Abstract
Background
Pediatric acute appendicitis (AA) is a challenging pathology to diagnose. In the last decades, multiple biomarkers have been evaluated in different human biological samples to improve diagnostic performance. This study aimed to examine the diagnostic performance of serum, fecal and urinary calprotectin as well as the role of the APPY-1 biomarker panel in pediatric acute appendicitis.
Methods
We conducted a systematic review of the literature that involved an extensive search in the main databases of medical bibliography (Medline, PubMed, Web of Science and SciELO). Two independent reviewers selected the relevant articles based on the previously defined inclusion and exclusion criteria. Methodological quality of the selected article was rated using the QUADAS2 index. Data extraction was performed by two independent reviewers. A synthesis of the results, a standardization of the metrics and two random-effect meta-analyses, one for serum calprotectin and one for APPY-1, were performed.
Results
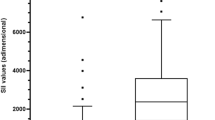
The research resulted in 173 articles. Thirty-eight duplicates were removed. Among the remaining 135 articles, we excluded 125 following the inclusion and exclusion criteria, resulting in the 10 studies included in this review. This systematic review included data from of 3901 participants (1276 patients with confirmed diagnosis of AA and 2625 controls). The age of the participants ranged from 0 to 21 years. Four of the studies compared serum calprotectin values and reported significant differences between groups, but inconsistent results regarding cutoff points, sensitivity and specificity. Two publications compared urinary values of calprotectin and presented inconsistent results regarding sensitivity and specificity as well. One publication evaluated the diagnostic performance of fecal calprotectin, but it did not provide data on measured values. Four studies evaluated the diagnostic performance of APPY-1 test in pediatric acute appendicitis. The calculated pooled sensitivity and specificity of those studies were 97.37 (95% CI 95.60–98.44) and 36.74 (95% CI 32.28–41.44), respectively, and the calculated pooled NLR, 0.0714 (95% CI 0.041–0.115).
Conclusion
Serum calprotectin has limited diagnostic yield in pediatric acute appendicitis. Its performance seems to increase with the hours of clinical evolution and in advanced AA, although the evidence is limited. There is not enough evidence on the usefulness of urinary or fecal calprotectin in the diagnosis of pediatric acute appendicitis. On the other hand, the APPY-1 is a reliable test to exclude the diagnosis of AA in patients at low or moderate risk according to PAS and Alvarado Score.





Similar content being viewed by others
Data availability
The data used to carry out this systematic review are available upon request from the review authors.
Change history
05 July 2022
A Correction to this paper has been published: https://doi.org/10.1007/s00068-022-02037-3
References
Becker C, Kharbanda A. Acute appendicitis in pediatric patients: an evidence-based review. Pediatr Emerg Med Pract. 2019;16(9):1–20 (Epub 2019 Sep 2 PMID: 31461613).
Glass CC, Rangel SJ. Overview and diagnosis of acute appendicitis in children. Semin Pediatr Surg. 2016;25(4):198–203. https://doi.org/10.1053/j.sempedsurg.2016.05.001 (Epub 2016 May 10 PMID: 27521708).
Snyder MJ, Guthrie M, Cagle S. Acute appendicitis: efficient diagnosis and management. Am Fam Physician. 2018;98(1):25–33 (PMID: 30215950).
Pedram A, Asadian F, Roshan N. Diagnostic accuracy of abdominal ultrasonography in pediatric acute appendicitis. Bull Emerg Trauma. 2019;7(3):278–83. https://doi.org/10.29252/beat-0703011 (PMID:31392228; PMCID:PMC6681883).
Benabbas R, Hanna M, Shah J, Sinert R. Diagnostic accuracy of history, physical examination, laboratory tests, and point-of-care ultrasound for pediatric acute appendicitis in the emergency department: a systematic review and meta-analysis. Acad Emerg Med. 2017;24(5):523–51. https://doi.org/10.1111/acem.13181 (PMID: 28214369).
Hajibandeh S, Hajibandeh S, Hobbs N, Mansour M. Neutrophil-to-lymphocyte ratio predicts acute appendicitis and distinguishes between complicated and uncomplicated appendicitis: a systematic review and meta-analysis. Am J Surg. 2020;219(1):154–63. https://doi.org/10.1016/j.amjsurg.2019.04.018 (Epub 2019 Apr 27 PMID: 31056211).
