Abstract
Background
In-hospital complications after trauma may result in prolonged stays, higher costs, and adverse functional outcomes. Among reported risk factors for complications are pre-existing cardiopulmonary comorbidities. Objective and quick evaluation of cardiovascular risk would be beneficial for risk assessment in trauma patients. Studies in non-trauma patients suggested an independent association between cardiovascular abnormalities visible on routine computed tomography (CT) imaging and outcomes. However, whether this applies to trauma patients is unknown.
Purpose
To assess the association between cardiopulmonary abnormalities visible on routine CT images and the development of in-hospital complications in patients in a level-1 trauma center.
Methods
All trauma patients aged 16 years or older with CT imaging of the abdomen, thorax, or spine and admitted to the UMC Utrecht in 2017 were included. Patients with an active infection upon admission or severe neurological trauma were excluded. Routine trauma CT images were analyzed for visible abnormalities: pulmonary emphysema, coronary artery calcifications, and abdominal aorta calcification severity. Drug-treated complications were scored. The discharge condition was measured on the Glasgow Outcome Scale.
Results
In total, 433 patients (median age 50 years, 67% male, 89% ASA 1–2) were analyzed. Median Injury Severity Score and Glasgow Coma Scale score were 9 and 15, respectively. Seventy-six patients suffered from at least one complication, mostly pneumonia (n = 39, 9%) or delirium (n = 19, 4%). Left main coronary artery calcification was independently associated with the development of any complication (OR 3.9, 95% CI 1.7–8.9). An increasing number of calcified coronary arteries showed a trend toward an association with complications (p = 0.07) and was significantly associated with an adverse discharge condition (p = 0.02). Pulmonary emphysema and aortic calcifications were not associated with complications.
Conclusion
Coronary artery calcification, visible on routine CT imaging, is independently associated with in-hospital complications and an adverse discharge condition in level-1 trauma patients. The findings of this study may help to identify trauma patients quickly and objectively at risk for complications in an early stage without performing additional diagnostics or interventions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
In the Netherlands, over 19,000 patients were admitted to a level-1 trauma center in 2017 [1]. In-hospital complication rates in level-1 trauma patients vary between 4.2 and 24.7% and are associated with prolonged stay, higher costs, and increased mortality [2,3,4,5]. In addition, a complicated hospital stay is associated with worse long-term functional outcomes, such as decreased mobility and social activity [6]. Infectious complications are the most prevalent, associated with increased mortality, and considered quality indicators [5, 7,8,9].
Previous studies in trauma patients have shown risk factors for developing complications, including age, sex, injury severity, and pre-existing cardiopulmonary comorbidities [10,11,12,13,14,15]. Most of these studies were based on medical history data to assess comorbidities. Risk factors for cardiovascular disease include age, smoking, high body mass index, diabetes mellitus, hyperlipidemia, hypertension, and renal disease [16,17,18]. Some risk factors can be easily obtained from medical history or through anamnesis. However, performing extensive anamnesis in the trauma bay can be challenging, and, for instance, blood pressure or renal function can be affected due to trauma. An objective and quick evaluation of cardiovascular disease in trauma patients would be helpful in risk assessment. Recent literature showed that cardiopulmonary abnormalities on routinely performed computed tomography (CT) images may independently predict short- and long-term outcomes in non-trauma patients [19,20,21]. In these studies, chest CTs were performed for various clinical purposes, while, to our knowledge, no such studies have been performed in trauma populations yet. CT images are routinely taken in trauma patients admitted to the trauma bay with suspected injuries of the chest or abdomen. These CT images can show abnormalities, suspectable for cardiopulmonary disease, that might predict complications.
Identifying patients at increased risk of complications might help prevent complications, as prophylactic treatment and additional tests could be started early. Yet, it remains unknown whether CT visible cardiopulmonary abnormalities can predict complications after trauma. Therefore, this study assessed the association between cardiopulmonary abnormalities visible on routine CT images and the development of in-hospital complications and discharge outcomes in patients in a level-1 trauma center.
Methods
Study design and participants
A retrospective cohort study was performed at the University Medical Center Utrecht (UMCU), a level-1 trauma center in the Netherlands. The medical ethical committee of the UMCU approved this study and waived the need for consent (protocol number 20-599/C).
