Abstract
Evidence from a few small randomized trials and retrospective cohorts mostly including various tumor entities indicates a prolongation of disease free survival (DFS) and overall survival (OS) from local ablative therapies in oligometastatic disease (OMD). However, it is still unclear which patients benefit most from this approach. We give an overview of the several aspects of stereotactic body radiotherapy (SBRT) in extracranial OMD in breast cancer from a radiation oncology perspective. A PubMed search referring to this was conducted. An attempt was made to relate the therapeutic efficacy of SBRT to various prognostic factors. Data from approximately 500 breast cancer patients treated with SBRT for OMD in mostly in small cohort studies have been published, consistently indicating high local tumor control rates and favorable progression-free (PFS) and overall survival (OS). Predictors for a good prognosis after SBRT are favorable biological subtype (hormone receptor positive, HER2 negative), solitary metastasis, bone-only metastasis, and long metastasis-free interval. However, definitive proof that SBRT in OMD breast cancer prolongs DFS or OS is lacking, since, with the exception of one small randomized trial (n = 22 in the SBRT arm), none of the cohort studies had an adequate control group. Further studies are needed to prove the benefit of SBRT in OMD breast cancer and to define adequate selection criteria. Currently, the use of local ablative SBRT should always be discussed in a multidisciplinary tumor board.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Traditionally, treatment for metastatic breast cancer has been regarded as palliative, with the corresponding therapeutic implications. However, this view has been challenged in recent years due to observations in other solid tumors. In 1968, Philip Rubin proclaimed that there are considerable prognostic differences in metastatic disease, and he asked: “Are metastases curable?” [1]. In the 1990s, the radiation oncologists Samuel Hellman and Ralph. R. Weichselbaum published their hypothesis of oligometastatic disease (OMD), which is to be understood as a transitional state between locally confined disease and widespread metastatic disease [2]. It was postulated that a subset of patients with a small number of macroscopic metastases may have a limited microscopic tumor burden and could be treated with “curative” local therapy and “adjuvant” drug therapy.
This approach is supported by the success of surgical series. In cohorts including several histological tumor sites with mostly colorectal cancer or sarcoma patients, surgical removal of liver or lung metastases resulted in 5‑year survival rates of up to 50 % depending on the risk constellation [3,4,5,6,7]. In the past, this hypothesis was further supported by several single-arm studies on stereotactic body radiotherapy (SBRT). However, most of these studies showing the efficacy of local ablative therapy with long-term survival in a subset of patients with oligometastatic disease enrolled a very limited number of breast cancer patients [8]. In recent years, further data have indicated that cure might be potentially possible in prognostically favorable cases of OMD [9,10,11]. However, although significant prognostic differences and various treatment approaches in the metastatic disease group are known, a definition of a favorable OMD group with the potential for cure is unclear.
In 2020, a group of 20 international experts of the ESTRO and EORTC OligoCare project developed a comprehensive system for characterization and classification [12], which aims to take into account the different clinical scenarios of OMD. Criteria for subclassification include timing of OMD (synchronous vs. metachronous), history of previous OMD (repeat vs. de novo OMD), systemic therapy at the time of OMD diagnosis (oligorecurrence vs. oligoprogression), response to systemic therapy (oligopersistence vs. oligoprogression), and previous history of polymetastatic disease (induced OMD). This classification was recently validated in a retrospective single-center cohort of 385 patients with OMD [13].
This classification is very useful for further studies but can only in part be applied to the currently available data. In current clinical trials, a maximum of 3–5 metastases are accepted in the context of OMD. However, whether the definition of OMD should strictly rely on a maximum number of metastatic sites is a matter of debate. Probably, the criteria used so far to classify OMD versus no OMD do not do sufficient justice to the biology of OMD. There is much to be said for a spectrum of diseases, with a fluent transition between local and systemic disease [14], and depending on this, a more or less pronounced benefit of local therapy.
An ESTRO-ASTRO OMD consensus document states on the one hand that “the possibility to safely deliver curative intent metastasis-directed radiotherapy determines the maximum number” [15], but on the other hand states that the ability to safely treat all oligometastases with radiotherapy does not mean that one should treat every patient irrespective of other prognostic factors.
In this review, we try to highlight the current data on oligometastatic breast cancer with regard to stereotactic body radiotherapy (SBRT) for extracranial disease sites. In addition, several aspects such as prognostic factors and systemic therapy will be addressed.
Methods
A PubMed search was conducted to extract relevant articles from 2000 to 2021. A search was performed using the following terms: (oligometastases OR oligometastasis OR oligometastatic disease OR oligo metastatic disease) AND (breast cancer OR breast neoplasm OR breast) AND (radiotherapy OR ablative radiotherapy OR stereotactic radiotherapy OR radiation).
