Abstract
Purpose
Hypofractionated radiotherapy for prostate cancer is well established for definitive treatment, but not well defined in the postoperative setting. The purpose of this analysis was to assess oncologic outcomes and toxicity in a large cohort of patients treated with conventionally fractionated three-dimensional (3D) conformal radiotherapy (CF) and hypofractionated volumetric modulated arc therapy (HF) after radical prostatectomy.
Methods
Between 1994 and 2019, a total of 855 patients with prostate carcinoma were treated by postoperative radiotherapy using CF (total dose 65–72 Gy, single fraction 1.8–2 Gy) in 572 patients and HF (total dose 62.5–63.75 Gy, single fraction 2.5–2.55 Gy) in 283 patients. The association of treatment modality with biochemical control, overall survival (OS), and gastrointestinal (GI) and genitourinary (GU) toxicity was assessed using logistic and Cox regression analysis.
Results
There was no difference between the two modalities regarding biochemical control rates (77% versus 81%, respectively, for HF and CF at 24 months and 58% and 64% at 60 months; p = 0.20). OS estimates after 5 years: 95% versus 93% (p = 0.72). Patients undergoing HF had less frequent grade 2 or higher acute GI or GU side effects (p = 0.03 and p = 0.005, respectively). There were no differences in late GI side effects between modalities (hazard ratio 0.99). Median follow-up was 23 months for HF and 72 months for CF (p < 0.001).
Conclusion
For radiation therapy of resected prostate cancer, our analysis of this largest single-centre cohort (n = 283) treated with hypofractionation with advanced treatment techniques compared with conventional fractionation did not yield different outcomes in terms of biochemical control and toxicities. Prospective investigating of HF is merited.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Radical prostatectomy with or without lymphadenectomy is a widely used therapeutic option for localized prostate cancer (PCA) [1, 2]. Despite definitive treatment, about 30% of patients experience biochemical recurrence [3]. External beam radiotherapy has shown a significant oncologic advantage in terms of reducing these recurrences in both the adjuvant and salvage settings [1, 4, 5].
Hypofractionation (HF) provides a logistic advantage of shorter overall treatment time, allowing more patients to be treated with given resources. This also shortens waiting times, benefitting patients and providers alike, in addition to lowering costs per treatment [6].
In a primary setting, HF for PCA is already well established, both in terms of oncological efficacy and safety [7, 8]. In the postoperative setting, however, no large randomized prospective studies on postoperative HF have been published yet. Some retrospective studies on postoperative HF have been published [9,10,11,12,13,14,15], but have included only small cohorts.
In 2013, our department was facing steadily increasing numbers of patients with limited resources. Therefore, we implemented a moderately hypofractionated schedule with a total of 62.5 Gy in 25 fractions instead of a 66 Gy total dose in 33 fractions, reducing treatment times by 25% and setting us up to treat a larger collective of postoperative prostate cancer patients, while using the same number of linear accelerators. To evaluate and compare this regimen with our prior treatment, we collected data regarding tumour control and side effects.
In 2014, Cozzarini et al. [11] showed in the presently largest available retrospective study (n = 1176) that moderate HF, administered with helical tomotherapy (n = 247), leads to more frequent severe (G3 or higher) late genitourinary (GU) side effects (18% at 5 years) compared with conventional fractionation (CF) (n = 929, 7% at 5 years) in postoperative radiotherapy of prostate cancer. In the absence of prospective evidence from randomized trials, these results may have contributed to the limited enthusiasm for HF in the postoperative setting.
The goal of our retrospective study was therefore to report biochemical control, survival, and acute and late gastrointestinal (GI) and GU toxicity in a large cohort of consecutively treated patients after radical prostatectomy, focusing on differences between CF and the largest hitherto reported HF cohort.
Materials and methods
The analysis of our patient cohort was accepted by the local ethics committee (EK Nr: 1226/2020).
