Abstract
Background
In recent years, ultrasound (US) has become more incorporated into anesthesia and intensive care medicine. The German Anesthesia Society established a modular curriculum to teach US skills. Until now, the efficacy of this modular curriculum has not been validated.
Objective
The main objective of this study was to determine whether there is an increase of knowledge and of psychomotor skills for the trainees in this curriculum.
Material and methods
After ethical committee approval, 41 anesthesia physicians were enrolled. To determine the increase of knowledge and of practical skills theoretical and practical tests performed were evaluated before and after two different US courses.
Results
Comparing before and after course tests, the participants showed significant improvement in theoretical multiple choice tests (p = 0.008). Regarding psychomotor skills following course 1, the trainees improved significantly in the time needed to perform the two practical tests (p = 0.03), but not in the performance of the test. Better needle visualization during simulated US-guided vessel puncture (p = 0.52) and better identification of the anatomical structures in the axillary region (p = 0.56) could not be achieved.
Conclusion
This study shows that although this US course curriculum has positively enhanced the trainees’ theoretical knowledge of US practice, it does not enhance the practical application of that theoretical knowledge. To improve this curriculum, a supervised clinically practical training should follow the course.
Zusammenfassung
Hintergrund
Ultraschall (US) hat in den letzten Jahren zunehmend Einzug in die Anästhesie und Intensivmedizin erhalten. Die Deutsche Gesellschaft für Anästhesiologie & Intensivmedizin hat ein modulares Kurssystem zur Vermittlung von US-Kompetenzen entwickelt. Die Wirksamkeit dieses modularen Curriculums wurde bisher nicht validiert.
Ziel
Ziel dieser Studie war zu ermitteln, ob es bei den Teilnehmern durch den Besuch von Modulen dieses Kurssystems zu einer Verbesserung theoretischer Kenntnisse und praktischer Fertigkeiten kommt.
Material und Methode
Nach Zustimmung durch die Ethikkommission wurden 41 Anästhesisten in die Studie eingeschlossen. Um den Zugewinn an Wissen und praktischen Fertigkeiten zu ermitteln, wurden theoretische und praktische Tests vor und nach zwei verschiedenen US-Kursen ausgewertet.
Ergebnisse
Nach den Kursen zeigten die Teilnehmer eine signifikante Verbesserung in den Ergebnissen der Multiple-Choice-Tests (p = 0,008). Hinsichtlich der psychomotorischen Fähigkeiten nach Kurs 1 verbesserten sich die Teilnehmer in der zur Durchführung der beiden praktischen Tests benötigten Zeit signifikant (p = 0,03), nicht aber in der Durchführung der Tests. Die praktischen Aufgaben konnten nach dem Kurs 1 zwar signifikant schneller durchgeführt werden (p = 0,03), die Qualität der Nadelführung (p = 0,52) und die korrekte Benennung anatomischer Strukturen in der Achselregion konnten aber nicht verbessert werden.
Schlussfolgerung
Diese Studie zeigt, dass obwohl dieses Kurssystem die theoretischen Kenntnisse über die US-Praxis verbessert hat, die praktische Anwendung dieses theoretischen Wissens aber nicht verbessert werden konnten. Um dieses Curriculum zu verbessern, sollte es von einem praktischen Training unter Anleitung ergänzt werden.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
In recent years, ultrasound (US) has become incorporated into anesthesia and intensive care medicine because it is a useful, non-invasive, portable, and relatively low-cost diagnostic imaging method and guiding tool for procedures [3]. Healthcare providers need to be trained in order to incorporate new procedures into routine clinical practice. Psychomotor skills are best acquired using a sequenced and step-by-step teaching approach [20]. There are a variety of widely accepted and published teaching models advanced by Fitts, Simpson and Posner [21]. The number of teaching steps used in these models varies from 2 to 11 [21]. Taking the various teaching models into account, many specialized programs and workshops have been designed to teach sonographic techniques to novice operators. Until now, no program has been found to be superior to the other. American and European guidelines have been published to offer assistance in the organization of US teaching programs [27]. In addition, for critical care sonography two international expert statements have acknowledged the challenges in providing appropriate training in echography and critical care US [8, 19]. In Germany this increased use has led to the introduction of an US curriculum in teaching programs. In 2011, the German Society of Anaesthesiology and Intensive Care Medicine (DGAI) established a modular curriculum called anesthesia-focused sonography (AFS) [4, 14, 25, 28, 29]. The first module covers basic aspects of the physical principles behind US, system