Abstract
Introduction
Quality improvement in prehospital emergency medical services (EMS) can only be achieved by high-quality research and critical appraisal of current practices. This study examines current opportunities and barriers in EMS research in the Netherlands.
Methods
This mixed-methods consensus study consisted of three phases. The first phase consisted of semi-structured interviews with relevant stakeholders. Thematic analysis of qualitative data derived from these interviews was used to identify main themes, which were subsequently discussed in several online focus groups in the second phase. Output from these discussions was used to shape statements for an online Delphi consensus study among relevant stakeholders in EMS research. Consensus was met if 80% of respondents agreed or disagreed on a particular statement.
Results
Forty-nine stakeholders participated in the study; qualitative thematic analysis of the interviews and focus group discussions identified four main themes: (1) data registration and data sharing, (2) laws and regulations, (3) financial aspects and funding, and (4) organization and culture. Qualitative data from the first two phases of the study were used to construct 33 statements for an online Delphi study. Consensus was reached on 21 (64%) statements. Eleven (52%) of these statements pertained to the storage and use of EMS patient data.
Conclusion
Barriers for prehospital EMS research in the Netherlands include issues regarding the use of patient data, privacy and legislation, funding and research culture in EMS organizations. Opportunities to increase scientific productivity in EMS research include the development of a national strategy for EMS data and the incorporation of EMS topics in research agendas of national medical professional associations.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Introduction
Over the past decades, prehospital emergency medical services (EMS) in the Netherlands developed tremendously. While ambulance services offered little more than a means of horizontal transportation in the early fifties, ambulances are currently manned by well-trained EMS clinicians able to offer evidence-based prehospital advanced (trauma) life support. Moreover, in severely ill and injured patients, ground EMS by ambulance is complemented by a physician-staffed helicopter emergency medical services (HEMS) [1]. Together with improvements in in-hospital resuscitation and treatment, these developments have led to better outcomes after prehospital cardiac arrest, trauma, and stroke [2, 3].
Progress of EMS would not have been possible without continuous adjustment and gradual improvement of regional and national networks and continuous appraisal and revision of local, regional, and national dispatch criteria and treatment protocols for both ground EMS and HEMS [4,5,6]. To do so, one would suppose that meticulous quality control and robust data from clinical studies are paramount.
However, the scientific evidence supporting many of the dispatch and treatment algorithms used by both ground emergency medical services and HEMS teams is not always as robust as desired [7, 8]. In addition, available evidence is often derived from in-hospital studies or EMS systems from abroad, which may not apply to the Dutch EMS system regarding level of training, organization of trauma systems, and geographic characteristics. Thus, to gain better understanding of which prehospital interventions do or do not benefit Dutch patients and how prehospital emergency medical and trauma care can be organized in a cost-effective manner, more research tailored to the Dutch situation is needed. And while high-quality EMS research is being undertaken in the Netherlands, there is little national coordination with regard to the organization and execution of EMS research.
Recently, an updated version of the 2016 Dutch EMS research agenda was published by Vloet et al., based on the results of an online Delphi consensus study [9, 10]. Six important themes for future EMS research were identified, most of which focused on organizational aspects of EMS (mostly ground EMS) in the Netherlands. However, an in-depth analysis of current opportunities and barriers for performing research in EMS was not explored. Initiatives from other countries (e.g., Canada) have shown that a focus on opportunities and barriers can be extremely instrumental when it comes to setting priorities for research and improving the basic conditions needed for effective EMS research [11,12,13]. We hypothesize that this will also be true for the Netherlands. Thus, the objective of this mixed-method approach consensus study was to identify potential opportunities and barriers for research in prehospital emergency care in the Netherlands.
Methods
This study was designed as a three-phase, mixed-method approach consensus study. Its design was based on the mixed-methods approach used to generate the Canadian national EMS research agenda [14]. Stakeholders currently involved in EMS research were personally invited to participate in the study after being identified using purposive sampling, starting with six Dutch HEMS physicians and ambulance nurses involved in recent prehospital research projects. This list of stakeholders was further expanded using snowball sampling: already identified stakeholders were asked to suggest other stakeholders with relevant activities in EMS research, who were subsequently invited to participate in the study as well. The list of stakeholders was updated throughout the first two phases of the study.
