Abstract
Purpose
Reduction and fixation of tibial plateau fractures associated with small, “floating” intra-articular fragments proposes a challenge. We use fully threaded headless compression screws for (interfragmentary) fixation of such fragments before final plate fixation when standard fixation of intra-articular fragments with k-wires or lag screws is deemed insufficient. Our aim is to describe our technique and clinical experience of this two-level fixation.
Methods
Between 2006 and 2021, 29 patients with a comminuted tibial plateau fracture were treated with this two-level fixation in this retrospective case series. Clinical baseline and surgical variables were collected for all patients. Clinical outcome variables were available for 28 patients with a median follow-up of 16.5 months (IQR 5–24). Functional outcomes were measured with the Knee Injury and Osteoarthritis Outcome Score (KOOS) and reported by 22 patients at a median of 5.2 years (IQR 3.5–9.8).
Results
Reduction was anatomic or good in 82% of cases, fair in 14%, and a malreduction in 4%. Arthrosis was graded as grade 0 in 25% of cases, 1 in 39%, 2 in 21%, and 3 in 14%. Flexion was 110 degrees (IQR 100–130). Five patients had an extension deficit of 5 to 10 degrees. Median KOOS for symptoms and stiffness was 69 points (IQR 45–78), for pain 71 (IQR 45–88), for ADL 85 (IQR 52–95), for sports 30 (IQR 11–55), and for quality of life 34 (IQR 19–56).
Conclusion
The use of fully threaded headless compression screws is a simple and helpful addition in the treatment of comminuted tibial plateau fractures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Fractures of the tibial plateau range from a simple non-displaced split to a severely comminuted fracture involving both medial and lateral plateau [1]. Treatment most often consists of open reduction and internal fixation (ORIF), during which the plateau is reconstructed using a step-by-step approach [2, 3]. These steps include a surgical approach that allows for elevation and repositioning of (impacted) fragments and temporary fixation with k-wires that are replaced with definitive osteo-synthesis using screws and plate(s). Metaphyseal defects are often filled with bone graft (substitutes) [3]. This strategy of anatomic reduction and stable fixation using a soft tissue preserving technique that allows early motion remains the cornerstone of treatment. However, there have been some advances in this area: (1) introduction of the three-column concept may allow better pre-op planning [4]; (2) new posterior-based surgical approaches allow for better access [3, 5]; and (3) plates are nowadays smaller and anatomic [6], and allow for a rafting technique giving better support of the subchondral bone.
Despite these advances, reduction and fixation of multiple “floating” small intra-articular fragments can still propose a challenge. If they are not fixated into a stable construct, they will likely displace in the early post-operative period. Reconstruction of these multiple small fragments into one large fragment on the side table or fixation of a small fragment against a “standing” part of the tibial plateau can be helpful in obtaining the perfect reduction. As these fragments may not have a cortical border, the use of standard lag screws can be insufficient. Giannoudis et al. used a “two-level” reconstruction technique to treat comminuted and displaced posterior wall fractures of the acetabulum and achieved good results [7]. They used 1.5 or 2 mm fully threaded cortical mini-screws to maintain anatomic reduction of osteochondral fragments and then reduced and fixated the overlying posterior wall fragment with 3.5 mm lag screws and a buttress plate. Triggered by their idea, we started using fully threaded headless cannulated compression screws (HCS) for fixation of intra-articular fragments in tibial plateau fractures.
The primary aim of the present report is to describe our technique and clinical experience of using HCS for (interfragmentary) fixation of intra-articular fragments in tibial plateau fractures.
Materials and methods
Between July 2002 and February 2021, 210 tibial plateau fractures were operated on by the senior author in our level 1 Trauma Center. In this group, we identified all patients that were treated with osteo-synthesis including at least one HCS using a prospectively maintained surgical logbook. After ethical approval was waived by the local Medical Ethics Review Committee (W21_182 # 21.197), we retrospectively reviewed the electronic medical records to check radiographs and operative notes to confirm the implantation of the HCS. The study was carried out in accordance with the World Medical Association Declaration of Helsinki. A total of 29 patients were identified and included in this series; the first was operated in 2006 and the last in February 2021.
Clinical baseline and surgical variables were collected for all patients from the electronic medical records. Clinical outcomes were available for 28/29 (97%) of patients. For one patient, clinical outcomes were not available due to foreign residency. The median clinical follow-up duration was 16.5 months (IQR 5–24) after surgery.
