Abstract
Purpose
Pelvic gynecologic trauma (PGT) includes injury to the uterus, ovaries or fallopian tubes. We hypothesized Injury Severity Score (ISS) ≥ 25, hypotension on admission and age ≥ 51 (average age for menopause) would be independent risk factors for resection compared to repair.
Methods
A retrospective analysis of the National Trauma Data Bank was performed between 2007 and 2015.
Results
Of 2,040,235 female patients, 1938 (< 0.1%) presented with PGT with the majority sustaining injury to the ovary or fallopian tubes (52.9%). Most patients were managed nonoperatively (77.1 vs 22.9%). On multivariable analysis, in patients with injury to the uterus, ISS ≥ 25 (OR 3.52, CI 1.67–7.48, p < 0.05) was associated with higher risk for hysterectomy compared to repair. In patients with injury to the ovaries or fallopian tubes, gunshot wound (OR 3.73, CI 1.43–9.68, p < 0.05) was associated with a higher risk for salpingectomy or oophorectomy compared to repair. Age ≥ 51 and hypotension on admission were not independent risk factors for resection in patients with PGT. Operative treatment was associated with a lower risk for mortality in patients with an injury to the uterus (OR 0.27, CI 0.14–0.51, p < 0.001) or ovaries/fallopian tubes (OR 0.37, CI 0.19–0.72, p < 0.001) compared to those managed nonoperatively.
Conclusion
In the largest study reported, PGT occurred in < 0.1% of traumas involving women. Patients with ISS ≥ 25 have higher risk for hysterectomy compared to repair. Gunshot injuries have higher risk for salpingectomy or oophorectomy compared to repair. Hypotension on arrival or age ≥ 51 are not independent risk factors for resection in PGT. Operative management is associated with lower risk of mortality in PGT patients.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Pelvic gynecologic trauma (PGT) includes injury to the uterus, ovaries or fallopian tubes. PGT rarely occurs in < 1% of blunt trauma [1, 2]. The female pelvis, designed for childbirth, is overall broader and transversely oval compared to the male pelvis, providing a safeguard for organs within its confines [3]. Except for a few case reports, there is a paucity of literature regarding PGT [4, 5].
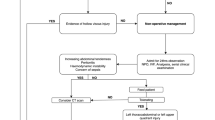
In previous studies, Injury Severity Score (ISS) ≥ 25 has been associated with increased morbidity and mortality in trauma [6, 7]. The presence of shock has been shown to be associated with higher risk of mortality with trauma as well as a higher risk of peri-partum hysterectomy [8,9,10]. Unfortunately, PGT may not be recognized until the patient is emergently brought into the operating room and under general anesthesia, making a preoperative discussion regarding the possible removal of reproductive organs unlikely. This may sway the decision of a trauma surgeon away from resection in a pre-menopausal woman. Therefore, we sought to perform a descriptive analysis of PGT and hypothesized ISS ≥ 25, hypotension on arrival and age ≥ 51 (national average age for menopause) would be independent risk factors for resection compared to repair of the uterus and ovary or fallopian tubes.
Methods
A retrospective analysis of the National Trauma Data Bank (NTDB) was performed between January 2007 and December 2015 [11]. All female patients ≥ 16 years of age were eligible for inclusion. We collected patients with an injury to the uterus, ovaries or fallopian tubes using International Classification of Diseases (ICD version 9) diagnosis codes (uterus injury: 867.4 and 867.5; ovary/fallopian tube injury 867.7). The NTDB does not separate diagnosis codes for ovarian and fallopian tube injuries so these patients were grouped together. Next, we stratified patients based on whether they underwent repair or resection of reproductive organs (hysterectomy or salpingectomy/oophorectomy) identified by the appropriate ICD-9 procedure-codes. The NTDB does not separate procedure codes for salpingectomy and oophorectomy so these patients were grouped together. Any associated pelvic fracture, pelvic hematoma and rectal or bladder injury were identified based on the appropriate ICD-9 diagnosis codes.
Patient demographic information was collected including age, presence of hypotension (systolic blood pressure < 90 mmHg) on arrival, pre-hospital comorbidities, ISS and abbreviated injury scale (AIS). The outcomes evaluated included in-hospital urinary tract infection, total hospital length of stay (LOS), Intensive Care Unit (ICU) LOS, ventilator days and mortality. Missing data points were not imputed but treated as missing data.