Phase 1
A semi-structured interview guide was used to steer the (online) interviews (Appendix 1). Participants were invited to elaborate on certain subjects using additional probing questions. Interviews were digitally recorded, transcribed, and stored on a password protected computer. Interviews were held till data saturation was reached. Data saturation was defined as the moment where no new information was gained from at least two interviews. Once the interviews were completed, the qualitative data derived from the interviews were analyzed according to the methodology for thematic analysis as described by Braun and Clarke [14] using software developed specifically for qualitative data analysis (ATLAS.ti version 8, ATLAS.ti, Scientific Software Development GmbH, Berlin, Germany). Topics were discussed and overarching themes were identified. For each theme, several overarching statements—capturing the entire theme—were derived from the list of topics.
Phase 2
In the second phase, each theme identified in the previous phase was presented in an online focus groups containing two to three participants from previous Phase 1, and at least one new participant. Again, participants were selected using purposive sampling and snowball sampling, based on their input during phase 1 of the study, or if their background was deemed relevant to the specific theme discussed (for instance, a physician with a degree in law and a psychologist with connections to EMS research groups to discuss specific themes). After a short presentation containing background information and results obtained, a discussion of the theme of interest was initiated based on the statements derived from the previous round. Once all focus groups were completed, data were analyzed in a similar way as in the first phase according to the same methodology as mentioned above.
Phase 3
The third phase of this study consisted of a two-round online Delphi consensus study [15]. For each theme, several statements were generated based on information gathered in the first two phases of the study. These statements were uploaded in Castor EDC, an online electronic data capture system (Castor EDC, Amsterdam, The Netherlands). In the first round, participants were invited to rank the importance of each statement on a five-point Likert scale (1: I don’t agree at all; 5: I fully agree). In addition, participants were asked to provide commentary on each statement. After closure of the first round, statements were adjusted based on the commentary given and statements on which no consensus had been reached in the first round were offered for a second round. For each statement, participants were provided with their own answer from the first round as well as the median answer of all other participants. Participants who completed at least 50% of the first round were asked to rank the remaining statements on a five-point Likert scale during a second online survey round. Answers 1 (I don’t agree at all) and 2 (I don’t agree) were combined and processed as disagreement; similarly, answers 4 (I agree) and 5 (I fully agree) were combined and processed as agreement. When 80% or more of respondents agreed or disagreed on a statement, it was considered as consensus was reached on that particular statement, as is customary for this type of research [14, 15].
Medical ethics approval
The study protocol was reviewed by the Medical Research Ethics Committee (MREC) of the Erasmus MC, Rotterdam, The Netherlands. The study was waived (MREC nr. Mec-2020-0464) as its content is not covered by the Medical Research Involving Human Subjects Act (Dutch: WMO (Wet Medisch-Wetenschappelijk Onderzoek met mensen)).
Results
During the first two phases of the study, 60 relevant stakeholders were identified using purposive and snowball sampling. Eventually, 49 stakeholders participated in at least one phase of the study (all were invited but 11 (18.3%) declined to participate for various reasons). Characteristics of participants in all three phases of the study are listed in Table 1.
Phase 1
In the first phase of this study, a total of twenty-two interviews were held between July 15, 2020, and October 2, 2020. Data saturation was reached after 22 interviews. Thematic analysis of the interviews resulted in five main themes being identified. These themes were: (1) data registration and data sharing, (2) laws and regulations, (3) financial aspects, (4) organization and culture, and (5) incentives for performing research.
Phase 2
Focus groups per theme took place between February 23, 2021 and March 31, 2021, and were held based on eighteen statements derived from the data gathered in the first step of this study, which are shown in Appendix 2. No new themes were identified, but the themes (4) organization and culture and (5) incentive for performing research showed such a high level of overlap it was agreed to merge these two themes for the remainder of the study.
Phase 3
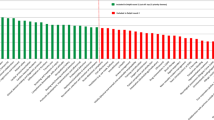
The third phase of this study was a two-round online Delphi survey. Fifty-three stakeholders were asked to participate. Information gathered in the first and second phase of this study was subsequently converted into thirty-three statements. Eventually, 32 of 53 stakeholders (60.4%) completed the first survey round and consensus was reached on thirteen statements (39.4%). The twenty statements for which no consensus was reached were send back to the stakeholders. Twenty-seven stakeholders (50.9%) completed the second survey round, and consensus was reached for an additional eight statements, setting the total number of statements with consensus at 21 (63.6%). All statements and their level of consensus are shown in Table 2. A brief overview of opportunities for Dutch EMS research is given in Table 3.