In addition, all patients were invited by phone to complete an electronic questionnaire on functional outcome measures and report on total knee arthroplasty (TKA). One patient had passed away and one patient could not participate due to medical reasons. Of the remaining patients, 22/26 (85%) responded at an average of 5.2 years (IQR 3.5–9.8) after surgery. The non-respondents could not be reached using the contact information that was available to us.
Operative technique
All patients received a pre-operative CT scan. The surgical approach was determined by the fracture pattern. In 14/29 cases, a single-incision approach was used: either anterolateral (n = 11), medial (n = 2), or posterior (n = 1). In 15/29 cases, a 2-incision approach was used: anterolateral/posteromedial (n = 8), anterolateral/posterior (n = 1), or anterolateral/medial (n = 6). Three patients were treated in a staged fashion with a posterior approach, followed by an anterolateral approach a few days later because of swelling. For the lateral plateau, the knee joint was routinely spanned with a large AO femoral distractor for improved visualization. A sub-meniscal arthrotomy was performed for access to the lateral plateau. An osteotomy of the fibular head was added if extensile exposure was necessary (n = 2). In bicondylar fractures, the medial plateau was reduced first. For the lateral plateau, the anterolateral fragment was rotated externally, providing access to the metaphyseal impaction. Fragments were reduced and temporarily stabilized with k-wires and clamps under direct vision and fluoroscopic control.
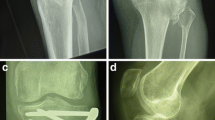
When multiple, adjacent intra-articular fragments were present that could not be sufficiently reduced with the use of lag screws (due to the absence of a cortical border), k-wires (due to insufficient compression), or that needed support complementary to the rafting screw construct (due to an inadequate purchase of bone stock of the fragment), inter-fragmentary fixation was performed using one or more (maximum 3) 20–30 mm HCS (Acutrak 2 mini screw; Acumed, Herzele, Belgium). Fragments were either extracted from the fracture site and then fixated on a side table under compression and direct visual control or fixated while maintained at the fracture site. The position of the screws was as close to the surface as possible where the bone quality is often the best. The HCS was always placed over a k-wire. The appropriate screw length was chosen to prevent interference with subsequent reduction of the reconstructed fragment into the fracture. An example is shown in Fig. 1. The screws were buried intra-osseous to not interfere with overlying implants or other fragments.
Example of inter-fragmentary fixation in a 52-year-old female with a Schatzker type V fracture of the left knee with two lateral fragments (patient 26). A Pre-operative axial CT-scan showing the two lateral fragments. B Intra-operative fluoroscopy displaying the HCS used for inter-fragmentary fixation of the lateral fragments and their placement as close to the surface as possible. Two HCS are used to fixate the tibial eminence. C Post-operative axial CT-scan showing the concept of “two-level” interfragmentary fixation, where the fused fragment is reduced and fixated with an overlying plate with rafting screws. D Radiograph 10 months after treatment with the HCS
For fixation of a tibial eminence fragment, the screws were placed either antegrade (from the fragment toward distal) or retrograde (from distal into the fragment).
Once the HCS was in place and all the fragments reduced as anatomic as possible, fixation was completed with a buttress (locking) plate with rafting screws. Autologous bone graft from ipsilateral iliac crest or bone graft substitutes were used to fill large metaphyseal gaps caused by dis-impacting the articular fragments.
Postoperatively, a removable splint was applied for 10 days to allow wound healing. Patients were put on anticoagulant and antibiotics for 24–48 h. Depending on fracture pattern and fixation used, patients were allowed early range of motion on post-operative day one. No continuous passive motion was used. Patients were started on toe-touch weight-bearing for the first 6 weeks which was then increased to partial weight-bearing for another 6 weeks. Full weight-bearing was allowed at 3 months.
Explanatory variables and outcomes
Clinical baseline variables retrieved from the electronic medical record included age, gender, mechanism of injury, Schatzker and AO/OTA fracture type [8, 9], and surgical treatments before the index procedure.
Surgical variables included fragment fixation type, operative approach, and number and length of the HCS, and their location. For presentation, we categorized the fragment fixation type into the following categories: (I) inter-fragmentary fixation of multiple, adjacent intra-articular fragments, (II) fixation of solitary intra-articular fragments (against an already reduced or non-fractured part of the tibial plateau), and (III) fixation of the tibial eminence. The location of fragments was described using the ten-column classification [10].
