Abstract
Objectives
We carried out a retrospective cohort study to differentiate geriatric odontoid fractures into stable and unstable and correlated it with fracture fusion rates. Results are based on the literature and on our own experience. The authors propose that the simple Anderson and D’Alonzo classification may not be sufficient for geriatric patients.
Methods
There were 89 patients ≥ 65 years who presented at our institution with type II and III odontoid fractures from 2003 until 2017 and were included in this study. Each patient was categorized with CT scans to evaluate the type of fracture, fracture gap (mm), fracture angulation (°), fracture displacement (mm) and direction (ventral, dorsal). Fractures were categorized as stable [SF] or unstable [UF] distinguished by the parameters of its angulation (< / > 11°) and displacement (< / > 5 mm) with a follow-up time of 6 months.
SFs were treated with a semi-rigid immobilization for 6 weeks, UFs surgically—preferably with a C1–C2 posterior fusion.
Results
The classification into SFs and UFs was significant for its angulation (P = 0.0006) and displacement (P < 0.0001). SF group (n = 57): A primary stable union was observed in 35, a stable non-union in 10, and an unstable non-union in 8 patients of which 4 were treated with a C1/2 fixation. The overall consolidation rate was 79%. UF group (n = 32): A posterior C1–C2 fusion was carried out in 23 patients, a C0 onto C4 stabilization in 7 and an anterior odontoid screw fixation in 2. The union rate was 100%. Twenty-one type II SFs (91%) consolidated with a nonoperative management (P < 0.001). A primary non-union occurred more often in type II than in type III fractures (P = 0.0023). There was no significant difference in the 30-day overall case fatality (P = 0.3786).
Conclusion
To separate dens fractures into SFs and UFs is feasible. For SFs, semi-rigid immobilization provides a high consolidation rate. Stable non-unions are acceptable, and the authors suggest a posterior transarticular C1–C2 fixation as the preferred surgical treatment for UFs.
Level of evidence
Level III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Odontoid fractures account for approximately 20% of the entity of cervical spine fractures in the adult population [3, 4]. However, they are the single most common observed cervical spine fracture in geriatric patients (≥ 65 years) [1, 2, 5, 6] and follow a bimodal population distribution with peaks in the early adulthood (high-energy trauma) and in the elderly (low-energy, minor trauma) [7, 8].
The so far established treatment protocols for odontoid fractures in the geriatric population remain controversial. A mortality rate of 26–47% has been reported for nonoperatively treated patients mainly due to respiratory-related complications from immobilization [9, 10].
In the literature, the reported rate of non-union for all treatment modalities varies greatly (2.4–82%) [10,11,12,13,14,15,16] and may be accounted for by various factors such as mechanism of injury, fracture type, direction of displacement, magnitude of angulation, blood-supply, osteoporosis, patients age, etc. [10, 12, 16,17,18,19,20]. Some authors consider a stable non-union as an acceptable outcome for the elderly [18, 50].
Surgical interventions, such as anterior odontoid screw fixation or posterior atlantoaxial arthrodesis are associated with significant complications in the elderly and are controversially discussed in the literature [21].
Harrop et al. and Yuan et al. state that anterior screw fixation in type II fractures is warranted in geriatric patients, as it offers the preservation of the C1–C2 rotatory motion and is less invasive [9, 22]. However, there are several reports on a high number of adverse events in the geriatric population and this operative procedure is more appropriate for younger patients [11, 12, 23, 24].
In contrast, posterior C1–C2 fixation reduces the rotatory motion but offers a high success rate with a bony union in the elderly with a low number of post-operative complications [21, 25,26,27].
In this observational, retrospective cohort study, we postulate that odontoid fractures in elderly patients can be differentiated into stable fractures (SFs) and unstable fractures (UFs) according to fracture angulation, displacement, and gap. The proposed fracture classification by Anderson and D’ Alonzo or its modifications are not suitable for type II fractures in the elderly due to high operative complication rates. Hence, a suitable alternative, as outlined in this study, represents the division of geriatric odontoid fracture into SFs and UFs, leading to safe outcomes. For this purpose, we analyzed non-operatively treated SFs and operatively treated UFs of the odontoid in the elderly and compared the two of them.