Ates U, Bahadir K, Ergun E, Gollu G, Durmaz M, Gunay F, Erguder I, Bingol-Kologlu M, Yagmurlu A, Dindar H, Cakmak M. Determination of pentraxin 3 levels in diagnosis of appendicitis in children. Pediatr Int. 2020;62(5):624–8. https://doi.org/10.1111/ped.14131 (PMID: 31886585).
Ulusoy E, Çitlenbik H, Akgül F, Öztürk A, Şık N, Ulusoy O, Küme T, Yılmaz D, Duman M. Is ischemia-modified albumin a reliable marker in accurate diagnosis of appendicitis in children? World J Surg. 2020;44(4):1309–15. https://doi.org/10.1007/s00268-019-05323-1 (PMID: 31820057).
Yap TL, Fan JD, Ho MF, Choo CSC, Ong LY, Chen Y. Salivary biomarker for acute appendicitis in children: a pilot study. Pediatr Surg Int. 2020;36(5):621–7. https://doi.org/10.1007/s00383-020-04645-9 (Epub 2020 Mar 26 PMID: 32219561).
Shabani F, Farasat A, Mahdavi M, Gheibi N. Calprotectin (S100A8/S100A9): a key protein between inflammation and cancer. Inflamm Res. 2018;67(10):801–12. https://doi.org/10.1007/s00011-018-1173-4 (Epub 2018 Aug 6 PMID: 30083975).
Vaos G, Kostakis ID, Zavras N, Chatzemichael A. The role of calprotectin in pediatric disease. Biomed Res Int. 2013;2013:542363. https://doi.org/10.1155/2013/542363 (Epub 2013 Sep 23. PMID: 24175291; PMCID: PMC3794633).
Kentsis A, Lin YY, Kurek K, Calicchio M, Wang YY, Monigatti F, Campagne F, Lee R, Horwitz B, Steen H, Bachur R. Discovery and validation of urine markers of acute pediatric appendicitis using high-accuracy mass spectrometry. Ann Emerg Med. 2010;55(1):62-70.e4. https://doi.org/10.1016/j.annemergmed.2009.04.020 (Epub 2009 Jun 25. PMID: 19556024; PMCID: PMC4422167).
Kharbanda AB, Rai AJ, Cosme Y, Liu K, Dayan PS. Novel serum and urine markers for pediatric appendicitis. Acad Emerg Med. 2012;19(1):56–62. https://doi.org/10.1111/j.1553-2712.2011.01251.x (Epub 2012 Jan 5. PMID: 22221321; PMCID: PMC3261304).
Huckins DS, Simon HK, Copeland K, Spiro DM, Gogain J, Wandell M. A novel biomarker panel to rule out acute appendicitis in pediatric patients with abdominal pain. Am J Emerg Med. 2013;31(9):1368–75. https://doi.org/10.1016/j.ajem.2013.06.016 (Epub 2013 Jul 26. Erratum in: Am J Emerg Med. 2015 Sep;33(9):1323. PMID: 23891596).
Huckins DS, Simon HK, Copeland K, Milling TJ Jr, Spandorfer PR, Hennes H, Allen C, Gogain J, APAB Study Group. Prospective validation of a biomarker panel to identify pediatric ED patients with abdominal pain who are at low risk for acute appendicitis. Am J Emerg Med. 2016;34(8):1373–82. https://doi.org/10.1016/j.ajem.2016.03.066 (Epub 2016 Apr 5. PMID: 27133536).
Sarsu SB, Erbagci AB, Ulusal H, Karakus SC, Bulbul ÖG. The place of calprotectin, lactoferrin, and high-mobility group box 1 protein on diagnosis of acute appendicitis with children. Indian J Surg. 2017;79(2):131–6. https://doi.org/10.1007/s12262-015-1441-2 (Epub 2016 Jan 14. PMID: 28442839; PMCID: PMC5386938).
Akgül F, Er A, Ulusoy E, Çağlar A, Çitlenbik H, Keskinoğlu P, Şişman AR, Karakuş OZ, Özer E, Duman M, Yilmaz D. Integration of physical examination, old and new biomarkers, and ultrasonography by using neural networks for pediatric appendicitis. Pediatr Emerg Care. 2019. https://doi.org/10.1097/PEC.0000000000001904 (Epub ahead of print. PMID: 31503129).
Del Castillo JG, Ayuso FJ, Trenchs V, de Zarate MMO, Navarro C, Altali K, Fernandez C, Huckins D, Martín-Sánchez FJ, INFURG-SEMES group. Diagnostic accuracy of the APPY1 Test in patients aged 2–20 years with suspected acute appendicitis presenting to emergency departments. Emerg Med J. 2016;33(12):853–9. https://doi.org/10.1136/emermed-2015-205259 (Epub 2016 Sep 9. PMID: 27613754).
