Abstract
Purpose
To evaluate the pre-hospital administration of tranexamic acid in ambulance-treated trauma patients with a severe hemorrhage after the implementation of tranexamic acid administration in the Dutch pre-hospital protocol.
Methods
All patients with a severe hemorrhage who were treated and conveyed by EMS professionals between January 2015, and December 2017, to any trauma-receiving emergency department in the eight participating trauma regions in the Netherlands, were included. A severe hemorrhage was defined as extracranial injury with > 20% body volume blood loss, an extremity amputation above the wrist or ankle, or a grade ≥ 4 visceral organ injury. The main outcome was to determine the proportion of patients with a severe hemorrhage who received pre-hospital treatment with tranexamic acid. A Generalized Linear Model (GLM) was performed to investigate the relationship between pre-hospital tranexamic acid treatment and 24 h mortality.
Results
A total of 477 patients had a severe hemorrhage, of whom 124 patients (26.0%) received tranexamic acid before arriving at the hospital. More than half (58.4%) of the untreated patients were suspected of a severe hemorrhage by EMS professionals. Patients treated with tranexamic acid had a significantly lower risk on 24 h mortality than untreated patients (OR 0.43 [95% CI 0.19–0.97]).
Conclusion
Approximately a quarter of the patients with a severe hemorrhage received tranexamic acid before arriving at the hospital, while a severe hemorrhage was suspected in more than half of the non-treated patients. Severely hemorrhaging patients treated with tranexamic acid before arrival at the hospital had a lower risk to die within 24 h after injury.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Traumatic injuries are responsible for one out of ten deaths worldwide, and approximately one-third of these patients die as a result of hemorrhage [1, 2]. Tranexamic acid is an antifibrinolytic agent which reduces mortality in hemorrhaging trauma patients, without increasing their chance of vascular-occlusive events [3, 4]. The improvement of survival is greatest when tranexamic acid is administered as soon as possible after injury [5,6,7]. Therefore, current clinical guidelines recommend administering the first dose of tranexamic acid at the scene of injury or en route to the hospital to trauma patients whom are hemorrhaging or at risk of a significant hemorrhage [8, 9].
In most inclusive trauma systems, pre-hospital treatment is generally performed by Emergency Medical Services (EMS) professionals, and the use of tranexamic acid has been widely adopted in their pre-hospital protocols over the past decade. Administrating tranexamic acid was incorporated in the Dutch National Protocol of Ambulance Services (NPAS) in 2014. Since then, Dutch EMS professionals are advised to administer tranexamic acid to patients with a hypovolemic shock due to an uncontrollable hemorrhage [10]. A previous study, performed in the United Kingdom, found that many hemorrhaging patients were not adequately treated with tranexamic acid after incorporating its use in their pre-hospital and in-hospital protocols [11]. However, pre-hospital treatment rates could not be determined as the proportion of patients treated before arriving at the hospital was not described.
It remains unclear to what extent patients who could benefit from tranexamic acid are accurately treated before arrival at the hospital. This study, therefore, aims to determine the proportion of ambulance-transported trauma patients with a severe hemorrhage who are treated with tranexamic acid and investigates the possible causes of non-treatment.
Methods
The current study was reported in line with the STROBE guidelines [12]. The Medical Ethical Committee of the University Medical Center Utrecht decided that the Medical Research Involving Human Subjects Act did not apply to this study (reference number: 20/500747).
Study setting
In this study, seven ambulance services and eight inclusive trauma regions participated in the data collection. Annually, around 550,000 patients are transported to a hospital by the participating ambulance services [13]. They serve a region of approximately 8000km2 that contains more than 6.5 million residents. The participating trauma regions comprise eight higher-level and 60 lower-level trauma centers. In the Netherlands, inclusive trauma regions contain at least one higher-level trauma center (i.e., level-I trauma center), specialized in treating severely injured patients, and multiple lower-level trauma centers (i.e., level-II and level-III trauma centers), designed to treat mildly and moderately injured patients [14]. Higher-level trauma centers in the Netherlands adhere to the standards of the American College of Surgeons Committee on Trauma (ACSCOT) for providing the highest level of trauma care [15].
