Abstract
Purpose
Lactate is a biomarker for hypoperfusion and subsequent resuscitation in trauma. It is also a predictor of mortality, but few studies have correlated lactate levels with relevant morbidities after trauma.
Methods
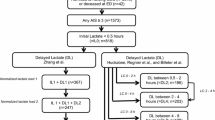
A retrospective review was performed of severely injured trauma patients entered into the Trauma Registry of the German Society for Trauma Surgery (TR-DGU) between 2002 and 2008. Adults requiring intensive care were categorized into two groups: lactate and no lactate. The lactate group had three subgroups: normal, elevated, and high lactate. Mean multiple organ failure (MOF) rates and composite endpoint of time (days) to complete organ failure resolution (CTCOFR) for 14 and 21 days and ventilator-free days (VFD) were compared, as well as other endpoints.
Results
We analyzed 2,949 patients, of which 1,199 had lactate measurements. The percentage of patients with MOF increased in each higher lactate subgroup (p < 0.001), as did the mean CTCOFR14 and CTCOFR21 scores (p < 0.001 and < 0.001, respectively). Conversely, the mean VFD decreased in each higher lactate subgroup (p < 0.001). Thus, patients in the elevated and high lactate subgroups had greater MOF rates; required more days, on average, to resolve organ failure; and required more days of ventilator support than patients in the normal lactate subgroup.
Conclusion
Elevated blood lactate levels from trauma were closely correlated with worse outcomes. Thus, lactate shows promise as a biomarker for resuscitation as well as a predictor of mortality. Furthermore, this study supports its use in critical care trials as an outcome measure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Trauma is a growing worldwide issue. The World Health Organization (WHO) estimates that 5.8 million people die each year as a result of injury [1]. In 2004, 78.8 million people suffered injuries due to road traffic accidents, falls, and violence [2]. Hemorrhage accounts for 30–40 % of all deaths after trauma [3]. The majority of remaining trauma mortality is due to brain injury, the mortality rates of which remain largely unchanged, despite current treatment. Therefore, hemorrhage and its consequences are the most productive current targets for novel treatment strategies.
The most serious global consequences of hemorrhage are the development of single organ failure and multiple organ failure (MOF) [4]. Yet, simple biomarkers for organ failure outcomes are not available [4, 5].
Lactate has been used clinically to guide resuscitation in trauma and surgical critical care of patients for decades. Lactate is quick and easy to measure and has repeatedly been shown to be a good predictor of mortality. Husain et al. [6] demonstrated that initial lactate concentrations separate survivors from nonsurvivors in surgical patients admitted to the intensive care unit (ICU). Elevated lactate levels, indicative of hypoperfusion and anaerobic metabolism in tissues and critical organs, track oxygen debt and the severity of hemorrhage shock [7]. Persistent oxygen deficit, and subsequent lactic acidosis, in critical care patients has been shown to correlate with poor outcomes and increased mortality [8]. In severely injured trauma patients, Claridge et al. [9] showed that lactic acidosis persisting for more than 12 h was associated with post-injury infection and prolonged hospital stays. Similar findings were described already in the early 1990s [10, 11].
Further study is needed, however, to define the correlation between elevated lactate concentrations and morbidity. We, therefore, performed a retrospective analysis of the Trauma Registry of the German Society for Trauma Surgery (TR-DGU) [12, 13] to validate the predictive value of lactic acidosis for the development of clinically relevant morbidity, as expressed by a composite endpoint of time (days) to complete organ failure resolution for 14 days (CTCOFR14), CTCOFR for 21 days (CTCOFR21) [14], and ventilator-free days (VFD) [15].
The TR-DGU is an anonymous, voluntary, standardized, prospective registry of injured patients founded to improve the quality of trauma care in Germany. Between 1993 and 2008, data were entered from 42,248 severely injured trauma patients admitted to 166 hospitals.