Descriptive statistics were performed for all variables. A Student’s t test was used to compare continuous variables and Chi square was used to compare categorical variables for bivariate analysis. Categorical data were reported as percentages and continuous data were reported as medians with interquartile range. The primary outcome was resection of reproductive organs (hysterectomy, salpingectomy/oophorectomy). Variables were chosen based on univariable analysis and review of the literature. Confounding variables were controlled for using a hierarchical multivariable logistic regression model. Risk of resection compared to repair was reported with an odds ratio (OR) and 95% confidence intervals (CI). All p values were 2-sided, with a critical significance level of < 0.05. All statistical analyses were performed with IBM SPSS Statistics for Windows, Version 24. (Armonk, NY: IBM Corp).
Results
From 2,040,235 female patients in the NTDB years 2007–2015, 1938 (< 0.1%) presented with PGT, with 1026 (51.3%) having injury to the ovaries or fallopian tubes. Most patients were managed nonoperatively (77.1 vs 22.9%). The most common missing data was LOS [81 (4.1%) missing]. In patients with an injury to the uterus, 5.8% had a hysterectomy, whereas 20.2% underwent repair. In patients with ovarian or fallopian tube trauma, 6.7% underwent salpingectomy or oophorectomy compared to 12.5% that required repair (Table 1).
Compared to patients with a uterus injury managed non-operatively, those requiring surgery had a higher median ISS (18.0 vs 14.0, p < 0.001), were more likely to have hypotension on arrival (17.5 vs 11.8%, p < 0.001), more likely to be a victim of gun violence (45.9 vs 9.6%, p < 0.001) but less likely to be involved in a motor vehicle collision (41.4 vs 67.3%, p < 0.001). Those requiring surgery also had a higher incidence of injuries to the rectum (13.1 vs 4.0%, p < 0.001), bladder/urethra (19.0 vs 7.2%, p < 0.001) and spine (25.7 vs 19.3%, p < 0.001).
When compared to patients with ovarian or fallopian tube injury managed non-operatively, those requiring surgery had a higher median ISS (18.0 vs 12.0, p < 0.001) and were more likely to have hypotension on arrival (18.2 vs 8.9%, p < 0.001). They also had a higher incidence of injuries to the rectum (8.9 vs 2.8%, p < 0.001) and bladder/urethra (24.3 vs 9.4%, p < 0.001) (Table 2). Patients with an injury to the uterus requiring surgery had a longer median LOS (10 vs 4 days, p < 0.001) and lower mortality rate (5.6% vs 11.9%, p < 0.001). Patients with an injury to the fallopian tube or ovaries requiring surgery had a longer median LOS (11 vs 5 days, p < 0.001) and lower mortality rate (6.1 vs 9.1%, p < 0.001) (Table 3).
Compared to those that underwent hysterectomy, patients undergoing repair of the uterus had a significantly lower median ISS (16.0 vs 26.0, p < 0.001) and were less likely to be hypotensive on arrival (15.7 vs 27.8%, p < 0.001). There was no difference in associated pelvic fractures, pelvic hematomas, rectal, bladder/urethra or spine injuries (cord or vertebrae), LOS, ICU LOS or ventilator days (all p > 0.05) (Table 4).
Compared to those that underwent salpingectomy or oophorectomy, patients with injury to the ovaries or fallopian tubes requiring only repair were significantly younger (median age, 25.0 vs 29.5 years), less likely to be hypotensive on arrival (15.6 vs 24.2%) and less likely to be involved in gunshot violence (24.2 vs 43.9%). There was no difference in associated pelvic fractures, pelvic hematoma, rectal, bladder/urethra or spine injuries, LOS, ICU LOS or ventilator days (p > 0.05).
On multivariable analysis, patients with injury to the uterus and ISS ≥ 25 (OR 3.52, 95% CI 1.67–7.48, p < 0.05) had higher risk for hysterectomy compared to repair. In patients with injury to the ovaries or fallopian tubes, gunshot wound (OR 3.73, 95% CI 1.43–9.68, p < 0.05) was associated with higher risk for salpingectomy or oophorectomy compared to repair (Table 5). Hypotension on arrival was not shown to be an independent risk factor for resection in PGT. Age ≥ 51 was not shown to be a risk factor. However, only 15 patients with PGT in this age group required surgery.