Trauma patients aged 16 years or older and hospitalized between January 1st, 2017, and December 31st, 2017, were identified through the local trauma registry. All consecutive patients who underwent CT imaging of the thorax, abdomen, aorta, thoracic spine, or lumbar spine within seven days of admission were included. At least one of the predefined radiologic parameters had to be assessed on these CT images. Exclusion criteria were an active infection upon admission, active outpatient antibiotic treatment or prophylaxis upon admission, transfer to another hospital during hospital admission, or treatment for more than 24 h in another hospital before transportation to the UMCU. Patients who suffered from severe brain injury—defined as an Abbreviated Injury Scale (AIS) score of the head of 3 or higher—were excluded as well since these injuries almost exclusively determine these patients' prognosis [22, 23].
Radiologic imaging and technique
All CT imaging was routinely performed using either 64- or 256-detector row scanners from Philips Medical Systems (Cleveland, OH, USA). All CT images were viewed using PACS IDS7 21.1.2 (SECTRA), and 0.9 and 5.0-mm slices were available. An intravenous contrast agent was administered in abdominal or thoracic CT imaging during trauma screening or angiographic scans of the aorta. In case an intravenous contrast agent was administered (89.6%, n = 388), the split bolus technique was used to simultaneously assess the portal and the arterial phase.
Radiologic parameter definitions and assessment
Thoracic CT images were analyzed for the presence of coronary artery calcifications and pulmonary emphysema, and abdominal CT images for the presence of calcification in the abdominal aorta and its degree of severity when present.
The coronary arteries and abdominal aorta were assessed on CT images in the bone and soft tissue settings; only calcified plaques were identified. The presence of coronary calcifications was assessed for the left main coronary artery (LM), left anterior descending (LAD) artery, left circumflex (LCx) artery, and right coronary artery (RCA) separately. The extent of calcification of the abdominal aorta was determined based on its circularity and divided per 90 degrees of circularity (i.e., possible scoring of 0 up to 4) as previously described by Hendriks et al. [24]. Pulmonary emphysema was determined using the pulmonary setting and considered present in case centrilobular emphysema was observed. Only centrilobular emphysema was considered in this study, as this specific entity has been associated with smoking, in contrast to other entities that might have more genetic or uncertain etiologies [25].
Two medical doctors (TK, AS) performed the radiologic assessment and discussed borderline cases with a senior staff radiologist with over 13 years of experience in thoracic and abdominal CT imaging evaluation (PdJ). The investigators were blinded to the outcomes during the radiologic analysis. Both investigators and the senior staff radiologist assessed sixty randomly selected cases to evaluate interobserver variability. The results of the interobserver variability analysis were very good, with Cohen's kappas of 0.77 or higher (Supplemental Table 1).
The inclusion criterion was any relevant CT imaging of the chest or abdomen. Therefore, it was unfeasible to assess all radiologic parameters in every patient. For example, when only abdominal imaging was performed, assessment of the coronary arteries was automatically excluded. If one or more radiologic parameters were unavailable, only these parameters were excluded from the analysis, while the available parameters were included. The number of incomplete examinations was stated in the tables as ‘missing’. No imputation methods were performed since we aimed to assess routine CT imaging. The results may be applied easily in patients with routine imaging; imputation methods would not increase the implementation of this opportunistic screening.
Outcomes
The medical health records were screened for outcomes. The primary outcome was the development of one or more complications, cumulated from all separately scored complications: infectious complications treated with antibiotics (i.e., pneumonia, urinary tract infection, wound infection, other infectious complications) and pharmacologically managed delirium (e.g., antipsychotics or benzodiazepines). Diagnosis and treatment of complications were part of regular care; no additional clinical criteria were used.
Secondary outcomes were intensive care unit (ICU) admission, hospital length of stay (HLOS) and ICU length of stay, days on mechanical ventilation, and the discharge condition measured using the Glasgow Outcome Scale (GOS) score. The local trauma registry provided secondary outcomes.
Follow-up lasted until hospital discharge or in-hospital death. No censoring for competing risks was performed; patients that died during hospital stay (1.8%, n = 8) were included in the analyses.
Variables
The local trauma registry provided age, gender, pre-trauma American Society of Anesthesiologists (ASA) classification, Injury Severity Score (ISS), Glasgow Coma Scale (GCS) score, AIS codes, and mechanism of injury. Radiologic images were obtained from the medical records manually.
