Abstract
Purpose
Diffuse large B‑cell lymphoma (DLBCL) is an aggressive lymphoma subtype treated successfully with immunochemotherapy. However, there are conflicting data on the role and impact of consolidative radiation therapy (RT). The publication of the national evidence-based guideline on DLBCL prompted us to review relevant passages on radiation oncology.
Methods
The following article reviews the evidence and recommendations given in the current German evidence-based guideline on DLBCL regarding RT and summarizes pivotal aspects. Additional literature is presented to provide a comprehensive background for the published recommendations.
Results
RT shall be administered to all patients with localized positron emission tomography(PET)-positive residues after completion of immunochemotherapy and should use a dose of 30–40 Gray in normofractionation. For RT planning, PET information before and after immunochemotherapy shall be used, with either a PET-CT in the RT treatment position or an image fusion to the planning CT. Conformal techniques shall be used for target volume coverage, with a risk–benefit evaluation for the individual patient. Additionally, RT may be used in the treatment context of various subtypes of DLBCL as well as in the recurrent or refractory treatment situation.
Conclusion
RT remains an integral part of the treatment repertoire of DLBCL. With the use of PET-guided treatment, RT is indicated for patients with metabolically active tumors. In the context of the ongoing development of targeted therapies, new RT indications may evolve.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diffuse large B‑cell lymphoma (DLBCL) is the most common aggressive non-Hodgkin lymphoma (NHL), constituting 31% of all NHL [1]. The current annual incidences are 29,100 cases in the United States and 26,000 in Western Europe, with a predicted increase in the next years [2]. Due to the otherwise dismal course of DLBCL, staging should be completed within a few weeks to initiate timely therapy thereafter. Immunochemotherapy with rituximab, cyclophosphamide, hydroxydaunorubicin, vincristine, and predniso(lo)ne (R-CHOP)-based regimens are the backbone of therapy to enable long-term cure, which is achieved in approximately 65% of patients [3]. However, the role of radiation therapy (RT) is yet to be defined and is subject to discussions.
During the past 2 years, experts in various disciplines such as hematology, pathology, radiology, and radiation oncology elaborated a common evidence-based guideline, which was published in June 2022 [4]. The project was funded and supported by the German Guideline Program in Oncology (registration no. 018-038OL).
The following article reviews important aspects for radiation oncologists.
Radiotherapy in first-line treatment—PET-guided therapy takes center stage
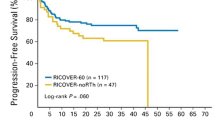
Historically, the indication for RT was based on prechemotherapy morphological risk factors such as extranodal involvement or bulky disease. The UNFOLDER trial randomized patients aged 18–60 years with an age-adjusted international prognostic index of 0–1 between three-weekly R‑CHOP-21 and a two-weekly schedule (R-CHOP-14) [5]. A second randomization occurred after completion of immunochemotherapy between consolidative RT to bulky and extranodal sites with 39.6 Gray (Gy) versus observation (see Table 1 for an overview). Despite the improvement of the primary endpoint event-free survival (EFS) by means of RT (84% vs. 68%; p = 0.001), no significant changes in progression-free survival (PFS) or overall survival (OS) could be demonstrated (PFS: 89% vs. 81%; p = 0.221; OS: 93% vs. 93%, p = 0.506) in an interim analysis [5]. Final results of this trial are pending. The RICOVER-60 trial identified six cycles of R‑CHOP-14 (plus two cycles of rituximab) as an optimal treatment for patients aged 61–80 years and administered RT with 36 Gy to sites of initial bulky (≥ 7.5 cm) disease or extralymphatic involvement [6]. A comparison with a subsequent trial (RICOVER-noRTh) using the same immunochemotherapy without RT revealed an inferior EFS without RT in patients with bulky disease (40%; 95% confidence interval [CI]: 26–55% vs. 66%; 95% CI: 57–75%; p = 0.001), mainly due to unplanned RT series counting as an event [7]. Focusing on patients with bulky disease treated according to protocol, significant advantages in 3‑year EFS (54%; 95% CI: 38–71% vs. 80%; 95% CI: 71–89%; p = 0.001), PFS (62%; 95% CI: 46–78% vs. 88%; 95% CI: 80–95%; p < 0.001), and OS (65%; 95% CI: 49–81% vs. 90%; 95% CI: 84–97%; p = 0.001) were reported with the use of RT. Without an obligatory positron emission tomography (PET) scan after systemic therapy, the role of the metabolic status remains elusive.
