Abstract
Purpose
The impact of the type of anesthesia (regional vs. general anesthesia) on in-hospital complications in ankle fractures has not been thoroughly studied yet. Identifying factors that place patients at risk for complications following ankle fractures may help reduce their occurrence. The primary goal of this study was (1) to describe the cohort of patients and (2) to evaluate independent risk factors for complications during hospitalization.
Methods
We analyzed patients from 2005 to 2019 with an operatively treated isolated fracture of the medial or lateral malleolus using a prospective national quality measurement database. Patients were selected based on international classifications (ICD) and national procedural codes (CHOP). Uni- and multivariate analysis were applied.
Results
In total, we analyzed 5262 patients who suffered a fracture of the malleolus; 3003 patients (57%) had regional and 2259 (43%) general anesthesia. Patients with regional anesthesia were significantly older (51 vs. 46 years), but healthier (23 vs. 28% comorbidities) than patients who received general anesthesia. The in-hospital complication rate was not significantly lower in regional anesthesia (2.2% vs 3.0%). The type of anesthesia was not an independent predictor for complications while controlling for confounders.
Conclusion
Type of anesthesia was not an independent predictor of complications; however, higher ASA class, age over 70 years, fracture of the medial versus lateral malleolus, longer preoperative stay, and duration of surgery were significant predictors of complications. Patient and procedure characteristics, as well as changes in medical care and epidemiological changes along with patient requests, influenced the choice of the type of anesthesia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ankle fractures are common and often require hospitalization [1]. They typically occur in young and active patients or older patients with reduced bone quality [2]. Previous studies found an increase in the incidence and severity of ankle fractures in recent years, mainly due to the aging population [3,4,5]. In a large Swedish registry study, over 80% of ankle fractures required operative treatment [6]. Depending on the patients age and comorbidities, different types of anesthesia may be preferred. Surgical treatment of ankle fractures is usually performed under general or regional anesthesia. Previous research on hip and knee arthroplasty suggests regional anesthesia may have lower complication rates and shorter hospital stays compared to general anesthesia [7,8,9,10].
However, the influence of the type of anesthesia on short-term complications in ankle fractures has not been well studied. Identifying factors that place patients at risk for complications following ankle fractures may help to reduce their occurrence.
This study aimed to investigate the association between the type of anesthesia and in-hospital complications in patients with operatively treated ankle fractures.
Methods
Study design
This study was conducted using a prospective surgical registry from the “Working Group for Quality Assurance in Surgery” (known in German as “Arbeitsgemeinschaft für Qualitätssicherung in der Chirurgie”, AQC). The goal of the AQC is to collect data on various operative interventions and surgical diseases and injuries [11]. The aim is to ensure quality assurance in surgery. Over 80 Swiss surgical departments register their surgical in-hospital cases online using the AdjumedCollect tool [12].
The AQC database is based on a two-part questionnaire. The first part contains information concerning the operation(s). Patient and general hospitalization information is collected in the second part of the questionnaire.
The AQC data include information on intraoperative and postoperative complications as well as general case-related complications. These are classified according to complications in the context of surgical access, positioning of the patient, the wound, and the corresponding operation performed. The case-related complications are listed by organ system, e.g., pulmonary, cardiac, and gastrointestinal with the most relevant respective associated diagnoses. Pain or a necessary reoperation was not counted as a complication per se, but the cause for which a reoperation became necessary, e.g., rotation error or instability.
The study has been approved by the institutional review board—no approval of the local cantonal ethical review board was needed because no identifiable patient information is registered in the AQC database. The present study was performed according to the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines [13].
Study subjects
All patients found in the AQC register between January 1, 2005, and December 31, 2019, with an operatively treated isolated fracture of the medial or lateral malleolus were included in our study. We identified patients with the corresponding World Health Organization (WHO) International Classification of Disease Code (ICD-10) [14] S82.5 (fractures of the medial malleolus) and S82.6 (fractures of the lateral malleolus).
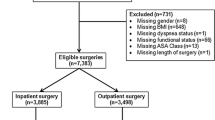
Exclusion criteria included a lack of information on the operation or the patient.
From 5839 cases, a total of 5262 patients met our criteria and were included for further examination.
Variables and outcome measures
The aim of this retrospective study was to investigate the outcome differences in malleolar fractures depending on the type of anesthesia used.