Due to the aforementioned paradoxical increased mortality associated with non-operative management compared to operative management of PGT, a post-hoc analysis using a multivariable logistic regression analysis was performed. After adjusting for age ≥ 65, hypotension on arrival, other major abdominal surgery and ISS, operative treatment (resection or repair) of PGT continued to be associated with a lower risk for mortality in patients with an injury to the uterus (OR 0.27, 95% CI 0.14–0.51, p < 0.001) or ovaries/fallopian tubes (OR 0.37, 95% CI 0.19–0.72, p < 0.001) compared to those managed nonoperatively.
Discussion
Our study attempted to fill a void in the literature regarding the management of PGT. In the largest study reported, we found PGT occurred in < 0.1% of traumas involving women. Interestingly, we were able to demonstrate that operative intervention in patients with PGT was associated with a lower mortality rate compared to those managed non-operatively. We sought to find predictors of resection vs repair within this patient population. The strongest independent risk factors for hysterectomy was ISS ≥ 25 while a gunshot wound was the strongest predictor for salpingectomy or oophorectomy. We did not find an association with age ≥ 51 and hypotension on arrival with resection compared to repair in patients with PGT.
Menopause may play a role in the decision to remove a reproductive organ in trauma. While PGT has an incidence less than 0.1%, the decision to resect or repair has immense personal ramifications for not only the patient’s ability to potentially bear children but also hormone-related effects including cardiovascular disease, neurological sequelae and potential psychiatric illness [12,13,14]. Menopause is defined as the permanent cessation of ovulation occurring at an average age of 51 years [15, 16]. In the non-trauma literature, risk of hysterectomy is associated with increased age [17]. Bhavnani et al. [18] conducted a survey on women awaiting resection of reproductive organs for benign conditions. A recurring theme in their responses was the fact that they felt unhappy with a “medicalized” menopause as opposed to a normal physiologic process suggesting patient dissatisfaction with any surgical induced menopause. This prompted us to investigate whether menopause is more likely to be associated with hysterectomy or salpingectomy/oophorectomy in PGT. In our study, we did not find age ≥ 51 (our surrogate for menopause as NTDB does not collect whether patient is menopausal or not) to be associated with resection vs repair. However, despite using a large national database, our study appears to be underpowered as only ten patients ≥ 51 years of age over an 8-year period sustained an injury to the uterus requiring surgical intervention (three hysterectomies and seven repairs). In the case of ovarian or fallopian tube injury, age ≥ 51 had a trend towards higher risk for salpingectomy or oophorectomy compared to repair but this was not statistically significant (p = 0.07). Only five patients ≥ 51 years of age with injuries to the fallopian tubes or ovaries underwent surgery (four oophorectomy/salpingectomy and one repair). Many more years of NTDB data will need to be accrued before we can make any conclusive statements regarding the role of age (menopause) in PGT patients requiring surgery.
Ongoing hemodynamic instability in the trauma patient can change the surgeon’s initial operative choice. In a multivariable logistic regression analysis, hypotension on admission was not found to be associated with higher risk for resection compared to repair in PGT patients, which may have been due to insufficient statistical power. In a post-hoc analysis, we analyzed the role of perioperative blood transfusion as a surrogate for intraoperative instability and did not find this to change our results. However, this is not a mandated data point in the NTDB. Unfortunately, the NTDB does not provide intraoperative vital signs, which may have reduced the effect that persistent hemodynamic instability had on the determination for resection vs repair by the surgeon. For instance, the determination to repair may be warranted if the patient were to arrive hypotensive but stabilize with resuscitation, whereas resection would be advocated if the patient remained in refractory shock. A guiding principal in damage-control surgery is the recognition by the surgeon of a cold, acidotic, and hypothermic patient [19, 20]. This calls for the focused effort on controlling surgical bleeding and intestinal spillage as expeditiously as possible even if that means resecting a non-vital organ that could otherwise have been repaired [19, 21, 22]. Sometimes an organ that is considered vital (e.g., liver) when hemorrhaging is treated with packing and/or topical hemostatic agents in an attempt to temporize the hemorrhage and preserve the organ. Uniquely, in the case of PGT, reproductive organs may be considered vital organs to the patient if they wish to preserve fertility. Future prospective studies that include intraoperative hemodynamics, temperature evaluation, assessment of coagulopathy, and whether surgical adjuncts such as packing and topical agents are used appear warranted to determine the relationship of damage control surgery and its effect on decision to repair vs resect pelvic gynecologic injuries.