Dutch ambulances are staffed by an EMS professional (i.e., specialized registered nurse) licensed to provide advanced life trauma care, and a qualified ambulance-driver able to provide medical assistance. Since 2014, the 8th version of the Dutch NPAS is used which recommends administering tranexamic acid to patients with a hypovolemic shock (systolic blood pressure < 90 mmHg) due to an uncontrollable hemorrhage [10]. Contra-indications to administer tranexamic acid according to the Dutch NPAS are: active thrombo-embolic events, > 3 h after the moment of injury, and age < 1 year. Before tranexamic acid was introduced in the Dutch NPAS, EMS professionals were trained and tested on the (contra) indications of administering tranexamic acid and the diagnostic limitation of recognizing severe hemorrhage was discussed. In the Netherlands, the Helicopter Emergency Medical Service (HEMS) can be dispatched to assist the EMS professionals at the scene of injury or during transportation to the hospital if a patient is unstable or expected to become unstable and is staffed by a specialized physician (i.e., trauma surgeon or emergency anesthesiologist). Due to the relatively short transportation distances in the Netherlands, only few patients are transported by helicopter. The Dutch HEMS uses the same criteria to administer tranexamic acid as described in the Dutch NPAS.
Patients
Patients with a severe hemorrhage, who were transported by a ground ambulance of one of the seven participating ambulance services to any trauma-receiving emergency department in the eight participating trauma regions, were included.
Data collection
Records of all patients transported by a ground ambulance of one of the seven participating ambulance services between January 1st, 2015, and December 31st, 2017, were prospectively collected. Non-trauma patients, patients transported to a non-participating trauma region, patients without the in-hospital diagnosis of a severe hemorrhage, and patients with a contra-indication to receive tranexamic acid, were excluded. Trauma patients were identified from unfiltered EMS records using a previously developed selection tool with an accuracy of 98.9% (95%-CI, 98.3–99.2) [16]. The pre-hospital patient records were written by EMS professionals and contained the patient’s demographics, pre-hospital vital signs, pre-hospital injury suspicion, tranexamic acid administration, HEMS assistance, and transportation details (e.g., transport destination). Pre-hospital patient records were assessed to determine if the EMS professional had a suspicion of a severe hemorrhage at the scene of injury and whether the patient had a contra-indication to receive tranexamic acid. Qualified data managers of the regional trauma registries collected injury mechanisms, in-hospital resource use, mortality status (all-cause), and designated AIS codes based on in-hospital diagnosed injuries, of all admitted patients. Pre-hospital and in-hospital patient records were linked with an externally validated linkage tool with an accuracy of 100.0% (95%-CI, 100.0–100.0) [16].
Outcomes and definitions
The main outcome of this study was to determine the proportion of ambulance-transported patients with a severe hemorrhage who were treated with tranexamic acid before arrival at the hospital. A severe hemorrhage was defined as an in-hospital diagnosed extracranial injury with AIS codes including the following descriptions: > 20% body volume blood loss, extremity amputation above the wrist or ankle, or grade ≥ 4 visceral organ injuries (Online Appendix 1) [17]. Patients were suspected to have a severe hemorrhage at the scene of injury if the EMS professionals described a substantial external hemorrhage (i.e., estimated blood loss ≥ 1000 ml) or the suspicion of an internal hemorrhage in the pre-hospital records, or if the patient had a systolic blood pressure < 90 mmHg at the scene of injury.
Missing data
Variables with missing values were systolic blood pressure (23.8%), heart rate (10.7%), respiratory rate (28.3%), Glasgow Coma Scale (10.7%), and total pre-hospital times (6.7%) and appeared to be missing at random. These variables were multiply imputed using, amongst others, patients’ characteristics, pre-hospital vital signs, and in-hospital outcomes, in a multilevel multiple imputation creating 48 imputed datasets based on 20 iterations per set.