We give an overview of results of prospective and retrospective studies using SBRT to treat extracranial disease sites for patients with oligometastatic breast cancer, as well as an overview of prognostic factors and further treatment aspects.
Summary of trials of SBRT for patients with oligometastatic breast cancer
In Table 1, relevant studies including breast cancer patients with OMD treated with SBRT are presented. Overall, the 10 studies included 505 patients. In six studies, the design was retrospective and in four studies prospective. All but one study were single-arm studies without a control arm. Regarding the only randomized study by Tsai et al., which reported a preplanned subgroup analysis on patients with oligoprogressive breast cancer, only an interim analysis in abstract form is available [16].
Analyses from seven studies [10, 17,18,19,20,21,22] encompassing a sample size of 15–120 patients with 1–5 metastases (mostly ≤ 2 lesions in 70.9–100 % of cases) reported LC rates at 1 and 2 years between 86.9 and 100 % and 79.2 and 100 %, respectively. The 1‑ and 2‑year PFS ranged from 38 to 80 % (seven studies) and 8 to 75 % (nine studies), respectively. Further details on the results are shown in Table 1.
Eight studies provided graded toxicity data. No grade 3 toxicities were seen in four of eight studies. Grade 3 toxicities were seen in four studies (4.2–18 %).
A recent systematic review and meta-analysis summarizes most of these data in a quantitative manner [23].
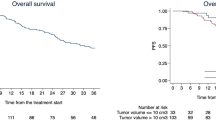
Outcome of patients with OMD from different primary tumors treated with SBRT
Overall, the abovementioned studies consistently show that local ablative radiotherapy in oligometastatic breast cancer patients leads to very high local control rates in the range of 90 % and, depending on disease- or patient-specific factors, more or less favorable PFS and OS. Randomized controlled trials of SBRT in patients with OMD demonstrated improvements in PFS and partly also in OS, especially in prognostically more favorable constellations [24,25,26,27,28,29,30]. However, these studies were not focused on breast cancer, but usually included different histologies. The SABR-COMET randomized phase II trial was the only trial to enroll a minority of breast cancer patients but did not report the results of the breast cancer subgroup separately [29, 30]. There was an imbalance in baseline characteristics, with more patients with prostate cancer randomized to the experimental arm. However, a post-hoc sensitivity analysis excluding patients with prostate cancer confirmed the findings in the overall cohort. The other randomized controlled trials were conducted in patients with lung or prostate cancer. While trials enrolling patients with prostate cancer mostly focused on metachronous oligorecurrence, lung cancer trials mainly enrolled patients with synchronous OMD. The interpretation of the data is not trivial due to the heterogeneity in tumor entities as well as previous and subsequent systemic therapy. Furthermore, almost all of the trials involving breast cancer patients were cohort studies without a control arm, rendering causal inferences impossible. In summary, there is evidence that SBRT is associated with high local control rates and low toxicity in patients with oligometastatic breast cancer. However, there is only indirect evidence that SBRT in OMD breast cancer may prolong survival in breast cancer patients. Further research is needed to define which breast cancer patients with OMD have a clinically relevant benefit from SBRT beyond local tumor control.
Prognostic factors in patients with oligometastatic breast cancer
Bone versus no bone metastases
It is well documented that in breast cancer, bone-only metastases are associated with a better prognosis for LC, OS, and PFS than visceral or brain metastases, irrespective of treatment [10, 31, 32]. The 5‑ and 10-year OS after SBRT for patients with bone-only metastases compared to patients with metastatic lesions at other sites were 83 and 75 %, and 31 and 17 %, respectively [10]. Milano et al. furthermore demonstrated an LC rate after SBRT of bone metastases after 10 years of 100 % vs. 73 % for other metastatic sites [10]. For patients with bone-only metastases, David et al. reported a 2-year LC of 100 % [17]. In a study by Onal et al. including only patients with liver metastases with or without bone or lung metastases, the 2‑year LC, PFS, and OS were 88, 8, and 57 %, respectively [33]. In an analysis by Wijtunga et al. including patients with oligometastatic breast cancer treated with SBRT, the presence of visceral or brain metastases was associated with an inferior prognosis as compared to bone-only disease (HRs for PFS and OS of 2.19 and 1.77, respectively) [32]. Furthermore, the study by Scorsetti et al., including only patients with visceral metastases, suggests inferior PFS and OS as compared to studies of patients with bone-only OMD, despite good local control with SBRT [18].