Patient population
Patients included were treated between January 1994 and December 2019 at the Department of Radiation Oncology. The following inclusion criteria had to be met:
-
Prostate cancer treated with radical prostatectomy (RPE) with or without lymph node dissection (LND),
-
pT2‑4 without evidence of lymph node involvement or distant metastases (c/pN0M0),
-
Documented preoperative, postoperative, and preirradiation prostate specific antigen (PSA) values and
-
Adjuvant or salvage radiotherapy: salvage RT was defined as PSA persisting or rising ≥ 0.2 ng/mL after surgery; patients with preradiation PSA ≤ 0.2 ng/mL were classified as having received adjuvant radiotherapy.
Interventions
Patients were treated with either conventionally fractionated three-dimensional (3D) conformal radiotherapy or hypofractionated volumetric modulated arc therapy, depending on the year of treatment. The switch between modalities happened near the end of 2013. For both groups, target volume definition was performed using computed tomography (CT) and magnetic resonance imaging (MRI). The target volume of the prostatic region for all patients was defined as described by Bolla et al. as “a volume that included the surgical limits from the seminal vesicles to the apex with a security margin to encompass sub-clinical disease in the periprostatic area” [16]. Due to our long observation range, patients were treated with either a 3D conformal 4‑field box or the Volumetric Intensity Modulated Arc Therapy (VMAT) technique in supine position. Planning target volume (PTV) margins were 7 mm for VMAT and 12 mm for 3D conformal radiotherapy. For 3D conformal radiotherapy, constraints were a coverage of 100% of the prescribed dose to 90% of the PTV. No constraints for organs at risk were assessed at that time. For the VMAT technique, constraints are listed in Appendix 1. Assumed α/β ratios, in coordination with our radiobiology department, were 3 Gy for the rectum [17] and 5 Gy for the bladder. As the bowel bag is treated with 2 Gy per fraction and femoral heads are of low priority in VMAT technique radiotherapy, no α/β ratios were assumed. Patients had to drink 250 mL of water 30 min before treatment and were told not to urinate for 1 h before treatment. Therefore, they were assumed to be treated with a full bladder. In the 3D conformal radiotherapy era, image-guided radiotherapy was performed with daily digitally reconstructed radiography. In the hypofractionated era, image-guided radiotherapy was performed by the use of daily ExacTrac (Brainlab, Munich, Germany) images.
For CF, doses were 65–67 Gy for patients without clinical recurrence and 70–72 Gy for patients with clinical recurrence, both at 1.8–2 Gy per fraction. For moderate HF, prescribed doses were 62.5 Gy with a single dose of 2.5 Gy in the absence of clinical recurrence, and 63.75 Gy with 2.55 Gy per fraction was applied to clinical recurrences. Assuming an α/β value of 3 Gy for prostate cancer, this equals 68.8 Gy EQD2Gy for the single dose of 2.5 Gy and 70.8 Gy for the single dose of 2.55 Gy. If the α/β value is supposed to be 1.5 Gy, EQD2Gy values were 71.4 Gy and 73.8 Gy, respectively. Patients at higher risk for lymph-node involvement received irradiation of the pelvic lymph nodes, in case the formula described by Roach et al. yielded a risk of positive lymph nodes of ≥ 15% [18]. Doses to the lymph nodes varied between 45 and 50 Gy with 1.8 to 2 Gy per fraction. The target volume included the external, internal, and common iliac lymph node stations, up to the aortic bifurcation (usually L4/5). Lymph node staging was performed via either LND or CT scan.
Androgen-deprivation therapy (ADT) was administered at the discretion of the attending urologist.
Outcomes
The primary end point was biochemical control after radiotherapy. Secondary end points were OS, as well as genitourinary and gastrointestinal toxicity according to the Radiation Therapy Oncology Group (RTOG). PSA levels, as well as GI and GU side effects using RTOG criteria [19], were assessed by the radiation oncologist during routine follow-up. The failure of biochemical control was defined as a rise of PSA levels > 0.2 ng/mL [20]. Patients were followed up immediately after therapy, 3 months after the end of therapy, 1 year after therapy, and annually thereafter. Survival data with the reference date December 31, 2019, were retrieved from the population census (Statistik Austria).