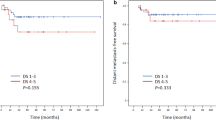
The present guideline follows the rationale of trials in the modern era by establishing a risk stratification via PET. Preliminary data from the OPTIMAL>60 study point towards the possibility of limiting RT to patients who are PET positive after systemic therapy [8, 9]. Patients treated in this study were 61–80 years old and randomization was undertaken after four cycles of immunochemotherapy with R‑CHOP or R‑CHLIP (liposomal vincristine instead of the conventional vincristine). Patients with a Deauville score of 3–5 were defined as PET positive and received two additional cycles of systemic therapy and involved-site radiotherapy of 39.6 Gy. This approach led to a 42% reduction of RT series without deterioration in PFS and OS as compared to RICOVER-60. Notably, only 22% of patients in the RT arm were not irradiated (mostly due to progression or medical reasons). Final results of this trial have not yet been published and are eagerly awaited.
In the absence of prospective evidence, the mainstay of PET-guided RT in DLBCL is a retrospective analysis from British Columbia [10]. In the work by Freeman and colleagues, 723 patients with a median age of 65 years were included, predominantly in Ann Arbor stage III or IV (74%) and with bulky disease in 39% of patients. RT was limited to patients with a Deauville score of 4 or 5 after at least six cycles of R‑CHOP. This approach could ameliorate the prognosis of patients with a positive end-of-treatment PET who underwent consolidative RT, reaching nearly the level of initial PET-negative patients (3-year time to progression: 76% vs. 83%; p = 0.3; 3‑year OS: 80% vs. 87% for the irradiated vs. initial PET-negative subgroups, respectively). Neither the initial presence of bulky disease, craniofacial involvement, nor skeletal manifestations heralded a worse time to progression. In summary, patients with localized PET-positive residual lymphoma after completion of immunochemotherapy shall receive consolidative RT.
Radiotherapy planning
Implementation of PET guidance in the treatment algorithm offers additional information for RT planning. Either expansion of the target volume due to detection of additional lesions or adaption due to better differentiation between vital and avital residues may result. Consequently, existent PET examinations before and after immunochemotherapy shall be used for RT planning. This recommendation was formulated in analogy to the evidence-based guideline on Hodgkin lymphoma [11]. Data focusing on DLBCL patents are sparse; one analysis from the Memorial Sloan Kettering Cancer Center comparing CT-based vs. PET-CT-based contouring included 118 patients, but only 18 with DLBCL, the latter demonstrating a gross target volume expansion > 5% in 33% and a reduction > 5% in 28% with the use of PET [12]. As a result, the International Lymphoma Radiation Oncology Group (ILROG) also recommends the use of PET-CT, ideally performed in the treatment position or fused to the planning CT scan [13, 14]. In analogy to other mediastinal lymphomas (e.g., Hodgkin lymphoma), RT planning and execution in deep inspiration breath-hold technique should be evaluated (Fig. 1). Concerning the radiation plan, there is no general recommendation: a conformal technique shall be used with an individual benefit–risk evaluation of different approaches (3D conformal RT, intensity-modulated RT, volumetric modulated arc therapy). Among the techniques, proton therapy may be used to reduce the RT dose to organs at risk in the mediastinum, the impact of which on (long-term) toxicity is yet to be determined.
Deep inspiration breath-hold technique for mediastinal lymphoma. Frontal CT scans of the same patient with a mediastinal lymphoma residue prior to radiotherapy (RT) with isodose lines of a planned intensity-modulated RT (IMRT) plan. Scans were acquired in a free breathing and b deep inspiration breath-hold. Note the inflation of the lungs and the displacement of the heart from the target volume, enabling better sparing of these organs at risk
Contouring
Modern RT planning shall use the concept of involved-site irradiation as introduced by the ILROG [13, 15]. The (sub)volumes used for RT planning are the gross tumor volume (GTV), clinical target volume (CTV), and planning target volume (PTV) with an optional internal target volume (ITV). The GTV covers macroscopic disease based on different examinations (PET, CT), whereas the CTV adapts the initial volume to the post-chemotherapy situation and adds an individual margin to account for subclinical spread (see Fig. 2). Importantly, the CTV has to include the post-chemotherapy (macroscopic) remaining lymphoma tissue. An ITV is essential for mobile target volumes in the thorax and abdomen and is established via 4D-CT or fluoroscopy. Otherwise, an isotropic margin of 1.5–2 cm may be used. Final expansions are introduced to consider positional uncertainties to receive the PTV.