and transducer technology as well as principles of doppler sonography [4]. The second module deals with vascular sonographic techniques and options for further use [29] and the third module with US for regional anesthesia [14]. Module 4 focuses on transthoracic echocardiography (TTE) [28] and module 5 on the sonography of the thorax and abdomen [25]. Module 4 was revised after conducting this study in 2017 and is now integrated into a new training concept called “Perioperative fokussierte Echokardiographie in der Anästhesiologie und Intensivmedizin (PFE, perioperative focused echocardiography in anesthesiology and intensive care)”. This new curriculum consists of five modules and has a distinct theoretical and practical division [11]. The AFS curriculum of the German society is a combination of didactic lectures followed by a two-step instructional approach to teach psychomotor skills in the form of hands-on training. Following the course, practitioners receive an attendance confirmation. A certification after additional clinical teaching is not issued. There is an option for obtaining various, however not validated degrees of a certification, provided by the interdisciplinary German Society of Ultrasound in Medicine (DEGUM). To our knowledge, the efficacy of the AFS modular curriculum of the DGAI has not been validated to date. Performing US based psychomotor skills requires the operator to develop visuomotor and visuospatial skills [20]. Probably, these skills cannot be learned through hands-on training sessions only, but only in the context of everyday clinical practice. Therefore, the main objective of this study was to determine if there is a relevant increase of knowledge and of psychomotor skills for the participants of the AFS curriculum.
Material and methods
The ethics committee of the Ludwig-Maximilians-University Munich (ethics committee number 593-16) approved the study, and participants provided written informed consent. For this monocentric prospective study 41 anesthesiologists of the University Hospital of Munich were enrolled. The anesthesiologists had different prior practical experience in sonography; the only exclusion criterion was earlier participation in certified US courses. Of these participants, 22 followed AFS modules 1–3 and 19 AFS modules 4–5. Modules 1–3 were held in a 2-day course in November 2016 (course 1), and modules 4 and 5 in a 2-day course in February 2017 (course 2). Because of the different focus of the two courses, prior participation in course 1 was not mandatory in order to attend course 2.
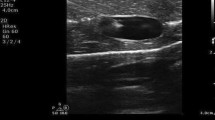
To assess baseline knowledge, all participants of course 1 filled out a 15-question multiple choice test in the hospital without external sources of information 1 week before participating in the courses (the multiple choice test is provided as a supplement). In brief, the multiple choice test was created in Microsoft Word (Microsoft Corporation, Redmond, WA, USA). A maximum of 30 points could be achieved. Together with the multiple choice test, all participants performed two practical exercises to assess psychomotor skills. To test visuomotor skills, a longitudinal (in-plane) puncture technique [6] was used on a custom made puncture model (Fig. 1). The goal of the task was to penetrate a noodle (Barilla, Tortiglioni, 9 mm; Barilla, Parma, Italy) embedded in gelatine at 3 cm depth with the tip of a regional anesthesia needle (Uniplex NanoLine, PajunkⓇ, Geisingen, Germany) using an in-plane puncture technique and to confirm that the tip of the needle is in the required position. A 38 mm 10–12 Hz linear transducer was used to visualize the real-time track of the needle to the target. An intervention imaging preset was selected which used a grey scale map with a frame rate of 24.5 frames per second and one focal zone. First, the time needed to complete the skill was measured (test 1). The time was started when the needle was picked up by the trainee and stopped when the trainee stated that the needle was inside the lumen of the noodle in the required position. This essentially mirrors the clinical use of US, as in a clinical setting there is no instructor to state whether the needle is in the correct place. It is up to the judgment of the operator and whether he considers the puncture to be successful. The time was only utilized for further analysis if the tip of the needle was correctly inside the noodle. Otherwise the task was considered incorrectly performed and this was recorded in the data. An instructor rated the task as 0 when during the entire procedure the needle tip and the shaft were never observed on two dimensional (2D) real-time visualization, as 1 when the needle shaft but not the tip was observed, as 2 when the needle tip but not the shaft was observed, and a mark of 3 was obtained when both the tip of the needle and shaft were continually observed.