Statistical analysis
Descriptive statistics were used to analyze the data, and the results are presented in frequencies and percentages or median and inter-quartile range (IQR). The χ2 or Mann–Whitney U test were used to compare groups and we considered p values < 0.05 as statistically significant. The results of the multiply imputed variables were pooled from each imputed data set following Rubin’s rules [18]. A Generalized Linear Model was performed to investigate the relationship between tranexamic acid and 24 h mortality, adjusted for age, gender, injury severity (i.e., ISS), penetrating injury, HEMS assistance, distance to level-1 trauma center, and vital parameters used in the Revised Trauma Score (RTS) (i.e., systolic blood pressure, respiratory rate, and Glasgow Coma Scale). We used restricted cubic splines to adjust for non-linearity. All statistical analyses were computed with R statistical software (R version 4.0.3) [19].
Results
A total of 165,109 trauma patients were transported to trauma-receiving emergency departments in the eight participating trauma regions during the study period, of whom 3760 patients (2.3%) were severely injured (Injury Severity Score [ISS] ≥ 16) (Fig. 1). In total, 478 patients had a severe hemorrhage, and after excluding one patient who had a contra-indication to receive tranexamic acid, 477 patients were included.
Baseline characteristics are shown in Table 1. The median age of the patients with a severe hemorrhage was 40.7 (IQR, 25.6–57.2) years, 335 (70.2%) patients were male, and 346 (72.5%) patients were severely injured (ISS ≥ 16). Fifty-five (11.5%) patients had a systolic blood pressure < 90 mmHg at the scene of injury, 146 (30.6%) patients had a penetrating injury, and 51 (10.7%) and 84 (17.6%) patients died within 24 h and 30-days, respectively.
Treatment rates
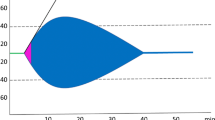
In total, 124 (26.0%) patients with a severe hemorrhage were treated with tranexamic acid before arrival at an emergency department. The HEMS assisted in 199 patients, of which 94 (47.2%) were treated with tranexamic acid. Treatment rates did not significantly change during the study period (26.9% in 2015, 27.5% in 2016, and 24.5% in 2017) (Fig. 2). Treatment rates ranged between 11.3% and 50.0% in the seven participating ambulance services (Online Appendix 2), and sensitivity analyses for patients without missing SBP or isolated grade ≥ 4 visceral organ injury showed treatment rates of 25.7% and 29.2%, respectively (Online Appendix 3).
Treated patients
Patients who were treated with tranexamic acid were younger (median age [IQR], 36.1 [25.2–53.8] vs. 42.7 [25.8–59.9]; p 0.160), more often male (97 [78.2%] vs. 238 [67.4%]; p 0.032), and more severely injured (median ISS [IQR], 28 [17–41] vs. 18 [13–29]; p < 0.001), than the untreated patients. The treated patients also had more often penetrating injuries (44 [35.5%] vs. 102 [28.9%]; p 0.209), had more often a decreased (< 12) RTS (72 [58.1%] vs. 98 [27.8%]; p < 0.001), and an emergency intervention was more often performed in these patients (51 [41.1%] vs 103 [29.2%]; p < 0.019). Furthermore, the treated patients were more often transported to a higher-level trauma center (vs. 115 [92.7%] vs. 264 [74.8%]; p < 0.001), their total pre-hospital times were longer (median minutes [IQR], 50.4 [38.5–64.7] vs. 42.0 [32.0–55.4]; p < 0.001), and the HEMS assisted more often in these patients (94 [75.8%] vs. 105 [29.7%]; p < 0.001).
Two-hundred-six (58.4%) patients who were not treated with tranexamic acid were suspected to have a severe hemorrhage (Table 2). Thirty-seven (18.0%) of these patients had a systolic blood pressure < 90 mmHg, 122 (59.2%) patients had substantial external blood loss at the scene of injury, and 88 (42.7%) patients were suspected to have an internal hemorrhage.