Clinical outcomes included (time to) union, reduction quality, arthrosis according to the Kellgren and Lawrence classification, range of motion (ROM), complications, and secondary surgeries. Union was determined by 3 out of 4 cortices having healed on plain radiographs and clinical assessment. In case of doubt of union, a dual energy CT scan with metal artifact reduction was obtained. Reduction quality was determined by measuring the maximal gap, step-off, and depression. Reductions were classified as anatomic (0 mm step-off, gap or depression), good (≤ 2 mm), fair (2–5 mm), or malreduction (> 5 mm) [11]. Depression was measured by drawing a line through the base of the tibial eminence parallel to the femoral condyles and then measuring the distance to the base of the tibial plateau. Arthrosis was assessed on the last available radiograph. The Kellgren and Lawrence classification system grades arthrosis on AP radiographs as 0 (none), 1 (doubtful), 2 (minimal), 3 (moderate), or 4 (severe), based on joint space narrowing, presence of osteophytes, sclerosis, and deformity [12].
Patient-reported outcome measures consisted of functional outcomes assessed with the Knee Injury and Osteoarthritis Outcome Score (KOOS) [13]. Outcome measures from patients that underwent TKA were recorded but excluded from statistical analysis.
Statistical analysis
Categorical variables are presented as frequencies with percentages. Numerical variables are presented as medians with interquartile range (IQR). Missing data were accounted for by pairwise deletion (complete case analysis). Normality of the data was assessed by visual inspection of histograms. Explanatory variables are categorized for: follow-up duration (0–3, 3–6, 6–9, or > 9 years); injury mechanism (low or high energy), Schatzker type (unicondylar I–IV or bicondylar V–VI); surgical approach (single or dual incision); reduction quality (anatomical or non-anatomical), and arthrosis grade (0–1 or 2–4). In bivariate analysis, differences in KOOS scores are assessed using Kruskal–Wallis test or Mann–Whitney U test based on the number of categories of the explanatory variable (based on non-normal distribution the data). Data from the electronic medical record were collected using a Microsoft Excel spreadsheet. Patient-reported outcomes were collected using Castor EDC [14]. Significance was set at two-tailed alpha < 0.05. All statistical analyses were performed using SPSS, version 27.0 (SPSS Inc., Chicago, IL, USA).
Results
Clinical baseline and surgical variables (n = 29)
There were 15 males and 14 females with an average age of 46 years (IQR 37–57). According to the Schatzker classification, there were 8/29 (28%) Schatzker II fractures, 1/29 (3%) Schatzker III, 6/29 (21%) Schatzker IV, 7/29 (24%) Schatzker V, and 7/29 (24%) Schatzker VI [8]. According to the AO/OTA classification, there were 14/28 (50%) 41B3 fractures, 9/28 (32%) 41C1, 2/28 (7%) 41C2, and 4/28 (14%) 41C3 [9]. One Schatzker type IV fracture was a variant with an isolated posterocentral fragment and was not classified according to AO/OTA. All injuries were closed. The mechanisms of injury were 8 falls, 11 traffic accidents (7 bike, 2 scooter, 2 motorbike) and 5 skiing accidents. There were missing data for the mechanism of injury in 5 patients.
One patient was treated with revision osteo-synthesis due to an unfavorable result from ORIF in another country.
There were 9/29 (31%) fractures temporary stabilized with an external fixator. In 2/29 (7%) patients, compartment syndrome developed, and a fasciotomy was performed prior to ORIF.
According to our categorization, the HCS was used in 10/29 (34%) patients for inter-fragmentary fixation of intra-articular fragments, in 8/29 (28%) for fixation of a solitary, intra-articular fragment and in 8/29 (28%) for fixation of the tibial eminence. In 2/29 (7%) patients, the HCS was used for inter-fragmentary fixation of intra-articular fragments and fixation of the tibial eminence concomitantly. In the remaining patient, multiple HCS were used for fragments of the tibial tuberosity. Individual patients and their specific fragment fixation are detailed in Table 1.
Clinical outcome measures (n = 28)
Union was achieved in all patients at an average of 3 months (IQR 2.7–3.3). Reduction was graded as anatomic (19) or good (4) in 23/28 (82%) of cases, fair in 4/28 (14%), and as a malreduction in 1/28 (4%) on radiographs.
According to the Kellgren and Lawrence classification, arthrosis was grade 0 in 7/28 (25%) patients, grade 1 in 11/28 (39%), grade 2 in 6/28 (21%), and grade 3 in 4/28 (14%).