Statistical analysis
All statistical analyses were performed using RStudio 1.4.1717 for Mac (© The R Foundation for Statistical Computing, 2019) with additional packages. The GOS score was separated into a favorable (i.e., good recovery or light disability) or an adverse discharge condition (i.e., severe disability, persistent vegetative state, or mortality) for further analysis. Coronary calcifications of the LAD, LCx, and RCA were made ordinal into one-, two-, or three-vessel coronary artery calcifications—as inspired by coronary artery disease; the LM was separately considered since it is considered a more severe condition associated with multivessel coronary artery disease [26, 27]. ASA classification was dichotomized into severe (ASA 3–4) or no severe comorbidities (ASA 1–2).
Normally distributed variables were described using the mean and standard deviation (SD), non-normally distributed or ordinal variables using the median and interquartile range (IQR), and categorical variables using the proportions.
The association between radiologic abnormalities and several outcomes—complications, infectious complications, pneumonia, delirium, an adverse discharge condition, and HLOS—was assessed. HLOS was log-transformed before analyses. Results were back-transformed before being presented.
Logistic regression analysis was used for the dichotomous and ordinal outcomes; results were presented with the odds ratio (OR) and 95% confidence interval (95% CI). Linear regression analysis was used for HLOS; results were presented with the beta-coefficient and 95% CI. Regression analyses were performed crude and adjusted for covariates. Age, sex, ASA classification, and ISS were chosen as covariates for each separate radiologic abnormality parameter based on clinical experience and previous literature [10,11,12,13,14,15]. Furthermore, age is a risk factor for the radiologic parameters [16,17,18, 28].
The p for trend was calculated for the number of coronary arteries and the degree of abdominal aorta calcification. In crude analysis, the Cochran-Armitage test was used for dichotomous or ordinal variables; linear regression was used for HLOS. In multivariable analysis, the additional value of the ordinal value to the model was assessed using the likelihood ratio test for all outcomes.
Outcomes were considered statistically significant with a p value < 0.05 despite the number of evaluated associations. No correction for multiple testing was made because of the study's explorative nature.
Results
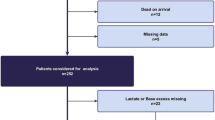
During the study period, 658 patients underwent a CT scan of the abdomen, thorax, lumbar or thoracic spine, or aorta within seven days of hospital admission. The study cohort consisted of 433 patients after the exclusion of patients due to infection (n = 10) or administration of antibiotics (n = 12), transfer to another hospital or treatment elsewhere for > 24 h (n = 49), an AIS of the head of 3 or higher (n = 153), or insufficient information after transfer to the UMCU (n = 1).
In the study cohort, the median age was 50 years (IQR 30–65), 67.0% of patients were male (n = 290), 33.0% were female (n = 143), and most patients were in good health prior to trauma (88.7% ASA classification 1–2). The most prevalent mechanisms of injury were motorized vehicle crashes (35.3%), low-energetic falls (21.7%), high-energetic falls (15.5%), and bicycle accidents (15.2%). The median ISS was 9 (IQR 5–14), and the median GCS score at admission was 15 (IQR 14–15). The scan was made within one day of emergency department admission in 98.6% (n = 427) of patients. All cohort characteristics are summarized in Table 1, and differences between subgroups in Supplemental Table 2.
Seventy-six patients (17.6%) suffered from one or more complications during their hospital stay. The most prevalent complications were pneumonia in 39 patients (9.0%) and delirium in 19 patients (4.4%). Twenty-seven patients (6.2%) had an adverse GOS score, of whom eight patients (1.8%) died during hospital stay. One death was due to pneumonia. The other deaths were direct sequelae of traumatic injuries (Table 2).
Table 3 shows the associations between all considered radiologic predictors and the development of one or more complications. Supplemental Tables 3–7 summarize the regression analysis results for the specific complications, HLOS, and an adverse discharge condition.