Adjunct interventions along with a multidisciplinary approach may allow for the improved management of patients with PGT. There may be a role for uterine artery ligation/embolization in the stable patient with PGT, as this adjunct has proven to be successful in hepatic and splenic injury [23, 24]. Furthermore, in non-trauma cases of pelvic gynecologic bleeding, uterine artery embolization has been demonstrated to have a clinical success rate up to 90% [25]. One other potential effect on the rate of resection is surgical comfort with repair as this is an infrequent injury for the general/trauma surgeon. In response to the increased complexity of some obstetrics/gynecologic emergency cases, a few centers have put forth a concerted effort to have acute care/trauma surgeons collaborate with obstetrics/gynecologic surgeons to treat hemorrhaging patients. Lee at el. [26]. demonstrated that in the case of postpartum hemorrhage requiring a “takeback” to the operating room and meeting the lethal triad (acidosis, hypothermia, coagulopathy), the cases involving acute care/trauma surgeons in the decision making and re-operation all had favorable outcomes compared to those that did not (0 vs 25% mortality rate). Similarly, trauma surgeons have often relied on the expertise of obstetricians/gynecologists in managing trauma cases involving complex gynecologic injuries or a gravid uterus [27]. This suggests that the combined effort of both acute care/trauma surgery and obstetricians/gynecologists may have an important role in injuries requiring a damage-control operation. Future studies to evaluate whether a multidisciplinary approach improves outcomes is needed.
PGT is associated with injury of organs in close proximity. Injury involving the pelvic viscera after trauma is usually limited to the bladder, rectum and soft tissue and per some previous reports often a result of penetrating trauma [28, 29]. The vast majority of PGT in our study occurred after blunt trauma (78.9%). Compared to PGT patients managed non-operatively, those requiring surgery had higher rates of associated injuries (bladder, urethra, rectal). However, there was no significant difference between the rate of rectal or bladder/urethral injuries among PGT patients undergoing resection compared to repair. Stone et al. [30] found all gynecologic injuries (220 patients) requiring exploratory laparotomy following blunt abdominal trauma to be a result of motor vehicle accidents and had some degree of polytrauma with the most common associated injury being a pelvic fracture (occurring in 40% of cases). We also found pelvic fractures to be the most commonly associated injury in PGT (36.3%). However, these injuries were not associated with higher risk for resection compared to repair. One possible explanation is that the bony pelvis absorbs the impact in blunt trauma and transmits the force to the lumbosacral spine and thus protects reproductive organs from extensive injury [31]. This is supported by our study in that the second most commonly associated injury in PGT was an injury to the spinal cord or vertebrae (26.6%).
The pelvis is an anatomically restricted area crowded with internal structures at risk for damage in penetrating trauma. DiGiacomo et al. [32] found that patients with penetrating trauma traversing the pelvis had up to an 85% risk of internal organ injury. Our study found patients with an injury to the ovaries or fallopian tubes after a gunshot wound had nearly a fourfold relative increased risk for resection compared to repair. In the case of smaller structures such as the ovaries and fallopian tubes, gunshot injuries with associated blast effect may prove to be too destructive limiting the possibility of repair.
Interestingly, our study showed that PGT patients requiring surgery had a paradoxically lower rate of mortality compared to those managed non-operatively. This remained true on a multivariable logistic regression analysis controlling for significant predictors of mortality in trauma (hypotension on arrival, ISS, other major abdominal surgery and age). The exact reason for this is unclear but one possible explanation is those patients who were attempted to be managed non-operatively may have needed operative management and were not appropriately recognized for need to rescue. Future prospective studies are needed to evaluate this finding and help determine other possible explanations.