Patients treated with tranexamic acid had significantly lower risk on 24 h mortality than untreated patients (OR 0.43 [95%CI, 0.19–0.97]) (Table 3).
Discussion
This study evaluated pre-hospital tranexamic acid administration in patients with a severe hemorrhage and found that 26% of these patients were treated with tranexamic acid before arrival at the hospital while more than half (58%) of the untreated patients were suspected to have a severe hemorrhage. Additionally, we found that patients who were treated with tranexamic acid before arrival at the hospital had significantly lower risk on 24 h mortality than untreated patients (adjusted OR 0.44 [95% CI, 0.19–0.97]).
This was, to our knowledge, the first trauma-region wide study that was able to adequately estimate the pre-hospital tranexamic acid administration rate in severely hemorrhaging patients. We found that a majority of these patients were not treated before arrival at the hospital, which is in line with the findings of previous studies [11, 20]. Coats et al. described the implementation of tranexamic acid in the pre-hospital and in-hospital protocols in England and Wales between 2010 and 2016 and found low administration rates in the TARN database (10%), even in patients with a systolic blood pressure < 100 mmHg at the emergency department (23.8%) [11]. This study, however, did not describe the proportion of patients that were treated before arrival at the hospital. Another study by Van Wessem et al. found that 49% of the severely injured patients who were admitted to a Dutch Level-I trauma center received tranexamic acid before arrival at the hospital [20]. In the current study, we found lower treatment rates probably due to the fact that we also included patients with a severe hemorrhage who were transported to a lower-level trauma center and/or were not severely injured (ISS < 16).
Accurately recognizing a severe hemorrhage at the scene of injury can be challenging as it is difficult to estimate the amount of external blood loss [21], internal hemorrhages can be difficult to recognize [22,23,24], and patients can become hypotensive at a later stage or due to other causes (e.g., neurogenic shock) [25, 26]. In the current study, solely a small proportion of the patients with a severe hemorrhage had a systolic blood pressure < 90 mmHg. This could suggest that, in a highly developed trauma system with short transportation distances, blood pressure might not be the right parameter to estimate if a patient is severely hemorrhaging at the scene of injury. The advice to administer tranexamic acid solely in patients with a hypovolemic shock due to an uncontrollable hemorrhage, as prescribed in the Dutch NPAS [10], might have caused the EMS professional to leave these patients untreated as more than half (58%) of the non-treated patients were suspected to have a severe hemorrhage. Moreover, the relatively short distances in the Netherlands, and the shorter total pre-hospital times in patients that did not receive tranexamic acid (median minutes, 42 vs. 50), might have caused the EMS professionals to postpone tranexamic acid administration until arrival at an emergency department in the patients they suspected to have a severe hemorrhage. However, every 15 min of treatment delay decreases the survival benefit of tranexamic acid by 10% [7], which indicates that 94% of the untreated patients could have benefited from pre-hospital tranexamic acid administration as they had a pre-hospital time longer than 15 min.
Strengths and limitations
The inclusion of patients from a large, consecutive cohort, is a great strength of this study. Pre-hospital records of patients transported by seven ambulance services, which serve rural, urban, and suburban areas, were linked to their in-hospital records from both higher-level and lower-level trauma centers in the eight participating trauma regions. All admitted trauma patients are registered by the Dutch trauma registry, and in the Netherlands, no patients are transported to or treated at a non-trauma center [27]. This resulted in the inclusion of as many patients with a severe hemorrhage as possible, even if transported to an adjacent trauma region. This study also has some limitations. First, the total number of patients that could have benefitted from tranexamic acid can be greater than outlined in this study, as we solely included patients with severe traumatic hemorrhages. Second, as there are no specific AIS codes for blood loss due to visceral organ injuries, we additionally included patients with grade ≥ 4 injuries to prevent excluding patients with severe hemorrhages due to visceral organ injuries. However, a sensitivity analysis in patients without grade ≥ 4 visceral organ injuries demonstrated a comparable treatment rate of 29.1% vs. 26.0% in all patients. Third, we performed a cohort study on patients that were severely hemorrhaging and retrospectively determined if they received tranexamic acid, which might contribute to the relatively low treatment rates. Final, we were unable to adjust the association between pre-hospital treatment with tranexamic acid and 24 h mortality for in-hospital tranexamic acid treatment, as it was not recorded by the Dutch Trauma Registry.
