Abstract
Introduction
Pelvic fractures were often associated with high-energy trauma in young patients, but data show a significant increase in osteoporotic pelvic fractures in old age due to the progressive demographic change. There is an ongoing discussion about the best fixation techniques, which are ranging from lumbopelvic fixation to sacral bars or long transiliac–transsacral (TITS) screws. This study analyzes TITS screw osteosynthesis and sacroiliac screw osteosynthesis (SI), according to biomechanical criteria of fracture stability in osteoporotic human pelvic cadavers ex vivo.
Methods
Ten osteoporotic cadaveric pelvises were randomized into two groups of 5 pelvises each. An FFP-IIc fracture was initially placed unilaterally and subsequently surgically treated with a navigated SI screw or a TITS screw. The fractured side was loaded in a one-leg stance test setup until failure. Interfragmentary movements were assessed by means of optical motion tracking.
Results
No significant difference in axial stiffness were found between the SI and the TITS screws (21.2 ± 4.9 N and 18.4 ± 4.1 N, p = 0.662). However, there was a significantly higher stability of the fracture treatment in the cohort with TITS-screws for gap angle, flexion, vertical movement and overall stability. The most significant difference in the cycle interval was between 6.000 and 10.000 for the gap angle (1.62 ± 0.25° versus 4.60 ± 0.65°, p = 0.0001), for flexion (4.15 ± 0.39 mm versus 7.60 ± 0.81 mm, p = 0.0016), interval 11.000–15.000 for vertical shear movement (7.34 ± 0.51 mm versus 13.99 ± 0.97 mm, p < 0.0001) and total displacement (8.28 ± 0.66 mm versus 15.53 ± 1.07 mm, p < 0.0001) for the TITS and the SI screws.
Conclusions
The results of this biomechanical study suggest a clear trend towards greater fracture stability of the TITS screw with significantly reduced interfragmentary movement. The application of a TITS screw for the treatment of the osteoporotic pelvic ring fracture may be prioritized to ensure the best possible patient care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The incidence of pelvic ring fracture, measured as a proportion of all fractures, is low, amounting to 3–8% [1,2,3]. However, entailing high mortality and morbidity, it poses enormous challenges to both the medical and the health care system. Pelvic fractures were often associated with high-energy trauma in young patients, but data show a significant increase in osteoporotic pelvic fractures in old age due the progressive demographic change [4]. To treat these fractures adequately, appropriate therapy algorithms are required. For this purpose, medicine applied existing treatment strategies used for pelvic ring fractures in the young patient, despite significant differences in terms of accident mechanism, fracture morphology, bone quality, and the patient itself [3, 5, 6]. In the geriatric patient, osteosynthesis must not only achieve sufficient fracture stabilization of the osteoporotic pelvic bone ensuring immediate full weight-bearing and allowing full mobilization, but it must also provide an acceptable perioperative risk considering the potentially accompanying multiple comorbidities [7, 8].
An evaluation of the German pelvic register from 1991 to 2003 shows a significant increase in the number of surgically treated cases [9]. However, the type of best surgical therapy continues to be discussed. There is an ongoing discussion about the best fixation techniques, which are ranging from lumbopelvic fixation to sacral bars or long transiliac–transsacral (TITS) screws [10]. Although minimally invasive surgical techniques have been established, literature on biomechanical studies evaluating the fracture stability using these techniques remains scarce up to date [11, 12]. These fixation techniques are well-established in young non-osteoporotic patients. Literature shows also promising long-term results in the treatment of fragility fractures of the pelvis but only in small study populations [7, 13, 14].
Various studies with bone models or embalmed pelvic cadavers can be found in the literature [13, 15,16,17]. Studies on fresh frozen human osteoporotic bones, however, are searched for in vain. This study biomechanically analyzes and compares the most used minimally invasive osteosynthesis procedures, SI and TITS screw osteosynthesis, in an osteoporotic human pelvic cadaveric model.
Materials and methods
Specimens and preparation
Institutional and prior ethical committee approval was obtained prior to the study. All pelvises were from donors who bequeathed their corpses to Science Care (Phoenix, AZ, USA) for use in medical science during their lifetime. Written consent by the patients before the decease or authorized family members is available. All experiments were carried out under the relevant guidelines and regulations of the local institution.