Possible confounders, such as age, sex, ASA classification, type of injury, experience level of surgeon, surgery and ICU duration, thromboembolism and antibiotic prophylaxis were assessed.
Statistical analysis
Analysis between groups of categorical data was done using the Chi-squared test and presented as the number of patients and percentages. The Student’s t-test was used to assess differences in means between groups for numerical data.
Binary logistic regression was used to determine independent risk factors for complications. A p < 0.05 was considered statistically significant. SPSS Version 26 (IBM, Armonk, New York, USA) was used to analyze the data.
Results
This study included a total of 5262 patients who suffered a fracture of the medial or lateral malleolus with a mean age of 49 years. Fifty-one percent of the patients were male.
In total, 57% (n = 3003) of the patients received a regional anesthesia. Fractures of the lateral malleolus were proportionally more frequently operated under regional anesthesia.
Patients with regional anesthesia were significantly older (51 vs. 46 years), healthier (lower ASA-classification), with less comorbidities (23% vs. 28%) than patients who received general anesthesia (p < 0.001) (Table 1).
Patients with regional anesthesia were operated on by more experienced surgeons (p < 0.001) and had shorter procedural duration (p < 0.001). In addition, the regional anesthesia cohort received fewer prophylactic antibiotics (p < 0.001). Table 2).
Outcome
Patients with regional anesthesia had a statistically significant shorter length of stay (6.7 vs. 7.8 days; p = < 0.001). Overall complications were comparable between both groups (3.0% vs. 2.2%; p = 0.079). The mortality rate did not differ, neither comparing the main diagnosis nor the type of anesthesia.
The most common reported intraoperative complications were lesions of the artery or tendon, a peripheral nerve lesion, thermal lesion, and iatrogenic fracture. The most common postoperative complications reported were wound-healing disorder, wound infection, secondary dislocation, and instability. The most common reported case-related complications were myocardial infarction, respiratory insufficiency, urinary tract infection and acute psychosis.
In multivariate analysis for any complications, the anesthesia type was not an independent risk factor. But a higher ASA class (III versus I), age over 70 years, fracture of medial versus the lateral malleolus, a longer length of stay preoperative, and duration of surgery were independent risk factors for complications (Table 3).
Discussion
This study aimed to evaluate independent risk factors for complications during hospitalization for patients with operatively treated malleolar fractures, with a focus on the type of anesthesia used. To the best of our knowledge, this has not been studied well. Identifying factors that place patients at risk for complications following ankle fractures may help to reduce their occurrence.
There are different types of anesthesia for fixation of malleolar fractures, mainly regional or general anesthesia [15]. The choice of anesthesia may affect peri-operative recovery and pain control [16], which can impact patient satisfaction with their treatment [17].
In our study, patients with regional anesthesia were significantly older, but healthier than patients who received general anesthesia. Anesthesia type was not an independent predictor for complications after controlling for confounders. This main finding aligns with previous research [18, 19] who showed no differences in complications and mortality comparing spinal and general anesthesia in ankle fractures.
A higher ASA-Score, the age over 70 years, the length of stay preoperative and the duration of surgery were significant predictors for complications in our study.
The importance of the ASA-class on complications in ankle fractures has been previously described [20, 21], especially on surgical site infection [22].
We also found the often-described bimodal age distribution in our cohort [5, 23]. There exist significant differences between men and women regarding age, lifestyle, comorbidities, and the type of ankle fracture sustained [24]. The complication rate in surgically treated ankle fractures increases with age [20, 21, 25]. Danilkowicz et al. found a linear increase in complications after open reduction and internal fixation of ankle fractures with age in 27,633 patients [25]. Interestingly, Gil et al. showed that patients aged 80–89 had a complication rate similar to patients aged 65–79 after controlling for the ASA class [26].
A longer length of stay preoperative is associated with poorer clinical outcomes [27] and poorer quality of life of patients [28, 29]. This relationship may be due to occurred complications who need more time to treat and other factors.
Contrary to the findings of our study, Vora et al. reported that patients with spinal anesthesia for ankle ORIF had a longer length of stay in the hospital [18].
In contrast, we found that the group with regional anesthesia had a shorter length of stay.