Range of motion was described for 23/28 (82%) patients. Median flexion was 110 degrees (IQR 100–130), and five patients had an extension deficit of 5 (n = 3) and 10 (n = 2) degrees.
Complications were seen in 7/28 (25%) patients. There were two deep and one superficial surgical site infections (SSI) [15]. Two patients with a deep SSI were successfully treated with revision fixation, debridement, and antibiotics and with debridement and antibiotics alone, respectively. The latter of these patients developed a footdrop, presumably due to peroneal nerve traction injury. One patient had a superficial SSI due to a remaining stitch which healed well without antibiotics. The patient was later diagnosed with a malunion (valgus axis) of the lateral plateau for which revision surgery was performed 7 months after the index procedure. The patient healed with good alignment 3 months later. Two other patients had a systemic complication: dyspnea, minor cardiac ischemia, and an allergic rash to antibiotics (n = 1), and deep venous thrombosis (n = 1). All complications resolved, except the peroneal nerve traction injury.
Two patients (7%) had a complication directly related to the HCS. One patient (patient 15) had inter-fragmentary fixation of 4 fragments for a Schatzker type II fracture and presented 22 months after the procedure with pain in the knee. A CT scan showed that one of the HCS had migrated behind the femoral head. There was no loss of reduction. All materials were removed in the operating theater, but the HCS could not be retrieved. Afterward the complaints improved, and the patient could walk 2 km without pain, indicating that the migrated screw was not the cause of the pain. In retrospect, the screw was not optimally placed within the subchondral bone as noted on a post-operative CT-scan.
One patient (patient 17) had inter-fragmentary fixation of 3 fragments for a Schatzker type II fracture. He admitted to mis-stepping several times within 4 months of the initial procedure. The patient experienced an ‘acute’ moment while mis-stepping in a pit while carrying a load which caused a collapse of the centrolateral plateau and migration of one HCS laterally into the soft tissue. The migrated HCS and one other HCS were removed. Five months later, an additional k-wire was removed. He underwent TKA within one year of the index surgery. At latest follow-up, he was doing well, including downhill skiing.
Other secondary surgeries consisted of hardware removal in 9/28 (32%) patients due to pain caused by the osteo-synthesis material. In 5 of these, at least one HCS was left in place because they were completely intra-osseous. One patient underwent surgery for heterotopic ossification around the patellar tendon and the medial ligaments. This may have been caused by excessive bone formation after demineralized bone matrix treatment [16]. Three patients had an arthroscopic procedure for arthrofibrosis (n = 2) and debridement of a small lateral meniscus tear (n = 1). One of these patients received an additional surgery in an outside institution to increase range of motion by arthrolysis. One additional patient underwent TKA for symptomatic arthrosis within 1 year after the index procedure.
Patient-reported outcome measures (n = 20)
The median KOOS score for symptoms and stiffness was 69 points (IQR 45–78), for pain 71 (IQR 45–88), for activities of daily living (ADL) 85 (IQR 52–95), for sports 30 (IQR 11–55), and for quality of life (QOL) 34 (IQR 19–56). The KOOS sub-scores are presented for categories of follow-up duration, injury mechanism, Schatzker type, surgical approach, reduction quality, and arthrosis grade in Table 2. Patients with unicondylar (Schatzker I–IV) reported better scores on all outcomes when compared to patients with bicondylar fractures (V–VI). This was a statistically significant difference for pain (88.9 vs. 51.4; p = 0.005), ADL (95.6 vs. 67.6; p = 0.002), sports (55.0 vs. 20.0; p = 0.047), QOL (56.3 vs. 25.0; p = 0.012), and overall KOOS (72.9 vs. 47.0; p = 0.002). Similarly, patients that underwent a single-incision surgical approach (compared to dual incision) had significantly better outcomes for pain (88.9 vs. 61.1; p = 0.042), QOL (62.5 vs. 31.3; p = 0.033), and overall KOOS (85.0 vs. 56.2; p = 0.033). No significant differences in scores were observed when comparing categories of follow-up duration and injury mechanism. Although patients with anatomical reduction (compared to non-anatomical reduction) showed higher scores on all subscores, this did not reach significance.
Discussion
The main objective in the surgical management of a tibial plateau fracture is anatomic restoration and stable fixation that allows early motion. In this report, we present a series of 29 patients with a comminuted tibial plateau fracture that were treated with open reduction and internal fixation using plates and screws with the addition of fully threaded headless cannulated compression screws for a “two-level fixation”.
