Abstract
Background
This study evaluated the impact of IC on the optimization of nutritional support and the achievement of +NB in patients with TBI.
Materials and methods
27 patients (GCS ≤ 8), treated with a 5-day multimodality monitoring and goal-directed therapy protocol, received enteral nutrition on day 1 followed by IC on days 3 and 5 and assessment of NB on day 7. In the first cohort (n = 11), no adjustment in kcal was made. In the second cohort (n = 16), nutrition was targeted to an RQ of 0.83 by day 3. The first cohort was analyzed with respect to NB status; the second cohort was compared to patients with (−) and +NB of the first cohort. Data (mean ± SD) were analyzed with unpaired t test, and Chi square and Fisher exact tests.
Results
4/11(36 %) patients in the first cohort had +NB. The predicted mortality by TRISS, substrate utilization, and RQ was significantly lower compared to the second cohort. The mortality predicted by the CrasH model did not differ between the two cohorts. A RQ of 0.74 was associated with the preferential use of fat and protein and −NB, whereas a RQ of 0.84 favored utilization of carbohydrates and +NB. All patients whose kcal intake was adjusted based on the RQ on day 3 reached a +NB by day 7.
Conclusion
An increase in kcal ≥25 % in patients with a RQ < 0.83 on day 3 improves substrate utilization, decreases protein utilization and optimizes the achievement of +NB by day 7.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Severe traumatic brain injury (sTBI) remains a significant public health issue. There are 1.4 million cases of TBI annually in the United States resulting in 270,000 hospitalizations and 52,000 deaths each year, with approximately 85 % of deaths occurring within the first 2 weeks of the injury [1, 2]. The consequences and burden of the care of TBI patients present specific challenges to the health care system making TBI one of the most disabling injuries with an associated cost greater than 100 billion dollars each year. Currently, the management of patients with sTBI is centered on the prevention of secondary brain injury by preventing the occurrence of hypoxia and hypotension and by maintaining an adequate cerebral perfusion pressure (CPP) with the optimization of the mean arterial blood pressure and the intracranial pressure (ICP) [3].
Patients with sTBI are hypermetabolic and remain catabolic even when given an adequate number of calories/kg and protein adjusted to their increased metabolic rate. Severe TBI triggers hypermetabolism and catabolism severely impairing nitrogen retention. The hypermetabolism is the result of a disproportionately higher pro-inflammatory cytokine production (e.g., tumor necrosis factor-α, interleukin-1 and interleukin-6) that is associated with increased production and release of counter-regulatory hormones, such as cortisol, glucagon, and catecholamines. This process causes increased systemic and cerebral energy requirements, even in sedated and paralyzed patients. Studies that have measured resting energy expenditure (REE) by indirect calorimetry (IC) have demonstrated that patients with sTBI have metabolic rates ranging from 120 to 250 % above predicted REE [4]. Variables that may contribute to this wide range of metabolic rates include the depth and duration of sedation, the use of neuromuscular blocking agents, the implementation of burst suppression therapy, the presence of hyperthermia, the use of normothermic protocols, and the use of beta blockade to modulate metabolic rates.
Despite the fact that patients with sTBI are known to be hypermetabolic, much less emphasis is placed on the early achievement of adequate nutritional support as opposed to the maintenance of adequate cerebral oxygen dynamics variables. In fact, based on two small randomized trials, the most recent guidelines for the management of sTBI recommend that the patients’ nutritional requirements should be reached by the end of the first week after TBI [3, 5, 6].
However, there is no agreement on the optimal timing or route of feeding [7, 8]. Current nutrition guidelines and formulas used to estimate calorie requirements for patients with sTBI do not take into consideration the impact of the many variables that may affect the metabolic rate of these patients and, hence, may lead to underfeeding and failure to achieve early a positive nitrogen balance (+NB). In view of the potential impact of achieving a +NB by day seven on the outcome of patients with sTBI, we investigated whether the use of IC offers advantages over the common formulas used to provide nutritional support to patients with sTBI from the standpoint of the achievement of +NB.