Data registration and data sharing
Registration, storage, and sharing of patient data proved to be one of the most important themes both enabling and hampering effective EMS research; 11 out of 21 statements on which consensus was reached in the Delphi study pertained to this theme. Barriers for EMS research mentioned during the interviews and focus groups and confirmed in the Delphi rounds included the absence of a common data set for emergency patients among different providers (HEMS, ground EMS, hospital emergency department), precluding effective exchange and merging of these data. The multitude of different electronic patient files used by different services further aggravates this problem. As one of the participants stated during an interview: “At this moment, the ambulance data registration system does not communicate well with the HEMS data registration system, neither with the hospital data registration system. So there are three systems for one patient in the first hour of its care and those systems don’t talk to each other.” Initiatives such as “the minimal data set for ground EMS” and the Dutch Emergency Medicine Database (NEED) were generally considered to be important steps toward achieving this goal. Moreover, the fact that all patient data in the Netherlands is already electronically recorded and stored was considered to be an important condition for such developments by most participants.
In addition, several participants had concerns regarding the quality of routinely gathered prehospital patient data. Currently, correct registration of health data at the source is hampered by limited compliance of prehospital personnel and poor ergonomics of data capture systems, resulting in incomplete and sometimes unreliable data. While non-compliance could be addressed during training of EMS workers as mentioned by some participants, improving ergonomics and data export for data capture requires more technical solutions.
Laws and regulations
Many participants commented on Dutch and European laws and regulations pertaining to EMS research. Two important subthemes within this theme were (1) informed consent in EMS research and (2) correct application of the European General Data Protection Regulation (GDPR) in EMS research. With regard to informed consent procedures, several participants commented that while there are laws in place that allow inclusion of emergency patients in prospective studies by so-called deferred consent, many prehospital healthcare workers and even members of MREC’s are unfamiliar with this kind of consent procedures. Moreover, the majority of participants felt that not all MREC’s are aware of the intricacies of prehospital EMS research, often leading to a delay in the review process (“MREC’s have no idea what EMS-work entails”).
Variable interpretation among different services of the GDPR was considered to be another threat for effective EMS research. As one participant stated; “There are many parties that are afraid of making a mistake (with regard to GDPR, red.).” As stated during one of the focus groups, there is considerable variation between organizations involved in emergency care with regard to their practices in data sharing. Having a uniform national policy based on best GDPR practice for emergency care research data exchange between emergency care organizations including EMS providers was considered to be a great opportunity in the same focus group.
Financial aspects
Opinions with regard to funding opportunities were widespread during the interviews. Some experienced a total inability to acquire funds for EMS research. As one of the interviewees states “the amount of work to submit a grant proposal is so disproportionally large compared to the chance of actually obtaining the grant, I don’t even get started anymore.” On the other hand, several other interviewees mentioned examples of successfully funded EMS research projects; these were most often projects initiated by researchers from university medical centers (medical specialists) collaborating with EMS organizations for their studies. In the Delphi consensus study, there was agreement on several statements regarding funding opportunities for EMS research. These were considered to be generally limited for EMS research. Participants in the study also agreed that part of this may be due to limited knowledge of funding opportunities among EMS workers and that this may be improved by further collaboration between EMS organizations and research institutes like university medical centers. In addition, during the focus group on this theme, the importance of national collaboration in research consortia for acquiring funds was mentioned as an important opportunity by several participants. At last, medical professional associations may play an important role in increasing the chance of funding being allocated for EMS projects, by including knowledge gaps regarding prehospital treatment of conditions of interest in their respective research and knowledge agendas.
Another important financial barrier for EMS research mentioned in the interviews was the limited amount of resources available to those who want to be involved in EMS research. As stated, some larger EMS providers have indeed allocated funds and time to accommodate EMS research activities, but many others do not. As one participant stated; “When you want to acquire funding for research, you first have to get the basics right.” In order to get these basics right, participants agreed that facilitating research should be among the core tasks of ambulance service providers and HEMS services. To achieve this, EMS organizations should allocate internal funds to provide basic conditions for research activities, such as allocated time, adequate (IT) facilities, and opportunities for learning about doing research.