Stable anatomic reduction of the tibial plateau can be challenging when there are more than 2–3 fragments without a cortical border. The lateral plateau is more prone to fragmentation and impaction due to its convex shape, as opposed to the medial tibial plateau which is concave [17]. Therefore, an axial load on the knee joint causes a multi-fragmentary lateral depression type fracture. We were the first to map tibial plateau fractures with CT images and identified a lateral split fragment with or without comminution (defined as fragments smaller than 1.0 cm2 in size) as one of four main features of tibial plateau fractures [18].
For this fracture pattern, standard treatment includes the use of a rafting construct to provide axial support [19]. Authors have suggested different construct variations to better support small fragments. Yoon et al. described the “inside out” technique, in which articular fragments are fixated with a k-wire that is inserted from lateral to medial and then retrieved from the medial side until the k-wire is on par with the lateral side of the fragment, after which the lateral split fragment is reduced, and the k-wires are advanced back to the lateral side [20].
As an alternative, Giordano et al. used a flattened one-third tubular plate that was placed in the subchondral bone after reduction of depressed fragments to treat four tibial plateau fractures with articular depression [21]. All four patients healed without a significant loss of reduction.
Similar to our technique, Reul et al. used free subchondral screws in 23 patients with depressed intra-articular fragments of the lateral plateau [22]. They performed an arthrotomy and osteotomy of the lateral tibial condyle after which the depressed fragment was reduced under direct visualization and fixated with one or more 2.7 mm stable angle screws. These were placed in the subchondral bone and intra-osseous. Full ROM was achieved in 10/23 (43%) patients, and 3/23 (13%) patients’ flexion was reduced by 30 degrees or more. 58% of patients’ reduction was suboptimal with a step-off of more than 2 mm and a suboptimal alignment based on post-operative CT scans.
In this report, we introduced the use of HCS to provide additional support for small fragments in comminuted tibial plateau fractures. Our standard to fragment fixation includes the use of k-wires or lag screws and the use of a rafting construct for support. The use of the HCS was indicated in fractures that presented with (multiple) small, intra-articular or tibial eminence fragment(s) that could not be sufficiently reduced with the use of lag screws (due to the absence of a cortical border) or k-wires (due to insufficient compression), or that needed additional support complementary to the rafting screw construct (due to an inadequate purchase of bone stock of the fragment). Although there were no specific contra-indications to the use of the HCS, a relative contraindication might be the use of HCS in elderly patients as these are prone to secondary a loss of fixation, especially in case of fractures with extensive fragmentation [23]. Because the HCS are buried intraosseous, removal during revision surgeries might propose problems. In our 15-year experience, we have not encountered this problem. This limitation is also relevant in patients that require TKA. In our experience, one patient that underwent TKA had a HCS in place at the moment of surgery. As this procedure was performed in an outside institution, we do not know if this caused any problems. Difficult removal could also be problematic in case of a deep infection. We therefore urge surgeons to be meticulous in their approach to prevent infectious complications. It should be noted that k-wires are easier to remove than HCS, which could circumvent some of the limitations of the HCS mentioned above. However, k-wires do not have the benefit of providing inter-fragmentary fixation and HCS have biomechanical advantages over k-wires [24].
In our series, we found the HCS to be very helpful for inter-fragmentary fixation of intra-articular fragments in the lateral plateau when standard fixation was deemed insufficient (Fig. 2). The benefits of the HCS are the following: first, the screws can be introduced from multiple directions, which allows for an optimal purchase of bone stock. Second, the head of the screw can be buried inside the plateau (intra-osseous), which enables freedom for subsequent placement of overlying plates and other fragments (“two-level” fixation) and is less likely to cause complaints. Third, it is possible to perform inter-fragmentary fixation on a side table under direct visual control. The variable pitch of the HCS provides compression between these fragments that can then be reduced into the fracture as a whole. To optimize the amount of inter-fragmentary compression, one should maximize screw length and place the center of the screw perpendicular to the fracture line [25]. Fourth, as they are titanium, they cause less artifact when performing MRI to evaluate post-traumatic changes of the cartilage, menisci, and cruciate ligaments.