To test visuospatial skills, the trainees had to demonstrate a 2D image of the axillary brachial plexus on a human model (test 2) visualizing prespecified structures. All participants performed the skill on the same human model. To obtain the best view of the brachial plexus a linear transducer was to be placed in the transverse plane at the lateral border of pectoralis major muscle. To optimize image quality, appropriate depth, focus range and gain had to be set by the operator. The structures of interest for this task were the axillary artery, the axillary veins, and the four terminal branches of the brachial plexus: the median (superficial and lateral to the artery), the ulnar (superficial and medial to the artery) and radial (posterior and lateral or medial to the artery) and the musculocutaneous (between the biceps and coracobrachialis muscles) nerves. Once the trainees were able to display all anatomical structures of interest on a 2D image, they had to print this image and correctly label the anatomical structures displayed on the printout. For each correctly identified anatomical structure, 0.5 points were allocated and a maximum of 3 points could be achieved. In addition, the time taken to create the image was measured. The time was started when the operator picked up the transducer and stopped when printing of the image was started.
To determine the increase of knowledge and of performance in psychomotor skills, the multiple choice test with identical questions in a randomized order plus the skills tests were repeated 1 week after the course. The following results were examined for each assessment: scores of the multiple choice tests, time to successfully perform test 1, the scores for needle visualization of test 1, time to successfully perform a 2D image of the axillary brachial plexus visualizing the aforementioned structures of interest, and scores of the anatomical structures visualized in the trainee made images.
For the pretest and posttest of course 2, a presentation in Microsoft PowerPoint (Microsoft Corporation) with a 20-question multiple choice test regarding the evaluation of US sequences or images were created. The questions were related to the topics covered by the AFS modules 4 and 5 and are provided as a supplement. The participants could access the computer-based diagnostic test under their clinic account, but the answers were marked on an enclosed answer sheet. Multiple answers were possible. The numbers of correct answers were not stated in the question. If the question was answered completely correct, 2 points were given, with partially correct answers being worth 1 point and 0 point for no correct answer. Consequently, a maximum of 40 points could be achieved. To assess baseline knowledge and increase of knowledge the pretest and posttest were respectively performed 1 week before and after the course.
The topics covered in course 1 allowed the participants to test their newly learned practical skills on healthy human models. Course 2 contained more pathological findings, and hence it was not possible for the participants to test their practical skills on healthy human models. During the course, hands-on training was organized in a rotation system, where trainee groups moved to the next station after a defined time frame of 25 min. Each station focused on a different task. The sessions were designed for small teaching groups with a maximum of five trainees on one instructor in order to guarantee 5min of teaching per trainee per station. The instructors did not rotate.
Statistical analysis was performed by using GraphPad Prism 5 (GraphPad Software, La Jolla, CA, USA). We evaluated the data for normal distribution with the Shapiro-Wilk test. In the case of normal distribution, the values are represented as mean (standard deviation, SD), otherwise as median (25th/75th percentile). Paired-t-test or the Mann-Whitney U-test were used to compare the values. All reported p-values are 2‑tailed. P-values <0.05 were considered statistically significant.
Results
Demographic characteristics of the study participants are shown in Table 1. The trainees did not differ in age and anesthesia work experience in both courses and we found no age or work experience differences within the course groups. In course 2 two participants did not give any information about gender and age. In course 1 the participants achieved an average of 16.10 (SD 2.98) points in the multiple choice pretest, in the posttest an average of 21.86 (SD 3.68) was reached. The improvement of the score (Fig. 2) was statistically significant (p < 0.0001).
For test 1 (Fig. 3), no trainee failed to perform the task. The participants improved significantly in the time needed to complete the skill from an average of 56s (25/75 percentiles: 39/79.50s) seconds in the pretest to an average of 36s (25/75 percentile: 22/50s) seconds in the posttest (p = 0.03). However, the quality of the needle visualization did not improve between the pretest (2, 25/75 percentile: 2/2.5) and the posttest (2, 25/75 percentile: 2/3) (p = 0.52). For test 2 (Fig. 4), the time to create a 2‑dimensional image of the axillary brachial plexus improved from 140.90s (SD 77.99s) to 73.50s (25/75 percentile: 60/103.5s) seconds (p = 0.03). No significant improvement was achieved in the correct identification of the anatomical structures from the pretest (1.45, SD 1.01) to the posttest (1.53, SD 0.72) (p = 0.56). In course 2, the participants improved in the computer-based diagnostic test (Fig. 5) from an average of 23.80 (SD 4.78) points in the pretest, to an average of 29.23 (SD 3.05) points in the posttest (p = 0.008).
Discussion
This study demonstrates that a modular US curriculum with didactic lectures and hands on training may be helpful in teaching US use for anesthesiologists, as trainees had significant improvement in their theoretical knowledge and in the time needed to perform psychomotor skills; however, an improvement in needle visualization in a visuomotor skill and in identification of correct anatomical structures in a visuospatial skill could not be achieved.