Ten fresh frozen (− 20°) cadaver female pelves from donors aged 87 ± 5 years (mean ± standard deviation, SD) (range 80–94 years) with intact sacroiliac, sacrospinous, sacrotuberous and symphyseal ligaments including the attached fifth lumbar vertebra were considered for biomechanical testing. To provide a consistent result of the biomechanical study, any specimens presenting pre-existent deformations, fractures, neoplasms or degenerative changes in the sacroiliac joint were excluded from the study. Bone mineral density (BMD) was measured before acquisition for each specimen with dual-emission X-ray absorptiometry at the level of S1. Based on BMD, the specimens were randomized into two non-paired groups for instrumentation using either an SI screw or a TITS screw, such that both anatomical sites of each pelvis received the same fixation technique, however, in sequential order comprising preparation, instrumentation and testing of one unilateral anatomical site first. Mean values of both cohorts are shown in Table 1. The Shapiro–Wilk test showed no difference between the groups regarding the distribution.
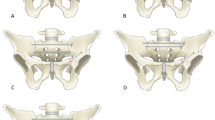
Prior to preparation and biomechanical testing, the specimens were thawed at room temperature for 24 h. Tissue dissection of skin and muscles was done carefully and all ligaments were preserved. After dissection, a fragility fracture of the pelvis (FFP) type IIc was simulated by means of osteotomies using a 1.47 mm oscillating surgical saw [18]. Therefore, the sacrum was cut between the SI-Joint and the neuroforamina in the sacral ala creating a vertical paraforaminal sacrum fracture in zone 1 after Denis classification [19]. Subsequently, the superior and inferior pubic rami were cut approximately 3 cm laterally from the symphysis to discontinue the force transmission to the contralateral hemipelvis site through the anterior pelvic ring during load application.
Under normal operating conditions, the specimens were reduced and treated with either a navigated SI-screw or TITS using a hybrid operating room which consists of a fixed robotic 3D flatpanel detector (Artis zeego, Siemens Healthineers, Germany) and a navigation system (BrainLab Curve, BrainLab, Germany). This ensured an optimal screw pathway for each pelvis. The fractured sacrum was anatomically reduced together with the superior and inferior pubic rami. Fully threaded self-tapping stainless steel 7.3 mm cannulated screws (DePuy Synthes, Zuchwil, Switzerland) were used with a standard washer for fracture fixation. Screw length was chosen specimen individually and according to the group assignment. Whereas for the SI screw fixation technique, care was taken that the screw tip did not cross the midline, for the TITS fixation technique, the screw tip was aimed to perforate all six cortices and extrude from the contralateral ilium. To create a machine fixation point, the L5-vertebrae was embedded in polymethylmethacrylate (PMMA, SCS-Beracryl D-28, Swiss Composite, Jägenstorf, Switzerland) cylinder, such that with the former oriented vertically, the pelvic tilt measured 45°. The fixation was enhanced with 5.0 mm screws. Finally, optical markers were attached to each side of the sacrum and superior ramus fracture, and to the ilium for motion tracking.
Due to the deterioration of the fresh frozen pelvis caused by thawing, two tests in the SI screw group and one test in the TITS screw group could not be completed and were excluded from the final evaluation.
Biomechanical testing
Biomechanical testing was performed on a servo hydraulic material testing system (MTS 858 Bionix, MTS Systems Corp., Eden Prairie, USA) equipped with a 4 kN load cell. Specimens were mounted to the machine in simulated upright standing position by fixing the L5 embedding to the machine transducer via an interconnected hinge joint, allowing for bending moment compensation in flexion–extension. One-leg stance was simulated by transferring the forces generated by the transducer, through the tested hemi-pelvic site to the ipsilateral acetabulum, which was seated on a hip stem with attached hemiarthroplasty component. The latter was firmly constrained to the machine base (Fig. 1).
The loading protocol commenced with an initial quasi-static ramp from 20 N preload to 100 at a rate of 8 N/s, followed by cyclic loading at 3 Hz under a physiological loading profile [20]. Whereas the valley load of 20 N was held constant, the peak load, starting at 100 N, was progressively increased at 0.006 N/cycle until the transducer reached 70 mm displacement with respect to its initial position prior to test start. The latter was found sufficient in a priori pilot tests to provoke failure in the bone-implant constructs and to retrospectively analyze the data for clinically relevant parameters.
