Abstract
Objective
To assess the clinical significance of nasal nitric oxide (nNO) and fractional exhaled nitric oxide (FeNO) concentrations in children with sleep-disordered breathing (SDB).
Methods
Enrolled in this study were 30 children with SDB and 15 healthy children. The nNO and FeNO concentrations were measured noninvasively using a NIOX MINO system (Aerocrine AB, Solna, Sweden). SPSS statistics 20.0 software (IBM SPSS statistics 20.0, Armonk, NY, USA) was used to analyze the data.
Results
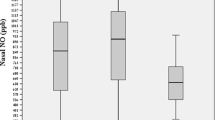
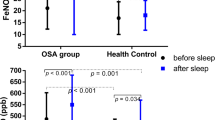
The median (25th and 75th percentiles) nNO concentration of SDB children measured in parts per billion (ppb) was 111.0 (44.0; 349.0) ppb; FeNO concentration of SDB children was 12.0 (9.8; 14.0) ppb. The nNO concentration of healthy children was 52.0 (22.0; 139.0) ppb; FeNO concentration of healthy children was 12.0 (10.0; 16.0) ppb. Compared to healthy children, nNO concentration was significantly higher in children with SDB (Z = −2.215, P = 0.027). Correlation analysis showed that SDB children’s nNO concentration directly correlated with apnea–hypopnea index (AHI; r = 0.429, P = 0.018), and inversely correlated with nadir oxygen saturation (SaO2; r = −0.482, P = 0.007). No other polysomnographic parameters significantly correlated with nNO concentration.
Conclusion
Our data suggest that nNO concentration might be useful for diagnosis and evaluation of disease severity in SDB children. Furthermore, these results suggest that nNO concentration has a greater prognostic value than FeNO concentration.
Zusammenfassung
Ziel
Ziel war die Bestimmung der klinischen Bedeutung der nasalen Stickstoffmonoxid- („nasal nitric oxide“, nNO) und der fraktionierten exhalierten Stickstoffmonoxidkonzentration („fractional exhaled nitric oxide“, FeNO) bei Kindern mit schlafbezogenen Atemstörungen (SBAS).
Methoden
An der Studie nahmen 30 Kinder mit SBAS und 15 gesunde Kinder teil. Die nNO- und die FeNO-Konzentration wurden nichtinvasiv unter Einsatz des Systems NIOX MINO® (Fa. Aerocrine AB, Solna, Schweden) gemessen. Für die Auswertung der Daten wurden die Software SPSS Statistics 20.0 (IBM SPSS Statistics 20.0, Armonk/NY, USA) verwendet.
Ergebnisse
Die nNO-Konzentration der Kinder mit SBAS lag bei 111,0 (44,0; 349,0) ppb („parts per billion“, 10-9) im Median (25. und 75. Perzentile). Die FeNO-Konzentration der Kinder mit SBAS betrug 12,0 (9,8; 14,0) ppb. Dagegen lag die nNO-Konzentration der gesunden Kinder bei 52,0 (22,0; 139,0) ppb. Die FeNO-Konzentration der gesunden Kinder betrug 12,0 (10,0; 16,0) ppb. Im Vergleich zu gesunden Kindern war die nNO-Konzentration bei Kindern mit SBAS signifikant höher (z =−2,215; p =0,027). Die Korrelationsanalyse zeigte, dass die nNO-Konzentration der Kinder mit SBAS direkt mit dem Apnoe-Hypopnoe-Index (AHI) korreliert war (r =0,429; p =0,018), eine umgekehrte Korrelation bestand mit dem Nadir der arteriellen Sauerstoffsättigung (SaO2; r =−0,482; p =0,007). Jedoch war die nNO-Konzentration nicht signifikant mit anderen polysomnographischen Parametern korreliert.
Schlussfolgerung
Den vorliegenden Daten zufolge ist die nNO-Konzentration möglicherweise nützlich für die Diagnosestellung und die Beurteilung des Schweregrads bei Kindern mit SBAS. Darüber hinaus ist nach den vorliegenden Ergebnissen die nNO-Konzentration dabei von höherer prognostischer Aussagekraft als die FeNO-Konzentration.




