Abstract
Purpose
The diagnosis of pediatric appendicitis is still a challenge, resulting in perforation and negative appendectomies. The aim of this study was to evaluate novel biomarkers in urine and to use the most promising biomarkers in conjunction with the Pediatric Appendicitis Score (PAS), to see whether this could improve the accuracy of diagnosing appendicitis.
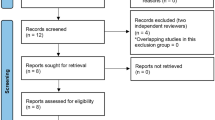
Methods
A prospective study of children with suspected appendicitis was conducted with assessment of PAS, routine blood tests, and measurements of four novel urinary biomarkers: leucine-rich α-2-glycoprotein (LRG), calprotectin, interleukin 6 (IL-6), and substance P. The biomarkers were blindly determined with commercial ELISAs. Urine creatinine was used to adjust for dehydration. The diagnosis of appendicitis was based on histopathological analysis.
Results
Forty-four children with suspected appendicitis were included, of which twenty-two (50 %) had confirmed appendicitis. LRG in urine was elevated in children with appendicitis compared to children without (p < 0.001), and was higher in children with gangrenous and perforated appendicitis compared to those with phlegmonous appendicitis (p = 0.003). No statistical significances between groups were found for calprotectin, IL-6 or substance P. LRG had a receiver operating characteristic area under the curve of 0.86 (95 % CI 0.79–0.99), and a better diagnostic performance than all routine blood tests. LRG in conjunction with PAS showed 95 % sensitivity, 90 % specificity, 91 % positive predictive value, and 95 % negative predictive value.
Conclusion
LRG, adjusted for dehydration, is a promising novel urinary biomarker for appendicitis in children. LRG in combination with PAS has a high diagnostic performance.


Similar content being viewed by others
References
Davies GM, Dasbach EJ, Teutsch S (2004) The burden of appendicitis-related hospitalizations in the United States in 1997. Surg Infect (Larchmt) 5(2):160–165
Buckius MT, McGrath B, Monk J, Grim R, Bell T, Ahuja V (2012) Changing epidemiology of acute appendicitis in the United States: study period 1993–2008. J Surg Res 175(2):185–190
Papandria D, Goldstein SD, Rhee D, Salazar JH, Arlikar J, Gorgy A et al (2013) Risk of perforation increases with delay in recognition and surgery for acute appendicitis. J Surg Res 184(2):723–729
Simpson J, Samaraweera AP, Sara RK, Lobo DN (2008) Acute appendicitis—a benign disease? Ann R Coll Surg Engl 90:313–316
Bundy DG, Byerley JS, Liles EA, Perrin EM, Katznelson J, Rice HE (2007) Does this child have appendicitis? JAMA 298(4):438–451
Bonadio W, Brazg J, Telt N, Pe M, Doss F, Dancy L et al (2015) Impact of in-hospital timing to appendectomy on perforation rates in children with appendicitis. J Emerg Med
Kulik DM, Uleryk EM, Maguire JL (2013) Does this child have appendicitis? A systematic review of clinical prediction rules for children with acute abdominal pain. J Clin Epidemiol 66(1):95–104
Salö M, Friman G, Stenström P, Ohlsson B, Arnbjörnsson E (2014) Appendicitis in children: evaluation of the pediatric appendicitis score in younger and older children. Surg Res Pract. 2014:438076
Doria AS, Moineddin R, Kellenberger CJ, Epelman M, Beyene J, Schuh S et al (2006) US or CT for diagnosis of appendicitis in children and adults? A Meta-Analysis. Radiology 241(1):83–94
Pearce MS, Salotti JA, Little MP, McHugh K, Lee C, Kim KP et al (2012) Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: A retrospective cohort study. Lancet 380(9840):499–505
Grönroos JM (2001) Do normal leucocyte count and C-reactive protein value exclude acute appendicitis in children? Acta Paediatr 90(6):649–651
Vaughan-Shaw PG, Rees JR, Bell E, Hamdan M, Platt T (2011) Normal inflammatory markers in appendicitis: evidence from two independent cohort studies. JRSM Short Rep. 2:43
Wang LT, Prentiss KA, Simon JZ, Doody DP, Ryan DP (2007) The use of white blood cell count and left shift in the diagnosis of appendicitis in children. Pediatr Emerg Care 23(2):69–76
Ilkhanizadeh B, Owji AA, Tavangar SM, Vasei M, Tabei SM (2001) Spot urine 5-hydroxy indole acetic acid and acute appendicitis. Hepatogastroenterology 48:609–613