After failure, whereas the dislocated fragments of tested anatomical side were anatomically re-aligned and re-fixed at the sacrum by means of 3 SI-Screws, the rami were re-fixed by plating. Subsequently, the procedure of fracture creation, stabilization, and testing was repeated on the contralateral side.
Data acquisition and analysis
Machine data in terms of axial displacement (mm) and load (N) were acquired at 128 Hz. Based on them, the initial construct stiffness was calculated from the ascending load–displacement curve of the initial quasi-static ramp within the load range 50–90 N.
Two optical cameras (Aramis SRX, Carl Zeiss GOM Metrology GmbH, Braunschweig, Germany), operating at 12 Megapixel, continuously recorded the three-dimensional positions of the attached markers at 20 Hz throughout the tests. Based on these, the relative movements between the medial and lateral aspects of the sacrum fracture were analyzed with respect to the marker positions at the beginning of the cyclic test, by means of calculation of the following parameters:
-
(i)
gap angle—angular displacement describing the combined fracture gap opening in frontal and transverse plane;
-
(ii)
flexion—angular displacement describing relative fragment rotation in sagittal plane;
-
(iii)
total displacement—magnitude of the translational displacement of the fracture aspect lying most anteriorly in the fracture gap.
Finally, to visually evaluate the gradual decay of the bone-implant constructs, antero-posterior X-rays were taken with a C-arm (Arcadis Varic, Siemens Healthineers, Erlangen, Germany) at test start, and then intermittently every 500 cycles in peak load condition. For that purpose, the cyclic test was interrupted for 2s in the corresponding load magnitude.
The outcome measures of these parameters were evaluated in peak loading conditions over the first 18,000 cycles in equidistant intervals of 1000 cycles. This range was chosen, because beyond it, the first specimens dropped out due to their failure (Fig. 2).
Statistical analysis was performed with SPSS Statistics (V21.0, IBM, Armonk, NY) and Graphpad (GraphPad Software, La Jolla California USA). Cohorts were tested with the Mann–Whitney U test for independent samples with not normally distributed data. Data pooling was done with time steps from 0 to 5000, 6000 to 10,000 as well as 11,000 to 15,000 cycles. Survival was defined by the failure of osteosynthesis or the maximum dislocation of the fragments, so that a measurement based on the optical markers can no longer be performed. The median survival rate of the implant was calculated using the Kaplan–Meier estimates and tested between the cohorts using a log-rank test. The level of significance was set to 0.05 for all statistical tests.
Results
Axial stiffness
The axial stiffness of the preparations was calculated via the compressive load of the servo-hydraulic testing machine. In order to be able to exclude an initial alignment, only a load interval of 50–90 N was included from the ramp test. This showed a higher stiffness in the long screw group without statistical significance (p = 0.662).
Fracture displacement
Outcome measures for the four parameters measured over the first 180,000 cycles are shown in Fig. 3 for intervals every 1000 and 5000 cycles, as well as for each group separately.
Gap angle, flexion, vertical dislocation and total dislocation. Thin blue lines for every specimen of the TITS group and grey thin lines for SI group. Thick lines show the mean and standard deviation for each group. Bar charts show mean values with standard deviation for the groups every 5000 cycles. **p < 0.01, ***p < 0.001, ****p < 0.0001
The mean gap angle was significantly higher in the SI group for all three intervals with the highest difference between 6000 and 10,000 cycles with 2.9° (p < 0.0001).
Flexion
The mean flexion in the plane of fracture was significantly higher in the SI group for all cyclic intervals (p < 0.01). After initial dislocation, the flexion was mainly limited through the ligaments. After ligament failure, flexion for both groups approximated. The highest significance was observed between 6000 and 10,000 cycles (p < 0.0001).
Vertical dislocation
The mean vertical dislocation was significantly higher in the SI group (p < 0.001). Dislocation increased with rising number of cycles. The difference between the groups was the highest between 11,000 and 15,000 cycles with 5.1 mm. The highest significances were observed between 6000 and 10,000 cycles (p < 0.0001).
Total dislocation
The mean total dislocation was significantly higher in the SI group with an earlier and higher dislocation (p < 0.001). The highest total dislocation difference between the groups was seen between 11,000 and 15,000 cycles with 5.0 mm (p < 0.0001).