Materials and methods
Patients
The primary inclusion criterion for enrolling patients into this retrospective study was the potential need for intensive care in adults sustaining major injury between 2002 and 2008. Patients documented before 2002 were excluded due to a different mode of data collection and the intention to have a more contemporary dataset with current treatment modalities. Cases involving preadmission deaths, burns, poisoning, and minor injuries were also excluded; thus, patients had Injury Severity Scores (ISS) of at least 9 points, were between 16 and 80 years of age, and were treated in the ICU during their hospitalization. This last requirement excluded patients who died shortly after hospital admission. Severe head injuries, defined as an Abbreviated Injury Scale (AIS) score of 4 or more, were excluded from analysis, since severe brain injuries can have a major confounding effect on organ failure endpoints that are driven by the need for mechanical ventilation in association with airway control. In addition, patients had to have a relevant blood loss, defined as bleeding that required the administration of at least one unit of packed red blood cells (pRBC). Ethical approval and informed consent were not required for this retrospective review of the registry’s anonymous data.
Lactate categories
Since the documentation of initial lactate values is incomplete in the TR-DGU, patients with and without documented lactate values were categorized into two groups: lactate and no lactate. Patients in the lactate group were further categorized into three subgroups based on their initial lactate levels: normal lactate (<2.2 mmol/L), elevated lactate (2.2–5.0 mmol/L), and high lactate (>5.0 mmol/L).
Data collection
The data collection for each patient included four consecutive phases of acute trauma care: (A) preclinical phase, with mechanism of injury, initial physiology, first therapy, neurological signs, and rescue time; (B) emergency room, with physiology, laboratory findings, suspected pattern of injury, therapy, and time sequence of diagnostics; (C) ICU, with status on admission, organ failure, sepsis, and duration of ventilation; and (D) final outcome, with hospital stay, survival, complete list of injuries, and operative procedures. Injuries were coded according to the AIS, version 1990 with 1998 update. The documentation was continued until the patient’s death or discharge from hospital. Data collection was completed anonymously, as part of the legally required activities of participating hospitals for external quality assessment; thus, no informed consent was required.
Parameters assessed
The outcome descriptors analyzed in this study were as follows: MOF rates, CTCOFR14, CTCOFR21, VFD, hospital mortality, 24-h mortality, days intubated, length of stay (LOS) in the ICU, and LOS in hospital. The following parameters were also assessed: age, sex, type of trauma, length of preclinical time (i.e., time from injury to hospital arrival), volume of preclinical fluids infused, presence of shock on admission (i.e., systolic blood pressure ≤90 mmHg), and the number of pRBC and fresh frozen plasma (FFP) units infused.
CTCOFR14 was based on the first 14 days of treatment in the hospital. If the patient survived the first 14 days after trauma, their CTCOFR14 corresponded to the number of days they experienced unresolved organ failure for the cardiovascular, respiratory, and renal systems during this period. If a patient’s organ failure was not resolved within the first 14 days, the CTCOFR14 was automatically set to 15. Patients who died within the first 14 days after admission received 16 points, by definition. Thus, the CTCOFR14 values ranged from 0 to 16, where lower scores represent a favorable outcome. Similarly, the CTCOFR21 was calculated for a period of 21 days, and the values ranged from 0 to 23.
For the purposes of determining the number of days patients experienced organ failure, cardiovascular failure was defined as 3–4 points in the Sepsis-related Organ Failure Assessment (SOFA) score [13]. This corresponds to the use of catecholamines in relevant doses. Renal failure was defined as the need for dialysis or hemofiltration. Respiratory failure was defined as the need for mechanical ventilation. The TR-DGU does not document organ failure in a day-by day manner; therefore, only cumulative days are available for defining organ failure and, for this analysis, we assume that the periods of organ failure and ventilation occurred on admission. Thus, the maximum number of days for the three above-mentioned organ failure definitions were used, and not the sum of days.
VFD were calculated as the number of days that patients did not require mechanical ventilation within the first 30 days after trauma. Nonsurvivors automatically received the worst value, zero.