Materials and methods
Study design
This is a retrospective study of clinical and radiological outcomes in a cohort of geriatric patients (≥ 65 years) with acute type II and III odontoid fractures (< 21 days since accident) managed operatively and non-operatively.
Extracted data after management included: fracture type, -angulation, -displacement, -gap, number and severity of initial neurological deficits, age, initial treatment modality, fracture healing, mortality, associated injuries, and sex.
Study population
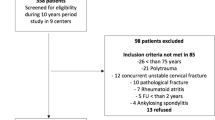
Medical records and CT scans of the cervical spine of 211 consecutive patients with odontoid fractures were analyzed who presented at our Level I tertiary-care center between May 2003 and December 2017.
Seventy-four patients were excluded because they were under 65 years old, presented with missing/incomplete radiologic/clinical data, had suffered a polytrauma (ISS > 16) [28], showed anatomical/congenital abnormalities of the C1/2 region, suffered from metastatic/rheumatoid disease, or fractures were of unknown age.
The remaining 137 patients were included aged 65 years or older and sustained a type II (74) or III (63) odontoid fracture (International Classification of Diseases, Ninth Revision, code 805.02) (Fig. 1).
Radiological fracture evaluation
Fracture evaluation was solely based on CT scans (Aquilion One; Toshiba, Canon Medical Systems, Vienna, Austria and Dual Source Somatom; Siemens, Munich, Germany) and classified according to Anderson and D’Alonzo [14]. Obtained measurements included fracture angulation (degrees), displacement (mm), and gap (mm) as well as a treatment modality.
Encountered odontoid fractures were differentiated into SFs and UFs, according to previously published clinical cutoff points [19, 20, 29, 30]. SFs displayed an initial ventral or dorsal displacement of < 5 mm and an angulation of < 11°. All other fractures were classified as UFs. The obtained measurements for the gap (mm) have been neglected as overall 63 fractures (71%; 45 SFs, 18 UFs) displayed a gap of 0.00 mm (Fig. 2).
Measurements were performed using the hospital’s web-based picture archiving and communication system, which is integrated into the medical record system, IMPAX EE (Agfa Health Care, Bonn, Germany). An additional MRI examination was carried out on 8 patients with neurological deficits either upon arrival or within 12 h after symptoms occurred.
Treatment protocol based on stable and unstable radiologic fracture evaluation
SFs were treated with a semi-rigid immobilization, Vista collar (Vista Orthese Aspen Medical Products, Griesheim, Germany) or Philadelphia collar (Philadelphia Cervical Collar Company, Thorofare, New Jersey, USA) for a minimum of 6 weeks.
UFs were treated operatively. The same three surgeons, with consistent surgical approaches, performed all procedures: An altered posterior transarticular C1–C2 fixation [12, 31] according to Magerl and Seemann [43, 44].
If anatomic landmarks prohibited a posterior C1–C2 arthrodesis due to extensive cystic lesions a C0 onto C4 stabilization was done.
An anterior odontoid screw fixation was performed if prone positioning was not possible due to concomitant spinal injuries. (Appendix 1).
Clinical and radiological follow-up
Follow-up monitoring was done in all patients (SFs and UFs) at the time of hospital discharge or suture removal, as well as at 6, 12- and 24 weeks post-treatment initiation.
Routine assessments consisted of clinical and radiographic evaluation (antero-posterior, lateral, open-mouth view, and if possible dynamic X-ray evaluation).
Successful fracture consolidation was defined as signs of osseous trabeculae crossing the fracture site in the absence of sclerotic margins along the fracture line with no change in neurology. Two individual and independent surgeons observed the X-rays at the given post-trauma intervals to state whether osseous trabeculae crossing at the fracture site was present. If conventional X-ray was not conclusive and fracture consolidation or stability could not be determined, or the patient complained about ongoing pain, an additional CT scan was carried out (62%) in the SF group. All patients in the UF group have been evaluated with a CT scan post-surgery to check upon fracture reduction and implant positioning to ensure adequate fracture healing.