Previous studies demonstrate the effectivity and safety of tranexamic acid in a wide spectrum of patients and indicate the importance of early administration [3, 7, 28,29,30,31]. The European guideline of major bleeding and coagulopathy following trauma therefore recommends, since 2016, to treat both hemorrhaging patients and patients at risk of a significant hemorrhage before arrival at the hospital to prevent undertreatment in patients who could have benefitted from tranexamic acid, as per the inclusion criteria of the CRASH-II study [5, 9]. Adjusting the current criteria of the Dutch NPAS for administering tranexamic acid, and alike protocols of other countries, to such a more liberal definition (i.e., administer tranexamic acid in patients with and patients suspected of a severe hemorrhage), could potentially improve pre-hospital treatment rates substantially as the majority of the patients (69%) was suspected of a severe hemorrhage by the EMS professionals. However, future research should investigate the effect of such a liberal adjustment on overtreatment and patient outcomes.
Additionally, although a large proportion of the patients with a severe hemorrhage were suspected of a severe hemorrhage by the EMS professionals, still a third of the patients remained unrecognized. Future research could focus on the development of pre-hospital prediction models to aid EMS professionals in recognizing a severe hemorrhage which could further improve pre-hospital treatment rates. Such a prediction model has been previously developed to predict if a patient is severely injured at the scene of injury [32].
Conclusion
This study found that approximately a quarter of the patients with a severe hemorrhage received tranexamic acid before arrival at the hospital, while more than half of the untreated patients were suspected to have a severe hemorrhage by the EMS professionals. The low treatment rate seemed to be caused by the short transportation distances, recommendations in the pre-hospital protocol to solely treat the most severely hemorrhaging patients, and the challenges of recognizing a severe hemorrhage in the field. Severely hemorrhaging patients treated with tranexamic acid before arrival at the hospital had lower risk to die within 24 h after injury. We suggest revising the pre-hospital protocol to a more user-friendly version in the field to aid EMS professionals in their on-scene decision making.
Data and code availability
The data that supports the findings of the current study is not publicly available due to its sensitive nature but is available upon a reasonable request that needs to be approved of the participating Emergency Medical Services and trauma regions, provided that appropriate ethical approval is sought. R-scripts are available upon request.
References
Kauvar DS, Lefering R, Wade CE. Impact of hemorrhage on trauma outcome: an overview of epidemiology, clinical presentations, and therapeutic considerations. J Trauma. 2006;60(6 Suppl):S3-11.
Organisation WH. Injuries and violence: the facts 2014. Geneva; 2014.
Olldashi F, Kerçi M, Zhurda T, Ruçi K, Banushi A, Traverso MS, et al. Effects of tranexamic acid on death, vascular occlusive events, and blood transfusion in trauma patients with significant haemorrhage (CRASH-2): a randomised, placebo-controlled trial. Lancet. 2010;376(9734):23–32.
Morrison JJ, Dubose JJ, Rasmussen TE, Midwinter MJ. Military application of tranexamic acid in trauma emergency resuscitation (MATTERs) study. Arch Surg. 2012;147(2):113–9.
Collaborators C. The importance of early treatment with tranexamic acid in bleeding trauma patients: an exploratory analysis of the CRASH-2 randomised controlled trial. Lancet. 2011;377(9771):1096-101.e2.