Our study has numerous limitations including the fact that the NTDB is a large national database and thus reporting bias is present. Furthermore, all our data was restricted to data fields available in the NTDB and were subject to input error. Not all data fields were complete and information regarding incomplete missing values was unavailable. Notable data fields relevant to our study that are missing in the NTDB include information regarding American Association for the Surgery of Trauma grades of both uterine and ovarian/fallopian tube injury. It is plausible that lower grade uterine injuries are less likely to have refractory bleeding and thus have lower risk for resection. Given the rarity of PGT, a prospective multicenter study would be most appropriate to further investigate risk factors for resection and to confirm our findings.
Conclusion
PGT occurs in < 0.1% of traumas involving women. Patients with ISS ≥ 25 are more likely to undergo hysterectomy compared to repair. Gunshot injuries are more likely to undergo salpingectomy or oophorectomy compared to repair. Hypotension on arrival was not shown to be an independent risk factor for resection in PGT. Additionally, age ≥ 51 was not shown to be a risk factor; however, the sample size is likely too small to draw any definitive conclusions. Interestingly, operative intervention for all PGT patients was associated with a lower risk of mortality compared to patients managed non-operatively. Future prospective research to confirm our findings and elucidate other significant risk factors for trauma resection vs repair of the uterus, ovaries, and fallopian tubes appears warranted.
References
Harrison SD, Nghiem HV, Shy K. Uterine rupture with fetal death following blunt trauma. Am J Roentgenol 1995;165(6):1452. https://doi.org/10.2214/ajr.165.6.7484584.
Mattox KL, Goetzl L. Trauma in pregnancy. Crit Care Med 2005;33(10 Suppl):S385–S389.
Agrawal S, Nayak P, Mitra S, Agrawal A, Jain A, Singh V. Pelvic trauma in women of reproductive age. J Orthop Traumatol Rehabil. 2014;7(1):23–28. https://doi.org/10.4103/0975-7341.134007.
Mikos T, Papanicolaou A, Tsalikis T, Ioannidis E. Uterine prolapse after pelvic trauma: case report and literature review. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(7):881–884. https://doi.org/10.1007/s00192-008-0774-9.
Barach E, Martin G, Tomlanovich M, Nowak R, Littleton R. Blunt pelvic trauma with urethral injury in the female: a case report and review of the literature. J Emerg Med 1984;2(2):101–105.
Kuwabara K, Matsuda S, Imanaka Y, Fushimi K, Hashimoto H, Ishikawa KB, et al. Injury severity score, resource use, and outcome for trauma patients within a Japanese administrative database. J Trauma 2010;68(2):463–470. https://doi.org/10.1097/TA.0b013e3181a60275.
Harnod D, Chen R-J, Chang WH, Chang R-E, Chang C-H. Mortality factors in major trauma patients: nation-wide population-based research in Taiwan. Int J Gerontol. 2014;8(1):18–21.
Shaheen B, Shaheen G. Peripartum hysterectomy, frequency, risk factors and maternal outcome. Khyber Med Univ J. 2015;6(4):178–82.
Bouglé A, Harrois A, Duranteau J. Resuscitative strategies in traumatic hemorrhagic shock. Ann Intensive Care. 2013;3(1):1.
Kauvar DS, Wade CE. The epidemiology and modern management of traumatic hemorrhage: US and international perspectives. Crit Care. 2005;9(5):S1.
Surgeons ACo. National trauma data bank. American College of Surgeons, Chicago 2016.
Rocca WA, Shuster LT, Grossardt BR, Maraganore DM, Gostout BS, Geda YE, et al. Long-term effects of bilateral oophorectomy on brain aging: unanswered questions from the Mayo Clinic Cohort Study of oophorectomy and aging. 2009;5:39–48.
Rocca WA, Grossardt BR, de Andrade M, Malkasian GD, Melton LJ. 3rd. Survival patterns after oophorectomy in premenopausal women: a population-based cohort study. Lancet Oncol. 2006;7(10):821–828. https://doi.org/10.1016/s1470-2045(06)70869-5.
Rivera CM, Grossardt BR, Rhodes DJ, Brown RD Jr, Roger VL, Melton LJ III, et al. Increased cardiovascular mortality following early bilateral oophorectomy. Menopause (New York). 2009;16(1):15.