Statistical analysis
Collected data are expressed as mean ± standard deviation. Frequency distributions and summary statistics were calculated for demographics and fracture types. For categorical variables, cross-tabulations were generated, and Fisher exact tests were used to compare distributions. Difference in survival between the SFs and UFs were modeled using the Cox proportional hazard model including adjustments for age and sex. A 30 day Kaplan–Meier survival plot was created for mortality comparison between SFs and UFs. The level of statistical significance was set at P < 0.050. Statistical analysis was conducted using GraphPad Prism 9.0.0 (San Diego, CA, USA).
Results
Patients characteristics
This study included 137 patients aged 65 years or older (60 male, mean age 80 ± 8 years; range 66–94 years). Of these, 34 patients (24.8%; 26 SFs, 8 UFs) were transferred to Level II/III trauma centers within the first 30 days or lost during follow-up and hence, excluded. Patients were transferred to a different hospital after initiating treatment due to closer proximity to their hometown. Within 30 days of initial treatment, 14 patients died (10.2%, 7 SFs; 7 UFs).
In the remaining 89 patients, there was no significant difference in the proportion of male versus female (P = 0.499) (Table 1).
A significant difference between the 2 groups, SFs and UFs according to fracture angulation (P = 0.001) and displacement (P < 0.0001) could be observed as depicted in Fig. 3. The average follow-up time of the remaining 89 patients, 57 SFs and 32 UFs, was 6.9 ± 12.3 and 6.9 ± 10.7 months, respectively.
Radiographic outcome: SFs
As depicted in Fig. 4, 57 SFs (23 type II, 34 type III) were identified after 6 months and divided into subgroups: stable union (SU), stable non-union (SNU) and unstable non-union (UNU). Union was defined as bony consolidation of the fracture and stability was determined by the absence of a secondary displacement (< 2 mm). UNU was characterized by the absence of osseous bony union and a secondary odontoid displacement (> 2 mm).
A SU was observed in 39 patients (12 type II, 27 type III). A primary SU occurred in 35 patients (11 type II, 24 type III) and a secondary-SU with consolidation after secondary dislocation in 4 patients (2 type II, 2 type III) after 6 months.
A Stable Non-Union (SNU) was observed in 10 patients (7 type II, 3 type III).
An Unstable Non-Union (UNU) occurred in 8 patients of which 4 could not undergo surgery due to comorbidities or they did not wish to be operated. The other 4 fractures were secondarily stabilized with a C1–C2 posterior fixation (2 type II, 2 type III) proceeding to bony fusion.
Overall, 79% of encountered SFs fully consolidated (P < 0.0001).
Radiographic outcome: UFs
Radiographic evaluation showed bony union at the site of posterior C1–C2 Arthrodesis in all patients that initially presented with UFs (15 type II, 8 type III fractures) [12, 31]. This included one patient (4%) with screw malpositioning that had to be surgically revised and the osseous union was attained within three months. A single screw breakage was observed in 3 patients, but all achieved full consolidation with no neurological deficits, and none needed revision.
Due to extensive cystic lesions in the odontoid, a C0 onto C4 Stabilization was used to stabilize the fracture (4 type II, 3 type III) and all consolidated.
Due to a concomitant luxated C6-C7 fracture with simultaneous ventral plate stabilization in one patient and a traumatic brain injury in the other, an Anterior Odontoid Screw Fixation (1 type II, 1 type III) was the surgical method of choice.
The overall consolidation rate of all UFs was 100% (Fig. 5).