Benito J, Acedo Y, Medrano L, Barcena E, Garay RP, Arri EA. Usefulness of new and traditional serum biomarkers in children with suspected appendicitis. Am J Emerg Med. 2016;34(5):871–6. https://doi.org/10.1016/j.ajem.2016.02.011 (Epub 2016 Feb 12 PMID: 26935221).
Benito J, Fernandez S, Gendive M, Santiago P, Perez-Garay R, Arana-Arri E, Mintegi S. A new clinical score to identify children at low risk for appendicitis. Am J Emerg Med. 2020;38(3):554–61. https://doi.org/10.1016/j.ajem.2019.05.050 (Epub 2019 May 28 PMID: 31171439).
Salö M, Roth B, Stenström P, Arnbjörnsson E, Ohlsson B. Urinary biomarkers in pediatric appendicitis. Pediatr Surg Int. 2016;32(8):795–804. https://doi.org/10.1007/s00383-016-3918-x (Epub 2016 Jun 28 PMID: 27351432).
Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;19(14):135. https://doi.org/10.1186/1471-2288-14-135 (PMID:25524443;PMCID:PMC4383202).
Arredondo Montero J, Bardají Pascual C, Bronte Anaut M, López-Andrés N, Antona G, Martín-Calvo N. Diagnostic performance of serum interleukin-6 in pediatric acute appendicitis: a systematic review. World J Pediatr. 2022;18(2):91–9. https://doi.org/10.1007/s12519-021-00488-z (Epub 2022 Jan 3 PMID: 34978051).
Wu HP, Chen CY, Kuo IT, Wu YK, Fu YC. Diagnostic values of a single serum biomarker at different time points compared with Alvarado score and imaging examinations in pediatric appendicitis. J Surg Res. 2012;174(2):272–7. https://doi.org/10.1016/j.jss.2011.01.047 (Epub 2011 Feb 23 PMID: 21529827).
Stankovic N, Surbatovic M, Stanojevic I, Simić R, Djuricic S, Milickovic M, Grujic B, Savic D, Marinovic VM, Stankovic M, Vojvodic D. Possible cytokine biomarkers in pediatric acute appendicitis. Ital J Pediatr. 2019;45(1):125. https://doi.org/10.1186/s13052-019-0726-7 (PMID:31615548;PMCID:PMC6794741).
Whiting PF, Rutjes AW, Westwood ME, Mallett S, Deeks JJ, Reitsma JB, Leeflang MM, Sterne JA, Bossuyt PM, QUADAS-2 Group. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. 2011;155(8):529–36. https://doi.org/10.7326/0003-4819-155-8-201110180-00009 (PMID: 22007046).
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;29(372): n71. https://doi.org/10.1136/bmj.n71 (PMID:33782057;PMCID:PMC8005924).
Acknowledgements
No acknowledgements to report.
Funding
This review did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. None of the authors has external funding to declare.
Author information
Authors and Affiliations
Contributions
JAM: Conceptualization and study design; literature search and selection, data curation and extraction, formal analysis; investigation; methodology; project administration; resources; validation; visualization; writing—original draft; writing—review and editing. CBP: Literature search and selection, data curation and extraction; investigation; writing—original draft. MBA: Literature search and selection, data curation and extraction, formal analysis; investigation; writing—original draft. GA: Literature search and selection, data curation and extraction; investigation; writing—original draft. NMC: Conceptualization and study design; literature search and selection, data curation and extraction, formal analysis; investigation; methodology; project administration; resources; validation; visualization; writing—original draft; writing—review and editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest. No financial or non-financial benefits have been received or will be received from any party related directly or indirectly to the subject of this article.
Ethical approval
This study did not involve the participation of human or animal subjects, and therefore, was exempt from formal assessment by the ethics committee for clinical research of our center.
Additional information
The original online version of this article was revised due to a retrospective Open Access cancellation.
Rights and permissions
About this article
Cite this article
Arredondo Montero, J., Bardají Pascual, C., Antona, G. et al. Diagnostic performance of calprotectin and APPY-1 test in pediatric acute appendicitis: a systematic review and a meta-analysis. Eur J Trauma Emerg Surg 49, 763–773 (2023). https://doi.org/10.1007/s00068-022-02000-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-022-02000-2