Statistics
Categorical variables were presented as the number of cases and percentages; continuous variables were presented as mean ± standard deviation (SD). Pearson’s correlation coefficient was calculated for initial lactate, ISS, pRBC, and FFP values. Differences between the lactate and no lactate groups were evaluated using a Chi-square test for categorical variables, and a t-test for continuous variables. Within the lactate group, the three subgroups were evaluated with the Chi-square test for trend or analysis of variance (ANOVA). A p-value <0.05 was considered to be statistically significant. However, due to the multiplicity of statistical comparisons, the risk of arbitrary findings was increased, thus, p-values should be interpreted cautiously. Besides statistical significance, the clinical relevance of the observed differences always needs to be considered, especially in studies with large sample sizes.
All statistical analyses were performed using SPSS/PASW version 18 (IBM Corp., Somers, NY).
Results
This review of the TR-DGU database yielded 26,083 trauma patients admitted to hospitals between 2002 and 2008. Of these, 17,998 met the ISS, age, and ICU criteria. However, 15,049 of these patients were excluded due to severe head injuries (n = 1,640) or the lack of receiving a blood transfusion (n = 13,409). Therefore, 2,949 of these severely injured patients were included for analysis in this study.
Among these 2,949 patients, 1,199 (40.7 %) had valid lactate measurements on hospital admission (lactate group).
There was no clinically significant difference between the lactate and the no lactate groups in terms of demographics, injury description, or initial treatment. A high percentage of cases (>90 %) involved blunt trauma, and the percentages were consistent across the study groups. The only statistically significant differences between the two main groups were limited to preclinical times and volume of preclinical crystalloids infused, with the no lactate group having a shorter preclinical time (4 min) and receiving a lower volume of crystalloids (74 mL).
Considering the lactate subgroups, patients in the elevated or high lactate subgroups had higher ISS values on average, had a higher percentage of penetrating trauma, and were more likely to receive a massive transfusion (i.e., ≥10 units of pRBC) than the normal lactate subgroup. Patient demographics, injury description, and initial treatment in the three lactate subgroups (normal, elevated, and high), the all lactates group, and the no lactate group are presented in Table 1.
There were significant differences between the three lactate subgroups in all selected outcome descriptors. Clear trends were observed in the MOF rates and CTCOFR14 and CTCOFR21 scores across the lactate subgroups. The percentage of patients experiencing MOF increased in each successively higher lactate subgroup (p < 0.001). This trend was also observed for CTCOFR14 and CTCOFR21, in that the mean scores increased in each increasing lactate subgroup (p < 0.001 and < 0.001, respectively); thus, patients in the elevated and high lactate groups required more days, on average, to resolve organ failures. In addition, the mean CTCOFR14 scores in patients who required massive transfusions were higher than in patients who received fewer than 10 units of pRBC across all three lactate subgroups. There is a low positive correlation of the initial lactate measurement with the number of pRBC transfused (Pearson’s r = 0.14). Figure 1 displays the mean composite endpoint CTCOFR14 scores grouped by patients with and without mass transfusion and plotted for the three lactate subgroups (normal, elevated, and high).
Mean composite endpoint CTCOFR14 for patients with and without mass transfusion for the three lactate subgroups (normal, elevated, and high) based on the initial lactate levels. Plotted against the three lactate categories, the solid line displays the mean CTCOFR14 scores of patients who received mass transfusions (>10 units of pRBC), while the dashed line displays the mean CTCOFR14 scores of patients who received 1–9 units of pRBC. This figure illustrates the correlation between the mean lactate levels and the mean CTCOFR14 scores. Patients with lower lactate levels upon hospital admission tended to require fewer days, on average, to resolve organ failures than patients who had higher lactate levels. In addition, patients who received <10 units of pRBC tended to require fewer days to resolve organ failures than those who received >10 units of pRBC
There was a reciprocal finding for VFD, in that the mean VFD decreased with increasing lactate subgroups (p < 0.001). In addition, there was an increase in hospital mortality and 24-h hospital mortality rates in each increasing lactate subgroup (p < 0.001 and < 0.001, respectively). Thus, patients in the elevated and high lactate groups required more days on ventilator support and had lower survival rates than patients in the normal lactate group. Figure 2 displays the survival rates (%) categorized by lactate subgroup (normal, elevated, and high) against days in hospital over a 28-day period.