The patient-reported functional outcomes of our series were compared to the existing literature. Jansen et al. evaluated 22 patients with intra-articular AO/OTA type C fractures after a mean follow-up of 67 months [26]. They report a mean KOOS score of 68 points (our series median: 60 points). Henkelmann et al. evaluated 246 patients with a AO type B and C tibial plateau fractures (without post-operative SSI) after a mean follow-up of 78.9 months [27]. They report mean KOOS subscores for pain of 75 (our series median: 71), symptoms and stiffness 75 (our series median: 69), ADL 81 (our series median: 85), sports 41 (our series median: 30), and QOL 56 (our series median: 34). Dreumel et al. evaluated 71 patients with a tibial plateau fracture treated with ORIF after a mean of 6 years [28]. They report median KOOS subscores for pain of 90, symptoms and stiffness of 91, ADL of 90, sports of 73, and QOL of 75. Timmers et al. assessed 82 patients with Schatzker type I to VI fractures treated with ORIF, and report similar KOOS subscores for symptoms and stiffness, pain, and ADL, but better subscores on sports (50 vs. our series: 30) and QOL (55 vs. our series: 34) [29]. An important difference between these studies and our series is that we used a dual incision approach with double plating in 52% of patients (compared to Jansen et al.: 14% [26], Henkelmann.: 14% [27], Timmers et al.: 3% [29]), which might explain the difference in scores: bivariate analysis in our series demonstrated that patients with bicondylar fractures (and consequently dual incision treatment) reported significantly lower functional outcomes. Another factor that might influence these results is indication bias; we only used HCS for fractures with comminuted, small, and intra-articular fragments in which reduction with standard implants was deemed insufficient. Lastly, it should be noted that all subscores of the KOOS in our series demonstrated substantially large interquartile ranges, depicting that there was a considerable difference between the outcomes reported by our patients.
The most feared short-term complication after tibial plateau fracture surgery is a SSI. These occur in approximately 10% of cases (range 2.6–45.0%; of which deep: 6.4%, superficial: 3.6%), and are associated with worse clinical and patient-reported outcomes [27, 30]. In our series, the rate of deep and superficial SSI was 7 and 4%, respectively, and all infections resolved with appropriate treatment. Infection risk can be mitigated by adequate timing of the surgery and careful soft tissue management. Other complications associated with tibial plateau fractures are malunions and systemic complications such as deep vein thrombosis. These complications only occurred incidentally in our series.
The most important long-term complication after a tibial plateau fracture is posttraumatic arthrosis. Important determinants for the development of arthrosis include alignment and articular congruity [31, 32]. In our series, 35% of patients had at least minimal signs of arthrosis at the end of clinical follow-up. This is in range with the literature. In a previous report of 109 tibial plateau fractures from our department, 31% of patients had developed secondary arthrosis after operative treatment [31]. Manidakis et al. found evidence of arthrosis in 26.4% of patients [33]. For Schatzker type V and VI fractures, this was as a high as 58%. Jansen et al. reported signs of arthrosis in 70% [26]. In our series, patients with arthrosis had considerably worse scores on all subscales of the KOOS, but this did not reach statistical significance. Despite the presence of arthrosis, we only know of 2/28 (7%) patients that underwent TKA. In one patient because of symptomatic arthrosis and in one patient due to a significant collapse of the lateral plateau after a misstep. This rate of TKA after operative treatment of tibial plateau fractures is within range of previous literature [28, 29, 33, 34].
The present study has several limitations. First, the retrospective design is associated with methodological drawbacks, such as the lack of predefined follow-up variables and standardized assessment of outcomes. For example, we do not routinely follow patients with CT scans to limit radiation exposure and as a consequence, we relied on standard radiographs to determine fracture reduction quality. Radiographs are less sensitive to detect reduction defects, which was also seen in two of our cases [35]. Moreover, we did not perform long leg standing radiographs and were therefore not able to determine alignment. Nevertheless, we were able to collect relevant clinical outcome variables from the electronic patient records and we were able to retrieve (long-term) functional outcomes of 76% of patients, which is comparable to previous studies [28, 29]. Second, we did not include a matched cohort to compare the use of HCS to standard fixation techniques for fragments (i.e., k-wires or lag screws). However, a case–control design would not provide an appropriate comparison due to selection bias: we used HCS only in fractures were standard fixation was deemed insufficient. Therefore, a comparison between these techniques would be inherently biased by the fracture pattern. Third, there was no single standardized surgical protocol as the screws were used to treat a variety of fragment types. However, we also believe that this variety displays the versatility to fixate fragments with these screws. Fourth, all patients were treated by a single surgeon in a single institution, which questions the generalizability to the overall population. However, the procedure is a relatively simple variation of standard treatment and can therefore easily be used by other surgeons as well. Lastly, comparing outcomes of treatment of tibial plateau fractures is difficult due to the variation in fracture patterns, treatments, and follow-up protocols. Therefore, we cannot make claims on the superiority of our approach to comminuted tibial plateau fractures.