Materials and methods
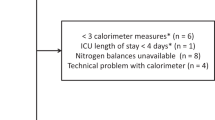
This study includes a retrospective review of prospectively acquired data on 27 patients with sTBI, defined by a Glasgow coma scale (GCS) ≤8, admitted to the Trauma Surgery Service from January, 2011 to November, 2013. The patients were treated in the trauma intensive care unit where they received enteral nutrition. The nutritional support protocol included initiation of peptide-based enteral nutrition solution (Pivot 1.5 Cal, Abbot Nutrition, Columbus, OH) either via post-pyloric placement (distal duodenum) of a Cortrak feeding tube (Corpack Med Systems, Buffalo Grove, IL, USA), with radiological confirmation of placement or via gastric feeding, at target goal (without titrating to goal) within 24 h of admission to the TICU, upon successful completion of the resuscitation phase that included airway management, respiratory and circulatory support. Calories received by propofol infusion were included in the calculation of calories when required.
Pivot®’s composition includes 45 % carbohydrate, 30 % fat and 25 % protein in addition to immune-enhancing micronutrients which include N3-eicosopentanoic acid, docosahexaenoic acid and arginine with a non-protein calorie/nitrogen ratio 75:1. All patients received IV metoclopramide 10 mg every 6 h to enhance gastrointestinal motility started before the initiation of enteral feeding and continued throughout the enteral feeding period. Patients received continuous enteral nutrition targeted to achieve 140 % of their REE (cREE) as calculated with the Harris–Benedict equation as suggested by the Trauma Brain Foundation guidelines [3]. Gastrointestinal intolerance was defined by a gastric residual volume ≥500 mL measured every 4 h. All patients had their head maintained at 45° throughout the multimodality monitoring and goal-directed therapy protocol used for the treatment of patients with sTBI.
The cREE was calculated with the following formulae:
Protein requirements were calculated at 1.5–2.0 g/kg/day. REE, substrate utilization and NB were measured using indirect calorimetry (IC) and 24-h urine urea nitrogen (UUN) collections, respectively. IC was performed on day 7 in the initial cohort of patients and on days 3 and 5 while patients were receiving continuous enteral nutrition at the goal rate. IC measurements were performed utilizing a VIASYS® Vmax™ 29 Encore Metabolic Cart (CareFusion, San Diego, CA) to obtain continuous measurements of inspired and expired oxygen, carbon dioxide, nitrogen and expired minute ventilation for a total of 30 min. These measurements were used to calculate the REE (mREE) with the Weir equation:
Equipment calibration was performed each day before IC readings.
All patients were treated with a 5-day protocol that included maintenance of normothermia (37° Celsius) with dry water immersion methodology (Arctic Sun ®5000, Medivanz, Louisville, CO), maintenance of CPP ≥ 60 mm Hg to keep brain oxygen tension (PbtO2) ≥20 mm Hg and bi-frontal Near Infrared Spectroscopy (NIRS) values ≥60 %, and ICP ≤ 20 mm Hg. All patients received sedation with midazolam and propofol at the dose necessary to have the patient synchronized with the ventilator. Intravenous acetaminophen at a dose of 1000 mg every 6 h was administered to all patients. To prevent shivering, buspirone 30 mg via the NGT every 8 h and skin warming with surface counter warming (Bear Hugger, 3 M™ Bair Hugger™ Therapy, St. Paul, MN, USA) set a 43 °C was used in all patients. The minute ventilation (Ve) was adjusted to maintain the PCO2 between 32 and 35 mm Hg. Norepinephrine was used, as needed, to maintain the target CPP, PbtO2, and NIRS’ values. Osmotherapy (3 % saline) was used at a rate of 40–60 ml/h as first-line therapy in patients with ICP > 20 mm Hg. Burst suppression with continuous electroencephalogram monitoring was used in patients whose ICP could not be controlled with osmotherapy using a combination of midazolam and propofol infusion a rate of 15 mg/h and 100 µg/kg/min, respectively. Decompressive craniectomy was used as rescue therapy in patients with intractable elevations of the ICP whose increased ICP was the result of mass effect.