Consolidative radiotherapy of positron emission tomography (PET-)positive residues. a Initial (prechemotherapy) CT scan revealing an abdominal bulk of DLBCL. b Postchemotherapy CT scan of the abdomen showing an excellent response with only minimal residues. c F18-FDG-PET-CT indicates metabolically active tumor (Deauville 4) despite the good morphological response. d Colorwash representation of the 95% isodose covering the planning target volume (thin orange line). Radiation treatment was delivered via a volumetric modulated arc therapy photon plan
Recent randomized trials on DLBCL such as MInT, RICOVER-60, UNFOLDER, and OPTIMAL > 60 utilize RT doses between 36 and 40 Gy in normofractionation [5, 6, 8, 9, 16], which may be seen as standard. However, a dose de-escalation study from the United Kingdom compared 30 Gy with 40–45 Gy as involved-field therapy for the treatment of aggressive lymphoma and failed to demonstrate differences in the rate of in-field recurrences (HR: 0.98; 95% CI: 0.68–1.4; p = 0.89) [17]. Overall, there are some limitations of this analysis, as the patient collective was mixed, covering treatments in the primary or recurrent situation and with curative as well as palliative intent. Radiological response assessment was not mandatory and no data on PET or morphological risk factors (e.g., bulk) were provided.
Specific subtypes: extranodal involvement of bone, breast, stomach, testis, and primary mediastinal B-cell lymphoma
Apart from nodal lymphoma, RT may be used for the treatment of various subtypes and extranodal sites. In some cases (involvement of bones, primary mediastinal B‑cell lymphoma, primary extranodal DLBCL of the breast, gastric DLBCL without indolent component) the recommendation follows the algorithm of the PET-guided strategy described earlier. This is of particular importance for osseous involvement, which has been considered as a standard indication for RT due to the results of a pooled meta-analysis by the German High-Grade Non-Hodgkin’s Lymphoma Study Group [18]. The addition of RT after R‑CHOP immunochemotherapy led to a significant amelioration of 3‑year EFS (75% vs. 36%, p = 0.001). In the study by Freeman et al. (s. “Radiotherapy in first-line treatment”), 142 patients revealed skeletal involvement, 73% of whom became PET negative after R‑CHOP [10]. In patients with initial skeletal involvement, the rate of PET-negativity after systemic therapy did not differ from the overall study population (p = 0.8) and there was no significant difference in the time to progression compared to PET-negative patients without skeletal manifestations of lymphoma.
An important differentiation is described for gastric lymphoma, as patients with an indolent component (present in approximately one third of aggressive lymphomas of the stomach [19]) should be offered consolidative RT without consideration of the PET status. This rationale is supported by a Korean recurrence analysis, showing local or combined relapses as the principle location of treatment failure [20].
Patients with primary testicular DLBCL should receive a unilateral orchiectomy and shall be treated with subsequent R‑CHOP chemotherapy in analogy to nodal DLBCL. RT should be administered prophylactically to the contralateral testis after completion of systemic therapy, also including the ipsilateral testis, if no orchiectomy has been performed. In this context, RT results in a significant improvement in local control [21, 22], with one retrospective analysis postulating even an OS benefit [23].
Recurrences/refractory disease
Regarding second-line therapy, a recommendation to irradiate patients with localized PET-positive residues after systemic therapy is given in the guideline, although there are no randomized studies addressing this aspect. Importantly, patients in the second-line situation who are unable/unfit to undergo systemic therapy shall be evaluated for palliative RT according to the respective ILROG guidelines [24]. The cited paper delineates different clinical scenarios for the refractory/recurrent situation, with a possible dose escalation beyond 40 Gy (up to 55 Gy). Additionally, RT shall be evaluated (beside chemo-, immuno-, or targeted therapy) in the setting of ≥ second recurrences or progression in a palliative setting or as a modality for remission induction before a curative (intended) therapy (“bridging” concept). For patients with primary mediastinal B‑cell lymphoma who did not receive RT, a localized recurrence should be irradiated.
