the mixture of K5 and VEGF was not significantly different from that in eyes injected with VEGF alone (p>0.05).
Effects of K5 on the hyperpermeability induced by VEGF and IGF-1. Adult rats were randomly assigned to four groups. Groups 1 and 2 received VEGF and IGF-1 intravitreal injections respectively in the right eye and PBS in the left eye as a control. Groups 3 and 4 received an injection of VEGF + K5 and IGF-1 + K5 cocktail solutions respectively in the right eye, with VEGF and IGF-1 alone in the left eye as controls. Six hours after the injections, vascular permeability was examined in the retina (a, c) and iris (b, d). The results were normalised by total protein concentrations and expressed as means ± SD, n=4. K5 plasminogen kringle 5, VEGF, vascular endothelial growth factor
The IGF-1 injection increased vascular permeability 3.1-fold in the retina and 1.7-fold in the iris, compared with the PBS controls (p<0.01, Fig. 6c, d). The permeability in eyes which received a mixture of IGF-1 and K5 was indistinguishable from that in PBS-injected eyes and lower than in eyes injected with IGF-1 alone (p<0.01, Fig. 6c, d), indicating that K5 completely blocks hyperpermeability induced by IGF-1.
Discussion
Vascular leakage in the retina is a major cause of macular oedema in diabetic retinopathy and other retinal diseases [1, 23, 24]. Currently, there is no satisfactory treatment for macular oedema. Our study reports that in addition to its anti-angiogenic activity, K5 prevents and reverses vascular hyperpermeability in diabetic rats and in rats with OIR, suggesting that K5 could be beneficial in the treatment of macular oedema.
OIR is a commonly used model for studies of retinal neovascularisation, such as retinopathy of prematurity and diabetic retinopathy [17, 18]. The change of vascular permeability in the OIR model and patients with retinopathy of prematurity has not been examined. Our study shows a transient but substantial increase in retinal vascular permeability in OIR. Significant vascular hyperpermeability occurs at P12. As shown in previous studies, there was no significant neovascularisation in the first 2 days (P12–P13) after the rats were returned from hyperoxia to normoxia in the same animal model. Apparent retinal neovascularisation appeared after P14 and declined after P22 [25]. Therefore, retinal vascular hyperpermeability, which indicates dysfunction of the blood-retinal barrier, appears earlier than retinal neovascularisation in the OIR model. Our study also suggests that the OIR rat is a good model for studying vascular leakage in the retina.
The mechanism underlying the breakdown of the blood-retinal barrier and vascular hyperpermeability at the early stage of OIR is mostly unclear. VEGF has recently been established as an important mediator of increased vascular permeability via a mechanism dependent on protein kinase C [11, 26]. VEGF is known to be an angiogenic stimulator, mitogenic factor and also a vasopermeability factor [9, 27, 28]. It is 50 000 times more potent than histamine in increasing dermal microvascular permeability [29]. Increased VEGF concentrations are a common pathological factor in neovascular ocular diseases of humans, as well as in the animal models of ischaemia-induced retinopathy [28, 30, 31, 32]. Recently, VEGF-targeted strategies, such as anti-VEGF antibodies and antagonists of VEGF receptors, have shown beneficial effects on the treatment of neovascular diseases [33, 34, 35]. Our previous studies showed that in OIR rats retinal VEGF concentrations increase to a peak at P16, 4 days after the animals are returned to normoxia [25], correlating with the peak of vascular permeability in the retina. These results suggest that VEGF is a major contributor to hyperpermeability in the OIR model.
Plasminogen kringle 5 is a potent angiogenic inhibitor [14]. We have previously shown that a single intravitreal injection of K5 prevents the development and arrests the progression of retinal neovascularisation in the OIR model [17]. The present study showed a new function of K5, i.e., its ability to prevent the breakdown of the blood-retinal barrier and reduce vascular leakage. In addition, K5 inhibited retinal neovascularisation at a dose of 10 µg per eye but not at 1 µg per eye [17]. We also showed that at a dose of 0.3 µg per eye K5 reduces retinal vascular permeability in the retina, as well as in the iris in the same animal model. This suggests that a lower dose of K5 is needed to affect vascular leakage than to achieve its anti-angiogenic activity.
The reduction of vascular permeability induced by K5 occurs early, 24 h after the K5 injection, when no detectable effect on neovascularisation is observed. The injection of K5 also reduced permeability in STZ-diabetic rats, which do not develop retinal neovascularisation [36, 37]. These results suggest that the K5-induced reduction of vascular leakage is not the result of inhibition of neovascularisation. The effect of K5 on retinal vascular permeability is transient and peaks at the second day after the K5 injection. The short duration of this effect could result from a short half-life of the peptide in the vitreous after a single intravitreal injection [17].