The following parameters remained constant in all patients during IC measurements: Ve, level of sedation, vasoactive drug dosage, and temperature. Urine was collected for 24 h to measure UUN. UUN in grams in 24 h was used to calculate the percent of substrate utilization (PSU) by entering these data in the Vmax Encore Metabolic Cart. Nitrogen balance was calculated using the following equation:
Nutritional support in kcal/kg was adjusted in the second cohort of the study following the IC measurements on day three, if the RQ was <0.83. Exclusion criteria included age <14 years, hemodynamic instability, the use of fraction of inspired oxygen (FI02) ≥ 60 %, and Hgb/Hct ≤ 9.0 g/dL and 27 %, respectively.
Data acquired included demographics, weight, GCS and injury severity score (ISS), abbreviated injury score of head (AIS-H), hemodynamic and cerebrospinal fluid dynamics data, temperature, Kcal/kg received, mREE and cREE (Kcal/kg), Ve, PSU, RQ, and nitrogen balance (NB).
Study design
The study is a retrospective analysis of a prospective observational study and a preliminary assessment of the feasibility of intervention based on an intervention cohort group of patients. The initial observation cohort included 11 patients who underwent IC measurements of their REE on day seven without any adjustment of their energy intake based on the results of the mREE and RQ. This cohort underwent measurement of NB on day 7. Following the analysis of this cohort of patients stratified by NB status, namely, positive (n = 4) and negative NB (n = 7), and normalization of the kcal/kg to the REE in the group with RQ < 0.83, we concluded that an RQ between 0.7 and 0.82 indicated the need to increase the kilocalories by 25 %. Therefore, the subsequent intervention cohort of 16 patients had their calories increased by 25 %, if day 3 IC showed an RQ < 0.83. This group underwent repeat IC on day 5 and further adjustment of kilocalories intake, if needed, based on the target RQ. The intervention cohort underwent measurement of NB on day 3 and 5.
The 14-day predicted mortality was calculated using the web-based CT CrasH model (“basic” model plus CT findings), which uses a combination of four demographic and clinical variables, namely age, GCS, pupil reactivity and the presence of major extra-cranial injuries and the CT presence of petechial hemorrhages, obliteration of the third ventricle or basal cisterns, subarachnoid bleeding, midline shift and non-evacuated hematoma [9].
Statistical analysis
For the purpose of statistical analysis, four comparisons were made. The first included the observation cohort of patients stratified by NB status (Tables 1, 2). The second comparison included the seven patients with negative NB of the first cohort of the study with the 16 patients of the second intervention cohort (Tables 3, 4). The third comparison included the four patients with +NB in the first cohort of the study with the patients in the second cohort to assess differences (Tables 6, 7).
A hypermetabolic state was defined as a metabolic index mREE/cREE > 1. Data are presented as mean ± standard deviation (SD). Parametric data were compared with unpaired Student t test, whereas nonparametric data were compared with Fisher exact or Chi square tests as applicable. Statistical significance was accepted to correspond to a p value < 0.05. The study was approved by the Institutional Research Board.
Results
Successful jejunal placement of the feeding tube was achieved in 20/27 (74 %) patients.
There was no difference in the number of patients who received jejunal feeding as opposed to gastric feeding in the two study cohorts: 8/11 (73 %) in first cohort as opposed to 12/16 (75 %) in the second cohort (p > 0.05). All patients, independent of feeding route, tolerated enteral feeding at the calculated target rate from the onset of feeding started within the first 24 h of injury.
Shown in Table 1 are the demographic, GCS, ISS scores and predicted and actual mortality of the patients in the first cohort of the study stratified by NB status. Patients with negative NB did not differ from those with +NB with respect to age, GCS, AIS(H), ISS score, temperature, minute ventilation, predicted mortality by both the TRISS and CrasH models and actual mortality.