Anterior displacement
The mean anterior total dislocation was significantly higher in the SI group. The highest total dislocation difference between the groups was seen between 11,000 and 15,000 cycles with 13.3 mm (p < 0.0001) The anterior displacement for every 5000 cycles is shown in Fig. 4.
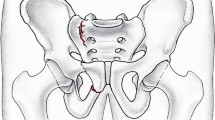
Radiographic results
The SI group showed vertical displacement due to screw penetration through the cancellous bone. In the TITS group radiographic vertical displacement was less and a bending of the screw was seen in all cases (Fig. 5).
Discussion
This study compared the biomechanical stability of anterior and posterior pelvic ring fractures after osteosynthesis with TITS or SI screws in an osteoporotic human cadaveric model. Axial stiffness as well as implant failure showed no significant differences in the cohorts. This suggests that both surgical procedures are initially adequate to stabilize an osteoporotic pelvic ring fracture. However, initial axial stiffness is not prognostic for durability of osteosynthesis after loading, a criterion of utmost relevance in osteoporotic bone. Complicated healing processes in the sense of screw loosening and screw dislocation with associated loss of fracture fixation, especially with sacroiliac screws, have been documented in the literature [18, 21]. A clear trend towards higher stability of the long screw could be demonstrated. Under biomechanical stability criteria, significantly reduced interfragmentary motion of the pelvis with long screw was shown in all cases. This demonstrates the biomechanical superiority of a TITS screw to achieve a more stable fracture treatment in osteoporotic pelvises.
To provide the best possible treatment for osteoporotic pelvic ring fractures, it was first necessary to determine the fracture morphology of these injuries. Scheyerer et al. were able to demonstrate a posterior pelvic ring lesion in elderly patients with pubic ramus fractures in over 96.8% [22]. In presenting their classification, Rommens and Hofmann showed that the primary injury patterns in osteoporotic pelvises also showed anterior and posterior involvement of the annular structure. In the 243 pelvises studied, the most common fracture morphology was FFP-IIb and -Iic [18]. Accordingly, a fracture according to FFP-IIc was considered for this test setup to provide the highest possible clinical relevance.
There is currently no scientifically based guideline for osteoporotic pelvic ring fracture treatment, even though there is a broad consensus in the community on a surgical approach. In a retrospective study, Walker et al. demonstrated the advantages of surgical management over conservatively managed osteoporotic pelvic fractures. Thus, patients in the surgically managed cohort benefited from a reduction in pain, better mobilization, as well as discharge to home, as opposed to a nursing facility [7]. Similar results were obtained by Maier et al. with a poor outcome of conservatively treated osteoporotic pelvic ring fractures [23].
Numerous osteosynthesis techniques have been developed and discussed in the past for stabilization of osteoporotic and non-osteoporotic pelvic ring fractures. Nowadays, a variety of osteosynthetic options are available to us: transiliac and other plate osteosynthesis procedures of the posterior and anterior pelvic rings, sacroiliac screws, sacral bars, lumbopelvic fixation, and triangular osteosynthesis as a combination of the different methods [9, 24,25,26,27,28]. If we focus on the osteosynthetic methods performed in this study, Schuetze et al. demonstrated in their clinical study that the SI screws as well as the TITS screws showed a good clinical success in the treatment of osteoporotic posterior pelvic ring fractures. In addition, a lower complication rate was shown in the TITS group [26].
With regard to the biomechanical aspects of the various osteosynthesis modalities and fracture types, Peng et al. were able to show in their study that in H- and U-type fractures the common methods such as lumbopelvic support and bilateral triangular stabilization achieve a stable result. However, TITS screw osteosynthesis was shown to be the most stable in all aspects studied [29]. Van Zwienen et al. as well as Yinger et al. found, in their biomechanical study, that the use of two instead of one short sacroiliac screw increases the rotational stiffness and improves the load of failure [15, 16]. In a similar experimental setup as in the present study, Tabaie et al. demonstrated that additional compression by a locked transsacral screw showed significantly increased stability in Type-C-Fractures compared to 2 sacroiliac screws [17]. On the contrary, Salari et al. found no significant difference in their biomechanical study comparing long iliosacral screws with transsacral screws in type C pelvic ring fractures [12]. Considering the simultaneous stabilization of the anterior pelvic ring in type C fractures, Lodde et al. in their biomechanical study was able to achieve higher stability using a retrograde pubis screw and a sacroiliac screw [30]. In their biomechanical study, Kußmaul et al. came to similar results. Here, the additional stabilization of the anterior pelvic ring was more stable, but statistical significance could not be achieved [31]. However, in both studies, a TITS screw was not considered. The literature indicates that the additional fixation of the anterior pelvic ring shows an advantage in terms of stability, especially in FFP II fractures [32, 33]. When plate osteosynthesis is considered, double plate osteosynthesis of the anterior pelvic ring showed an advantage regarding the screw loosening rate compared to single plate osteosynthesis [34].