In conclusion, the use of fully threaded headless cannulated compression screws is a simple and helpful addition in the treatment of comminuted tibial plateau fractures in which fixation of intra-articular fragments with k-wires or lag screws is deemed insufficient. The screws can be used for two-level, (inter-fragmentary) fixation of intra-articular fragments and for fixation of the tibial eminence.
References
Kfuri M, Schatzker J. Revisiting the Schatzker classification of tibial plateau fractures. Injury. 2018;49(12):2252–63. https://doi.org/10.1016/j.injury.2018.11.010.
Prat-Fabregat S, Camacho-Carrasco P. Treatment strategy for tibial plateau fractures: an update. EFORT Open Rev. 2016;1(5):225–32. https://doi.org/10.1302/2058-5241.1.000031.
Kuner E, et al. Reposition und Stabilisation von Tibiaplateaufrakturen. Oper Orthop Traumatol. 2020;32(2):139–57. https://doi.org/10.1007/s00064-020-00655-x.
Wang Y, et al. Updated three-column concept in surgical treatment for tibial plateau fractures—a prospective cohort study of 287 patients. 1879–0267 (Electronic).
Luo C-F, et al. Three-column fixation for complex tibial plateau fractures. J Orthop Trauma. 2010;24(11):683–92.
Chen MJ, et al. Low profile fragment specific plate fixation of lateral tibial plateau fractures—a technical note. Injury. 2021;52(4):1089–94. https://doi.org/10.1016/j.injury.2020.12.037.
Giannoudis PV, Tzioupis C, Moed BR. Two-level reconstruction of comminuted posterior-wall fractures of the acetabulum. J Bone Jt Surg Br. 2007;89(4):503–9. https://doi.org/10.1302/0301-620x.89b4.18380.
Schatzker J. Compression in the surgical treatment of fractures of the tibia. Clin Orthop Relat Res. 1974;105:220–39.
Meinberg EG, et al. Fracture and dislocation classification compendium-2018. J Orthop Trauma. 2018;32(Suppl 1):S1-s170. https://doi.org/10.1097/bot.0000000000001063.
Krause M, et al. Intra-articular tibial plateau fracture characteristics according to the “Ten segment classification.” Injury. 2016;47(11):2551–7. https://doi.org/10.1016/j.injury.2016.09.014.
Weil YA, et al. Posteromedial supine approach for reduction and fixation of medial and bicondylar tibial plateau fractures. J Orthop Trauma. 2008;22(5):357–62.
Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16(4):494–502. https://doi.org/10.1136/ard.16.4.494.
de Groot IB, et al. The Dutch version of the knee injury and Osteoarthritis Outcome Score: a validation study. Health Qual Life Outcomes. 2008;6:16. https://doi.org/10.1186/1477-7525-6-16.
Castor EDC. Castor electronic data capture. 2019 August 28, 2019. Available from: https://castoredc.com.
CDC Surgical Site Infection (SSI) [23-02-2022]. Available from: http://www.cdc.gov/nhsn/pdfs/pscmanual/9pscssicurrent.pdf.
Nota SP, Kloen P. Heterotopic ossification around the knee after internal fixation of a complex tibial plateau fracture combined with the use of demineralized bone matrix (DBM): a case report. Arch Bone Jt Surg. 2014;2(4):250–4.
Eggli S, et al. Unstable bicondylar tibial plateau fractures: a clinical investigation. J Orthop Trauma. 2008;22(10):673–9. https://doi.org/10.1097/BOT.0b013e31818b1452.
Molenaars RJ, et al. Tibial plateau fracture characteristics: computed tomography mapping of lateral, medial, and bicondylar fractures. J Bone Jt Surg Am. 2015;97(18):1512–20. https://doi.org/10.2106/jbjs.N.00866.
Karunakar MA, et al. Split depression tibial plateau fractures: a biomechanical study. J Orthop Trauma. 2002;16(3):172–7. https://doi.org/10.1097/00005131-200203000-00006.
Yoon Y-C, et al. Inside out rafting K-wire technique for tibial plateau fractures. Arch Orthop Trauma Surg. 2012;132(2):233–7. https://doi.org/10.1007/s00402-011-1409-z.