Number of metastases
In general, the available data show that prognosis on survival endpoints declines with an increasing number of metastases. Regarding the prognostic influence of the number of metastases, Weykamp et al. identified a solitary metastasis as an independent prognostic factor for PFS (HR 0.363) and distant control (HR 0.186) compared to > 1 metastases [21]. Further, Steenbruggen et al., based on the Netherlands Cancer Registry (n = 3447) including 612 breast cancer patients with OMD, showed that patients with a maximum of 3 metastases vs. > 3 metastases had an estimated 10-year survival of 14.9 vs. 3.4 % [34]. The HRs for OS for patients with 1 metastasis, 2–3 metastases, and 4–5 metastases versus > 5 metastases were 0.70 (p = 0.03), 0.63 (p = 0.009), and 0.91 (n. s.), respectively. In this analysis, however, only 20 % of patients received local ablative treatment to metastatic sites, which mostly consisted of SBRT. Again, it should be emphasized that patients with 3–5 metastatic lesions were underrepresented in most studies. In the publications mentioned in Table 1, 70–100 % of the patients had a maximum of 2 metastases.
Time of metastases
Whether the timing of OMD diagnosis plays a prognostic role is still a matter of debate in breast cancer. Dawood et al. analyzed a large cohort of metastatic breast cancer patients, albeit without mentioning the number of OMD patients. The results suggest that patients with synchronous metastases have a significantly better OS than those with metachronous metastases [31]. Interestingly, if the metastases occurred > 5 years after the initial diagnosis, the difference in survival was not significantly different compared to patients with synchronous metastases. Also, Wijtunga et al. saw better OS rates for patients developing metastases > 5 years after primary diagnosis vs. < 5 years (HR 4.17; p = 0.003) in the OMD setting [32].
In this context, systemic therapy, often given initially as part of an adjuvant treatment regimen, plays an important role. Adjuvant therapy may select particularly aggressive or resistant cell clones, which then leads to an adverse prognosis of metachronous metastatic disease [35, 36]. In turn, a long disease-free interval from curative treatment until the development of metastatic disease seems to be prognostically favorable [31].
Further prognostic factors
Numerous further clinical factors are well known to influence the prognosis of breast cancer patients. Beside others, these include age, hormonal receptor status, HER2 status, clinical tumor stage at diagnosis, tumor grading, and the performance status of the patient [37]. The prognostic relevance of these factors has been established mainly in the context of studies dealing with systemic therapy. However, the extent to which these factors are also meaningful for SBRT of OMD is still far less clear. Kucharczyk et al. performed a systematic review exploring factors defining an OMD population that may benefit from ablative therapies including mostly surgery and SBRT [38]. Overall, 41 retrospective studies with 1813 breast cancer patients were identified. Of these patients, 113 had extracranial OMD, including 79 treated with ablative dose radiotherapy. No quantitative meta-analysis was conducted due to the heterogeneity of the included studies. Positive prognostic factors included tumor biology (hormone receptor positive/HER2 negative vs. other subtypes), longer disease-free interval before local ablative treatment, and number of lesions. The authors assessed that the existing evidence does not show a clear direction as to which patients can benefit from such a treatment approach. Further, the authors concluded that the use of an ablative therapy per se (versus no ablative therapy) is supported by low-level evidence.
This observation was confirmed in the previously mentioned database analysis by Steenbruggen et al., independent of systemic treatment [34]. Multivariate analyses revealed a survival benefit in favor of local ablative treatment (mostly SBRT) with an HR of 0.57 (p = 0.02) in patients with 1–3 breast cancer metastases. However, in the absence of randomization, a relevant bias in favor of patients receiving local ablative therapies cannot be excluded in this analysis.
Tumor biology and systemic treatment
The benefit of local ablative therapy for survival is expected to be dependent on the propensity for further systemic progression and efficacy of systemic therapy. Not surprisingly, most studies have focused on patients with hormone receptor-positive and HER2-negative breast cancer, while especially patients with triple-negative breast cancer (TNBC) were underrepresented. Just recently, Wijetunga et al. highlighted the association between clinical outcomes and clinical and molecular factors in a cohort treated with SBRT [32]. Overall, 79 breast cancer patients with 103 metastatic lesions were identified. Patients with HR+/HER-, HER2+ (irrespective of HR expression), and TNBC breast cancer had a median OS of 86 months, not reached, and 18 months, respectively. Tan et al. confirmed the poor prognosis of patients with TNBC treated with SBRT [22].
Response to systemic therapy may be another important factor to consider. There has been growing interest in the use of local ablative treatment in patients with oligoprogression during systemic therapy. Mainly, this has been used as a means to keep patients on the same systemic therapy regimen while treating progressing metastases locally. Contrary to the concept of treating all existing metastatic lesions with local ablative therapy, these treatments are often applied to progressive lesions only. It is important to mention that the term “oligoprogression” may include patients with OMD as well as patients with polymetastatic disease. The abovementioned ESTRO-EORTC classification of OMD specifically designates the term “induced OMD” for patients with prior history of polymetastatic disease [12].