There was no difference between the patients with negative NB and +NB with respect to the dose of midazolam, propofol, fentanyl, norepinephrine, mannitol from the IV acetoaminophen and the use of burst suppression therapy: 5 ± 2 vs. 6 ± 4 mg/h, 50 ± 25 vs. 75 ± 25 mcg/kg/min, 100 ± 25 vs.100 ± 50 mcg/h, 5/7 vs. 3/4 patients at mean of 12 ± 8 vs. 15 ± 5 mcg/min, 11.4 ± 5.6 vs. 11.4 ± 3.8 g/day, 0/7 vs. 0/4 burst suppression, respectively.
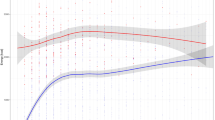
However, patients with negative NB had a lower RQ compared to those with +NB, 0.74 ± 0.05 vs. 0.84 ± 0.01, p = 0.003. The average ratio of energy intake to mREE was higher in patients with +NB (1.34 ± 0.31; n = 4) than in patients with negative nitrogen balance (0.96 ± 0.21; n = 7; p = 0.03). Patients with +NB in the first cohort of the study had an average intake of energy ≥25 % mREE. Furthermore, they had a statistically significant difference in their utilization of substrate; namely, they used preferentially fat and proteins as opposed to carbohydrates (Table 2). Patients with negative NB had a higher metabolic index (mREE/cREE) compared to patients with +NB 1.03 ± 0.22 vs. 0.74 ± 0.11, respectively, p = 0.03.
Shown in Table 3 is the comparison of the demographics, GCS, ISS, predicted and actual mortality of the patients with negative NB of the first cohort of the study and all patients in the second cohort of the study. Patients did not differ with respect to GCS, AIS(H), and ISS scores. Predicted and actual mortality were also not significantly different between the two groups. However, patients in the second cohort were older and had a higher predicted mortality by TRISS. They also had a significantly lower mREE compared to patients with negative NB, 24 ± 3 versus 32 ± 8, respectively (p < 0.05). Patients with negative NB had a lower RQ compared to those with +NB, 0.74 ± 0.05 versus 0.84 ± 0.09 (p = 0.01); of note, they used preferentially fat and proteins instead of carbohydrates (Table 4). The average ratio of energy intake to mREE was higher in 16 patients in the intervention group (1.12 ± 0.12) than in patients with negative nitrogen balance (0.96 ± 0.21; n = 7; p = 0.03). Patients with +NB in the intervention cohort of the study had an average intake of energy 11 % higher than the mREE.
Five of 16 (31 %) patients in the second cohort of the study required a 25 % increase in kcal following day 3 RQ measurements. One patient required further adjustment following IC on day 5. The increased number of kilocalories yielded a statistically significant increase in the RQ by day 5, 0.71 ± 0.06 to 0.85 ± 0.03 RQ day 3 vs. 5, respectively (p < 0.001), as well as a decrease in UUN from day 3 to day 5 (Table 5). Of note, these five patients did not differ from the remaining 11 patients in the intervention group with respect to age, gender, GCS, ISS, AIS(H) and PM: 46 ± 19 vs. 50 ± 17 years, 2/3 and 4/7 female/male, 5 ± 2 vs. 4 ± 1, 25 ± 8 vs. 27 ± 7, 4 ± 1 vs. 5 ± 1, and 58 ± 31 vs. 24 ± 18, respectively. However, two of the five patients had decompressive craniectomy within 2 h on injury as opposed to no craniotomy or craniectomy in the other 11 patients.
Patients with negative NB had a higher metabolic index compared to the patients with positive NB, 1.03 ± 0.22 versus 0.88, respectively. Furthermore, patients with negative NB had a statistically significant difference in their utilization of substrate; namely, they used preferentially fat and proteins as opposed to carbohydrates. Of note, as shown in Table 4, the +NB group who had their kcal adjusted by RQ on day 3 and 5, if necessary, had an even higher rate of utilization of carbohydrates when compared to the +NB patients in the first cohort of the study 52 ± 17 vs. 35 ± 10, respectively, p = 0.02. There was no difference in the mortality rate between the negative NB and +NB groups, 2/7 (28.6 %) vs. 2/16 (12.5 %), respectively (p = 0.56) (Tables 6, 7).