Survival curve of the lactate subgroups in a 28-day period. The blue (normal lactate), green (elevated lactate), and red (high lactate) lines illustrate the correlation between lactate levels upon hospital administration and survival. Patients in the normal and elevated lactate categories tended to have survival rates above 90 % through day 28, while patients in the high lactate category tended to have a considerably lower survival rate (<80 % for the majority of the 28-day period)
In the remaining outcomes, days intubated, LOS in ICU, and LOS in hospital, the mean number of days was higher in the elevated lactate group compared to the normal lactate group, but there was a slight decrease in the means between the elevated lactate group and the high lactate group, associated with an increased mortality rate. However, the differences observed among the subgroups for these outcomes were still statistically significant (p = 0.001, 0.003, and 0.05, respectively). Outcome measures in the lactate group, no lactate group, and the three lactate subgroups (normal, elevated, and high) are presented in Table 2.
Discussion
The study methodology used to review the TR-DGU database yielded patient populations with similar injury patterns and demographics in the two main groups (lactate versus no lactate), as well as across the three lactate subgroups (normal, elevated, and high). The two differences between the lactate group and the no lactate group, preclinical time and crystalloid volume infused, were of minimal clinical importance. The similarities between the two main groups in this study indicate that the lactate group is representative of severely injured patients in the TR-DGU database, regardless of the availability of lactate levels, which was the purpose of incorporating the no lactate group (control) into the study design.
It should be noted that the TR-DGU contains few penetrating trauma cases, which is typical of European trauma registries. This accounts for the high percentage of blunt trauma across the groups analyzed in this study. This prevalence of blunt trauma should be taken into consideration when comparing these findings to populations containing a higher percentage of penetrating trauma patients.
Interestingly, the lactate subgroups were similar in terms of preclinical time and volume of preclinical fluids administered. These observations suggest that the preclinical care givers either could not identify patients at greater risk of severe hemorrhage or were unable to intensify or accelerate treatment and transport (e.g., preclinical protocols dictate that all trauma victims be handled as a high risk of severe hemorrhage). The minimally increased volume (74 mL) of crystalloids used in the lactate group appears to be too small to explain the apparent differences in lactate levels at admission. In general, it appears as if the indication to trigger the measurement and documentation of lactate in the TR-DGU was based on random grounds and not on a registry-wide protocol or guideline.
Once in the emergency room, operating room, and ICU phase, however, patients in the different groups were treated markedly differently and differed in clinical outcome. There was a clear dose-dependent relationship between increasing mean lactate levels and an increase in overall mortality, 24-h mortality, and, to a lesser degree, the MOF rate.
An unexpected finding was that mortality increased simultaneously with MOF rate. It was expected that an increase in mortality, especially early mortality, would attenuate outcome signals based upon the development of MOF. That is, patients dying acutely from hemorrhage would not have enough time to develop organ failure. Consequently, the parallel increase in MOF and mortality rates seen with increasing mean lactate levels points to a true morbidity signal induced by, or at least associated with, the higher shock load of patients with high lactate levels and the consequent higher transfusion load of such patients. This shock load may be a function of time and area under the curve of hypoperfusion and hypo-oxygenation of critical organs [16]. The longer and greater the load, the more severely lactic acidosis is expressed and finally measured by the blood lactate values. This finding clearly points to a link between high lactate values and the administration of blood products. The detrimental effects of the shock load are supported by many of the therapeutic interventions during the initial resuscitation. Among the best described is the transfusion-mediated immune modulation (TRIM) [9, 17].
Given the increase in MOF rate, it was also unexpected that LOS in the ICU and LOS in hospital were highest in the elevated lactate group, whereas the respective outcome for the normal lactate and high lactate groups revealed briefer stays in the ICU and in the hospital. In general, if mortality rates increase, there is an inverse effect on the LOS data, since nonsurvivors typically die earlier than survivors leave the hospital. Results similar to the normal lactate and high lactate groups were found in the no lactate group.