Organization and culture
The theme “organization and culture in EMS research” was widely elaborated on by participants. There was general agreement that substantial investments should be made to achieve a better research culture among EMS organizations. Examples from the interviews of current barriers include little incentive for doing research among EMS organizations, lack of enthusiasm for and knowledge about research among EMS workers (“if you sign up for ambulance work, you don’t sign up for research”), and little perceived benefits for the patient due to a lack of feedback from past research projects. Indeed, implementation of scientific results from EMS research in treatment protocols was perceived to be insufficient at the moment. Several participants praised the foundation of the scientific committee with the Dutch National Sector Organization for Ambulance Care (Dutch: AmbulanceZorg Nederland) and the publication of the national research agenda for (ground) EMS for their contribution to establishing a vital research culture among EMS organizations. However, no consensus was met on statements involving these initiatives in the Delphi rounds, and many participants mentioned that such initiatives can only be successful if they aim for intensive collaboration between ambulance services, HEMS services, and research institutes on a national level. Emphasizing how research may change daily practice by quickly implementing findings from national studies in national guidelines could further contribute to a viable research culture.
Discussion
In this mixed-methods consensus study, opportunities and barriers for performing research in EMS in the Netherlands were examined. Four themes important for EMS research in the Netherlands; were identified: (1) data registration and sharing, (2) laws and regulations, (3) financial aspects, and (4) organization and culture.
Probably the most challenging topic identified in this study is the way health data are currently collected, stored, and shared for EMS research in the Netherlands. As vast amounts of health data are currently collected for each patient traveling through the emergency care system, improvements in data capture and handling have a huge potential regarding quality control and research [16]. Unfortunately, as this study shows, tapping into this potential is currently hindered by several factors. First, manual entry of patient characteristics and vital parameters in EMS electronic medical records creates a risk of incomplete and unreliable data being stored. Second, various data sets used by various EMS providers combined with a myriad of software applications unable to communicate with each other and incapable of running simple (or complex) data queries make combining the data sets from HEMS, ground EMS, and hospitals almost impossible. Thirdly, varying interpretation of privacy laws and regulations with regard to data sharing between organizations (leading to data sharing practices ranging from liberal sharing of data to outright refusal to share any data) leads to difficult and time consuming procedures when data sets need to be acquired and combined. Research projects that have succeeded in combining data from different providers often had to come up with complicated legal constructs [17].
The current study provides several suggestions to address these issues. First, arrangements should be made to align the way data are currently being collected among different organizations involved in the emergency treatment of critically ill or injured patients. Data sets should be easy to combine, contain the same variables, should be easy to query for scientific purposes and quality control, and should abide to the FAIR principles [18], all with respect for patients’ privacy and relevant laws and regulations. National data registries such as the National Trauma Registration (Dutch: Landelijke TraumaRegistratie; LTR) and Netherlands Intensive Care Evaluation (NICE) and examples such as the Danish database for prehospital emergency medical services could serve as examples to build upon [19,20,21]. Second, knowledge regarding (privacy) rules and regulations should be increased among all organizations involved, by education and—for example—publication of a best practice guideline for EMS research and privacy (and other) regulations. Finally, the reliability of data can be improved by increasing the level of automation and ergonomics of data registration systems. Automated registration and storage of vital parameters, speech capture software, and automatic linking of the registered data to a unique personal patient number will all facilitate the right information being accurately and completely recorded and linked to the right patient.
Participants in our study stated that investing in a research culture among EMS workers may have a positive impact on EMS research in the Netherlands. Incorporating research activities in training as well as emphasizing the importance of research and making the impact of research on day-to-day clinical work more visible (e.g., development of decision aids) may further increase awareness and enthusiasm. Ambulance nurses and HEMS physicians interested in performing or participating in research projects should be encouraged to do so. This can be done by offering them time, funds, and support to develop their own research ideas and should been given tools to bring these interests to practice successfully. EMS research agenda’s from other countries have identified similar issues; lack of time and resources was identified as one of the major threats to a vital research culture in the Canadian EMS research agenda too [11]. In addition, EMS workers with less research ambition can be involved by emphasizing the importance of evidence-based practice and by organizing journal clubs and research presentations to offer a clear outlook on how (national) research can lead to better patient care and new guidelines. In order to make these changes happen, it is important that individual ambulance care and HEMS organizations expand their focus from pure operational aspects toward a more quality-of-care-driven focus. While not all ambulance services may be able to initiate research on their own, all ambulance and HEMS services in the Netherlands should be able to accommodate research projects initiated by other parties, preferably based on a national policies. At last, by intensifying cooperation between ambulance services and (university) medical centers on a regional and national level, resources and experience can be combined and new projects can be more successful. The fact that most studies in Dutch EMS research have been initiated by (university) medical centers, shows that there is great interest in this particular field of care in academia, which could be improved by more systematic collaboration between hospitals and EMS providers.