Sonographic techniques are challenging to learn. Learning US requires the integration of multiple skill sets including identification of appropriate patients, image acquisition, image interpretation, and integration of findings into the clinical management of patients [18]. To perform medical sonographic examinations, the use of psychomotor skills is crucial. Central components of medical US imaging are visuomotor and visuospatial psychomotor skills [20]. These skills are best acquired in stages using a sequenced and stepped teaching approach. Therefore, critical care US programs include didactic teaching, direct supervision and maintenance of a logbook [9]. Unlike other programs, the German AFS sonography curriculum includes a combination of both didactic lectures and hands-on training. An attendance confirmation is provided but without proof of clinical practical training. For this reason, we tried to show whether or not an US course without subsequent retraining in daily clinical practice improves participants’ knowledge and psychomotor skills. We were able to show that these skills can only partially be improved by the given US courses. The trainees improved significantly in the time needed to perform the tasks, but not in puncture quality and in correctly identifying anatomical structures. In contrast, theoretical knowledge improved significantly. Consequently, we do not feel that completion of this course is sufficient to perform independently US for regional anesthesia or for diagnostic purposes.
In this study, psychomotor skills were practiced by the trainee immediately after lecture demonstration. The instructors followed a traditional two-step model to teach psychomotor skills. After a short demonstration of the skill the instructor acted mainly as a coach, following instructional strategies relevant for teaching complex skills in US [18, 21]. Despite frequent hands-on training during the course, it seems likely that an improvement in psychomotor skills can only be achieved through everyday clinical practice. Indeed, a longitudinal US curriculum, compared to a single stand-alone workshop, improved the ability of internal medical residents to correctly identify static US images at 6 months [15]. In addition, after 1 year of training point of care sonography anesthesiology residents can successfully acquire images of acceptable quality [24]. Interestingly, the greatest improvements in quality and acquisition time were for vascular access and pulmonary US. In an emergency medicine study, physicians acquired the ability to interpret focused assessment with sonography in trauma (FAST) images earlier than the technical skills required to actually perform the examination. The incidence of specific technical errors improved with hands-on experience [12]. From this study it was concluded that more than 60 examinations are needed to reduce the incidence of technical errors below 5%. In contrast, for focused TTE, other studies have demonstrated that it can be performed by novice practitioners with minimal training only [13, 23]. As in our course, the goals were achieved using a combination of both didactic lectures and small group skills training, which were practiced by the learner immediately after the initial lecture demonstration to facilitate the clinical expertise and skill reinforcement [23]. In addition, an only 60-min didactic presentation on TTE for intensive care unit (ICU) trainees may be useful in teaching basic TTE skills and encouraging the use of bedside TTE in the ICU [17]. Such a short didactic presentation was chosen, because the authors proposed that one of the most common barriers to implementing TTE education is the lack of time. The barriers to delivering a high-quality training program are often the lack of trainers and no spare time for further medical training [9]. The major challenge in the posttest was to perform better in describing anatomical structures correctly and in better needle visualization in our puncture model. Although all participants have entered the noodles without continuous needle visualization thereby saving time, advancing the needle without observing the needle tip is not recommended due to a higher complication rate during vascular access procedures and also during regional anesthesia [26]. To improve these practical skills it seems mandatory, that clinical experience must be supported by a trainer and supervised by an expert and, thus, constantly mentored after an US course. Effectiveness of the educational modality used in sonographic training merits further investigation. Delivery of didactic teaching varies between face to face courses and online teaching modules, and differs in the duration and structure. Model simulation education strategies may improve training more than standardized didactic lectures. Videoclip-based pathology lectures may improve content retention [24]. These two education strategies are also used for the AFS curriculum. They could perhaps be extended by exercises on real patients in order to improve practical skills. It has been shown that education taught on non-ideal, real-world patients and not healthy volunteers can increase the efficacy of learning [17]. In addition, novices’ sonographic skills showed greater improvement when feedback was combined with validated metrics [1]. Systematic reviews have shown that simulation-based training in health care is significantly more effective than alternative teaching methods or no intervention [7]. Simulation-based medical education training was effective in improving short and long-term competency in, and knowledge of central venous catheter insertion [5]. Most likely for lack of time, the AFS curriculum does not incorporate this teaching methodology; however, the new PFE curriculum includes US simulators as an optional tool and it could be an additional methodology in the context of clinically practical training also in the other AFS modules. As an alternative to the two-step model used during the hands-on training, other step-by-step instructional models could perhaps improve the training modules. The efficacy of using different step-by-step instructional models to teach psychomotor skills is subject of ongoing debate. When using the five-step George and Doto model or the Walker and Peyton four-step model, simple skill acquisition was significantly enhanced in studies [30, 31]. In contrast, other studies comparing different skill teaching models identified no significant differences in cases of complex skill acquisition [2, 10, 16, 22]. Because of this paucity of evidence it does not seem necessary to change the use of the two-step model.