El-Menyar A, Sathian B, Asim M, Latifi R, Al-Thani H. Efficacy of prehospital administration of tranexamic acid in trauma patients: a meta-analysis of the randomized controlled trials. Am J Emerg Med. 2018;36(6):1079–87.
Gayet-Ageron A, Prieto-Merino D, Ker K, Shakur H, Ageron F-X, Roberts I, et al. Effect of treatment delay on the effectiveness and safety of antifibrinolytics in acute severe haemorrhage: a meta-analysis of individual patient-level data from 40 138 bleeding patients. Lancet. 2018;391(10116):125–32.
National Institute for Health and Care Excellence. Major trauma: assessment and initial management. London: NICE; 2016.
Spahn DR, Bouillon B, Cerny V, Duranteau J, Filipescu D, Hunt BJ, et al. The European guideline on management of major bleeding and coagulopathy following trauma fifth edition. Crit Care. 2019;23(1):98.
Nederland A. Landelijk Protocol Ambulancezorg (versie 8.1) Zwolle; 2016. https://www.ambulancezorg.nl/themas/kwaliteit-van-zorg/protocollen-en-richtlijnen/landelijk-protocol-ambulancezorg. Accessed 17–06–2021.
Coats TJ, Fragoso-Iñiguez M, Roberts I. Implementation of tranexamic acid for bleeding trauma patients: a longitudinal and cross-sectional study. Emerg Med J. 2019;36(2):78–81.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453–7.
AmbulanceZorg Nederland. Tabellenboek 2018. Zwolle; 2018. https://www.ambulancezorg.nl/publicatiepagina/sectorkompas-ambulancezorg. Accessed 30–10–2021.
Lansink KW, Leenen LP. Do designated trauma systems improve outcome? Curr Opin Crit Care. 2007;13(6):686–90.
American College of Surgeons Committee on Trauma. Resources for optimal care of the injured patient Chicago, IL: American College of Surgeons 2014. https://www.facs.org/-/media/files/quality-programs/trauma/vrc-resources/resources-for-optimal-care.ashx. Accessed 15–12–2020.
van der Sluijs R, Lokerman RD, Waalwijk JF, de Jongh MAC, Edwards MJR, den Hartog D, et al. Accuracy of pre-hospital trauma triage and field triage decision rules in children (P2–T2 study): an observational study. Lancet Child Adolesc Health. 2020;4(4):290–8.
Association for the Advancement of Automotive Medicine. Abbreviated Injury Scale 2005, Update 2008. Barrington: 2008.
Rubin DB. Multiple imputations for nonresponse in surveys. New York: Wiley; 1987.
R: A Language and Environment for Statistical Computing [computer program]. Vienna, Austria: R Foundation for Statistical Computing; 2020.
van Wessem KJP, Leenen LPH. Does liberal prehospital and in-hospital tranexamic acid influence outcome in severely injured patients? A prospective cohort study. World J Surg. 2021;45(8):2398–407.
Patton K, Funk DL, McErlean M, Bartfield JM. Accuracy of estimation of external blood loss by EMS personnel. J Trauma Acute Care Surg. 2001;50(5):914–6.
Hasler RM, Kehl C, Exadaktylos AK, Albrecht R, Dubler S, Greif R, et al. Accuracy of prehospital diagnosis and triage of a Swiss helicopter emergency medical service. J Trauma Acute Care Surg. 2012;73(3):709–15.
Mulholland SA, Cameron PA, Gabbe BJ, Williamson OD, Young K, Smith KL, et al. Prehospital prediction of the severity of blunt anatomic injury. J Trauma. 2008;64(3):754–60.
Muhm M, Danko T, Madler C, Winkler H. Preclinical prediction of prehospital injury severity by emergency physicians : approach to evaluate validity. Anaesthesist. 2011;60(6):534–40.
Guly HR, Bouamra O, Spiers M, Dark P, Coats T, Lecky FE. Vital signs and estimated blood loss in patients with major trauma: testing the validity of the ATLS classification of hypovolaemic shock. Resuscitation. 2011;82(5):556–9.