Similar to our study, other researchers found that the duration of surgery is an independent risk factor for complications [21, 30]. Louie et al. found that resident involvement per se is not a significant risk factor in malleolar fractures [21].
The effect of our two continuous measures (length of stay and duration of surgery) seems to be rather small. This is because the odds ratio shown only shows the change per additional unit (one day or one minute).
In the past 20 years, there has been a global increase in obesity [31]. A higher bodyweight increases the risk of experiencing a severe ankle fracture in a linear fashion [32]. Obese patients tend to have worse long-term outcomes following a fracture. In our study, we did not have enough data on patient weight to further investigate this effect or other medical conditions that may influence the outcome or more details in fracture type, which also play a role in the outcome [33, 34].
As expected for isolated extremity fractures, the mortality rate in our study was very low,
which is consistent with the findings of previous research on this topic [35, 36].
It is expected that in coming years, older, and sicker patients will need surgery for ankle fractures [37]. This, along with socioeconomic changes, may influence the choice of anesthesia. This trend has already been partially noticed in patients undergoing hip fracture surgery [38]. Patient’s characteristics and the type of surgery may influence the choice between general and regional anesthesia [39].
One potential consideration when choosing the type of anesthesia is the ease of postoperative recovery and the effectiveness of pain control [16]. These factors may impact overall patient satisfaction with their treatment [17].
Limitation
A strength of our study is the large sample size. Because of the nature of the data source, our study has various limitations. One important limitation is the use of de-identified data, which made it impossible to obtain missing information. Furthermore, we only had information about the course of events during hospitalization and no data about further course. Another weakness, as in many registry studies, is the quality of collecting and recording data, which is dependent on many different physicians.
The findings of our study may not be generalizable in other populations or settings, as the study is based on the specific situation and medical procedures in Switzerland.
The results of this study may be affected over time by changes in practices or technologies, which may affect the findings. Especially the development of new drugs and techniques has greatly enhanced the safety of anesthesia, reducing the risk of complications and side effects [40]. In addition, we did not have more detailed information about the anesthesia such as who performed the anesthesia and what technique, and equipment was used.
Conclusion
Type of anesthesia was not an independent predictor of complications; however, higher ASA class, age over 70 years, fracture of the medial versus lateral malleolus, longer preoperative stay, and duration of surgery were significant predictors of complications. Patient and procedure characteristics, as well as changes in medical care and epidemiological changes along with patient requests, influenced the choice of the type of anesthesia.
Data availability
The data that support the findings of this study are available from the corresponding author, [Claudio Canal], upon reasonable request.
References
Jennison T, Brinsden M. Fracture admission trends in England over a ten-year period. Ann R Coll Surg Engl. 2019;101(3):208–14. https://doi.org/10.1308/rcsann.2019.0002 (Epub 2019/01/31, PubMed PMID: 30698459; PubMed Central PMCID: PMCPMC6400910).
Beerekamp MSH, de Muinck Keizer RJO, Schep NWL, Ubbink DT, Panneman MJM, Goslings JC. Epidemiology of extremity fractures in the Netherlands. Injury. 2017;48(7):1355–62. https://doi.org/10.1016/j.injury.2017.04.047 (Epub 2017/05/11, PubMed PMID: 28487101).
Silva ARB, Martinez LC, Pinheiro MM, Szejnfeld VL. Low-trauma ankle fractures in Brazil: secular trends in patients over 50 years old from 2004 to 2013. Arch Osteoporos. 2020;15(1):105. https://doi.org/10.1007/s11657-020-00777-6 (Epub 2020/07/24, PubMed PMID: 32700025).
Elsoe R, Ostgaard SE, Larsen P. Population-based epidemiology of 9767 ankle fractures. Foot Ankle Surg. 2018;24(1):34–9. https://doi.org/10.1016/j.fas.2016.11.002 (Epub 2018/02/08, PubMed PMID: 29413771).
Pflüger P, Wurm M, Biberthaler P, Pförringer D, Crönlein M. Analysis of 6851 foot and ankle injuries from 2010–2017 in an emergency department. Unfallchirurg. 2021. https://doi.org/10.1007/s00113-021-01081-9 (Epub 2021/10/01, PubMed PMID: 34591136).