Oligoprogressive disease has a comparatively worse prognosis. Tan et al. demonstrated that for patients treated with SBRT, those with oligoprogressive disease had an inferior prognosis as compared to patients with OMD, with 1‑ and 2‑year PFS rates of 19.6 and 8 % compared to 66 and 52 %, respectively [22]. Despite this, or even because of it, oligoprogression may be a particularly interesting subclass for local therapies within OMD. For example, Tan et al. pointed out that SBRT as an “alternate line of therapy” may delay the potential unfavorable effects on quality of life with regard to toxicities due to switching systemic therapy [22].
Preliminary data from a randomized phase II trial, the CURB trial, were presented by Tsai et al. [16]. Latest interim results presented by Tsai et al. at the ASTRO Annual Meeting 2021 must be considered with caution due to inclusion of different entities—NSCLC and breast cancer—with different outcomes of the small subgroups. The data favored the addition of SBRT to oligoprogressive lesions but could not demonstrate a benefit from additional SBRT in the subgroup of patients with oligoprogressive breast cancer. However, it should be emphasized that only 44 breast cancer patients have been analyzed so far (22 patients per arm), including 16 patients with TNBC. Further, it should be underscored here that patients included in the study by Tsai et al. were at a high risk per se on the one hand, and still oligoprogressive on the other. This is probably an unfavorable subgroup of patients for SBRT. A general recommendation in one direction or the other cannot be derived from these preliminary data of a very specific high-risk population. However, this demonstrates once again the importance of developing meaningful selection criteria for SBRT in OMD as well as appropriate subclassifications as proposed by Guckenberger et al. [12].
In general, systemic therapy is generally recommended in the setting of metastatic breast cancer. As expected, systemic therapies were applied before and also after SBRT in the vast majority of cases in the considered studies (Table 1). It is currently unclear whether there may be patients with a favorable prognosis and a low propensity for further systemic spread (i.e., metachronous oligorecurrence with a long treatment-free interval), where SBRT may be used as the sole treatment. In addition, it is not clear whether SBRT to oligoprogressive sites may allow for continuation of systemic therapy beyond progression. Here, however, it should be mentioned again that local ablative therapy of the metastases per se was recently shown by Steenbruggen et al. to be a favorable prognostic factor, independent of the systemic treatment [34]. However, when interpreting the retrospective observational study of Steenbruggen et al., a possible bias must be taken into account.
When combining SBRT and concomitant systemic therapy, possible interactions in terms of toxicity need to be considered. There is a lack of prospective clinical trials in this regard. A systematic review published in 2017 provides an overview of toxicity data of SBRT in combination with targeted agents and immunotherapy [39]. There were signs of potentially increased toxicity of SBRT in combination with EGFR-targeting tyrosine kinase inhibitors and bevacizumab. For CDK4/6 inhibitors there is conflicting evidence, with some reports of increased toxicity; however, these mostly included patients treated with standard treatment techniques and not SBRT [40].
There has been growing interest in the combination of radiotherapy and immunotherapy, also in breast cancer [41]. Currently, the use of immunotherapy in breast cancer outside of clinical trials is limited to patients with TNBC. A recent analysis conducted by the Food and Drug Administration did not show major increases in toxicity in patients treated with radiotherapy followed by immunotherapy when compared to immunotherapy alone based on data of more than 15000 patients of which approximately 3000 patients received radiotherapy [42].
A patterns-of-care survey among German-speaking countries established by the German Society for Radiation Oncology (DEGRO) working group for radiosurgery and stereotactic radiotherapy assessed patterns of care regarding combinations of systemic therapy and SBRT [43]. The majority of clinics pause targeted therapy or immunotherapy 1 week before and after SRT, irrespective of the type of systemic therapy given. However, a recent retrospective analysis of 158 patients by the same group did not show a difference in toxicity according to whether systemic therapy was interrupted during radiotherapy or not [44]. Overall, the rate of acute and chronic grade 3+ toxicity was below 5 %.
In clinical practice, an individual assessment based on treatment site, expected dose to organs at risk, type of systemic therapy, and risk of systemic disease progression is necessary. A multidisciplinary discussion is advised. Prolonged discontinuation of systemic therapy should be avoided wherever possible.
Primary tumor control
Older retrospective data suggest that there is a survival benefit for local treatment including surgery in stage IV breast cancer [45]. However, recent prospective randomized studies have shown that in the case of synchronous metastasis, radical therapy of the primary breast tumor does not provide a prognostic advantage [46,47,48]. However, these trials were not specifically conducted in patients with OMD. Furthermore, these trials did not include local treatment to metastatic sites.