Coronary artery calcifications showed associations with several outcomes. Both LM calcification (OR 4.5, 95% CI 2.3–8.8) and the number of coronary arteries with calcifications (p for trend < 0.001) were associated with complications. After adjustment for covariates, calcification of the LM (OR 3.9, 95% CI 1.7–8.9) was still significantly associated with the development of complications; coronary artery calcifications still showed strong signals of an association with complications, yet without significantly adding value to the multivariable model (p likelihood = 0.07). LM calcifications increased the risk of developing an infectious complication (OR 3.9, 95% CI 1.6–9.2) and delirium (OR 3.3, 95% CI 1.0–11.1). The association between LM calcification and HLOS was not statistically significant (β coefficient 1.3, p = 0.07). Furthermore, the number of calcified coronary arteries significantly contributed to predicting an adverse discharge condition (p likelihood = 0.02).
The degree of the abdominal aorta calcification was significantly associated with complications (p for trend < 0.001), pneumonia (p = 0.01), delirium, infectious complications, and HLOS (all p < 0.001) in crude analysis but with none of the outcomes after adjustment.
Pulmonary emphysema showed no association with the development of complications in the crude or adjusted logistic regression analysis. Pulmonary emphysema was only associated with developing an infectious complication in crude analysis (p = 0.02), which was no longer apparent in the multivariable model.
Discussion
The current study assessed whether cardiopulmonary abnormalities visible on routine trauma CT predict in-hospital complications in Dutch level-1 trauma patients. To our knowledge, this is the first study that considers associations between these radiologic parameters and complications in trauma patients. Calcification in the left main coronary artery was independently associated with developing any in-hospital complication, infectious complications, and delirium. An increasing number of calcified coronary arteries showed a trend towards an independent association with in-hospital complications and was significantly associated with an adverse discharge condition. Pulmonary emphysema and calcification of the abdominal aorta were not independently associated with complications or outcomes.
Previous studies in trauma patients that investigated comorbidities as a risk factor for complications frequently used either ASA classification or the Charlson Comorbidity Index (CCI) to score the severity of comorbidities [11, 12, 14, 15]. A study by Lima et al. of elderly hip fracture patients found that the CCI score was not independently associated with in-hospital delirium (p ≥ 0.862), but heart disease and chronic obstructive pulmonary disease were [14]. When considering 30-day complications in elderly hip fracture patients, CCI is significantly associated with complications, but ASA classification appears to be a better predictor [29]. In the current study, calcification of the LM was still associated with complications, even after adjustment for ASA classification [12]. Hence, a quick assessment of the LM might provide additional predictive value, besides other proven predictors, to identify trauma patients at risk for in-hospital complications.
The findings in the current study correspond with previous studies of non-trauma patients. Borggreve et al. found that coronary artery calcification is independently associated with anastomotic leakage in esophagectomy patients (OR 2.3, 95% CI 1.3–4.1) [19]. Their multivariable analysis corrected for age, body-mass index, comorbidities (i.e., cardiovascular, chronic obstructive pulmonary disease, diabetes mellitus), and a history of smoking. Coronary artery calcifications were considered an ordinal variable, with a score ranging from 0 to 2 (with a higher score representing more severe calcifications), though the number of affected arteries was not considered. The present study of trauma patients reported similar odds ratios for complication development when considering the LM.
Coronary artery disease is often concomitant with other comorbidities, such as diabetes, hypertension, and obesity [16,17,18]. Moreover, patients with LM coronary artery disease have poorer outcomes than patients without an affected LM [30]. Therefore, one could speculate that LM calcification is indicative of a higher (pre-trauma) risk profile with decreased resilience and subsequently with in-hospital complications in trauma patients.
Cohen's kappas were very good for all measured radiologic predictors. This coefficient was calculated for sixty randomly selected patients, in whom both the senior staff radiologist and the scoring investigators without any significant radiologic experience scored the considered radiologic abnormalities. Therefore, readers with limited experience could perform a quick but proper risk assessment in the emergency department. The reliability and convenience of the described cardiovascular and pulmonary abnormalities enable opportunities for future clinical implementation.
The results of this study provide a basis for future research. Screening for coronary artery calcification could aid in patient-specific and early risk assessment. Ultimately, earlier diagnostics and preventative measures could be initiated. Trauma patients might benefit from opportunistic screening using routine trauma CT images. However, this potential requires further study, and external validation of our findings in a comparable trauma population is needed. Furthermore, adding patient-specific risk factors to prediction models and performance analyses could result in quality improvement. Also, it could improve benchmark analysis across medical centers and medical systems.