Thur CK, Edgren G, Jansson K, Wretenberg P. Epidemiology of adult ankle fractures in Sweden between 1987 and 2004: a population-based study of 91,410 Swedish inpatients. Acta Orthop. 2012;83(3):276–81. https://doi.org/10.3109/17453674.2012.672091 (Epub 2012/03/10, PubMed PMID: 22401675; PubMed Central PMCID: PMCPMC3369155).
Contino V, Abrams JH, Arumugam S, Sinha SK, Vellanky SS, Cremins MS, et al. Spinal anesthesia using ropivacaine leads to earlier ambulation after total hip arthroplasty. Orthopedics. 2021;44(3):e343–6. https://doi.org/10.3928/01477447-20210414-04 (Epub 2021/05/28, PubMed PMID: 34039195).
Pugely AJ, Martin CT, Gao Y, Mendoza-Lattes S, Callaghan JJ. Differences in short-term complications between spinal and general anesthesia for primary total knee arthroplasty. J Bone Jt Surg Am. 2013;95(3):193–9. https://doi.org/10.2106/jbjs.K.01682 (Epub 2012/12/28, PubMed PMID: 23269359).
Protić A, Horvat M, Komen-Usljebrka H, Frkovic V, Zuvic-Butorac M, Bukal K, et al. Benefit of the minimal invasive ultrasound-guided single shot femoro-popliteal block for ankle surgery in comparison with spinal anesthesia. Wien Klin Wochenschr. 2010;122(19–20):584–7. https://doi.org/10.1007/s00508-010-1451-9 (Epub 2010/09/25, PubMed PMID: 20865457).
Zixuan L, Chen W, Li Y, Wang X, Zhang W, Zhu Y, et al. Incidence of deep venous thrombosis (DVT) of the lower extremity in patients undergoing surgeries for ankle fractures. J Orthop Surg Res. 2020;15(1):294. https://doi.org/10.1186/s13018-020-01809-0 (Epub 2020/08/02, PubMed PMID: 32736663; PubMed Central PMCID: PMCPMC7393865).
AQC. AQC—Arbeitsgemeinschaft für Qualitätssicherung in den Chirurgischen Disziplinen 2022. https://aqc.ch. 2 Mar 2022.
AG AS. AdjumedAnalyze 2022. https://adjumed.com/en/. 2 Mar 2022.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495–9. https://doi.org/10.1016/j.ijsu.2014.07.013 (Epub 2014/07/22, PubMed PMID: 25046131).
2016 W-I-V. International statistical classification of diseases and related health problems 10th revision: World health organization. 2022. https://icd.who.int/browse10/2016/en. Accessed 5 Mar 2022.
Anderson JG, Bohay DR, Maskill JD, Gadkari KP, Hearty TM, Braaksma W, et al. Complications after popliteal block for foot and ankle surgery. Foot Ankle Int. 2015;36(10):1138–43. https://doi.org/10.1177/1071100715589741 (Epub 20150624, PubMed PMID: 26109605).
Richman JM, Liu SS, Courpas G, Wong R, Rowlingson AJ, McGready J, et al. Does continuous peripheral nerve block provide superior pain control to opioids? A meta-analysis. Anesth Analg. 2006;102(1):248–57. https://doi.org/10.1213/01.Ane.0000181289.09675.7d (Epub 2005/12/22, PubMed PMID: 16368838).
Peters ML, Sommer M, de Rijke JM, Kessels F, Heineman E, Patijn J, et al. Somatic and psychologic predictors of long-term unfavorable outcome after surgical intervention. Ann Surg. 2007;245(3):487–94. https://doi.org/10.1097/01.sla.0000245495.79781.65 (PubMed PMID: 17435557; PubMed Central PMCID: PMCPMC1877005).
Vora M, Samineni AV, Sing D, Salavati S, Tornetta P 3rd. Spinal anesthesia associated with increased length of stay compared to general anesthesia for ankle open reduction internal fixation: a propensity-matched analysis. J Foot Ankle Surg. 2021;60(2):350–3. https://doi.org/10.1053/j.jfas.2020.08.035 (Epub 2021/01/20, PubMed PMID: 33461921).
Jordan C, Davidovitch RI, Walsh M, Tejwani N, Rosenberg A, Egol KA. Spinal anesthesia mediates improved early function and pain relief following surgical repair of ankle fractures. J Bone Jt Surg Am. 2010;92(2):368–74. https://doi.org/10.2106/jbjs.H.01852 (Epub 2010/02/04, PubMed PMID: 20124064).