Type II fractures: SFs versus UFs
A total of 43 type II fractures (23 SF, 20 UF) were analyzed in this cohort. In the SF group, 23 type II fractures were treated nonoperatively and resulted in either a primary non-union (SNU n = 7, UNU n = 4) or a SU (n = 12). In the UF group, 20 type II fractures were treated operatively leading to a stable union (100%). Ninteen out of the twenty-three type II fractures (83%) in the SF group healed as a SU or SNU with non-operative management compared to type II fracturs in the UF group. This is significant (P < 0.001) and indicates that not all type II fractures need to be operated on and to be considered as stable or to reach bony union. Figure 6 depicts that there is a significant difference (P = 0.0115) in angulation (mean SF: 12.87° ± 15.45; mean UF: 20.50° ± 15.19) compared to its theoretical mean cutoff point of 11 degrees between type II SFs and UFs. The significance of type II fractures between both groups also applies to its dislocation (mean SF: 1.04 mm ± 1.80; mean UF: 6.28 mm ± 4.08; P < 0.0001) compared to its theoretical mean cutoff point of 5 mm.
Case fatality rate over 30 days
Patients who died within 30 days after diagnosis were not included in the summarized statistic above and evaluated separately. Overall, 14 patients died (17 SFs, 7 UFs).
In the SF group (5 type II, 2 type III), 6 died shortly after the initial injury due to cardiac arrest and/or respiratory insufficiency. One patient deceased within 3 weeks due to multi-organ failure.
Of the 7 patients in the UF group (4 type II, 3 type III), 6 died due to cardiorespiratory insufficiency and one patient due to multiorgan failure. All deceased patients were treated with a posterior transarticular C1–C2 fixation. One of these patients presented initially with tetraplegia.
The overall case fatality rate (CFR) does not reflect a significant difference between SFs and UFs (P = 0.3786), between males (n = 7) and females (n = 7) (P > 0.9999) or type II (n = 9) and III fractures (n = 5) (P = 0.3896). The hazard ratio of death within the first 30 days of presentation in the SF group compared to patients in the UF group was 1.47 (95% CI = 0.44–4.87).
The Effect of neurological deficits on the CFR
Initial neurological deficits were observed in 14 patients (Table 2) and 5 deceased within 30 days. All deceased patients were quadriplegic (2 SFs with nonoperative treatment due to cardiac resuscitation and respiratory insufficiency, 3 UFs with C1/2 fixation).
A dorsal fracture dislocation was observed in 9 patients (P = 0.5055). Four out of the five patients who died suffered from a dorsal dislocation as well (P = 0.4000). An MRI examination was carried out in patients whose vital functions permitted the investigation.
Discussion
The available literature reports on different treatment modalities for type II and III odontoid fractures in the elderly but lacks specific guidelines for its application.
Observed radiographic parameters (angulation, displacement) are important to decide whether an operative treatment is warranted and are predictive of treatment outcomes [28, 45]. Karamian et al. demonstrated that the obtained measurements via CT scans, as used in our study, are reliable [46]. The classification of odontoid fractures into SFs and UFs based on CT scan measurements was constituted on previously mentioned cut-off points [19, 20, 29, 30] and were significant in the measurements obtained in our study. According to our calculation and further stratification, to classify odontoid fractures not based on the previously published guidelines of Anderson and D’ Alonzo, but rather into SFs and UFs is justifiable.
Semi-rigid immobilization with a cervical collar is biomechanically superior to the halo orthoses with a significantly lower device-associated complications [18, 19, 29, 31] and was used as the treatment of choice. Overall, 35 patients (61%) in the SF group advanced to a SU which is within the range reported by others [48]. A SNU was seen in 10 patients (18%), with no observed neurological deficits and no instability at the fracture site (dynamic X-ray evaluation) [18, 32,33,34]. According to our results, we agree that stable fibrous union is an acceptable outcome in geriatric odontoid fractures [49]. The evaluation of fracture union is one of the most important and fundamental clinical determinations made in orthopedics. If the observed X-rays showed signs of fracture consolidation, an additional CT scan evaluation was omitted in the SF group. If there were any signs of non-union or pain, a CT scan was carried out to evaluate fracture fusion rates. In summary, 79% presented with a stable fracture and we concur with many authors that fracture stability is the main goal to pursue with or without proper osseous union [12, 18, 32, 49].