Limitations
The study has several limitations. First, it was conducted at a single center, which limits generalizability. Moreover, additional ultrasound exposure during the follow-up period after the course was not accounted for. Finally, we did not provide long-term follow-up to assess skill retention. Nevertheless, we have for the first time scientifically assessed the efficacy of the AFS curriculum of the DGAI. We show that the AFS curriculum provides improvement in theoretical US knowledge but needs improvement in teaching practical skills.
Conclusion
This study showed that although the AFS US course curriculum has positively enhanced the trainees’ knowledge of US practice, it did not enhance the practical application of that knowledge. The trainees could not improve their performance in the implementation of psychomotor skills. As a supplement to the AFS curriculum, a systematic practical training of sonographic techniques should follow the course. This could be provided by routine clinical work under supervision, or by special courses including simulation-based training. Further studies should aim to analyze the duration of this additional practical trainings.
References
Ahmed OMA, Niessen T, O’Donnell BD et al (2017) The effect of metrics-based feedback on acquisition of sonographic skills relevant to performance of ultrasound-guided axillary brachial plexus block. Anaesthesia 72:1117–1124
Archer E, van Hoving DJ, de Villiers A (2015) In search of an effective teaching approach for skill acquisition and retention: teaching manual defibrillation to junior medical students. Afr J Emerg Med 5:54–59
Baltarowich OH, Di Salvo DN, Scoutt LM et al (2014) National ultrasound curriculum for medical students. Ultrasound Q 30:13–19
Bleise S, Einhaus F, Pfeiffer K et al (2011) DGAI-certified course series anaesthesia focused sonography: module 1: basics of sonography. Anasthesiol Intensivmed Notfallmed Schmerzther 46:750–754
Cartier V, Inan C, Zingg W et al (2016) Simulation-based medical education training improves short and long-term competency in, and knowledge of central venous catheter insertion: a before and after intervention study. Eur J Anaesthesiol 33:568–574
Chapman GA, Johnson D, Bodenham AR (2006) Visualisation of needle position using ultrasonography. Anaesthesia 61:148–158
Cook DA, Brydges R, Zendejas B et al (2013) Technology-enhanced simulation to assess health professionals: a systematic review of validity evidence, research methods, and reporting quality. Acad Med 88:872–883
Expert Round Table on Ultrasound in ICU (2011) International expert statement on training standards for critical care ultrasonography. Intensive Care Med 37:1077–1083
Galarza L, Wong A, Malbrain MLNG (2017) The state of critical care ultrasound training in Europe: a survey of trainers and a comparison of available accreditation programmes. Anaesthesiol Intensive Ther 49:382–386
Greif R, Egger L, Basciani RM et al (2010) Emergency skill training—a randomized controlled study on the effectiveness of the 4‑stage approach compared to traditional clinical teaching. Resuscitation 81:1692–1697
Greim CA, Weber S, Göpfert M (2017) Perioperative fokussierte Echokardiographie in der Anästhesiologie und Intensivmedizin. Neues Fortbildungskonzept und Modifikation des TEE-Zertifikats. Anasth Intensivmed 58:616–648
Jang T, Kryder G, Sineff S et al (2012) The technical errors of physicians learning to perform focused assessment with sonography in trauma. Acad Emerg Med 19:98–101
Jones AE, Tayal VS, Kline JA (2003) Focused training of emergency medicine residents in goal-directed echocardiography: a prospective study. Acad Emerg Med 10:1054–1058
Kefalianakis F, Döffert J, Hillmann R et al (2011) The DGAI training module 3 in anaesthetic focussed sonography: neurosonography. Anasthesiol Intensivmed Notfallmed Schmerzther 46:760–765
Kelm DJ, Ratelle JT, Azeem N et al (2015) Longitudinal ultrasound curriculum improves long-term retention among internal medicine residents. J Grad Med Educ 7:454–457
Krautter M, Weyrich P, Schultz J‑H et al (2011) Effects of Peyton’s four-step approach on objective performance measures in technical skills training: a controlled trial. Teach Learn Med 23:244–250