Similar content being viewed by others
References
Mahr TA, Malka J, Spahn JD (2013) Inflammoeometry in pediatric asthma: a review of fractional exhaled nitric oxide in clinical practice. Allergy Asthma Proc 34(3):210–219
Culla B, Guida G, Brussino L et al (2010) Increased oral nitric oxide in obstructive sleep apnoea. Respir Med 104:316–320
Torretta S, Bossi A, Capaccio P et al (2010) Nasal nitric oxide in children with adenoidal hypertrophy: A preliminary study. Int J Pediatr Otorhinolaryngol 74:689–693
Riva Tauman MD, Louise M et al (2004) Sleep pressure score: a new index of sleep disruption in snoring children. Sleep 27(2):274–278
Petrosyan M, Perraki E, Simoes D et al (2008) Exhaled breath markers in patients with obstructive sleep apnoea. Sleep Breath 12:207–215
Foresi A, Leone C, Olivieri D, Cremona G (2007) Alveolar-derived exhaled nitric oxide is reduced in obstructive sleep apnea syndrome. Chest 132:860–867
Berry RB, Brooks R, Gamaldo CE et al (2012) The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications, version 2.0. American Academy of Sleep Medicine, Darien
Franco RA, Rosenfeld RM, Rao M (2000) First place-resident clinical science award 1999. Quality of life for children with obstructive sleep apnea. Otolaryngol Head Neck Surgery 123:9–16
Bove PF, Van der Vliet A (2006) Nitric oxide and reactive nitrogen species in airway epithelial signaling and inflammation. Free Radic Biol Med 41(4):515–527
Scadding G, Scadding GK (2009) Update on the use of nitric oxide as a noninvasive measure of airways inflammation. Rhinology 47(2):115–120
Friberg D, Ansved T, Borg K, Carlsson-Nordlander B, Larsson H, Svanborg E (1998) Histological indications of a progressive snorers disease in an upper airway muscle. Am J Respir Crit Care Med 157(2):586–593
Olopade CO, Christon JA, Zakkar M et al (1997) Exhaled pentane and nitric oxide levels in patients with obstructive sleep apnea. Chest 111:1500–1504
Goldbart AD, Goldman JL, Li RC, Brittian KR, Tauman R, Gozal D (2004) Differential expression of cysteinyl leukotriene receptors 1 and 2 in tonsils of children with obstructive sleep apnea syndrome or recurrent infection. Chest 126:13–18
Depalo A, Carpagnano GE, Spanevello A et al (2008) Exhaled NO and iNOS expression in sputum cells of healthy, obese and OSA subjects. J Intern Med 263(1):70–78
Chua AP, Aboussouan LS, Minai OA et al (2013) Long-term continuous positive airway pressure therapy normalizes high exhaled nitric oxide levels in obstructive sleep apnea. J Clin Sleep Med 15;9(6):529–535
Berry RB, Gleeson K (1997) Respiratory arousal from sleep: mechanisms and significance. Sleep 20:654–675
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Y. Huang, Y. Zou, F. Mai, X. Zhang, Y. Liu, and X. Lin state that there are no conflicts of interest.
All studies on humans described in the present manuscript were carried out with the approval of the responsible ethics committee and in accordance with national law and the Helsinki Declaration of 1975 (in its current, revised form). Informed consent was obtained from all patients included in studies.
Additional information
Redaktion
P.K. Plinkert, Heidelberg
B. Wollenberg, Lübeck
Yaping Huang and Yu Zou contributed equally to this manuscript.
Rights and permissions
About this article
Cite this article
Huang, Y., Zou, Y., Mai, F. et al. Sleep-disordered breathing children. HNO 64, 169–174 (2016). https://doi.org/10.1007/s00106-016-0120-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00106-016-0120-3