In relevant studies, a controlled primary tumor is a prerequisite for SBRT of OMD in breast cancer [20, 24, 31]. In addition, only patients with controlled primary tumors were eligible for the randomized SABR-COMET study [29]. Generally, in a concept in which all pathological lesions are treated ablatively, it seems logical to also treat the primary ablatively.
Current clinical trials
An overview of randomized controlled trials enrolling only patients with breast cancer is given in Table 2. Radiotherapy is the predominant local treatment modality. Trials include patients with 3–5 metastases; however, three trials have additional limits including maximum size and/or volume of the metastatic lesions. Three out of five trials are limited to the first-line metastatic setting while only one trial restricts enrollment in terms of tumor biology. Progression-free and overall survival are the most common primary endpoints, although quality of life is used as a co-primary endpoint in the OLIGOMA trial [49].
Interestingly, there are also few trials on oligoprogressive breast cancer. The AVATAR trial (NCT04530513) is a phase II trial of patients with up to five oligoprogressive sites during treatment with endocrine therapy and a CDK4/6 inhibitor [50]. All patients will receive local ablative radiotherapy to the progressing lesions. The time to change of systemic therapy, measured from the commencement of SBRT to change in systemic therapy, was selected as the primary endpoint. Repeat local ablative radiotherapy is allowed in the case of new oligoprogressive lesions.
Details regarding radiotherapy treatment regimens are only available for NRG BR-002, AVATAR, and OLIGOMA. While SBRT in 1–5 fractions is mandated in NRG BR-002 and AVATAR, there is some flexibility to use more protracted regimens under specific clinical circumstances (e.g., large lesions, locoregional recurrences, spinal cord compression) in the OLIGOMA trial, in part due to the broader inclusion criteria [49]. Nevertheless, SBRT is strongly favored in the OLIGOMA trial.
Recommendations
Based on the discussed data, recommendations of the DEGRO breast cancer expert panel as well as the level of evidence depending on the classification/subclassification of OMD and clinical presentation are given in Table 3. An interdisciplinary tumor board should be involved.
Adequate classification of OMD [12] and judicious patient selection, also considering systemic therapy, are of high importance in this context.
Essential requirements for ablative radiotherapy are the implementation of adequate treatment planning, dosage, and dose prescription as well as the highest standard of technical quality, quality assurance, and documentation. Regarding these requirements, we refer to the recommendations and guidelines published by the DEGRO/DGMP [51, 52]. Careful consideration of organ dose constraints from consensus publications and international collaborations is strongly advised [53,54,55,56].
Conclusion
Local ablative radiotherapy is a promising treatment option for patients with oligometastatic breast cancer, offering high rates of local control with very limited toxicity. Currently, prospective cohort studies show very favorable results in selected patients. Randomized controlled trials are needed to demonstrate an additional benefit of SBRT in the setting of optimal systemic therapy. The use of SBRT in patients with oligometastatic breast cancer should always be discussed in a multidisciplinary conference.
References
Rubin P (1968) Comment: are metastases curable? JAMA 204(7):612–613
Hellman S, Weichselbaum RR (1995) Oligometastases. J Clin Oncol 13(1):8–10. https://doi.org/10.1200/JCO.1995.13.1.8
Nordlinger B, Sorbye H, Glimelius B et al (2013) Perioperative FOLFOX4 chemotherapy and surgery versus surgery alone for resectable liver metastases from colorectal cancer (EORTC 40983): long-term results of a randomised, controlled, phase 3 trial. Lancet Oncol 14(12):1208–1215. https://doi.org/10.1016/S1470-2045(13)70447-9
Pastorino U, Buyse M, Friedel G et al (1997) Long-term results of lung metastasectomy: prognostic analyses based on 5206 cases. J Thorac Cardiovasc Surg 113(1):37–49. https://doi.org/10.1016/s0022-5223(97)70397-0
Robertson DJ, Stukel TA, Gottlieb DJ et al (2009) Survival after hepatic resection of colorectal cancer metastases: a national experience. Cancer 115(4):752–759. https://doi.org/10.1002/cncr.24081