Discussion
The current management of patients with sTBI continues to be focused on the prevention of secondary brain injury by avoiding periods of hypoxia and hypotension and by maintaining CPP, ICP, PbtO2 within specific target values for a period of three to 5 days after the injury [10]. Nutrition is not yet viewed as an adjunctive treatment modality that can be used in conjunction with primary surgical and non-surgical treatment modalities of sTBI to decrease mortality and improve the long-term functional recovery of these patients. Patients with sTBI are hypermetabolic and remain catabolic even when given an adequate number of Kcal/kg and protein adjusted to their increased metabolic rate. Well-nourished patients with sTBI may have energy requirements approaching 50 kcal/kg/day during the first week of injury [11]. This level of energy requirement needed to maintain lean body mass and immune function is unlikely to be met following the nutritional recommendation by the Brain Trauma Foundation.
A 2008 study by the Brain Trauma Foundation using data from 22 centers on the effect of feeding on outcome of patients with TBI found that mortality improved for each 10 kcal/kg/day increase in intake up to 25 kcal/kg/day. Furthermore, it found that death was twice as likely for patients not fed within 5 days and four times more likely if not fed within 7 days of TBI [12]. However, identifying the ideal timing of initiation and the amount of nutrition required to meet the energy expenditures of well-nourished patients with sTBI remains problematic using the conventional predictive nutritional formulas. The nutritional support provided to patients with sTBI continues to be based on the BTF guidelines and is gaged by nutritional predictive formulas that do not take into consideration the many variables affecting the metabolic rate of these patients, hence, potentially leading to underfeeding. While permissive underfeeding may have the theoretical benefits of improved glycemic control and of a down-regulated inflammatory response, it has not been shown to be associated with improved outcome [13, 14].
In contrast, two Cochrane reviews have provided strong evidence for improvement in mortality and neurologic outcome from early aggressive feeding in sTBI [15, 16]. In view of the potential impact of achieving adequate nutritional support and a +NB by day seven on the outcome of patients with sTBI, we investigated whether the use of IC could offer advantages over the common predictive nutritional formulas to reach early a +NB.
Several findings from our study can be used to optimize the nutritional support of patients with sTBI. First, the results of our study do not support the presence of the upper gastrointestinal intolerance reported by others during the first 2 weeks after traumatic brain injury [17, 18]. The majority of our patients tolerated enteral feeding, which was started within 24 h of injury, upon successful completion of the resuscitation phase that included airway management, respiratory and circulatory support and craniotomy or craniectomy, when indicated, at the goal rate necessary to provide the number of kilocalories based on 140 % of the predicted energy expenditure by the Harris–Benedict equation whether feeding was provided in the stomach or in the distal duodenum or proximal jejunum. However, we must point out that we elected to define gastrointestinal intolerance using a higher gastric residual volume (≥500 mL) as opposed to the more conservative gastric residual volume of 200 mL used by other authors [19].
Second, in the absence of adjustment of the number of kilocalories provided to the patients based on the measured RQ, 64 % (7/11) of patients in the first cohort of the study had a negative NB. Since all patients with negative NB in the first cohort received and tolerated enteral nutrition at the target rate required to meet the predicted energy expenditure, we can state that underfeeding was not caused by gastrointestinal intolerance which has been identified as the cause of underfeeding in other studies [20]. However, the lower RQ with the preferential utilization of fat and protein is suggestive of underfeeding probably secondary to an increased metabolic index from cytokines activation. Since there was no difference in the ISS between the patients with negative and +NB, it is plausible that the patterns on injury rather than the ISS may explain the increased energy needs in the patients with negative NB. The data on substrate utilization in this group show a higher protein and fat oxidation in patients with a negative nitrogen balance with a decrease in protein and fat oxidation with higher energy intake, suggesting that the amount of energy intake delivered above the mREE may affect protein metabolism and, ultimately, nitrogen balance.