Posterior transarticular C1–C2 fixation resulted in 100% bony union (n = 23). It was our primary choice of treatment in the UF group [34], and the observed rate of consolidation is concurrent with published literature results [27, 35]. The difficulty in placing screws has been reported previously in up to 26% of patients [36]. In our case study, obstacles were observed due to an excessive thoracic kyphosis or a high-riding vertebral artery, as well as destructive cystic lesions [29, 38]. Several authors reported decreased functional results with a considerable impairment in cervical spine motion as well as chronic pain symptoms [36,37,38].
In contrast to a posterior arthrodesis, direct anterior screw fixation of the dens preserves the C1–C2 rotation [23]. Based on our own experience and on published reports, it is the preferred treatment in patients younger than 65 years of age [11] with a type II fracture, no osteoporosis, and with a horizontal or an anterior–posterior declining fracture line [12, 24, 30, 34].
Smith et al. reviewed trends in the surgical management of type II fractures over 20 years in their institution and noted posterior methods for fracture stabilization were used much more than anterior odontoid screw fixation [39]. The latter was associated with significantly higher rates of postoperative pneumonia, swallowing dysfunction, and increased technical problems [7, 24, 30, 39, 40]. Osti et al. analyzed failure after anterior screw fixation in geriatric patients and found a significant association between both failure-to-heal and age, as well as failure-to-heal and severity of degenerative changes, such as cystic lesions in the odontoid [41].
According to our radiological UF results, posterior atlantoaxial screw fixation is a good alternative in geriatric patients due to a significantly higher rate of bony union. We further propose that an anterior screw fixation should only be carried out in geriatric patients when a C1–C2 fusion is not suitable such as in patients with traumatic brain injury when supine positioning is not achievable or concomitant surgical approaches have to be carried out.
On the one hand, Anderson and D’Alonzo referred to surgical fracture stabilization of all type II fractures. Based on our observed results by delineating fractures into stable and unstable, not all type II fractures have to undergo surgery to achieve consolidation. Out of 23 nonoperatively treated type II fractures, 21 attained a primary healing or a stable pseudoarthrosis with no neurological dysfunction (P < 0.001). Only one patient (4%) developed delayed-onset myelopathy 5 days after injury and had to be managed operatively which is not a well-established risk factor in the literature [14, 18, 34, 35].
On the other, our results are concurrent with Anderson and D’Alonzo that non-operatively treated type II fractures produce a primary non-union more often than type III odontoid fractures (9 type II, 4 type III) [14]. Hence in the SF group, a SU or SNU in geriatric type II odontoid fractures are an acceptable outcome.
The 30-day case fatality rate showed a hazard ratio of 1.47, indicating a slightly higher rate of survival among patients that were treated nonoperatively (95% [confidence interval] CI = 0.44–4.87, P = 0.4064), but was not significant as described by other authors [47]. The highest rate of fatality in patients with neurological deficiencies could be observed in geriatric patients with quadriplegia below C2. There was no significant difference in survival in patients with neurological deficits that were operated (HR = 0.08; CI = 0.00–1.82; P = 11.38).
In our study, neurological deficits were documented in 14 patients of whom 9 patients presented with a dorsal fracture dislocation (64%). These results compare to the findings of Ryan and Taylor [42] and Mueller et al. [12] indicating that a higher incidence of concomitant spinal cord injury is found in patients that are older than seventy years with a dorsal fracture dislocation. Even though there seems to be enough space in the spinal cord canal, the cord is at greater risk with dorsal fracture dislocation [12].
This retrospective, non-randomized study is not without limitations. Only analyzed data collected from documented electronic records and a median follow-up time of 6 months. It was not possible to obtain a functional dislocation measurement in mm for the entire cohort (lateral flexion–extension radiographs), and therefore the data could not be included. There was no control group, the degree of osteoporosis was not determined, and this study was conducted at a single designated trauma center without randomization.
In the geriatric population, patient’s health considerations, such as osteoporosis/altered bone mineral density and cardiopulmonary comorbidities play an additional role in deciding upon the accurate treatment modality [12] and should be incorporated before an operative procedure is carried out.