In addition to a basis for future research, it could be interesting to assess other cardiovascular abnormalities visible on CT imaging, such as calcifications in the supra-aortic and iliac arteries. These predictors also could illustrate a worse pre-injury condition. Moreover, determining a patient-specific condition might be predictive for complications we did not investigate, such as arrhythmias, electrolyte disorders, and respiratory failure.
There were several limitations to the current study. Firstly, the models might have been overfitted due to the small number of events in the study cohort, possibly resulting in overestimating or underestimating the actual effect sizes. Furthermore, the small number of events in this study population could limit the power of our study; no (post hoc) power analysis was conducted. Secondly, coronary calcifications were scored on CT images performed according to our trauma protocol instead of electrocardiogram-guided, which is requisite in actual diagnostics. The routine imaging mode attenuates the possibility of detecting small calcifications in the coronary arteries or grading stenosis severity; however, the study situation reflects clinical practice in the trauma setting and is not intended for dedicated coronary artery disease diagnosis. Thirdly, we did not correct for competing risks using a statistical method, such as Fine and Gray modeling. Competing risks impede the occurrence of the (primary) outcome. The main competing risk in our study was death, which was part of an adverse discharge condition. We hypothesize that deceased patients were in a worse clinical state before dying than those alive were before being discharged; the development of a complication would be more likely around death than discharge. Hence, the eight deaths among 433 patients with 93 complications might have resulted in a small underestimation of the actual effect size. Lastly, patients could be included with first CT imaging up to seven days after admission. This criterion makes it harder to select the exact moment that opportunistic screening can be performed for risk assessment, and the indication for imaging will be different for early and later CT scans. However, as roughly 100% of the analyzed images were made within one day of admission, the results remain directive for early risk assessment. Furthermore, the results and conclusions were similar when only patients with a CT on the day of admission were included in the analyses (unpublished data).
In conclusion, left main coronary artery calcification visible on routine CT imaging in level-1 trauma patients was independently associated with in-hospital complications. Furthermore, increasing multivessel coronary artery calcification visible on CT is significantly associated with an adverse discharge condition. The findings of this study may help to identify trauma patients quickly and objectively at risk for complications in an early stage without performing additional diagnostics or interventions.
Data availability
The study data will not be made available.
Abbreviations
- AIS:
-
Abbreviated Injury Scale
- ASA:
-
American Society of Anesthesiologists
- CCI:
-
Charlson Comorbidity Index
- CI:
-
Confidence interval
- CT:
-
Computed tomography
- GCS:
-
Glasgow Coma Scale
- GOS:
-
Glasgow Outcome Scale
- HLOS:
-
Hospital length of stay
- ICU:
-
Intensive care unit
- IQR:
-
Interquartile range
- ISS:
-
Injury Severity Score
- LAD:
-
Left anterior descending coronary artery
- LCx:
-
Left circumflex coronary artery
- LM:
-
Left main coronary artery
- OR:
-
Odds ratio
- RCA:
-
Right coronary artery
- SD:
-
Standard deviation
- UMCU:
-
University Medical Center Utrecht
References
Kuipers EJ, Leenen LPH. Nationwide Trauma Registry 2013–2017. 2018.
Jakobsen RK, Bonde A, Sillesen M. Assessment of post-trauma complications in eight million trauma cases over a decade in the USA. Trauma Surg Acute Care Open. 2021;6(1): e000667. https://doi.org/10.1136/tsaco-2020-000667.
Halvachizadeh S, Baradaran L, Cinelli P, Pfeifer R, Sprengel K, Pape HC. How to detect a polytrauma patient at risk of complications: a validation and database analysis of four published scales. PLoS ONE. 2020;15(1): e0228082. https://doi.org/10.1371/journal.pone.0228082.
Osler T, Glance LG, Hosmer DW. Complication-associated mortality following trauma: a population-based observational study. Arch Surg. 2012;147(2):152–8. https://doi.org/10.1001/archsurg.2011.888.
Glance LG, Stone PW, Mukamel DB, Dick AW. Increases in mortality, length of stay, and cost associated with hospital-acquired infections in trauma patients. Arch Surg. 2011;146(7):794–801. https://doi.org/10.1001/archsurg.2011.41.