Perspective
RT remains an important instrument in the orchestra of treating DLBCL. With the help of diagnostic tools and predictive markers, a further individualized treatment is awaited, enabling a risk-adapted strategy. The development of new targeted therapies challenges the position of RT but also offers the possibility of new synergistic combinations, the analysis of which will be a major task for the radiation oncology community in the years to come.
References
Thandra KC, Barsouk A, Saginala K et al (2021) Epidemiology of Non-Hodgkin’s lymphoma. Med Sci 9:5. https://doi.org/10.3390/medsci9010005
Kanas G, Ge W, Quek RGW et al (2022) Epidemiology of diffuse large B‑cell lymphoma (DLBCL) and follicular lymphoma (FL) in the United States and Western Europe: population-level projections for 2020–2025. Leuk Lymphoma 63:54–63. https://doi.org/10.1080/10428194.2021.1975188
Cunningham D, Hawkes EA, Jack A et al (2013) Rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisolone in patients with newly diagnosed diffuse large B‑cell Non-Hodgkin lymphoma: a phase 3 comparison of dose intensification with 14-day versus 21-day cycles. Lancet 381:1817–1826. https://doi.org/10.1016/S0140-6736(13)60313-X
Leitlinienprogramm Onkologie (Deutsche Krebsgesellschaft, Deutsche Krebshilfe, AWMF) (2022) Diagnostik, Therapie und Nachsorge für erwachsene Patient*innen mit einem diffusen großzelligen B‑Zell-Lymphom und verwandten Entitäten (AWMF-Registernummer: 018/038OL)
Pfreundschuh M, Murawski N, Ziepert M et al (2018) Radiotherapy (RT) to bulky (B) and extralymphatic (E) disease in combination with 6xR-CHOP-14 or R‑CHOP-21 in young good-prognosis DLBCL patients: results of the 2x2 randomized UNFOLDER trial of the DSHNHL/GLA. J Clin Oncol 36:7574–7574. https://doi.org/10.1200/JCO.2018.36.15_suppl.7574
Pfreundschuh M, Schubert J, Ziepert M et al (2008) Six versus eight cycles of bi-weekly CHOP-14 with or without rituximab in elderly patients with aggressive CD20+ B‑cell lymphomas: a randomised controlled trial (RICOVER-60). Lancet Oncol 9:105–116. https://doi.org/10.1016/S1470-2045(08)70002-0
Held G, Murawski N, Ziepert M et al (2014) Role of radiotherapy to bulky disease in elderly patients with aggressive B‑cell lymphoma. J Clin Oncol 32:1112–1118. https://doi.org/10.1200/JCO.2013.51.4505
Pfreundschuh M, Christofyllakis K, Altmann B et al (2017) Radiotherapy to bulky disease PET-negative after immunochemotherapy in elderly DLBCL patients: results of a planned interim analysis of the first 187 patients with bulky disease treated in the OPTIMAL〉60 study of the DSHNHL. J Clin Oncol 35:7506–7506. https://doi.org/10.1200/JCO.2017.35.15_suppl.7506
Pfreundschuh M, Murawski N, Christofyllakis K et al (2017) Excellent outcome of elderly patients with favourable-prognosis DLBCL treated with 4 cycles CHOP/Chlip-14 plus 8 applications of rituximab and a PET-based intensification strategy that includes involved-site radiotherapy (IS-RT): results of the first 120 patients of the OPTIMAL〉60 trial of the Dshnhl. Blood 130:1549–1549. https://doi.org/10.1182/blood.V130.Suppl_1.1549.1549
Freeman CL, Savage KJ, Villa D et al (2020) Long-term results of PET-guided radiation in advanced-stage diffuse large B‑cell lymphoma patients treated with R‑CHOP. Blood. https://doi.org/10.1182/blood.2020005846
Leitlinienprogramm Onkologie (Deutsche Krebsgesellschaft, Deutsche Krebshilfe, AWMF) (2019) Diagnostik, Therapie und Nachsorge des Hodgkin Lymphoms bei erwachsenen Patienten. http://www.leitlinienprogramm-onkologie.de/leitlinien/hodgkin-lymphom. Accessed 5 Mar 2022 (Langversion 2.1)