With regard to findings that K5 displayed anti-angiogenic activity only in OIR rats, but not in the normal retina [17], we showed that K5 only reduces vascular permeability in the retina of OIR and diabetic rats to the normal range, but does not further decrease permeability in normal rats matched for age. These results are consistent with the observation that K5 only down-regulates VEGF expression in the retina with ischaemia but does not decrease VEGF concentrations in the normal retina. Moreover, the K5 dose-dependent reduction of vascular permeability correlates with the dose-dependent down-regulation of VEGF in the OIR model. These observations suggest that the K5-induced reduction in permeability could result from its inhibitory effect on VEGF expression.
To further confirm that the K5-induced reduction in vascular permeability occurs by blocking the expression of endogenous VEGF, we compared the effect of K5 on (i) hyperpermeability induced by injection of exogenous VEGF and (ii) hyperpermeability induced by injection of IGF-1. IGF-1-induced hyperpermeability is dependent on the up-regulation of endogenous VEGF expression whereas that induced by VEGF injection is not [38]. Our results show that K5 prevents hyperpermeability induced by IGF-1 but not that induced by exogenous VEGF. This indicates that K5 does not reduce vascular leakage once the VEGF has been produced, providing further support that the K5-induced reduction of permeability occurs, at least in part, through blocking the production of endogenous VEGF.
Abbreviations
- K5:
-
plasminogen kringle 5
- OIR:
-
oxygen-induced retinopathy
- STZ:
-
streptozotocin
- VEGF:
-
vascular endothelial growth factor
- P:
-
postnatal day
References
Ciulla TA, Danis RP, Harris A (1998) Age-related macular degeneration: a review of experimental treatments. Surv Ophthalmol 43:134–146
Antonetti DA, Lieth E, Barber AJ, Gardner TW (1999) Molecular mechanisms of vascular permeability in diabetic retinopathy. Semin Ophthalmol 14:240–248
Klein R (1996) Diabetic retinopathy. Annu Rev Public Health 17:137–158
Cunha-Vaz JG, Gray JR, Zeimer RC, Mota MC, Ishimoto BM, Leite E (1985) Characterization of the early stages of diabetic retinopathy by vitreous fluorophotometry. Diabetes 34:53–59
Yoshida A, Ishiko S, Kojima M, Ogasawara H (1993) Permeability of the blood-ocular barrier in adolescent and adult diabetic patients. Br J Ophthalmol 77:158–161
Moss SE, Klein R, Klein BE (1998) The 14-year incidence of visual loss in a diabetic population. Ophthalmology 105:998–1003
Qaum T, Xu Q, Joussen AM et al. (2001) VEGF-initiated blood-retinal barrier breakdown in early diabetes. Invest Ophthalmol Vis Sci 42:2408–2413
Dvorak HF (1986) Tumors: wounds that do not heal. Similarities between tumor stroma generation and wound healing. N Engl J Med 315:1650–1659
Dvorak HF, Brown LF, Detmar M, Dvorak AM (1995) Vascular permeability factor/vascular endothelial growth factor, microvascular hyperpermeability, and angiogenesis. Am J Pathol 146:1029–1039
Aiello LP, Wong JS (2000) Role of vascular endothelial growth factor in diabetic vascular complications. Kidney Int Suppl 77:S113–S119
Aiello LP (1997) Vascular endothelial growth factor and the eye: biochemical mechanisms of action and implications for novel therapies. Ophthalmic Res 29:354–362
Murata T, Nakagawa K, Khalil A, Ishibashi T, Inomata H, Sueishi K (1996) The relation between expression of vascular endothelial growth factor and breakdown of the blood-retinal barrier in diabetic rat retinas. Lab Invest 74:819–825
Hammes HP, Lin J, Bretzel RG, Brownlee M, Breier G (1998) Upregulation of the vascular endothelial growth factor/vascular endothelial growth factor receptor system in experimental background diabetic retinopathy of the rat. Diabetes 47:401–406
Cao Y, Chen A, An SS, Ji RW, Davidson D, Llinas M (1997) Kringle 5 of plasminogen is a novel inhibitor of endothelial cell growth. J Biol Chem 272:22924–22928
Chang Y, Mochalkin I, McCance SG, Cheng B, Tulinsky A, Castellino FJ (1998) Structure and ligand binding determinants of the recombinant kringle 5 domain of human plasminogen. Biochemistry 37:3258–3271
Gao G, Li Y, Gee S et al. (2002) Down-regulation of vascular endothelial growth factor and up-regulation of pigment epithelium-derived factor: a possible mechanism for the anti-angiogenic activity of plasminogen kringle 5. J Biol Chem 277:9492–9497