Treasure T, Fiorentino F, Scarci M et al (2012) Pulmonary metastasectomy for sarcoma: a systematic review of reported outcomes in the context of Thames cancer registry data. BMJ Open. https://doi.org/10.1136/bmjopen-2012-001736
Wei AC, Greig PD, Grant D et al (2006) Survival after hepatic resection for colorectal metastases: a 10-year experience. Ann Surg Oncol 13(5):668–676. https://doi.org/10.1245/ASO.2006.05.039
Tree AC, Khoo VS, Eeles RA et al (2013) Stereotactic body radiotherapy for oligometastases. Lancet Oncol 14(1):e28–37. https://doi.org/10.1016/S1470-2045(12)70510-7
Milano MT, Biswas T, Simone CB 2nd et al (2021) Oligometastases: history of a hypothesis. Ann Palliat Med 10(5):5923–5930. https://doi.org/10.21037/apm.2020.03.31
Milano MT, Katz AW, Zhang H et al (2019) Oligometastatic breast cancer treated with hypofractionated stereotactic radiotherapy: some patients survive longer than a decade. Radiother Oncol 131:45–51. https://doi.org/10.1016/j.radonc.2018.11.022
Makhlin I, Fox K (2020) Oligometastatic breast cancer: is this a curable entity? A contemporary review of the literature. Curr Oncol Rep 22(2):15. https://doi.org/10.1007/s11912-020-0867-2
Guckenberger M, Lievens Y, Bouma AB et al (2020) Characterisation and classification of oligometastatic disease: a European society for radiotherapy and oncology and European organisation for research and treatment of cancer consensus recommendation. Lancet Oncol 21(1):e18–e28. https://doi.org/10.1016/S1470-2045(19)30718-1
Willmann J, Badra EV, Adilovic S et al (2022) Evaluation of the prognostic value of the ESTRO EORTC classification of oligometastatic disease in patients treated with stereotactic body radiotherapy: a retrospective single center study. Radiother Oncol. https://doi.org/10.1016/j.radonc.2022.01.019
Pitroda SP, Weichselbaum RR (2019) Integrated molecular and clinical staging defines the spectrum of metastatic cancer. Nat Rev Clin Oncol 16(9):581–588. https://doi.org/10.1038/s41571-019-0220-6
Lievens Y, Guckenberger M, Gomez D et al (2020) Defining oligometastatic disease from a radiation oncology perspective: An ESTRO-ASTRO consensus document. Radiother Oncol 148:157–166. https://doi.org/10.1016/j.radonc.2020.04.003
Tsai CJ, Yang JT, Guttmann DM et al (2021) Consolidative use of radiotherapy to block (CURB) oligoprogression—interim analysis of the first randomized study of stereotactic body radiotherapy in patients with oligoprogressive metastatic cancers of the lung and breast. Int J Radiat Oncol Biol Phys 111(5):2. https://doi.org/10.1016/j.ijrobp.2021.09.014
David S, Tan J, Savas P et al (2020) Stereotactic ablative body radiotherapy (SABR) for bone only oligometastatic breast cancer: a prospective clinical trial. Breast 49:55–62. https://doi.org/10.1016/j.breast.2019.10.016
Scorsetti M, Franceschini D, De Rose F et al (2016) Stereotactic body radiation therapy: a promising chance for oligometastatic breast cancer. Breast 26:11–17. https://doi.org/10.1016/j.breast.2015.12.002
Lemoine P, Bruand M, Kammerer E et al (2021) Stereotactic body radiation therapy for oligometastatic breast cancer: a retrospective multicenter study. Front Oncol 11:736690. https://doi.org/10.3389/fonc.2021.736690
Trovo M, Furlan C, Polesel J et al (2018) Radical radiation therapy for oligometastatic breast cancer: results of a prospective phase II trial. Radiother Oncol 126(1):177–180. https://doi.org/10.1016/j.radonc.2017.08.032
Weykamp F, Konig L, Seidensaal K et al (2020) Extracranial stereotactic body radiotherapy in oligometastatic or oligoprogressive breast cancer. Front Oncol 10:987. https://doi.org/10.3389/fonc.2020.00987
Tan H, Cheung P, Louie AV et al (2021) Outcomes of extra-cranial stereotactic body radiotherapy for metastatic breast cancer: treatment indication matters. Radiother Oncol 161:159–165. https://doi.org/10.1016/j.radonc.2021.06.012
Viani GA, Gouveia AG, Louie AV et al (2021) Stereotactic body radiotherapy to treat breast cancer oligometastases: a systematic review with meta-analysis. Radiother Oncol 164:245–250. https://doi.org/10.1016/j.radonc.2021.09.031
Chalkidou A, Macmillan T, Grzeda MT et al (2021) Stereotactic ablative body radiotherapy in patients with oligometastatic cancers: a prospective, registry-based, single-arm, observational, evaluation study. Lancet Oncol 22(1):98–106. https://doi.org/10.1016/S1470-2045(20)30537-4