Terezakis SA, Schöder H, Kowalski A et al (2014) A prospective study of 18FDG-PET with CT coregistration for radiation treatment planning of lymphomas and other hematologic malignancies. Int J Radiat Oncol Biol Phys 89:376–383. https://doi.org/10.1016/j.ijrobp.2014.02.006
Wirth A, Mikhaeel NG, Aleman BMP et al (2020) Involved site radiation therapy in adult lymphomas: an overview of international lymphoma radiation oncology group guidelines. Int J Radiat Oncol Biol Phys. https://doi.org/10.1016/j.ijrobp.2020.03.019
Mikhaeel NG, Milgrom SA, Terezakis S et al (2019) The optimal use of imaging in radiation therapy for lymphoma: guidelines from the international lymphoma radiation oncology group (ILROG). Int J Radiat Oncol Biol Phys 104:501–512. https://doi.org/10.1016/j.ijrobp.2019.02.001
Illidge T, Specht L, Yahalom J et al (2014) Modern radiation therapy for nodal Non-Hodgkin lymphoma-target definition and dose guidelines from the international lymphoma radiation oncology group. Int J Radiat Oncol Biol Phys 89:49–58. https://doi.org/10.1016/j.ijrobp.2014.01.006
Pfreundschuh M, Kuhnt E, Trümper L et al (2011) CHOP-like chemotherapy with or without rituximab in young patients with good-prognosis diffuse large-B-cell lymphoma: 6‑year results of an open-label randomised study of the MabThera International trial (MInT) group. Lancet Oncol 12:1013–1022. https://doi.org/10.1016/S1470-2045(11)70235-2
Lowry L, Smith P, Qian W et al (2011) Reduced dose radiotherapy for local control in non-Hodgkin lymphoma: a randomised phase III trial. Radiother Oncol 100:86–92. https://doi.org/10.1016/j.radonc.2011.05.013
Held G, Zeynalova S, Murawski N et al (2013) Impact of rituximab and radiotherapy on outcome of patients with aggressive B‑cell lymphoma and skeletal involvement. J Clin Oncol 31:4115–4122. https://doi.org/10.1200/JCO.2012.48.0467
Chan JK, Ng CS, Isaacson PG (1990) Relationship between high-grade lymphoma and low-grade B‑cell mucosa-associated lymphoid tissue lymphoma (MALToma) of the stomach. Am J Pathol 136:1153–1164
Kang HJ, Lee HH, Jung S‑E et al (2020) Pattern of failure and optimal treatment strategy for primary gastric diffuse large B‑cell lymphoma treated with R‑CHOP chemotherapy. PLoS ONE 15:e238807. https://doi.org/10.1371/journal.pone.0238807
Zucca E, Conconi A, Mughal TI et al (2003) Patterns of outcome and prognostic factors in primary large-cell lymphoma of the testis in a survey by the international extranodal lymphoma study group. J Clin Oncol 21:20–27. https://doi.org/10.1200/JCO.2003.11.141
Zouhair A, Weber D, Belkacémi Y et al (2002) Outcome and patterns of failure in testicular lymphoma: a multicenter rare cancer network study. Int J Radiat Oncol Biol Phys 52:652–656. https://doi.org/10.1016/s0360-3016(01)02647-5
Park B‑B, Kim JG, Sohn SK et al (2007) Consideration of aggressive therapeutic strategies for primary testicular lymphoma. Am J Hematol 82:840–845. https://doi.org/10.1002/ajh.20973
Ng AK, Yahalom J, Goda JS et al (2018) Role of radiation therapy in patients with relapsed/refractory diffuse large B‑cell lymphoma: guidelines from the international lymphoma radiation oncology group. Int J Radiat Oncol Biol Phys 100:652–669. https://doi.org/10.1016/j.ijrobp.2017.12.005
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M. Oertel, C. Berdel, G. Held, K. Herfarth, H. Schmidberger, M. Ernst, G. Lenz, P. Borchmann, and H.T. Eich declare that they have no competing interests.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Oertel, M., Berdel, C., Held, G. et al. The new German evidence-based guideline on diffuse large B-cell lymphoma—key aspects for radiation oncologists. Strahlenther Onkol 199, 115–120 (2023). https://doi.org/10.1007/s00066-022-02035-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-022-02035-9