Zhang D, Kaufman PL, Gao G, Saunders RA, Ma JX (2001) Intravitreal injection of plasminogen kringle 5, an endogenous angiogenic inhibitor, arrests retinal neovascularization in rats. Diabetologia 44:757–765
Smith LE, Wesolowski E, McLellan A et al. (1994) Oxygen-induced retinopathy in the mouse. Invest Ophthalmol Vis Sci 35:101–111
Gao G, Li Y, Fant J, Crosson CE, Becerra SP, Ma JX (2002) Difference in ischemic regulation of vascular endothelial growth factor and pigment epithelium-derived factor in brown norway and sprague dawley rats contributing to different susceptibilities to retinal neovascularization. Diabetes 51:1218–1225
Xu Q, Qaum T, Adamis AP (2001) Sensitive blood-retinal barrier breakdown quantitation using Evans blue. Invest Ophthalmol Vis Sci 42:789–794
Radius RL, Anderson DR (1980) Distribution of albumin in the normal monkey eye as revealed by Evans blue fluorescence microscopy. Invest Ophthalmol Vis Sci 19:238–243
Rohrer B, Stell WK (1995) Localization of putative dopamine D2-like receptors in the chick retina, using in situ hybridization and immunocytochemistry. Brain Res 695:110–116
Bresnick GH (1986) Diabetic macular edema. A review. Ophthalmology 93:989–997
Lopes de Faria JM, Jalkh AE, Trempe CL, McMeel JW (1999) Diabetic macular edema: risk factors and concomitants. Acta Ophthalmol Scand 77:170–175
Gao G, Li Y, Zhang D, Gee S, Crosson C, Ma J (2001) Unbalanced expression of VEGF and PEDF in ischemia-induced retinal neovascularization. FEBS Lett 489:270–276
Petrova TV, Makinen T, Alitalo K (1999) Signaling via vascular endothelial growth factor receptors. Exp Cell Res 253:117–130
Battegay EJ (1995) Angiogenesis: mechanistic insights, neovascular diseases, and therapeutic prospects. J Mol Med 73:333–346
Pierce EA, Avery RL, Foley ED, Aiello LP, Smith LE (1995) Vascular endothelial growth factor/vascular permeability factor expression in a mouse model of retinal neovascularization. Proc Natl Acad Sci USA 92:905–909
Senger DR, Connolly DT, Water L van de, Feder J, Dvorak HF (1990) Purification and NH2-terminal amino acid sequence of guinea pig tumor-secreted vascular permeability factor. Cancer Res 50:1774–1778
Adamis AP, Miller JW, Bernal MT et al. (1994) Increased vascular endothelial growth factor levels in the vitreous of eyes with proliferative diabetic retinopathy. Am J Ophthalmol 118:445–450
Aiello LP, Avery RL, Arrigg PG et al. (1994) Vascular endothelial growth factor in ocular fluid of patients with diabetic retinopathy and other retinal disorders. N Engl J Med 331:1480–1487
Pe’er J, Shweiki D, Itin A, Hemo I, Gnessin H, Keshet E (1995) Hypoxia-induced expression of vascular endothelial growth factor by retinal cells is a common factor in neovascularizing ocular diseases. Lab Invest 72:638–645
Aiello LP, George DJ, Cahill MT et al. (2002) Rapid and durable recovery of visual function in a patient with von hippel-lindau syndrome after systemic therapy with vascular endothelial growth factor receptor inhibitor su5416. Ophthalmology 109:1745–1751
Ryan AM, Eppler DB, Hagler KE et al. (1999) Preclinical safety evaluation of rhuMAbVEGF, an antiangiogenic humanized monoclonal antibody. Toxicol Pathol 27:78–86
Via LE, Gore-Langton RE, Pluda JM (2000) Clinical trials referral resource. Current clinical trials administering the antiangiogenesis agent SU5416. Oncology (Huntington) 14:1321–1323
Engerman RL (1976) Animal models of diabetic retinopathy. Trans Am Acad Ophthalmol Otolaryngol 81:OP710–OP715
Miyamoto K, Khosrof S, Bursell SE et al. (1999) Prevention of leukostasis and vascular leakage in streptozotocin-induced diabetic retinopathy via intercellular adhesion molecule-1 inhibition. Proc Natl Acad Sci USA 96:10836–10841
Aiello LP, Bursell SE, Clermont A et al. (1997) Vascular endothelial growth factor-induced retinal permeability is mediated by protein kinase C in vivo and suppressed by an orally effective beta-isoform-selective inhibitor. Diabetes 46:1473–1480
Acknowledgements
This study was supported in part by NIH grants EY12231, EY015650 (J-XM) and EY-13520 (BR) and by research awards from Juvenile Diabetes Foundation, American Diabetes Association and South Carolina Lions Club.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zhang, S.X., Sima, J., Shao, C. et al. Plasminogen kringle 5 reduces vascular leakage in the retina in rat models of oxygen-induced retinopathy and diabetes. Diabetologia 47, 124–131 (2004). https://doi.org/10.1007/s00125-003-1276-4
Received:
Revised:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-003-1276-4