Conclusion
To differentiate odontoid fractures into SFs and UFs is feasible and showed valuable results. The authors suggest that type II fractures can be treated nonoperatively with a semi-rigid immobilization if they are classified as SFs. If a fracture classifies as an UF, operative treatment is warranted, and we suggest using a posterior C1–C2 fixation in geriatric patients as it showed a 100% fusion rate. There is no necessity for all type II fractures to be operatively stabilized if the fractures are delineated correctly into SFs and UFs. Overall, a SNU is acceptable in the geriatric population.
References
Korres DS. Fractures of the odontoid process. In: Korres DS, editor. The axis vertebra. Rome: Springer; 2013. p. 45–9.
Ryan MD, Henderson JJ. The epidemiology of fractures and fracture-dislocation of the cervical spine. Injury. 2002;23:38–40.
Gauer JN, Shafi B, Hilibrand AS, Harrop J, Kwon BK, Beiner JM, Albert TJ, Fehlings MG, Vaccaro AR. Proposal of a modified, treatment-oriented classification of odontoid fractures. Spine J. 2005;5:123–9.
Korres DS, Macrogenis AF, Gratsias P, Posantzis MJ, Giannakopoulos EA, Efstathopoulos NE. Type D fractures of the odontoid process. ArgoSpine News J. 2011;23(3):125–8.
Elgafy H, Dvorak MF, Vaccaro AR, Ebraheim N. Treatment of displaced type II odontoid fractures in the elderly patients. Am J Ortohop (Belle Mead NJ). 2009;28(8):410–6.
White AP, Hashimoto R, Norvell DC, Vaccaro AR. Morbidity and mortality related to odontoid fracture surgery in the elderly population. Spine. 2010;35(9):146–57.
Clark CR, White AA. Fractures of the dens. A multicenter study. J Bone Joint Surg Am. 1985;67(9):1340–8.
Ochoa G. Surgical management of odontoid fractures. Injury. 2005;36(Suppl 2):54–64.
Harrop JS, Przybylski GJ, Vaccaro AR. Efficacy of anterior odontoid screw fixation in elderly patients with Type II odontoid fractures. Neurosurg Focus. 2000;8: e6.
Hanigan WC, Powell FC, Elwood PW, Henderson JP. Odontoid fractures in elderly patients. J Neurosurg. 1993;78(1):32–5.
Aebi M, Etter C, Coscia M. Fractures of the odontoid process. Treat anterior screw fixat Spine. 1989;14(10):1065–70.
Mueller EJ, Wick M, Russe O, Muhr G. Management of odontoid fractures in the elderly. Eur Spine J. 1999;8:360–5.
Chiba K, Fujimura Y, Toyama Y, Takahata T, Nakanishi T, Hirabayashi K. Anterior screw fixation for odontoid fracture: clinical results in 45 cases. Eur Spine J. 1993;2:76–81.
Anderson LD, D’Alonzo RT. Fractures of the odontoid process of the axis. J Bone Joint Surg Am. 1974;56:1663–74.
Pointillart V, Lopez Orta A, Freitas J, Vital JM, Senegas J. Odontoid fractures. Eur Spine J. 1994;3:282–5.
Amling M, Wening VJ, Posl M, Grote JH, Hahn M, Delling G. Die Struktur des Axis-Schluessel zur Struktur der Densfraktur. Chirurgie. 1994;65:964–9 (Germany).
Schatzker J, Rorabeck CH, Waddell JP. Fractures of the dens (odontoid process): an analysis of thirty-seven cases. J Bone Joint Surg Br. 1971;53:392–405.
Mueller EJ, Schwinnen I, Fischer K, Wick M, Muhr G. Non-rigid immobilization of odontoid fractures. Eur Spine J. 2003;12(5):522–5.
Apuzzo ML, Heiden JS, Weiss MH, Ackerson TT, Harvey JP, Kurze T. Acute fractures of the odontoid process. An analysis of 45 cases. J Neurorurg. 1978;48(1):85–91.
Konieczny MR, Gstrein A, Mueller EJ. Treatment algorithm for dens fractures: Rigid immobilization, anterior screw fixation, or posterior transarticular C1–C2 fixtation. J Bone Joint Surg Am. 2012;94: e144.