In terms of funding, participants perceived that funding for EMS research is scarce and that many involved in EMS research are not informed about existing funding opportunities. Improvement of the aforementioned collaboration between ambulance services and (university) medical centers may increase knowledge to funding opportunities for EMS researchers. Likewise, participants stated that scientific organizations (such as the Dutch associations and societies for trauma surgery, internal medicine, cardiology, anesthesiology, neurology, and emergency medicine) could have an important role in expanding opportunities for EMS research funding by incorporating prehospital treatment of ailments within their specific area of interest on their research agendas.
In the 2015 Canadian Research Agenda for EMS research, most strengths, opportunities, barriers, and recommendations pertained to funding, time for doing research, and organizational culture [12]. Likewise, the 2003 USA research agenda addresses five major impediments for the performance of high-quality EMS research in the USA. Four of these major impediments are similar to our findings and address funding, data organization and collection, informed consent, and research culture [13]. The Dutch EMS system differs markedly from EMS systems in Canada and the USA (ambulance nurses instead of EMS technicians, national coverage of physician-staffed HEMS, geographic differences), and significant time has passed since the Canadian and USA research agendas were published. However, similarities between the outcomes of aforementioned research agendas and the current study suggest that challenges in performing prehospital EMS research are universal and not easily to overcome. Identifying barriers and formulating opportunities is therefore an important first step to increase scientific productivity in a given prehospital system and it may be advocated that similar studies like this study are performed in other countries as well [16, 22, 23].
Several limitations apply to this study. First, the overrepresentation of physicians in all phases of this study may have colored the overall results. However, the majority of EMS research in the Netherlands is initiated and conducted by physicians and many of the physicians participating in this study have connections to ambulance services. We therefore feel our sample to be representative of the EMS research landscape in the Netherlands as it currently is. In addition, for our focus groups, we were limited to small groups and relatively short sessions due to COVID restrictions at the time of the study. Ideally, a moderated session involving all stakeholders at the same time would have been preferred, as this would have given all participants the opportunity to extensively reflect on each identified theme. While this may have impacted on the development of the statements for the Delphi study, all statements were subjected to multiple rounds of consensus formation in the subsequent Delphi study, leveling out the effect of the small focus groups.
Conclusion
Barriers for prehospital EMS research in the Netherlands include issues regarding the use of patient data, privacy and legislation, funding, and research culture in EMS organizations. Opportunities to increase scientific productivity in EMS research include the development of a national strategy for EMS data and the incorporation of EMS topics in research agendas of national medical professional associations.
Data availability
Data will be made available upon reasonable request to the corresponding author.
References
Backus BE, Ter Avest E, Gerretsen BM, Viljac A, Tolsma RT. Organization of prehospital care in the Netherlands: a perspective article. Eur J Emerg Med. 2020;27(6):398–9.
de Visser M, Bosch J, Bootsma M, Cannegieter S, van Dijk A, Heringhaus C, et al. An observational study on survival rates of patients with out-of-hospital cardiac arrest in the Netherlands after improving the “chain of survival.” BMJ Open. 2019;9(7):e029254.
Den Hartog D, Romeo J, Ringburg AN, Verhofstad MH, Van Lieshout EM. Survival benefit of physician-staffed Helicopter Emergency Medical Services (HEMS) assistance for severely injured patients. Injury. 2015;46(7):1281–6.
Rehn M, Kruger AJ. Quality improvement in pre-hospital critical care: increased value through research and publication. Scand J Trauma Resusc Emerg Med. 2014;22:34.
Hart HN. Integrated approach to prehospital coronary care in Rotterdam. Am J Emerg Med. 1984;2(3):225–9.
van Vugt AB, van Olden GD, Edwards MJ. Emergency ambulance assistance in The Netherlands: is the Dutch situation optimal? Eur J Emerg Med. 1995;2(4):212–6.