Five of 16 (31 %) of the patients in the intervention cohort of the study would have had a negative NB by day seven, if correction of the kilocalories provided to these patients had not been done based on the result of the IC on day 3. Therefore, we can postulate based on our data that in the absence of IC data, 44 % of patients with sTBI undergoing enteral nutrition via the gastric or jejunal route based on the REE estimated with the Harris–Benedict Equation may be at risk of underfeeding leading to a negative NB by day seven. The five patients who had an increase in kcal/kg had an improvement in nitrogen balance. The increase in energy intake increased the average ratio on energy intake to mREE from 1 to 1.25 ± 0.02.
The comparison of patients with +NB in the first cohort of the study with patients in the second cohort showed that the average ratio of energy intake to mREE was lower in the 16 patients in the second cohort compared to the four patients with +NB in the first cohort. Additionally, patients with +NB in the intervention cohort had an average intake of energy 11 % higher than the mREE compared to >25 % in the four patients with +NB in the observation cohort of the study. Furthermore, patients in the second cohort used more CHO than fat to achieve a +NB. The reason why patients in the second cohort of the study achieved a +NB with a lower average ratio of energy intake to mREE can be ascribed to two likely factors, namely the significantly older age and lower temperature in the patients in this group, both of which could account for difference. The reported change in energy expenditure per degree Celsius is 11 %. These observation suggest that an RQ on day 3 < 0.83 may be used as a surrogate marker for negative nitrogen balance and the need to increase the ratio of energy intake to mREE since there is a strong correlation between the RQ and the NB (r 2 = 0.54, p = 0.002).
Limitations
Our study has the following limitations. First, since we measured severity of injury using the ISS, we did not identify the impact of specific injury patterns (long bones versus chest or abdominal injuries) on the energy requirements of the patients with RQ < 0.83. Second, we did not continue indirect calorimetry and nitrogen balance measurements past the first 7 days of traumatic brain injury; therefore, we have limited information regarding the duration of the hypermetabolism and the optimization of the nutritional support by IC in a later phase of sTBI. Third, we did not compare the Harris–Benedict formula to the other formulas used to estimate REE, such as the Penn State equation, the Swinamer and/or the Ireton–Jones formula from the standpoint of accuracy [21–23]. Fourth, since our study was limited to evaluating the impact of IC on the early achievement of NB, we were unable to draw any conclusion with respect to the impact of the early achievement on nitrogen balance using IC on days of ventilation, ICU stay, overall morbidity, as well as the early and late outcome of patients with sTBI. Fifth, due to the very small number of patients studied, we believe that our conclusions should not be over-interpreted from the standpoint of generalizability but should be viewed as a preliminary assessment of a potential intervention, namely the use of IC-guided nutritional support to achieve early positive nitrogen balance in patients with sTBI.
Conclusions
We believe based on the results of our study that patients with severe TBI should ideally receive nutritional support within the first 24 h on injury upon completion of the resuscitation phase, starting immediately at the goal rate of infusion and adjusting the amount of kilocalories based on the results of the indirect calorimetry done on days 3 and 5 to achieve early a positive nitrogen balance. This nutritional support strategy using IC to optimize nutritional support is critical to limiting the intensity of the inflammatory response associated with sTBI and it may improve the early and late outcome of patients with sTBI.
References
Bulger EM, Nathens AB, Rivara FP, Moore M, MacKenzie EJ, Jurkovich GJ. Management of severe head injury: institutional variations in care and effect on outcome. Crit Care Med. 2002;30:1870–6.
Faul M, Xu L, Wald MM, Coronado VG. Traumatic brain injury in the United States: Emergency department visits, hospitalizations and deaths 2002–2006. Atlanta, GA: Centers for Disease Control and Prevention.
Bullock R, Chesnut RM, Clifton G, et al. Guidelines for the management of severe traumatic brain injury. Brain Trauma Foundation. J Neurotrauma. 2000;17:449–554.
Raurich JM, Ibanez J. Metabolic rate in severe head trauma. J Parenteral Enteral Nutr. 1994;18(6):521–4.
Rapp RP, Young B, Twyman D, et al. The favorable effect of early parenteral feeding on survival in head-injured patients. J Neurosurg. 1983;58:906–12.
Young B, Ott L, Twyman D, et al. The effect of nutritional support on outcome from severe head injury. J Neurosurg. 1987;67:668–76.