To improve screw fixation, Suero et al. showed in their biomechanical study better results for augmented sacroiliac screws and TITS screw fixation compared to non-augmented short screws [11]. However, it should be noted that augmentation of the screws bears the risk of cement leakage as well as TITS osteosynthesis shows a higher risk of malposition and neurological damage [35, 36].
This study has several limitations. As in most biomechanical studies, the small group size does not allow definitive conclusions about any statistical significances. Moreover, it is in the nature of biomechanical studies that they can be translated into reality theoretically, but only to a limited extent practically. Degenerative pre-existing conditions could alter the outcome outside the test setup. Additional pulling and compressive forces from surrounding muscles allow only limited clinical relevance. Fixation of the anterior pelvic ring may provide better stability. In further biomechanical studies, the additional stabilization of the anterior pelvic ring in combination with a transiliacal–transsacral screw should be investigated.
Conclusion
In this study, we could show that the use of transiliacal–transsacral screws in FFP-IIc fractures in osteoporotic pelvic fractures is biomechanically advantageous in almost all aspects investigated, such as flexion, vertical dislocation and gap angle. In addition, a smaller anterior dislocation has been shown. For clinical practice, we also recommend to consider a minimally invasive TITS screw in osteoporotic FFP IIc fractures. If necessary, osteosynthesis of the anterior pelvic ring should be considered in case of large fragment dislocation.
Data availability
The authors confirm that the data supporting the findings of this study are available within the article and its supplementary materials.
References
Grotz MRW, Allami MK, Harwood P, Pape HC, Krettek C, Giannoudis PV. Open pelvic fractures: epidemiology, current concepts of management and outcome. Injury. 2005;36(1):1–13. https://doi.org/10.1016/j.injury.2004.05.029.
Hauschild O, Strohm PC, Culemann U, et al. Mortality in patients with pelvic fractures: results from the german pelvic injury register. J Trauma Inj Infect Crit Care. 2008;64(2):449–55. https://doi.org/10.1097/TA.0b013e31815982b1.
Pohlemann T, Tscherne H, Baumgärtel F, et al. Pelvic fractures: epidemiology, therapy and long-term outcome. Overview of the multicenter study of the Pelvis Study Group. Unfallchirurg. 1996;99(3):160–7.
Fuchs T, Rottbeck U, Hofbauer V, Raschke M, Stange R. Beckenringfrakturen im Alter: Die unterschätzte osteoporotische Fraktur. Unfallchirurg. 2011;114(8):663–70. https://doi.org/10.1007/s00113-011-2020-z.
Pohlemann T, Stengel D, Tosounidis G, et al. Survival trends and predictors of mortality in severe pelvic trauma: estimates from the German Pelvic Trauma Registry Initiative. Injury. 2011;42(10):997–1002. https://doi.org/10.1016/j.injury.2011.03.053.
Tosounidis G, Holstein JH, Culemann U, Holmenschlager F, Stuby F, Pohlemann T. Changes in epidemiology and treatment of pelvic ring fractures in Germany: an analysis on data of German Pelvic Multicenter Study Groups I and III (DGU/AO). Acta Chir Orthop Traumatol Cech. 2010;77(6):450–6.
Walker JB, Mitchell SM, Karr SD, Lowe JA, Jones CB. Percutaneous transiliac–transsacral screw fixation of sacral fragility fractures improves pain, ambulation, and rate of disposition to home. J Orthop Trauma. 2018;32(9):452–6. https://doi.org/10.1097/BOT.0000000000001243.
Sanders D, Fox J, Starr A, Sathy A, Chao J. Transsacral–transiliac screw stabilization: effective for recalcitrant pain due to sacral insufficiency fracture. J Orthop Trauma. 2016;30(9):469–73. https://doi.org/10.1097/BOT.0000000000000596.