Holbrook TL, Hoyt DB, Anderson JP. The impact of major in-hospital complications on functional outcome and quality of life after trauma. J Trauma. 2001;50(1):91–5. https://doi.org/10.1097/00005373-200101000-00016.
Komori A, Iriyama H, Kainoh T, Aoki M, Naito T, Abe T. The impact of infection complications after trauma differs according to trauma severity. Sci Rep. 2021;11(1):13803. https://doi.org/10.1038/s41598-021-93314-5.
Abe T, Komori A, Shiraishi A, Sugiyama T, Iriyama H, Kainoh T, et al. Trauma complications and in-hospital mortality: failure-to-rescue. Crit Care. 2020;24(1):223. https://doi.org/10.1186/s13054-020-02951-1.
Moore L, Lauzier F, Stelfox HT, Kortbeek J, Simons R, Berthelot S, et al. Derivation and validation of a quality indicator to benchmark in-hospital complications among injury admissions. JAMA Surg. 2016;151(7):622–30. https://doi.org/10.1001/jamasurg.2015.5484.
Andermahr J, Greb A, Hensler T, Helling HJ, Bouillon B, Sauerland S, et al. Pneumonia in multiple injured patients: a prospective controlled trial on early prediction using clinical and immunological parameters. Inflamm Res. 2002;51(5):265–72.
Brown CA, Boling J, Manson M, Owens T, Zura R. Relation between prefracture characteristics and perioperative complications in the elderly adult patient with hip fracture. South Med J. 2012;105(6):306–10. https://doi.org/10.1097/SMJ.0b013e3182574bfd.
Folbert EC, Hegeman JH, Gierveld R, van Netten JJ, Velde DV, Ten Duis HJ, et al. Complications during hospitalization and risk factors in elderly patients with hip fracture following integrated orthogeriatric treatment. Arch Orthop Trauma Surg. 2017;137(4):507–15. https://doi.org/10.1007/s00402-017-2646-6.
Lakomkin N, Sathiyakumar V, Wick B, Shen MS, Jahangir AA, Mir H, et al. Incidence and predictive risk factors of postoperative sepsis in orthopedic trauma patients. J Orthop Traumatol. 2017;18(2):151–8. https://doi.org/10.1007/s10195-016-0437-4.
Lima BR, Nunes BKG, Guimaraes L, Almeida LF, Pagotto V. Incidence of delirium following hospitalization of elderly people with fractures: risk factors and mortality. Rev Esc Enferm USP. 2021;55: e20200467. https://doi.org/10.1590/1980-220X-REEUSP-2020-0467.
Warnack E, Pachter HL, Choi B, DiMaggio C, Frangos S, Klein M, et al. Postinjury complications: retrospective study of causative factors. JMIR Hum Factors. 2019;6(3): e14819. https://doi.org/10.2196/14819.
Kimani C, Kadota A, Miura K, Fujiyoshi A, Zaid M, Kadowaki S, et al. Differences between coronary artery calcification and aortic artery calcification in relation to cardiovascular disease risk factors in Japanese men. J Atheroscler Thromb. 2019;26(5):452–64.
Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140:e596–646. https://doi.org/10.1161/CIR.0000000000000678.
Yazdanyar A, Newman AB. The burden of cardiovascular disease in the elderly: morbidity, mortality, and costs. Clin Geriatr Med. 2009;25(4):563–vii. https://doi.org/10.1016/j.cger.2009.07.007.
Borggreve AS, Goense L, van Rossum PSN, van Hillegersberg R, de Jong PA, Ruurda JP. Generalized cardiovascular disease on a preoperative CT scan is predictive for anastomotic leakage after esophagectomy. Eur J Surg Oncol. 2018;44(5):587–93. https://doi.org/10.1016/j.ejso.2018.01.225.
Takx RA, Vliegenthart R, Mohamed Hoesein FA, Isgum I, de Koning HJ, Mali WP, et al. Pulmonary function and CT biomarkers as risk factors for cardiovascular events in male lung cancer screening participants: the NELSON study. Eur Radiol. 2015;25(1):65–71. https://doi.org/10.1007/s00330-014-3384-6.
de Jong PA, Gondrie MJ, Buckens CF, Jacobs PC, Mali WP, van der Graaf Y, et al. Prediction of cardiovascular events by using non-vascular findings on routine chest CT. PLoS ONE. 2011;6(10): e26036. https://doi.org/10.1371/journal.pone.0026036.