An interesting aspect may be that the vast majority of late deaths (>48 h) occurred in the high lactate group. In line with these findings are the results for CTCOFR14, CTCOFR21, and VFD. A dose-dependent trend is also observed in these parameters, which is a consequence of the underlying methodology. Both endpoint concepts incorporate mortality by taking the worst morbidity outcome into account. In a way, effects on mortality are enhanced and may drive the effects on CTCOFR and VFD. Interestingly, the above-mentioned concept of mortality effects as part of the morbidity endpoints CTCOFR and VFD show a dose-dependent effect curve, whereas the mean intubation days plateau in the elevated and high lactate groups.
The overall mortality findings from this study correlate well with the study by Manikis et al. [18] showing that high initial lactate levels predicted mortality in major trauma. Again, Husain et al. [6] showed significant separation of survivors and nonsurvivors based on initial lactate levels in surgical patients admitted to the ICU.
Conclusions
In this study, elevated blood lactate levels induced by trauma and hemorrhage closely correlated with worsening patient outcomes. Based on this evidence, we conclude that elevated blood lactate may constitute a valid early indicator for the identification of patients at higher risk for major morbidities. In addition, lactate appears to have the potential to serve as a marker for goal-directed therapies. Moreover, therapies for shock that improve microcirculation or antagonize tissue hypoxemia should have effects that can be monitored by serum lactate levels. Such treatments should also attenuate the subsequent development of multiple organ failure (MOF) and morbidity, which should also be predictable on the basis of serial blood lactate levels.
Abbreviations
- AIS:
-
Abbreviated Injury Scale
- ANOVA:
-
Analysis of variance
- CTCOFR14 :
-
Composite endpoint of time (days) to complete organ failure resolution for 14 days
- CTCOFR21 :
-
Composite endpoint of time (days) to complete organ failure resolution for 21 days
- FFP:
-
Fresh frozen plasma
- ICU:
-
Intensive care unit
- ISS:
-
Injury Severity Score
- LOS:
-
Length of stay
- MOF:
-
Multiple organ failure
- pRBC:
-
Packed red blood cells
- SD:
-
Standard deviation
- TR-DGU:
-
Trauma Registry of the German Society for Trauma Surgery
- TRIM:
-
Transfusion-mediated immune modulation
- VFD:
-
Ventilator-free days
References
World Health Organization (WHO). Guidelines for trauma quality improvement programmes. Geneva: WHO Press. 2009. http://whqlibdoc.who.int/publications/2009/9789241597746_eng.pdf.
World Health Organization (WHO). The global burden of disease. 2004 Update. Geneva: WHO Press. 2008. http://www.who.int/healthinfo/global_burden_disease/GBD_report_2004update_full.pdf.
Kauvar DS, Wade CE. The epidemiology and modern management of traumatic hemorrhage: US and international perspectives. Crit Care. 2005;9(Suppl 5):S1–9.
Ciesla DJ, Moore EE, Johnson JL, Burch JM, Cothren CC, Sauaia A. A 12-year prospective study of postinjury multiple organ failure: has anything changed? Arch Surg. 2005;140(5):432–8; discussion 438–40.
Sauaia A, Moore FA, Moore EE, Moser KS, Brennan R, Read RA, Pons PT. Epidemiology of trauma deaths: a reassessment. J Trauma. 1995;38(2):185–93.
Husain FA, Martin MJ, Mullenix PS, Steele SR, Elliott DC. Serum lactate and base deficit as predictors of mortality and morbidity. Am J Surg. 2003;185(5):485–91.
Rossaint R, Bouillon B, Cerny V, Coats TJ, Duranteau J, Fernández-Mondéjar E, Hunt BJ, Komadina R, Nardi G, Neugebauer E, Ozier Y, Riddez L, Schultz A, Stahel PF, Vincent JL, Spahn DR; Task Force for Advanced Bleeding Care in Trauma. Management of bleeding following major trauma: an updated European guideline. Crit Care. 2010;14(2):R52.