Schade MA, Hollenbeak CS. Early postoperative infection following open reduction internal fixation repair of closed malleolar fractures. Foot Ankle Spec. 2018;11(4):335–41. https://doi.org/10.1177/1938640017735887 (Epub 2017/10/17, PubMed PMID: 29029574).
Louie PK, Schairer WW, Haughom BD, Bell JA, Campbell KJ, Levine BR. Involvement of residents does not increase postoperative complications after open reduction internal fixation of ankle fractures: an analysis of 3251 cases. J Foot Ankle Surg. 2017;56(3):492–6. https://doi.org/10.1053/j.jfas.2017.01.020 (Epub 2017/03/02, PubMed PMID: 28245974).
Rascoe AS, Kavanagh MD, Audet MA, Hu E, Vallier HA. Factors associating with surgical site infection following operative management of malleolar fractures at an urban level 1 trauma center. OTA Int. 2020;3(2):e077. https://doi.org/10.1097/oi9.0000000000000077 (Epub 20200506, PubMed PMID: 33937701; PubMed Central PMCID: PMCPMC8022901).
Pflüger P, Wurm M, Biberthaler P, Pförringer D, Crönlein M. Analysis of 6851 foot and ankle injuries from 2010–2017 in an emergency department. Unfallchirurgie (Heidelb). 2022;125(10):801–10. https://doi.org/10.1007/s00113-021-01081-9 (Epub 20210930, PubMed PMID: 34591136; PubMed Central PMCID: PMCPMC9515139).
Vieira Cardoso D, Dubois-Ferrière V, Gamulin A, Baréa C, Rodriguez P, Hannouche D, et al. Operatively treated ankle fractures in Switzerland, 2002–2012: epidemiology and associations between baseline characteristics and fracture types. BMC Musculoskelet Disord. 2021;22(1):266. https://doi.org/10.1186/s12891-021-04144-5 (Epub 2021/03/13, PubMed PMID: 33706724; PubMed Central PMCID: PMCPMC7953683).
Danilkowicz RM, Grimm NL, Kim J, O’Donnell JA, Allen NB, Adams SB. Increasing age and modifiable comorbidities are associated with short-term complications after open reduction and internal fixation of ankle fractures. Eur J Orthop Surg Traumatol. 2022;32(1):113–9. https://doi.org/10.1007/s00590-021-02927-z (Epub 2021/03/25, PubMed PMID: 33759030).
Gil JA, Goodman AD, Kleiner J, Walsh DF, Kosinski LR, Hsu R. Mortality and morbidity of surgical management of geriatric ankle fractures. J Am Acad Orthop Surg. 2020;28(16):678–83. https://doi.org/10.5435/jaaos-d-19-00048 (Epub 2020/08/10, PubMed PMID: 32769723).
Pilskog K, Gote TB, Odland HEJ, Fjeldsgaard KA, Dale H, Inderhaug E, et al. Association of delayed surgery for ankle fractures and patient-reported outcomes. Foot Ankle Int. 2022. https://doi.org/10.1177/10711007211070540 (Epub 2022/02/22, PubMed PMID: 35184581).
De Las Heras Romero J, Lledó Alvarez A, Torres Sánchez C, Luna Maldonado A. Operative treatment of ankle fractures: predictive factors affecting outcome. Cureus. 2020;12(10):e11016. https://doi.org/10.7759/cureus.11016 (Epub 20201018, PubMed PMID: 33094040; PubMed Central PMCID: PMCPMC7574997).
Velleman J, Nijs S, Hoekstra H. Operative management of AO type 44 ankle fractures: determinants of outcome. J Foot Ankle Surg. 2018;57(2):247–53. https://doi.org/10.1053/j.jfas.2017.08.021 (Epub 20171219, PubMed PMID: 29273186).
Vehling M, Canal C, Ziegenhain F, Pape HC, Neuhaus V. Short-term outcome of isolated lateral malleolar fracture treatment is independent of hospital trauma volume or teaching status: a nationwide retrospective cohort study. Eur J Trauma Emerg Surg. 2021. https://doi.org/10.1007/s00068-021-01771-4 (Epub 2021/08/17, PubMed PMID: 34398247).