Kuza CM, Hanifi MT, Koç M, Stopfkuchen-Evans M (2018) Providing transthoracic echocardiography training for intensive care unit trainees: an educational improvement initiative. J Surg Educ. https://doi.org/10.1016/j.jsurg.2018.03.004
Landry A, Eicken J, Dwyer K et al (2017) Ten strategies for optimizing ultrasound instruction for group learning. Cureus 9:e1129
Mayo PH, Beaulieu Y, Doelken P et al (2009) American College of Chest Physicians/La Société de Réanimation de Langue Française statement on competence in critical care ultrasonography. Chest 135:1050–1060
Nicholls D, Sweet L, Hyett J (2014) Psychomotor skills in medical ultrasound imaging: an analysis of the core skill set. J Ultrasound Med 33:1349–1352
Nicholls D, Sweet L, Muller A, Hyett J (2016) Teaching psychomotor skills in the twenty-first century: revisiting and reviewing instructional approaches through the lens of contemporary literature. Med Teach 38:1056–1063
Orde S, Celenza A, Pinder M (2010) A randomised trial comparing a 4-stage to 2‑stage teaching technique for laryngeal mask insertion. Resuscitation 81:1687–1691
Price S, Ilper H, Uddin S et al (2010) Peri-resuscitation echocardiography: training the novice practitioner. Resuscitation 81:1534–1539
Ramsingh D, Rinehart J, Kain Z et al (2015) Impact assessment of perioperative point-of-care ultrasound training on anesthesiology residents. Anesthesiology 123:670–682
Röhrig S, Seibel A, Zechner P et al (2011) DGAI-zertifizierte Seminarreihe Anästhesie Fokussierte Sonografie – Modul 5: Thorakoabdominelle Sonografie (E-FAST plus). Anasthesiol Intensivmed Notfallmed Schmerzther 46:772–781
Scholten HJ, Pourtaherian A, Mihajlovic N et al (2017) Improving needle tip identification during ultrasound-guided procedures in anaesthetic practice. Anaesthesia 72:889–904
Sites BD, Chan VW, Neal JM et al (2010) The American Society of Regional Anesthesia and Pain Medicine and the European Society of Regional Anaesthesia and Pain Therapy joint committee recommendations for education and training in ultrasound-guided regional anesthesia. Reg Anesth Pain Med 35:S74–S80
Tonner P, Bein B, Breitkreutz R et al (2011) DGAI-zertifizierte Seminarreihe Anästhesie Fokussierte Sonografie – Modul 4: Kardiosonografie. Anasthesiol Intensivmed Notfallmed Schmerzther 46:766–770
Trautner H, Markus CK, Steinhübel B et al (2011) The DGAI training module 2 in anaesthetic focussed sonography: vascular sonography. Anasthesiol Intensivmed Notfallmed Schmerzther 46:756–759
Virdi MS, Sood M (2011) Effectiveness of a five-step method for teaching clinical skills to students in a dental college in India. J Dent Educ 75:1502–1506
Wang TS, Schwartz JL, Karimipour DJ et al (2004) An education theory-based method to teach a procedural skill. Arch Dermatol 140:1357–1361
Acknowledgements
We thank Mr. Xaver Marstaller for editing the manuscript.
Funding
No external funding was obtained for this study. This study was supported by departmental funding only.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Funding
Open Access funding provided by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
Author contributions
RT helped perform the study and collect data. In addition, RT analyzed and interpreted the data and wrote the paper. KS performed the study, collected and analyzed the data. PS designed and performed the study, helped collect data and helped write the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
R. Tomasi, K. Stark and P. Scheiermann declare that they have no competing interests.
All procedures performed in studies involving human participants or on human tissue were in accordance with the ethical standards of the institutional and/or national research committee and with the 1975 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study. The ethics committee of the Ludwig-Maximilians-University Munich (ethics committee number 593-16) approved the study.
Caption Electronic Supplementary Material
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tomasi, R., Stark, K. & Scheiermann, P. Efficacy of a certified modular ultrasound curriculum. Anaesthesist 69, 192–197 (2020). https://doi.org/10.1007/s00101-020-00730-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00101-020-00730-9
Keywords
- Ultrasound in anesthesia
- Modular ultrasound curriculum
- Certified ultrasound course
- Ultrasound teaching
- AFS curriculum