Borzotta AP, Pennings J, Papasadero B, et al. Enteral versus parentera; nutrition after severe closed head injury. J Trauma. 1994;37:459–68.
Taylor SJ, Fettes SB, Jewkes C, Nelson RJ. Prospective, randomized, controlled trial to determine the effect of early enhanced enteral nutrition on clinical outcome in mechanically ventilated patients suffering head injury. Crit Care Med. 1999;27:2525–31.
Medical Research Council CRASH Trial Collaborators. Predicting outcome after traumatic brain injury: practical prognostic models based on large cohort of international patients. BMJ. 2008;336:425–9.
Bratton SL, Chestnut RM, Ghajar J, et al. Guidelines for the management of severe traumatic brain injury. XII. Nutrition. J Neurotrauma. 2007;24:S77–82.
Erdman J, Oria M, Pillsbury L, Editors; Committee on Nutrition, Trauma and the Brain; Institute of Medicine. Nutrition and Traumatic Brain Injury: Improving Acute and Subacute Health Outcomes in Military Personnel. http://www.nap.edu/catalog.php?record_id=13121.
Hart R, Gerber LM, Ni Q, Ghajar J. Effect of early nutrition on deaths due to severe traumatic brain injury. J Neurosurg. 2008;109:50–6.
Rovlias A, Kotsou S. The influence of hyperglycemia on neurological outcome in patients with severe head injury. Neurosurgery. 2000;46:335–43.
Burke P, Young L, Bistrian B. Metabolic vs. nutrition support: a hypothesis. J Parenter Enteral Nutr. 2010;34:546–8.
Perel P, Yanagawa T, Bunn F, Roberts I, Wentz R, Pierro A. Nutritional support for head-injured patients. Cochrane Database Syst Rev. 2006;3:CD001530.
Yanagawa T, Bunn F, Roberts I, Wentz R, Pierro A. Nutritional support for head-injured patients. Cochrane Database Syst Rev. 2002;3:CD001530.
Tan M, Zhu JC, Yin HH. Enteral nutrition in patients with severe traumatic brain injury: reasons for intolerance and medical management. Br J Neurosurg. 2001;25(1):2–8.
Pinto TF, Rocha R, Paula CA, de Jesus RP. Tolerance to enteral nutrition therapy in traumatic brain injury patients. Brain Inj. 2012;26(9):1113–7.
Dickerson RN, Mitchell JN, Morgan LM, et al. Disparate response to metoclopramide therapy for gastric feeding intolerance in trauma patients with and without traumatic brain injury. J Parenter Enteral Nutr. 2009;33(6):645–55.
Griffiths RD. Parenteral nutrition in adults with a functional gastrointestinal tract. Lancet. 2006;368:1868–9.
MacDonald A, Hildebrandt L. Comparison of formulaic equations to determine energy expenditure in the critically ill patient. Nutrition. 2003;19(3):233–9.
Swinamer DL, Grace MG, Hamilton SM, Jones RL, Roberts P, King G. Predictive equation for assessing energy expenditure in mechanically ventilated critically ill patients. Crit Care Med. 1990;18(6):657–61.
Ireton-Jones C. Improved equations for predicting energy expenditure in patients: the Ireton-Jones Equations. Nutr Clin Pract. 2002;17(1):29–31.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Jacqueline Maxwell, Carlo Gwardschaladse, Gary Lombardo, Patrizio Petrone, Anthony Policastro, Dimitriy Karev, Kartik Prabhakaran, Alejandro Betancourt, and Corrado P. Marini declare that they have no conflict of interest.
Ethical approval
The study was designed as a retrospective study, and approved by the Institutional Review Board (IRB) of the New York Medical College. No informed consent was required.
Rights and permissions
About this article
Cite this article
Maxwell, J., Gwardschaladse, C., Lombardo, G. et al. The impact of measurement of respiratory quotient by indirect calorimetry on the achievement of nitrogen balance in patients with severe traumatic brain injury. Eur J Trauma Emerg Surg 43, 775–782 (2017). https://doi.org/10.1007/s00068-016-0724-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-016-0724-z