Brazier H, Murphy AW, Lynch C, Bury G. Searching for the evidence in pre-hospital care: a review of randomised controlled trials. On behalf of the Ambulance Response Time Sub-Group of the National Ambulance Advisory Committee. J Accid Emerg Med. 1999;16(1):18–23.
Cone DC. Knowledge translation in the emergency medical services: a research agenda for advancing prehospital care. Acad Emerg Med. 2007;14(11):1052–7.
Vloet LCM, Hesselink G, Berben SAA, Hoogeveen M, Rood PJT, Ebben RHA. The updated national research agenda 2021–2026 for prehospital emergency medical services in the Netherlands: a Delphi study. Scand J Trauma Resusc Emerg Med. 2021;29(1):162.
van de Glind I, Berben S, Zeegers F, Poppen H, Hoogeveen M, Bolt I, et al. A national research agenda for pre-hospital emergency medical services in the Netherlands: a Delphi-study. Scand J Trauma Resusc Emerg Med. 2016;24:2.
Jensen JL, Bigham BL, Blanchard IE, Dainty KN, Socha D, Carter A, et al. The Canadian National EMS Research Agenda: a mixed methods consensus study. CJEM. 2013;15(2):73–82.
Jensen JL, Blanchard IE, Bigham BL, Carter A, Brown R, Socha D, et al. The Canadian National EMS Research Agenda: impact and feasibility of implementation of previously generated recommendations. CJEM. 2015;17(5):484–90.
Sayre MR, White LJ, Brown LH, McHenry SD, Implementation SP. National EMS research agenda: proceedings of the implementation symposium. Acad Emerg Med. 2003;10(10):1100–8.
Jensen JL, Blanchard IE, Bigham BL, Dainty KN, Socha D, Carter A, et al. Methodology for the development of a Canadian national EMS research agenda. BMC Emerg Med. 2011;11:15.
Hasson F, Keeney S, McKenna H. Research guidelines for the Delphi survey technique. J Adv Nurs. 2000;32(4):1008–15.
Janke AT, Overbeek DL, Kocher KE, Levy PD. Exploring the potential of predictive analytics and big data in emergency care. Ann Emerg Med. 2016;67(2):227–36.
Bossers SM, Boer C, Bloemers FW, Van Lieshout EMM, Den Hartog D, Hoogerwerf N, et al. Epidemiology, prehospital characteristics and outcomes of severe traumatic brain injury in The Netherlands: the BRAIN-PROTECT Study. Prehosp Emerg Care. 2021;25(5):644–55.
Eva G, Liese G, Stephanie B, Petr H, Leslie M, Roel V, et al. Position paper on management of personal data in environment and health research in Europe. Environ Int. 2022;165:107334.
Driessen MLS, Sturms LM, Bloemers FW, Ten Duis HJ, Edwards MJR, den Hartog D, et al. The Dutch nationwide trauma registry: the value of capturing all acute trauma admissions. Injury. 2020;51(11):2553–9.
Alstrup K, Petersen JAK, Barfod C, Knudsen L, Rognas L, Moller TP. The Danish helicopter emergency medical service database: high quality data with great potential. Scand J Trauma Resusc Emerg Med. 2019;27(1):38.
van de Klundert N, Holman R, Dongelmans DA, de Keizer NF. Data resource profile: the Dutch National Intensive Care Evaluation (NICE) registry of admissions to adult intensive care units. Int J Epidemiol. 2015;44(6):1850-h.
Blanchard IE, Williamson TS, Ronksley P, Hagel B, Niven D, Dean S, et al. Linkage of emergency medical services and hospital data: a necessary precursor to improve understanding of outcomes of prehospital care. Prehosp Emerg Care. 2021;26:1–10.
Demotes-Mainard J, Cornu C, Guerin A, participants of GiensXRTCr. How the new European data protection regulation affects clinical research and recommendations? Therapie. 2019;74(1):31–42.