Statistical analysis
Patient baseline characteristics were compared between HF and CF with absolute and relative frequencies and the Χ2 test for qualitative variables, and the mean, standard deviation (SD), median and two-sample t‑test or Wilcoxon test for quantitative variables (Table 1). To assess the influence of baseline characteristics on time to biochemical control as the primary end point, univariate Cox regression analyses were performed and hazard ratios (HR), 95% confidence intervals (CI), and p-values were reported. All baseline variables with p < 0.05 were further considered in a multivariable model. Predefined subgroup analyses were performed for Roach > 15% and lymph node irradiation, and sensitivity analyses were conducted, censoring all patients with at 4‑year follow-up (due to unequal follow-up times between groups). Further Cox regressions were performed for time to death for overall survival, and time to late maximum GI or GU toxicity (grade 2 or higher considered as event). Logistic regression analyses were computed to investigate the influence of HF versus CF on acute maximum GI or GU toxicity (grade 0–1 versus 2 or more). Due to the exploratory and retrospective character of the study, statistical significance was considered at p 0.05, but not in a confirmatory manner, and no adjustment for multiplicity was performed. All analyses were done using the R program (R 4.0.3).
Results
Patient characteristics are shown in Table 1. There was a difference in the administration of ADT as well as a higher percentage of patients with pelvic lymph node irradiation in patients treated with moderate HF compared with patients treated with CF. Patients receiving HF were slightly older (2.3 years) and the time between RPE and RT increased, being 24 months for HF and 13 months for CF (16 months for both groups combined). Median follow-up was 23 months for HF and 72 months for CF (42 months for both groups combined).
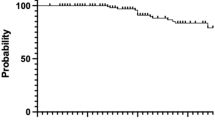
The results regarding biochemical control for all patients are displayed in Fig. 1. Biochemical control rates at 2 years were 77% for HF and 81% for CF, and at 5 years were 58% and 64%, respectively (p = 0.20). We also performed subgroup sensitivity for lymph node irradiation, as well as Roach > 15% and ≤ 15%. In none of these comparisons were we able to detect any significant difference (p = 0.25, 0.11, 0.41, and 0.71, respectively). Due to the relatively shorter follow-up in the HF group, we also performed a sensitivity analysis and censored patients with a follow-up after 48 months; this also revealed no significant differences between the two treatments (4-year biochemical control rates: 61% after HF and 70% after CF, p = 0.15).
In a subgroup analysis for adjuvant and salvage indications, no significant influence of fractionation on time to failure of biochemical control was found for both groups (Table 2), but of note, the sample size was smaller with only 8 events (69 censored) in the HF group, compared with 36 events (150 censored) in the CF group. We also performed Kaplan–Meier tests for all patients treated with adjuvant and salvage indications. In the adjuvant group, we observed biochemical control rates for the HF group of 89% and 58% after 2 and 5 years, respectively, with only 5 patients at risk after 5 years, and 92% and 81% for the CF group at 2 and 5 years, respectively. In the salvage group, control rates after 2 and 5 years, respectively, were 73% and 57% in the HF group, and 75% and 54% in the CF group. No significant differences were observed (adjuvant p = 0.23 and salvage p = 0.68).
Overall survival at 5 years was 93% and 95%, and disease-specific survival at 5 years was 97% and 99%, respectively, for CF and HF. Both differences were not significant (p = 0.72 and 0.34).
The highest reported grades of side effects during treatment are displayed in Table 3. Only one patient from the CF group developed a grade 4 late GU toxicity, while none were observed in the HF group. For analytic purposes, we grouped toxicities of grade 0 and 1, and of grade 2 or higher. Acute GI side effects were significantly lower (p = 0.02) in patients treated with HF. For acute GU side effects, we also found a significant difference in favour of HF (p = 0.03), and a similar result for late GI and GU side effects (p = 0.03 and 0.01 in favour of HF, respectively). Overall, the majority of patients showed no or mild side effects, especially regarding late side effects.
Table 4 displays our results regarding the time to onset of late toxicities with an RTOG grade of 2 and higher. The common denominator for late toxicity was any acute toxicity of some kind. For GI toxicity, no further significant parameter was observed and therefore, no multivariable analysis was performed. In terms of late GU toxicity, HF showed higher late GU toxicity only in univariable analysis. Adjusting for age and acute GU toxicity, the difference between HF and CF vanished.