Arroyo-Johnson C, Mincey KD. Obesity Epidemiology Worldwide. Gastroenterol Clin North Am. 2016;45(4):571–9. https://doi.org/10.1016/j.gtc.2016.07.012 (PubMed PMID: 27837773; PubMed Central PMCID: PMCPMC5599163).
Cardoso DV, Paccaud J, Dubois-Ferrière V, Barea C, Hannouche D, Veljkovic A, et al. The effect of BMI on long-term outcomes after operatively treated ankle fractures: a study with up to 16 years of follow-up. BMC Musculoskelet Disord. 2022;23(1):317. https://doi.org/10.1186/s12891-022-05247-3 (Epub 20220404, PubMed PMID: 35379212; PubMed Central PMCID: PMCPMC8978374).
Smeeing DPJ, Briet JP, van Kessel CS, Segers MM, Verleisdonk EJ, Leenen LPH, et al. Factors associated with wound- and implant-related complications after surgical treatment of ankle fractures. J Foot Ankle Surg. 2018;57(5):942–7. https://doi.org/10.1053/j.jfas.2018.03.050 (Epub 2018/07/15, PubMed PMID: 30005967).
SooHoo NF, Krenek L, Eagan MJ, Gurbani B, Ko CY, Zingmond DS. Complication rates following open reduction and internal fixation of ankle fractures. J Bone Jt Surg Am. 2009;91(5):1042–9. https://doi.org/10.2106/jbjs.H.00653 (Epub 2009/05/05, PubMed PMID: 19411451).
Reider L, Pollak A, Wolff JL, Magaziner J, Levy JF. National trends in extremity fracture hospitalizations among older adults between 2003 and 2017. J Am Geriatr Soc. 2021;69(9):2556–65. https://doi.org/10.1111/jgs.17281 (Epub 2021/06/02, PubMed PMID: 34062611).
Basques BA, Miller CP, Golinvaux NS, Bohl DD, Grauer JN. Morbidity and readmission after open reduction and internal fixation of ankle fractures are associated with preoperative patient characteristics. Clin Orthop Relat Res. 2015;473(3):1133–9. https://doi.org/10.1007/s11999-014-4005-z (Epub 2014/10/23, PubMed PMID: 25337977; PubMed Central PMCID: PMCPMC4317425).
Happonen V, Kröger H, Kuismin M, Sund R. Ankle fractures in Finland: 118,929 operatively treated between 1987 and 2019. Acta Orthop. 2022;93:327–33. https://doi.org/10.2340/17453674.2022.2071 (Epub 2022/02/12, PubMed PMID: 35147707; PubMed Central PMCID: PMCPMC8833737).
Maxwell BG, Spitz W, Porter J. Association of increasing use of spinal anesthesia in hip fracture repair with treating an aging patient population. JAMA Surg. 2020;155(2):167–8. https://doi.org/10.1001/jamasurg.2019.4471 (Epub 2019/11/21, PubMed PMID: 31746959; PubMed Central PMCID: PMCPMC6902104).
Capdevila X, Aveline C, Delaunay L, Bouaziz H, Zetlaoui P, Choquet O, et al. Factors determining the choice of spinal versus general anesthesia in patients undergoing ambulatory surgery: results of a multicenter observational study. Adv Ther. 2020;37(1):527–40. https://doi.org/10.1007/s12325-019-01171-6 (Epub 2019/12/13, PubMed PMID: 31828612; PubMed Central PMCID: PMCPMC6979445).
Harbell MW, Methangkool E. Patient safety education in anesthesia: current state and future directions. Curr Opin Anaesthesiol. 2021;34(6):720–5. https://doi.org/10.1097/aco.0000000000001060 (PubMed PMID: 34817450).
Funding
Open access funding provided by University of Zurich. No funding to declare.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethical review committee statement
The data of this study are based on anonymized, de-identified data; our institutional review board waves the necessity for cantonal institutional review board approval.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Canal, C., Kaserer, A., Morax, L.S. et al. Does the type of anesthesia (regional vs. general) represent an independent predictor for in-hospital complications in operatively treated malleolar fractures? A retrospective analysis of 5262 patients. Eur J Trauma Emerg Surg 49, 1587–1593 (2023). https://doi.org/10.1007/s00068-023-02235-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-023-02235-7