Nguyen HB, Rivers EP, Knoblich BP, Jacobsen G, Muzzin A, Ressler JA, Tomlanovich MC. Early lactate clearance is associated with improved outcome in severe sepsis and septic shock. Crit Care Med. 2004;32(8):1637–42.
Claridge JA, Crabtree TD, Pelletier SJ, Butler K, Sawyer RG, Young JS. Persistent occult hypoperfusion is associated with a significant increase in infection rate and mortality in major trauma patients. J Trauma. 2000;48(1):8–14; discussion 14–5.
Abramson D, Scalea TM, Hitchcock R, Trooskin SZ, Henry SM, Greenspan J. Lactate clearance and survival following injury. J Trauma. 1993;35(4):584–8; discussion 588–9.
Blow O, Magliore L, Claridge JA, Butler K, Young JS. The golden hour and the silver day: detection and correction of occult hypoperfusion within 24 hours improves outcome from major trauma. J Trauma. 1999;47(5):964–9.
Dutton RP, Lefering R, Lynn M. Database predictors of transfusion and mortality. J Trauma. 2006;60(6 Suppl):S70–7.
Vincent JL, de Mendonça A, Cantraine F, Moreno R, Takala J, Suter PM, Sprung CL, Colardyn F, Blecher S. Use of the SOFA score to assess the incidence of organ dysfunction/failure in intensive care units: results of a multicenter, prospective study. Working group on “sepsis-related problems” of the European Society of Intensive Care Medicine. Crit Care Med. 1998;26(11):1793–800.
Nadel S, Goldstein B, Williams MD, Dalton H, Peters M, Macias WL, Abd-Allah SA, Levy H, Angle R, Wang D, Sundin DP, Giroir B; REsearching severe Sepsis and Organ dysfunction in children: a gLobal perspective (RESOLVE) study group. Drotrecogin alfa (activated) in children with severe sepsis: a multicentre phase III randomised controlled trial. Lancet. 2007;369(9564):836–43.
Schoenfeld DA, Bernard GR; ARDS Network. Statistical evaluation of ventilator-free days as an efficacy measure in clinical trials of treatments for acute respiratory distress syndrome. Crit Care Med. 2002;30(8):1772–7.
Rixen D, Siegel JH. Bench-to-bedside review: oxygen debt and its metabolic correlates as quantifiers of the severity of hemorrhagic and post-traumatic shock. Crit Care. 2005;9(5):441–53.
Hill GE, Frawley WH, Griffith KE, Forestner JE, Minei JP. Allogeneic blood transfusion increases the risk of postoperative bacterial infection: a meta-analysis. J Trauma. 2003;54(5):908–14.
Manikis P, Jankowski S, Zhang H, Kahn RJ, Vincent JL. Correlation of serial blood lactate levels to organ failure and mortality after trauma. Am J Emerg Med. 1995;13(6):619–22.
Acknowledgments
The authors would like to thank Rita C. Tomlin, BS (MT), MA for conducting the literature review, drafting the text, and providing medical writing support. Ms. Tomlin is a medical writing consultant for Sangart, Inc.
The conduct and presentation of this research study was sponsored and funded by Sangart, Inc., San Diego, CA, USA.
Conflict of interest
Dr.med. Dirk Zielske and Howard Levy, MD are employed by Sangart, Inc., which funded this research. Bertil Bouillon, MD, Carl Hauser, MD, and Rolf Lefering, PhD have served as paid consultants for Sangart, Inc., on other projects, but not for this research study. The research presented in this manuscript has not been presented at any meetings or conferences.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lefering, R., Zielske, D., Bouillon, B. et al. Lactic acidosis is associated with multiple organ failure and need for ventilator support in patients with severe hemorrhage from trauma. Eur J Trauma Emerg Surg 39, 487–493 (2013). https://doi.org/10.1007/s00068-013-0285-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00068-013-0285-3