Burger HG, Hale GE, Robertson DM, Dennerstein L. A review of hormonal changes during the menopausal transition: focus on findings from the Melbourne Women’s Midlife Health Project. Hum Reprod Update. 2007;13(6):559–565. https://doi.org/10.1093/humupd/dmm020.
Kaunitz AM, Manson JE. Management of Menopausal Symptoms. Obstet Gynecol. 2015;126(4):859–876.
Sievert LL, Murphy L, Morrison LA, Reza AM, Brown DE. Age at menopause and determinants of hysterectomy and menopause in a multi-ethnic community: the Hilo Women’s Health Study. Maturitas. 2013;76(4):334–341.
Bhavnani V, Clarke A. Women awaiting hysterectomy: a qualitative study of issues involved in decisions about oophorectomy. BJOG Int J Obstet Gynaecol. 2003;110(2):168–174.
Rotondo MF, Schwab CW, McGonigal MD, Phillips GR, Fruchterman TM, Kauder DR, et al. ‘Damage control’: an approach for improved survival in exsanguinating penetrating abdominal injury. J Trauma Acute Care Surg. 1993;35(3):375–383.
Kashuk JL, Moore EE, Millikan JS, Moore JB. Major abdominal vascular trauma—a unified approach. J Trauma. 1982;22(8):672–679.
Feliciano DV, Mattox KL, Burch JM, Bitondo CG, Jordan GL. Jr. Packing for control of hepatic hemorrhage. J Trauma. 1986;26(8):738–743.
Rotondo MF, Zonies DH. The damage control sequence and underlying logic. Surg Clin N Am. 1997;77(4):761–777.
Bouras A-F, Truant S, Pruvot F-R. Management of blunt hepatic trauma. J Visc Surg. 2010;147(6):e351–e358.
Haan JM, Bochicchio GV, Kramer N, Scalea TM. Nonoperative management of blunt splenic injury: a 5-year experience. J Trauma Acute Care Surg. 2005;58(3):492–498.
Kim T, Shin JH, Kim J, Yoon HK, Ko GY, Gwon DI, et al. Management of bleeding uterine arteriovenous malformation with bilateral uterine artery embolization. Yonsei Med J. 2014;55(2):367–373. https://doi.org/10.3349/ymj.2014.55.2.367.
Lee SK, Carrillo EH, Rosenthal A, Sanchez R, Kiffin C, Davare DL. Acute care/trauma surgeon’s role in obstetrical/gynecologic emergencies (The OBCAT Alert). World J Emerg Med. 2016;7(4):274–277. https://doi.org/10.5847/wjem.j.1920-8642.2016.04.006.
Jain V, Chari R, Maslovitz S, Farine D, Bujold E, Gagnon R, et al. Guidelines for the management of a pregnant trauma patient. J Obstet Gynaecol Can. 2015;37(6):553–574.
Elias M. Rupture of the pregnant uterus by external violence. Lancet. 1950;2(6624):253–254.
Quast DC, Jordan GL Jr. Traumatic wounds of the female reproductive organs. J Trauma. 1964;4:839–844.
Stone NN, Ances I, Brotman S. Gynecologic injury in the nongravid female during blunt abdominal trauma. J Trauma. 1984;24(7):626–627.
Frassica FJ, Inoue N, Virolainen P, Chao EY, (Eds) Skeletal system: biomechanical concepts and relationships to normal and abnormal conditions. Seminars in nuclear medicine; 1997; Elsevier, Amsterdam.
DiGiacomo JC, Schwah CW, Rotondo MF, Angood PA, McGonigal MD, Kauder DR, et al. Gluteal gunshot wounds: who warrants exploration? J Trauma Acute Care Surg. 1994;37(4):622–628.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Areg Grigorian, Victor Joe, Patrick T. Delaplain, Sebastian Schubl, Bel Barker, Viktor Gabriel, Austin R. Dosch, Cristobal Barrios and Jeffry Nahmias declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Grigorian, A., Joe, V., Delaplain, P.T. et al. Risk of hysterectomy and salpingectomy or oophorectomy compared to repair after pelvic gynecologic trauma. Eur J Trauma Emerg Surg 45, 403–410 (2019). https://doi.org/10.1007/s00068-018-0936-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-018-0936-5