Acknowledgements
The members of the Dutch Opportunities & Barriers in EMS research group are: Jelmer Alsma, David N. Baden, Timo Bevelander, Joost Bierens, Jan Bollen, Jan Bosch, Bert Dercksen, Johannes J. Duvekot, Menno I. Gaakeer, Geert-Jan van Geffen, Dorien H. F. Geurts, Pierre M. van Grunsven, Mark van Heijl, Arnoud van ’t Hof, Markus W. Hollmann, Nico Hoogerwerf, Isabelle C. Huig, Fabian Kooij, Marcel A. de Leeuw, Caroline D. van der Marel, Marlies Morsink, Gerrit J. Noordergraaf, Harm van de Pas, Joost H. Peters, Martijn Poeze, Paul Richelle, Bob Roozenbeek, Patrick Schober, Lisette Schoonhoven, Hans van Schuppen, Arjen Siegers, Dick Tibboel, Rudolf T. Tolsma, Nigel M. Turner, Matthijs de Visser, Lilian C. M. Vloet, Ronald de Vos, Bas van Wageningen, Angelique van der Weerd.
Funding
This study was not funded.
Author information
Authors and Affiliations
Consortia
Contributions
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data. All authors were involved in drafting the article or critically revising it for important intellectual content. And, finally, all authors approved the version to be published.
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts of interest in the materials or subject matter dealt with the manuscript.
Additional information
The members of the Dutch Opportunities & Barriers in EMS research group are given in Acknowledgements.
Appendices
Appendix 1: Semi-structured interview guide
-
1.
In what way are you involved in prehospital emergency medical care (research) in the Netherlands?
-
2.
In what type of research are you (currently) involved?
-
3.
In which area of prehospital emergency medical care are you conducting research?
-
4.
What facilitates prehospital emergency medical care research in the Netherlands?
-
5.
What are the opportunities for prehospital research in the Netherlands?
-
6.
What barriers did you encounter conducting prehospital emergency medical care research in the Netherlands?
-
7.
What are your thoughts about the way prehospital emergency medical care research is currently funded in the Netherlands?
-
8.
Do the results of (published) studies find their way to the prehospital emergency medical care protocols in the Netherlands?
-
9.
Is it of importance that the opportunities and barriers for prehospital emergency medical care research in the Netherlands are identified to carry out future research?
-
10.
What are three areas within prehospital emergency medical care that need more research?
-
11.
Have any studies been carried out abroad that you think should be repeated/re-examined in the Netherlands?
-
12.
Are there any relevant topics within prehospital emergency medical care that we have not discussed yet?
-
13.
Who else do you think should be interviewed regarding this topic?
Appendix 2: Statements used for focus groups
Theme | Statement |
|---|---|
Data registration and data sharing | All prehospital collected patient data should be stored in a central database |
Thorough quality control at a national level is impossible without uniform data collection and storage | |
The Dutch/European legislation and regulations with regard to the storage of patient data is a major obstacle in organizing a national data strategy | |
Due to the unreliability of the entered data, all initiatives to store and make prehospital patient data available on a large scale are pointless in advance | |
Research in prehospital emergency care in the Netherlands would benefit from more collaboration | |
Laws and regulations | The General Data Protection Regulation (GDPR) and its variable interpretation are a major obstacle to conducting research in prehospital emergency care |
Separate legislation and regulations must be drawn up for medical scientific research outside the hospital | |
A designated Medical Ethics Review Committee (MREC) with knowledge about the assessment of prehospital medical scientific research should be installed | |
Financial aspects | There are currently insufficient funding options for conducting research in prehospital emergency care in the Netherlands |
There should be a national funding program for scientific research in prehospital emergency care in the Netherlands | |
Regional ambulance care providers should be obliged to invest part of their turnover in scientific research | |
The Dutch National Sector Organization for Ambulance Care should have a facilitating role in financing research projects in prehospital emergency care | |
Organization and culture | The Dutch prehospital emergency care has a long and thorough research history |
Quality control and innovation through scientific research should be among the core tasks of every ambulance care provider | |
Every ambulance worker in the Netherlands should be trained in academic skills | |
Incentive for performing research | The Dutch prehospital emergency care is in need of a professor of prehospital emergency care |
There should be a financial incentive for conducting research in ambulance care | |
There should be a mandatory quality control for ambulance care |
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Vianen, N.J., Maissan, I.M., den Hartog, D. et al. Opportunities and barriers for prehospital emergency medical services research in the Netherlands; results of a mixed-methods consensus study. Eur J Trauma Emerg Surg 50, 221–232 (2024). https://doi.org/10.1007/s00068-023-02240-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-023-02240-w