Gomez DR, Tang C, Zhang J et al (2019) Local consolidative therapy vs. maintenance therapy or observation for patients with oligometastatic non-small-cell lung cancer: long-term results of a multi-institutional, phase II, randomized study. J Clin Oncol 37(18):1558–1565. https://doi.org/10.1200/JCO.19.00201
Iyengar P, Wardak Z, Gerber DE et al (2018) Consolidative radiotherapy for limited metastatic non-small-cell lung cancer: a phase 2 randomized clinical trial. JAMA Oncol 4(1):e173501. https://doi.org/10.1001/jamaoncol.2017.3501
Milano MT, Katz AW, Zhang H et al (2012) Oligometastases treated with stereotactic body radiotherapy: long-term follow-up of prospective study. Int J Radiat Oncol Biol Phys 83(3):878–886. https://doi.org/10.1016/j.ijrobp.2011.08.036
Ost P, Reynders D, Decaestecker K et al (2018) Surveillance or metastasis-directed therapy for oligometastatic prostate cancer recurrence: a prospective, randomized, multicenter phase II trial. J Clin Oncol 36(5):446–453. https://doi.org/10.1200/JCO.2017.75.4853
Palma DA, Olson R, Harrow S et al (2019) Stereotactic ablative radiotherapy versus standard of care palliative treatment in patients with oligometastatic cancers (SABR-COMET): a randomised, phase 2, open-label trial. Lancet 393(10185):2051–2058. https://doi.org/10.1016/S0140-6736(18)32487-5
Palma DA, Olson R, Harrow S et al (2020) Stereotactic ablative radiotherapy for the comprehensive treatment of oligometastatic cancers: long-term results of the SABR-COMET phase II randomized trial. J Clin Oncol 38(25):2830–2838. https://doi.org/10.1200/JCO.20.00818
Dawood S, Broglio K, Ensor J et al (2010) Survival differences among women with de novo stage IV and relapsed breast cancer. Ann Oncol 21(11):2169–2174. https://doi.org/10.1093/annonc/mdq220
Wijetunga NA, Dos Anjos CH, Zhi WI et al (2021) Long-term disease control and survival observed after stereotactic ablative body radiotherapy for oligometastatic breast cancer. Cancer Med 10(15):5163–5174. https://doi.org/10.1002/cam4.4068
Onal C, Guler OC, Yildirim BA (2018) Treatment outcomes of breast cancer liver metastasis treated with stereotactic body radiotherapy. Breast 42:150–156. https://doi.org/10.1016/j.breast.2018.09.006
Steenbruggen TG, Schaapveld M, Horlings HM et al (2021) Characterization of oligometastatic disease in a real-world nationwide cohort of 3447 patients with de novo metastatic breast cancer. JNCI Cancer Spectr 5(3):pkab10. https://doi.org/10.1093/jncics/pkab010
Patel PH, Palma D, McDonald F et al (2019) The dandelion dilemma revisited for oligoprogression: treat the whole lawn or weed selectively? Clin Oncol (R Coll Radiol) 31(12):824–833. https://doi.org/10.1016/j.clon.2019.05.015
Guth U, Magaton I, Huang DJ et al (2014) Primary and secondary distant metastatic breast cancer: two sides of the same coin. Breast 23(1):26–32. https://doi.org/10.1016/j.breast.2013.10.007
Holleczek B, Stegmaier C, Radosa JC et al (2019) Risk of loco-regional recurrence and distant metastases of patients with invasive breast cancer up to ten years after diagnosis—results from a registry-based study from Germany. BMC Cancer 19(1):520. https://doi.org/10.1186/s12885-019-5710-5
Kucharczyk MJ, Parpia S, Walker-Dilks C et al (2017) Ablative therapies in metastatic breast cancer: a systematic review. Breast Cancer Res Treat 164(1):13–25. https://doi.org/10.1007/s10549-017-4228-2
Kroeze SG, Fritz C, Hoyer M et al (2017) Toxicity of concurrent stereotactic radiotherapy and targeted therapy or immunotherapy: a systematic review. Cancer Treat Rev 53:25–37. https://doi.org/10.1016/j.ctrv.2016.11.013
Bosacki C, Bouleftour W, Sotton S et al (2021) CDK 4/6 inhibitors combined with radiotherapy: a review of literature. Clin Transl Radiat Oncol 26:79–85. https://doi.org/10.1016/j.ctro.2020.11.010
Ho AY, Wright JL, Blitzblau RC et al (2020) Optimizing radiation therapy to boost systemic immune responses in breast cancer: a critical review for breast radiation oncologists. Int J Radiat Oncol Biol Phys 108(1):227–241. https://doi.org/10.1016/j.ijrobp.2020.05.011
Anscher MS, Arora S, Weinstock C et al (2022) Association of radiation therapy with risk of adverse events in patients receiving immunotherapy: a pooled analysis of trials in the US food and drug administration database. JAMA Oncol. https://doi.org/10.1001/jamaoncol.2021.6439