Shousha M, Alhashash M, Allouch H, Boehm H. Surgical treatment of type II odontoid fractures in elderly patients: a comparison of anteriorodontoid screw fixation and posterior atlantoaxial fusion using the Magerl-Gallie technique. Eur Spine J. 2019. https://doi.org/10.1007/s00586-019-05946-x.
Yuan S, Wei B, Tian Y, Yan J, Xu W, Wang L, Liu X. The comparison of clinical outcome of fresh type II odontoid fracture treatment between anteriorcannulated screws fixation and posterior instrumentation of C1–2 without fusion: a retrospective cohort study. J Orthop Surg Res. 2018;13(1):3.
Apfelbaum RI, Lonser RR, Veres R, Casey A. Direct anterior screw fixation for recent and remote odontoid fractures. J Neurosurg. 2000;93(2):227–36.
Andersson S, Rodrigues M, Olerud C. Odontoid fractures: high complication rate associated with anterior screw fixation in the elderly. Eur Spine J. 2000;9(1):56–9.
Magerl F, Seemann PS. Stable posterior fusion of the atlas and axis by transarticular screw fixation. Cervical spine. 1987;1:322–7.
Jeanneret B, Magerl F. Primary posterior fusion C1/2 in odontoid fractures: indications, technique, and results of transarticular screw fixation. J Spinal Disord. 1992;5(4):464–75.
Kaminski A, Gstrein A, Muhr G, Mueller EJ. Transarticular C1–C2 screw fixation: results of unstable odontoid fractures and peuseoarthrosis in the elderly. Unfallchirurg. 2008;111(3):167–72 (Germany).
Baker SP, O’Neil B, Haddon W Jr, Long WB. The injury severity score: a method for describing patients with multiple injuries and evaluating emergency care. J Trauma. 1974;14(3):187–96.
Hadley MN, Dickman CA, Browner CM, Sonntag VK. Acute axis fractures: a review of 229 cases. J Neurosurg. 1992;23(1):38–40.
Seybold EA, Bayley JC. Functional outcome of surgically and conservatively managed dens fractures. Spine (Phila Pa 1976). 1998;23(17):1837–45.
Patel A, Zakaria R, Al-Mahfoudh R, Clark S, Barrett C, Sarsam Z, Pillay R, Drummond T, Wilby PG. Conservative management of type II and III odontoid fractures in the elderly at a regional spine centre: a prospective and retrospective cohort study. Br J Neurosurg. 2015;29(2):249–53.
Hart R, Saterbak A, Rapp T, Clark C. Nonoperative management of dens fracture nonunion in elderly patients without myelopathy. Spine. 2000;25(11):1339–43.
Platzer P, Thalhammer G, Sarahrudi K, Kovar F, Veksyler G, et al. Nonoperative management of odontoid fractures using a halothoracic brace. Neurosurgery. 2007;61(3):522–30.
Pal D, Sell P, Grevitt M. Type II odontoid fractures in the elderly: an evidence-based narrative review of management. Eur Spine J. 2011;20:195–204.
Crockard A, Heilman A, Stevens J. Progressive myelopathy secondary to odontoid fractures: clinical, radiographic and surgical features. Neurosurgery. 1995;78:579–86.
Berlemann U, Schwarzenbach O. Dens fractures in the elderly. Results of anterior scew fixation in 19 elderly patients. Acta Orthop Scand. 1997;68:319–24.
Fielding JW, Hawkins RJ, Ratzan SA. Spine fusion for altlanto-axial instability. J Bone Joint Surg Am. 1976;58:400–7.
Platzer P, Thalhammer G, Oberleitner G, Schuster R, Vecsei V. Gaebler C Surgical treatment of dens fractures in elderly patients. J Bone Joint Surg Am. 2007;89:1716–22.
Smith HE, Vaccaro AR, Maltenfort M, Albert TJ, Hilibrand AS, et al. Trends in surgical management of type II odontoid fractures: 20 years of experience at a regional spinal cord injury center. J Bone Joint Surg Br. 2008;80:452–5.