Geeraedts LMG, Kaasjager HAH, van Vugt AB, Frölke JPM. Exsanguination in trauma: a review of diagnostics and treatment options. Injury. 2009;40(1):11–20.
van der Vliet QMJ, Hietbrink F, Leenen LPH. Inclusion of all patients admitted for trauma in trauma registries. JAMA Surg. 2020;155(3):264–5.
Guyette FX, Brown JB, Zenati MS, Early-Young BJ, Adams PW, Eastridge BJ, et al. Tranexamic acid during prehospital transport in patients at risk for hemorrhage after injury: a double-blind, placebo-controlled randomized clinical trial. JAMA Surg. 2020;156(1):11–20.
Perel P, Prieto-Merino D, Shakur H, Clayton T, Lecky F, Bouamra O, et al. Predicting early death in patients with traumatic bleeding: development and validation of prognostic model. BMJ. 2012;345: e5166.
Roberts I, Perel P, Prieto-Merino D, Shakur H, Coats T, Hunt BJ, et al. Effect of tranexamic acid on mortality in patients with traumatic bleeding: prespecified analysis of data from randomised controlled trial. BMJ. 2012;345: e5839.
Thurston B, Chowdhury S, Edu S, Nicol AJ, Navsaria PH. Time since injury is the major factor in preventing tranexamic acid use in the trauma setting: an observational cohort study from a major trauma centre in a middle-income country. S Afr J Surg. 2015;53:13–8.
van Rein EAJ, van der Sluijs R, Voskens FJ, Lansink KWW, Houwert RM, Lichtveld RA, et al. Development and validation of a prediction model for prehospital triage of trauma patients. JAMA Surg. 2019;154(5):421–9.
Acknowledgements
The authors thank all participating members of the Pre-hospital Trauma Triage Research Collaborative and the research staff of the participating Emergency Medical Services and trauma regions. Collaborative group: Koen W.W. Lansink (ETZ Hospital Tilburg), Mariska A.C. de Jongh (Netwerk Acute Zorg Brabant), Dennis den Hartog (Erasmus University Medical Center), Jens A. Halm (Amsterdam University Medical Center), Georgios F. Giannakópoulos (Amsterdam University Medical Center), Michael J.R. Edwards (Radboud University Medical Center), Martijn Poeze (Maastricht University Medical Center), Pierre M. van Grunsven (Veiligheidsregio Gelderland-Zuid), Nancy W.P.L. van der Waarden (Regionale Ambulance Voorziening Rotterdam-Rijnmond), Arjen Siegers (Regionale Ambulance Voorziening Ambulance Amsterdam-Amstelland; Regionale Ambulance Voorziening, Zaanstreek-Waterland), Risco van Vliet (Regionale Ambulance Voorziening Brabant Midden-West-Noord), Laura M. Esteve Cuevas (Regionale Ambulance Voorziening Zuid-Holland Zuid).
Funding
This study was partly funded by grants from the Netherlands Organisation for Health Research and Development (ZonMw) and the Innovation Fund Health Insurers. The funding sources had no influence on the study design, data collection, statistical analysis, interpretation of data and writing of the report.
Author information
Authors and Affiliations
Contributions
MG and RDL: contributed equally and share first authorship. All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by MG, RDL and JFW. The first draft of the manuscript was written by MG. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest to declare.
Ethical approval
The current study was reported in line with the STROBE guidelines. The Medical Ethical Committee of the University Medical Center Utrecht decided that the Medical Research Involving Human Subjects Act did not apply to this study (reference number: 20/500747).
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gulickx, M., Lokerman, R.D., Waalwijk, J.F. et al. Pre-hospital tranexamic acid administration in patients with a severe hemorrhage: an evaluation after the implementation of tranexamic acid administration in the Dutch pre-hospital protocol. Eur J Trauma Emerg Surg 50, 139–147 (2024). https://doi.org/10.1007/s00068-023-02262-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-023-02262-4