Discussion
With this study, we want to share our experiences in the treatment of a large postoperative prostate cancer patient cohort with moderate HF. To become a clinically recommendable treatment option, HF should yield equally effective oncological results compared with CF, and side effects during and after treatment should be comparable as well.
As for biochemical control rates, our data show two very similar curves with no significant difference. Our results with rates of 58% for HF and 64% for CF after 5 years are in accord with Tramacere et al. [12] and Kruser et al. [13], who reported rates of 67% for moderate HF after 5 and 4 years in initially 69 and 108 patients, respectively. More recently, these results were confirmed by Franzese et al., who reported rates of 72.3% after 5 years [14]. Macchia et al. reported a rate of 87% at 5 years for moderate HF [15]. However, almost 80% of their reported 124 patient collective received ADT, making a direct comparison with our HF collective, with only 14% receiving ADT, difficult. In summary, neither our results with no significant difference, nor the reported results in the literature with HF biochemical control rates being even higher than those for CF, show an inferiority of HF. However, caution is advised, as our median follow-up for the HF group was only 23 months and our treatment groups were imbalanced regarding ADT prescription, Gleason score, Roach formula results, and radiotherapy indication, favouring the CF group, and lymph node irradiation, favouring the HF group concerning biochemical control rates. However, none of the performed sensitivity analyses changed any of the results. The slightly increased amount of salvage irradiation performed in the HF group might also be an indicator of a worse outcome, as corroborated by several studies [21, 22]. The large difference concerning lymph node irradiation can be explained by a more reluctant practice in pre-VMAT times. Nevertheless, no significant difference between the two treatment groups regarding failure of biochemical control could be detected.
Our results have to be taken with caution, as our HF group was exclusively treated with the VMAT technique and had a 67% inclusion of pelvic lymph nodes, whereas our CF group was treated with 3D conformal radiotherapy and had only 34% inclusion of lymph nodes. In addition, the safety margins were 7 mm for the HF group and 12 mm for the CF group, leading to even more potential toxicity. This was due to the consecutive cohort design of our study, as our department changed not only the dose prescription, but also the irradiation technique at the same time, leading to treatment- and time-disjunct groups.
An increased inclusion of lymph nodes would suggest higher toxicity for HF a priori. However, in terms of acute side effects, we observed significantly lower GI and GU side effects after HF in the VMAT technique compared with CF with a 3D conformal 4‑field-box. This also matches the results of Barra et al. [10], Kruser et al. [13], and the authors of the PRIAMOS‑1 trial [23] who, with the exception of Kruser, also reported low acute toxicity after HF, using Common Terminology for Adverse Events (CTCAE) grading.
For late toxicity, treatment was overall well received, as reported in Table 3. This again is noteworthy, as 67% of the HF patients also received pelvic lymph node irradiation, a known cause of increased late side effects [24, 25]. Regarding the influence of irradiation technique, a British study with over 3000 patients described no significant difference in late GI and GU toxicity between 3D conformal and intensity-modulated radiotherapy [26] after RPE. However, the used doses were low, ranging between 60 and 66 Gy in the CF and 52.5 and 55 Gy in 20 fractions in the HF arm.
Regarding late GU side effects in postoperative HF, it is most important to address Cozzarini et al. [11], who reported a 5-year CTCAE grade 3 GU toxicity rate of 18%, but they administered higher doses compared to the doses administered to our cohort. In addition, improvements in surgery might be reflected in the shift to more postoperative radiotherapy in salvage settings, as indicated in Table 1. Moreover, in the study by Cozzarini et al., the median time between RPE and RT was 5 months in the HF group, whereas our median duration was 24 months.
The most important limitation of our study is its retrospective nature and, more specifically, having observed and compared patient collectives in different periods of time. Moreover, our patient collectives are not balanced, especially regarding inclusion of pelvic lymph nodes, ADT, irradiation technique, Gleason score, and irradiation indication. Moreover, the follow-up in our HF group was relatively short, with a median of 23 months. Due to these differences, we performed various sensitivity subgroup analyses and adjusted analyses where possible to detect any signals of differences in outcomes. However, no such signals could be detected.