Rollmann MF, Herath SC, Holstein JH, Pohlemann T, Menger MD, Histing T. Surgical treatment of pelvic ring fractures in the elderly now and then: a pelvic registry study. Aging Clin Exp Res. 2017;29(4):639–46. https://doi.org/10.1007/s40520-016-0612-8.
Hu P, Wu T, Wang H, et al. Biomechanical comparison of three internal fixation techniques for stabilizing posterior pelvic ring disruption: a 3D finite element analysis. Orthop Surg. 2019;11(2):195–203. https://doi.org/10.1111/os.12431.
Suero EM, Greiner A, Becker CA, et al. Biomechanical stability of sacroiliac screw osteosynthesis with and without cement augmentation. Injury. 2021;52(10):2707–11. https://doi.org/10.1016/j.injury.2020.01.043.
Salari P, Moed BR, Bledsoe JG. Supplemental S1 fixation for type C pelvic ring injuries: biomechanical study of a long iliosacral versus a transsacral screw. J Orthop Traumatol. 2015;16(4):293–300. https://doi.org/10.1007/s10195-015-0357-8.
Zhao Y, Zhang S, Sun T, et al. Mechanical comparison between lengthened and short sacroiliac screws in sacral fracture fixation: a finite element analysis. Orthop Traumatol Surg Res. 2013;99(5):601–6. https://doi.org/10.1016/j.otsr.2013.03.023.
Wagner D, Ossendorf C, Gruszka D, Hofmann A, Rommens PM. Fragility fractures of the sacrum: how to identify and when to treat surgically? Eur J Trauma Emerg Surg. 2015;41(4):349–62. https://doi.org/10.1007/s00068-015-0530-z.
Yinger K, Scalise J, Olson SA, Bay BK, Finkemeier CG. Biomechanical comparison of posterior pelvic ring fixation. J Orthop Trauma. 2003;17(7):481–7. https://doi.org/10.1097/00005131-200308000-00002.
van Zwienen CMA, van den Bosch EW, Snijders CJ, Kleinrensink GJ, van Vugt AB. Biomechanical comparison of sacroiliac screw techniques for unstable pelvic ring fractures. J Orthop Trauma. 2004;18(9):589–95. https://doi.org/10.1097/00005131-200410000-00002.
Tabaie SA, Bledsoe JG, Moed BR. Biomechanical comparison of standard iliosacral screw fixation to transsacral locked screw fixation in a type C zone II pelvic fracture model. J Orthop Trauma. 2013;27(9):521–6. https://doi.org/10.1097/BOT.0b013e3182781102.
Rommens PM, Hofmann A. Comprehensive classification of fragility fractures of the pelvic ring: recommendations for surgical treatment. Injury. 2013;44(12):1733–44. https://doi.org/10.1016/j.injury.2013.06.023.
Denis F, Davis S, Comfort T. Sacral fractures: an important problem. Retrospective analysis of 236 cases. Clin Orthop. 1988;227:67–81.
Bergmann G, Deuretzbacher G, Heller M, et al. Hip contact forces and gait patterns from routine activities. J Biomech. 2001;34(7):859–71. https://doi.org/10.1016/S0021-9290(01)00040-9.
Culemann U, Scola A, Tosounidis G, Pohlemann T, Gebhard F. Versorgungskonzept der Beckenringverletzung des alten Patienten: Eine Herausforderung. Unfallchirurg. 2010;113(4):258–71. https://doi.org/10.1007/s00113-010-1762-3.
Scheyerer MJ, Osterhoff G, Wehrle S, Wanner GA, Simmen HP, Werner CML. Detection of posterior pelvic injuries in fractures of the pubic rami. Injury. 2012;43(8):1326–9. https://doi.org/10.1016/j.injury.2012.05.016.
Maier GS, Kolbow K, Lazovic D, et al. Risk factors for pelvic insufficiency fractures and outcome after conservative therapy. Arch Gerontol Geriatr. 2016;67:80–5. https://doi.org/10.1016/j.archger.2016.06.020.
Failinger MS, McGanity PL. Unstable fractures of the pelvic ring. J Bone Jt Surg Am. 1992;74(5):781–91.
Matta JM, Tornetta P. Internal fixation of unstable pelvic ring injuries. Clin Orthop. 1996;329:129–40. https://doi.org/10.1097/00003086-199608000-00016.