Kroeze SGC, Fritz C, Basler L et al (2019) Combination of stereotactic radiotherapy and targeted therapy: patterns-of-care survey in German-speaking countries. Strahlenther Onkol 195(3):199–206. https://doi.org/10.1007/s00066-018-01422-5
Kroeze SGC, Fritz C, Schaule J et al (2021) Continued versus interrupted targeted therapy during metastasis-directed stereotactic radiotherapy: a retrospective multi-center safety and efficacy analysis. Cancers (Basel). https://doi.org/10.3390/cancers13194780
Harris E, Barry M, Kell MR (2013) Meta-analysis to determine if surgical resection of the primary tumour in the setting of stage IV breast cancer impacts on survival. Ann Surg Oncol 20(9):2828–2834. https://doi.org/10.1245/s10434-013-2998-2
Lane WO, Thomas SM, Blitzblau RC et al (2019) Surgical resection of the primary tumor in women with de novo stage IV breast cancer: contemporary practice patterns and survival analysis. Ann Surg 269(3):537–544. https://doi.org/10.1097/SLA.0000000000002621
Badwe R, Hawaldar R, Nair N et al (2015) Locoregional treatment versus no treatment of the primary tumour in metastatic breast cancer: an open-label randomised controlled trial. Lancet Oncol 16(13):1380–1388. https://doi.org/10.1016/S1470-2045(15)00135-7
Khan SA, Zhao F, Solin LJ, Goldstein LJ (2020) A randomized phase III trial of systemic therapy plus early local therapy versus systemic therapy alone in woman with de-novo stage IV breast cancer: a trial of the ECOg-ACRIN research group (E2108). J Clin Oncol. https://doi.org/10.1200/JCO.2020.38.18_suppl.LBA2
Krug D, Vonthein R, Illen A et al (2021) Metastases-directed radiotherapy in addition to standard systemic therapy in patients with oligometastatic breast cancer: study protocol for a randomized controlled multi-national and multi-center clinical trial (OLIGOMA). Clin Transl Radiat Oncol 28:90–96. https://doi.org/10.1016/j.ctro.2021.03.012
Alomran R, White M, Bruce M et al (2021) Stereotactic radiotherapy for oligoprogressive ER-positive breast cancer (AVATAR). BMC Cancer 21(1):303. https://doi.org/10.1186/s12885-021-08042-w
Schmitt D, Blanck O, Gauer T et al (2020) Technological quality requirements for stereotactic radiotherapy : expert review group consensus from the DGMP working group for physics and technology in stereotactic radiotherapy. Strahlenther Onkol 196(5):421–443. https://doi.org/10.1007/s00066-020-01583-2
Guckenberger M, Baus WW, Blanck O et al (2020) Definition and quality requirements for stereotactic radiotherapy: consensus statement from the DEGRO/DGMP working group stereotactic radiotherapy and radiosurgery. Strahlenther Onkol 196(5):417–420. https://doi.org/10.1007/s00066-020-01603-1
Gerhard SG, Palma DA, Arifin AJ et al (2021) Organ at risk dose constraints in SABR: a systematic review of active clinical trials. Pract Radiat Oncol 11(4):e355–e365. https://doi.org/10.1016/j.prro.2021.03.005
Timmerman R (2022) A story of hypofractionation and the table on the wall. Int J Radiat Oncol Biol Phys 112(1):4–21. https://doi.org/10.1016/j.ijrobp.2021.09.027
Hanna GG, Murray L, Patel R et al (2018) UK consensus on normal tissue dose constraints for stereotactic radiotherapy. Clin Oncol (R Coll Radiol) 30(1):5–14. https://doi.org/10.1016/j.clon.2017.09.007
Benedict SH, Yenice KM, Followill D et al (2010) Stereotactic body radiation therapy: the report of AAPM task group 101. Med Phys 37(8):4078–4101. https://doi.org/10.1118/1.3438081
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M.D. Piroth, D. Krug, P. Feyer, R. Baumann, S. Combs, M.-N. Duma, J. Dunst, G. Fastner, R. Fietkau, M. Guckenberger, W. Haase, W. Harms, T. Hehr, F. Sedlmayer, R. Souchon, V. Strnad, and W. Budach declare that they have no competing interests.
Ethical standards
For this article no studies with human participants or animals were performed by any of the authors. All studies mentioned were in accordance with the ethical standards indicated in each case.
Additional information
Marc D. Piroth and David Krug contributed equally to this work
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Piroth, M.D., Krug, D., Feyer, P. et al. Oligometastasis in breast cancer—current status and treatment options from a radiation oncology perspective. Strahlenther Onkol 198, 601–611 (2022). https://doi.org/10.1007/s00066-022-01938-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-022-01938-x