Marciano RD, Seaman B, Sharma S, Wood T, Karas C. Narayan K Incidence of dysphagia after odontoid screw fixation of type II odontoid fracture in the eldery. Surg Neurol Int. 2018;9:84.
Osti M, Philipp H, Meusburger B. Benedetto KP Analysis of failure following anterior screw fixation of type II odontoid fractures in geriatric patients. Eur Spine J. 2011;20(11):1915–20.
Ryan MD, Taylor TKF. Odontoid fractures in the elderly. J Spinal Disord. 1993;6:397–401.
Gallie WE. Fracturs and dislocations of the cervical spine. The American Jourcal of Surgery. 1939;46(3):495–9.
Magerl FSCS, Seemann PS. Stable posterior fusion of the atlas and axis by transarticular screw fixation. In: Pierre K, Andreas W, editors. Cervical spine I. Vienna: Springer; 1986. p. 322–7.
Greene KA, Dickman CA, Marciano FF, Drabier JB, Hadley MN, Sonntak VK. Acute axis fractures. Analysis of management and outcome in 340 consecutive cases. Spine. 1997;22:1843–52.
Karamian BA, Liu N, Ajiboye RM, Cheng I, Hu SS, Wood KB. Reliability of radiological measurements of type 2 odontoid fractures. Spine J. 2019. https://doi.org/10.1016/j.spinee.2019.04.020.
Butler JS, Dolan RT, Burbridge M, Hurson CJ, O’Byrne JM, McCormack D, Synnott K, Poynton AR. The long-term functional outcome of type II odntoid fractures managed non-operatively. Eur Spine J. 2010;19:1635–42.
Molinari RW, Khera OA, Gruhn WL, McAssey RW. Rigid cervical collar treatment for geriatric type II odontoid fractures. Eur Spine J. 2012;21:855–62.
Joestl J, Lang NW, Tiefenboeck TM, Hajdu S, Platzer P. Management and outcome of dens fractures nonunions in geriatric patients. J Bone Joint Surg AM. 2016;98:193–8.
Blauth Blauth M, Richter M, Kiesewetter B, Lange U. Operative oder konservative behandlung der pseudarthrose des Dens axis Wie gefährlich ist es, eine Denspseudarthrose nicht zu stabilisieren? Chirurg. 1999;70(11):1225–38.
Frankel HL, Hancock DO, Hyslop G, et al. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. Paraplegia. 1969;7:179–92.
Funding
Open access funding provided by Paracelsus Medical University. There was no external source of funding for this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no Conflict of intererst.
Ethical approval
Approved by the Austrian Ethics Committee, S2021-09.
Appendix 1: Concomitant spinal injuries
Appendix 1: Concomitant spinal injuries
Age | Concomitant injuries of the cervical spine |
|---|---|
83 | Atlas arch fracture |
72 | C2 pedicle fracture |
78 | C2 pedicle fracture |
85 | Atlas arch fracture |
87 | Osteolysis |
90 | Atlas arch fracture |
72 | Atlas arch fracture |
91 | Jefferson fracture |
65 | Atlas arch fracture |
67 | Articular process abruption C2 |
80 | Atlas arch fracture |
76 | C2-abruption proc. Spinosus |
82 | Atlas arch fracture |
81 | C2-abruption proc. Spinosus |
82 | C4-right arch fracture |
71 | Atlas arch fracture |
72 | Atlas arch fracture |
92 | Atlas arch fracture |
88 | Atlas arch fracture |
91 | Atlas arch fracture |
79 | C2-abruption proc. Spinosus |
84 | Atlas arch fracture |
88 | Atlas arch fracture |
92 | C2 pedicle fracture |
70 | Cystic lesion |
74 | Cystic lesion |
72 | C2 pedicle fracture |
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Deluca, A., Wichlas, F., Deininger, C. et al. Reevaluation of a classification system: stable and unstable odontoid fractures in geriatric patients—a radiological outcome measurement. Eur J Trauma Emerg Surg 48, 2967–2976 (2022). https://doi.org/10.1007/s00068-022-01985-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-022-01985-0