Mihmanli M, Uysalol M, Coskun H, Demir U, Dilege E, Eroglu T (2004) The value of 5-hydroxyindolacetic acid levels in spot urine in the diagnosis of acute appendicitis. Ulus Travma Acil Cerrahi Derg. 10(3):173–176
Hernandez R, Jain A, Rosiere L, Henderson SO (2008) A prospective clinical trial evaluating urinary 5-hydroxyindoleacetic acid levels in the diagnosis of acute appendicitis. Am J Emerg Med 26(3):282–286
Bolandparvaz S, Vasei M, Owji AA, Ata-Ee N, Amin A, Daneshbod Y et al (2004) Urinary 5-hydroxy indole acetic acid as a test for early diagnosis of acute appendicitis. Clin Biochem 37(11):985–989
Jangjoo A, Varasteh A-R, Mehrabi Bahar M, Tayyebi Meibodi N, Esmaili H, Nazeri N et al (2012) Is urinary 5-hydroxyindoleacetic acid helpful for early diagnosis of acute appendicitis? Am J Emerg Med 30(4):540–544
Ozel SK, Ilhan N, KazezA, Apak SNI (2006) Is urinary 5-HIAA determination a valuable method in diagnosis of acute appendicitis in children? J Indian Assoc Pediatr Surg 11(1):35–8
Kharbanda AB, Rai AJ, Cosme Y, Liu K, Dayan PS (2012) Novel serum and urine markers for pediatric appendicitis. Acad Emerg Med 19(1):56–62
Kentsis A, Ahmed S, Kurek K, Brennan E, Bradwin G, Steen H et al (2012) Detection and Diagnostic Value of Urine Leucine-Rich alpha-2-Glycoprotein in Children With Suspected Acute Appendicitis. Ann Emerg Med 60(1):78–83 e1
Murphy CG, Glickman JN, Tomczak K, Wang YY, Beggs AH, Shannon MW et al (2008) Acute appendicitis is characterized by a uniform and highly selective pattern of inflammatory gene expression. Mucosal Immunol 1(4):297–308
O’Donnell LC, Druhan LJ, Avalos BR (2002) Molecular characterization and expression analysis of leucine-rich alpha2-glycoprotein, a novel marker of granulocytic differentiation. J Leukoc Biol 72:478–485
Kentsis A, Lin YY, Kurek K, Calicchio M, Wang YY, Monigatti F et al (2010) Discovery and validation of urine markers of acute pediatric appendicitis using high-accuracy mass spectrometry. Ann Emerg Med 55(1):62–70.e4
Kharbanda AB, Cosme Y, Liu K, Spitalnik SL, Dayan PS (2011) Discriminative accuracy of novel and traditional biomarkers in children with suspected appendicitis adjusted for duration of abdominal pain. Acad Emerg Med 18(6):567–574
Sack U, Biereder B, Elouahidi T, Bauer K, Keller T, Tröbs R-B (2006) Diagnostic value of blood inflammatory markers for detection of acute appendicitis in children. BMC Surg 6:15
Andersson M, Rubér M, Ekerfelt C, Hallgren HB, Olaison G, Andersson RE (2014) Can new inflammatory markers improve the diagnosis of acute appendicitis? World J Surg 38(11):2777–2783
Ozguner IF, Kizilgun M, Karaman A, Cavusoglu YH, Erdogan D, Karaman I et al (2014) Are neutrophil CD64 expression and interleukin-6 early useful markers for diagnosis of acute appendicitis? Eur J Pediatric Surg 179–83
Di Sebastiano P, Fink T, di Mola FF, Weihe E, Innocenti P, Friess H et al (1999) Neuroimmune appendicitis. Lancet 354(9177):461–466
Emil S, Gaied F, Lo A, Laberge JM, Puligandla P, Shaw K et al (2012) Gangrenous appendicitis in children: a prospective evaluation of definition, bacteriology, histopathology, and outcomes. J Surg Res 177(1):123–126
Peter SDS, Sharp SW, Holcomb GW, Ostlie DJ (2008) An evidence-based definition for perforated appendicitis derived from a prospective randomized trial. J Pediatr Surg 43(12):2242–2245
Samuel M (2002) Pediatric appendicitis score. J Pediatr Surg 37(6):877–881
Goldman RD, Carter S, Stephens D, Antoon R, Mounstephen W, Langer JC (2008) Prospective validation of the pediatric appendicitis score. J Pediatr 153(2):278–282
Buchanan SGSC, Gay NJ (1996) Structural and functional diversity in the leucine-rich repeat family of proteins. Prog Biophys Mol Biol 65(1):1–44
Weivoda S, Andersen JD, Skogen A, Schlievert PM, Fontana D, Schacker T et al (2008) ELISA for human serum leucine-rich alpha-2-glycoprotein-1 employing cytochrome c as the capturing ligand. J Immunol Methods 336:22–29
Acknowledgments
The study was financed by Grants from the Development Foundation of Region Skåne and Magtarmfonden.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Salö, M., Roth, B., Stenström, P. et al. Urinary biomarkers in pediatric appendicitis. Pediatr Surg Int 32, 795–804 (2016). https://doi.org/10.1007/s00383-016-3918-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-016-3918-x