Giordano V, et al. Subchondral rafting plate for the treatment of fragmented articular central depression tibial plateau fracture patterns: case series and technical illustration. Cureus. 2021;13(1):e12740–e12740. https://doi.org/10.7759/cureus.12740.
Reul M, et al. Open reduction and internal fixation of lateral tibial plateau fractures with free subchondral 2.7 mm screws. Oper Orthop Traumatol. 2017;29(5):431–51. https://doi.org/10.1007/s00064-017-0502-z.
Ali AM, El-Shafie M, Willett KM. Failure of fixation of tibial plateau fractures. J Orthop Trauma. 2002;16(5):323–9. https://doi.org/10.1097/00005131-200205000-00006.
Avery DM 3rd, Klinge S, Dyrna F, Pauzenberger L, Lam D, Cote M, DiVenere J, Obopilwe E, Mazzocca A, Rodner C. Headless compression screw versus kirschner wire fixation for metacarpal neck fractures: a biomechanical study. J Hand Surg Am. 2017;42(5):392.e1–e6. https://doi.org/10.1016/j.jhsa.2017.02.013.
Patel S, et al. Interfragmentary compression forces vary based on scaphoid bone screw type and fracture location. Hand (NY). 2019;14(3):371–6. https://doi.org/10.1177/1558944717745663.
Jansen H, et al. Medium-term results after complex intra-articular fractures of the tibial plateau. J Orthop Sci. 2013;18(4):569–77. https://doi.org/10.1007/s00776-013-0404-3.
Henkelmann R, et al. Impact of surgical site infection on patients’ outcome after fixation of tibial plateau fractures: a retrospective multicenter study. BMC Musculoskelet Disord. 2021;22(1):531. https://doi.org/10.1186/s12891-021-04402-6.
van Dreumel RL, et al. Mid- to long-term functional outcome after open reduction and internal fixation of tibial plateau fractures. Injury. 2015;46(8):1608–12. https://doi.org/10.1016/j.injury.2015.05.035.
Timmers TK, et al. Functional outcome after tibial plateau fracture osteosynthesis: a mean follow-up of 6years. Knee. 2014;21(6):1210–5. https://doi.org/10.1016/j.knee.2014.09.011.
Henkelmann R, et al. Infection following fractures of the proximal tibia—a systematic review of incidence and outcome. BMC Musculoskelet Disord. 2017;18(1):481. https://doi.org/10.1186/s12891-017-1847-z.
Rademakers MV, et al. Operative treatment of 109 tibial plateau fractures: five- to 27-year follow-up results. J Orthop Trauma. 2007;21(1):5–10. https://doi.org/10.1097/BOT.0b013e31802c5b51.
Parkkinen M, et al. Factors predicting the development of early osteoarthritis following lateral tibial plateau fractures: mid-term clinical and radiographic outcomes of 73 operatively treated patients. Scand J Surg. 2014;103(4):256–62. https://doi.org/10.1177/1457496914520854.
Manidakis N, et al. Tibial plateau fractures: functional outcome and incidence of osteoarthritis in 125 cases. Int Orthop. 2010;34(4):565–70. https://doi.org/10.1007/s00264-009-0790-5.
Wasserstein D, et al. Risk of total knee arthroplasty after operatively treated tibial plateau fracture: a matched-population-based cohort study. JBJS. 2014;96(2):144–50.
Borrelli J Jr, Ricci WM, Steger-May K, Totty WG, Goldfarb C.Postoperative radiographic assessment of acetabular fractures: a comparison of plain radiographs and CT scans. J Orthop Trauma. 2005;19(5):299–304.
Funding
No funding was received to assist with the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
Both authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by both authors. The first draft of the manuscript was written by RKW, and PK commented on previous versions of the manuscript. Both authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to declare that are relevant to the content of this article.
Ethics approval
The Medical Ethics Review Committee confirmed that the Medical Research Involving Human Subjects Act (WMO) does not apply to this study and that an official approval of this study by the committee is not required (reference number: W21_182 # 21.197). The study was carried out in accordance with the World Medical Association Declaration of Helsinki.
Consent
Verbal informed consent to participate was obtained from participants. As per local institutional guidelines, if it was impossible to obtain consent, research using previously collected and patient data is allowed (ground: general no-objection).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wagner, R.K., Kloen, P. Two-level fixation with headless compression screws for tibial plateau fractures. Eur J Trauma Emerg Surg 48, 4683–4698 (2022). https://doi.org/10.1007/s00068-022-01982-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-022-01982-3