Schuetze K, Eickhoff A, Dehner C, Blidon A, Gebhard F, Richter PH. Short-term outcome of fragility fractures of the pelvis in the elderly treated with screw osteosynthesis and external fixator. Eur J Trauma Emerg Surg Off Publ Eur Trauma Soc. 2022;48(3):2413–20. https://doi.org/10.1007/s00068-021-01780-3.
Pohlemann T, Angst M, Schneider E, Ganz R, Tscherne H. Fixation of transforaminal sacrum fractures: a biomechanical study. J Orthop Trauma. 1993;7(2):107–17. https://doi.org/10.1097/00005131-199304000-00002.
Schildhauer TA, Ledoux WR, Chapman JR, Henley MB, Tencer AF, Routt MLC. Triangular osteosynthesis and iliosacral screw fixation for unstable sacral fractures: a cadaveric and biomechanical evaluation under cyclic loads. J Orthop Trauma. 2003;17(1):22–31. https://doi.org/10.1097/00005131-200301000-00004.
Peng Y, Zhang G, Zhang S, et al. Biomechanical study of transsacral-transiliac screw fixation versus lumbopelvic fixation and bilateral triangular fixation for “H”- and “U”-type sacrum fractures with traumatic spondylopelvic dissociation: a finite element analysis study. J Orthop Surg. 2021;16(1):428. https://doi.org/10.1186/s13018-021-02581-5.
Lodde MF, Katthagen JC, Schopper CO, et al. Biomechanical comparison of five fixation techniques for unstable fragility fractures of the pelvic ring. J Clin Med. 2021;10(11):2326. https://doi.org/10.3390/jcm10112326.
CavalcantiKußmaul A, Greiner A, Kammerlander C, et al. Biomechanical comparison of minimally invasive treatment options for Type C unstable fractures of the pelvic ring. Orthop Traumatol Surg Res. 2020;106(1):127–33. https://doi.org/10.1016/j.otsr.2019.09.032.
Rommens PM, Arand C, Hofmann A, Wagner D. When and how to operate fragility fractures of the pelvis? Indian J Orthop. 2019;53(1):128–37. https://doi.org/10.4103/ortho.IJOrtho_631_17.
Oberkircher L, Ruchholtz S, Rommens PM, Hofmann A, Bücking B, Krüger A. Osteoporotic Pelvic Fractures. Dtsch Ärztebl Int. 2018. https://doi.org/10.3238/arztebl.2018.0070. (Published online February 2).
Herteleer M, Boudissa M, Hofmann A, Wagner D, Rommens PM. Plate fixation of the anterior pelvic ring in patients with fragility fractures of the pelvis. Eur J Trauma Emerg Surg. 2022;48(5):3711–9. https://doi.org/10.1007/s00068-021-01625-z.
Höch A, Pieroh P, Henkelmann R, Josten C, Böhme J. In-screw polymethylmethacrylate-augmented sacroiliac screw for the treatment of fragility fractures of the pelvis: a prospective, observational study with 1-year follow-up. BMC Surg. 2017;17(1):132. https://doi.org/10.1186/s12893-017-0330-y.
Zwingmann J, Hauschild O, Bode G, Südkamp NP, Schmal H. Malposition and revision rates of different imaging modalities for percutaneous iliosacral screw fixation following pelvic fractures: a systematic review and meta-analysis. Arch Orthop Trauma Surg. 2013;133(9):1257–65. https://doi.org/10.1007/s00402-013-1788-4.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
RC: contribution: study design, manuscript preparation. CF: contribution: study design, performed measurements. IZ: contribution: study design, performed measurements, manuscript preparation. BG-R: contribution: study design, performed measurements. FG: contribution: ethical report, manuscript preparation. KS: contribution: statistical analysis, study design, manuscript preparation.
Corresponding author
Ethics declarations
Conflict of interest
None of the authors received financial support for this study. The authors declare no conflicts of interest.
Ethical approval
The study was approved by the institutional ethical committee. The study was performed in the premises of the AO Research Institute in Davos.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cintean, R., Fritzsche, C., Zderic, I. et al. Sacroiliac versus transiliac–transsacral screw osteosynthesis in osteoporotic pelvic fractures: a biomechanical comparison. Eur J Trauma Emerg Surg 49, 2553–2560 (2023). https://doi.org/10.1007/s00068-023-02341-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-023-02341-6