Lansink KW, Gunning AC, Leenen LP. Cause of death and time of death distribution of trauma patients in a level I trauma centre in the Netherlands. Eur J Trauma Emerg Surg. 2013;39(4):375–83. https://doi.org/10.1007/s00068-013-0278-2.
Gravesteijn BY, Sewalt CA, Ercole A, Akerlund C, Nelson D, Maas AIR, et al. Toward a new multi-dimensional classification of traumatic brain injury: a collaborative European NeuroTrauma Effectiveness Research for Traumatic Brain Injury Study. J Neurotrauma. 2020;37(7):1002–10. https://doi.org/10.1089/neu.2019.6764.
Hendriks EJE, de Jong PA, Beulens JWJ, van der Schouw YT, Forbang NI, Wright CM, et al. Annularity of aorto-iliac arterial calcification and risk of all-cause and cardiovascular mortality. JACC Cardiovasc Imaging. 2018;11(11):1718–9. https://doi.org/10.1016/j.jcmg.2018.01.029.
Janssen R, Piscaer I, Franssen FME, Wouters EFM. Emphysema: looking beyond alpha-1 antitrypsin deficiency. Expert Rev Respir Med. 2019;13(4):381–97. https://doi.org/10.1080/17476348.2019.1580575.
Taggart DP, Kaul S, Boden WE, Ferguson TBJ, Guyton RA, Mack MJ, et al. Revascularization for unprotected left main stem coronary artery stenosis stenting or surgery. J Am Coll Cardiol. 2008;51(9):885. https://doi.org/10.1016/j.jacc.2007.09.067.
Serruys PW, Morice MC, Kappetein AP, Colombo A, Holmes DR, Mack MJ, et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;360(10):961. https://doi.org/10.1056/NEJMoa0804626.
Morsch P, Mansour KMK, da Silva ALG. Aging and pulmonary emphysema: current issues. Geriatr Med Care. 2017;1(2):1–6. https://doi.org/10.15761/GMC.1000110.
Hasan O, Barkat R, Rabbani A, Rabbani U, Mahmood F, Noordin S. Charlson comorbidity index predicts postoperative complications in surgically treated hip fracture patients in a tertiary care hospital: retrospective cohort of 1045 patients. Int J Surg. 2020;82:116–20. https://doi.org/10.1016/j.ijsu.2020.08.017.
Lee PH, Ahn JM, Chang MC, Baek S, Yoon SH, Kang SJ, et al. Left main coronary artery disease—secular trends in patient characteristics, treatments, and outcomes. J Am Coll Cardiol. 2016;68(11):1233–46.
Acknowledgements
We would like to express our great appreciation to R.H.H. Groenwold, MD, PhD, for his advice on methodology and statistical considerations. Also, our special thanks go out to A. Alnasser, BA, for his help and efforts in improving the language and grammar of this paper. This greatly increased the readability.
Author information
Authors and Affiliations
Contributions
Conceptualization, all authors. Methodology TK, AS, YK, PdJ, and MvB. Formal analysis TK and AS. Investigation TK and AS. Writing—original draft preparation TK and AS. Writing—review & editing YK, MH, WV, LL, PdJ and MvB. Visualization TK and AS. Supervision MH, WV, LL, PdJ and MvB. All authors have read and agreed to the published version of the manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
PA de Jong is a consultant for Vifor Pharma and Philips Healthcare. WB Veldhuis is a cofounder of Quantib-U, a spin-off from the University Medical Center Utrecht. The Department of Radiology at the University Medical Center Utrecht is receiving research support from Philips Healthcare.
Ethical approval
Ethical approval was waived by the medical ethical committee of the University Medical Center Utrecht in view of the study's retrospective nature, and all the procedures being performed were part of routine care.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kobes, T., Sweet, A.A.R., Klip, I.T. et al. Cardiovascular parameters on computed tomography are independently associated with in-hospital complications and outcomes in level-1 trauma patients. Eur J Trauma Emerg Surg 49, 1295–1302 (2023). https://doi.org/10.1007/s00068-022-02168-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-022-02168-7