As for strengths, to our knowledge this is the largest study on postoperative HF to date, with almost 300 patients included in this treatment group. Our study is monocentric, and a single attending physician has been in charge of treatment, resulting in highly homogeneous treatment delivery and toxicity scoring. However, prospective randomized trials confirming our results regarding HF postoperative radiotherapy are needed.
Conclusion
Moderate HF might become an option for postoperative prostate cancer patients regarding biochemical control, pending prospective clinical trials. Concerning GI and especially GU toxicities, HF applied with the VMAT technique is well tolerated, and our results challenge those in important prior literature regarding this topic.
References
Cornford P et al (2021) EAU-EANM-ESTRO-ESUR-SIOG guidelines on prostate cancer. Part II—2020 update: treatment of relapsing and metastatic prostate cancer. Eur Urol 79:263–282
Mohler JL et al (2019) NCCN clinical practice guidelines in oncology—prostate cancer version 4.2019. J Natl Compr Canc Netw. https://doi.org/10.6004/jnccn.2019.0023
Van den Broeck T, van den Bergh RCN, Arfi N (2019) Prognostic value of biochemical recurrence following treatment with curative intent for prostate cancer : a systematic review. Eur Urol 75:967–987
Kneebone A et al (2020) Adjuvant radiotherapy versus early salvage radiotherapy following radical prostatectomy (TROG 08.03/ANZUP RAVES): a randomised, controlled, phase 3, non-inferiority trial. Lancet Oncol 21:1331–1340
Parker CC et al (2020) Timing of radiotherapy after radical prostatectomy (RADICALS-RT): a randomised, controlled phase 3 trial. Lancet 396:1413–1421
Yu JB (2017) Hypofractionated radiotherapy for prostate cancer: further evidence to tip the scales. J Clin Oncol 35:1867–1869
Dearnaley D et al (2016) Conventional versus hypofractionated high-dose intensity-modulated radiotherapy for prostate cancer: 5‑year outcomes of the randomised, non-inferiority, phase 3 CHHiP trial. Lancet Oncol 17:1047–1060
Sharfo AWM et al (2018) Late toxicity in the randomized multicenter HYPRO trial for prostate cancer analyzed with automated treatment planning. Radiother Oncol 128:349–356
Cuccia F et al (2018) Hypofractionated postoperative helical tomotherapy in prostate cancer: a mono-institutional report of toxicity and clinical outcomes. Cancer Manag Res 10:5053–5060
Barra S et al (2018) Moderate hypofractionated radiotherapy after prostatectomy for cancer patients: toxicity and clinical outcome. Cancer Manag Res 10:473–480
Cozzarini C et al (2014) Higher-than-expected severe (grade 3–4) late urinary toxicity after postprostatectomy hypofractionated radiotherapy: a single-institution analysis of 1176 patients. Eur Urol 66:1024–1030
Tramacere F et al (2018) Postoperative hypofractionated radiotherapy for prostate cancer. Anticancer Res 38:2951–2956
Kruser TJ et al (2011) Early hypofractionated salvage radiotherapy for postprostatectomy biochemical recurrence. Cancer 117:2629–2636
Franzese C et al (2020) Moderate hypofractionated radiotherapy for post-operative treatment of prostate cancer: long-term outcome and pattern of toxicity. Strahlenther Onkol. https://doi.org/10.1007/s00066-020-01691-z
Macchia G et al (2017) Hypofractionated postoperative IMRT in prostate carcinoma: a phase I/II study. Anticancer Res 37:5821–5828
Bolla M et al (2005) Postoperative radiotherapy after radical prostatectomy: a randomised controlled trial (EORTC trial 22911). Lancet 366:572–578
Rana S, Cheng C (2014) Radiobiological impact of planning techniques for prostate cancer in terms of tumor control probability and normal tissue complication probability. Ann Med Health Sci Res 4:167
Roach M et al (2006) Whole-pelvis, “mini-pelvis,” or prostate-only external beam radiotherapy after neoadjuvant and concurrent hormonal therapy in patients treated in the radiation therapy oncology group 9413 trial. Int J Radiat Oncol Biol Phys 66:647–653
Cox JD, Stetz J, Pajak TF (1995) Toxicity criteria of the radiation therapy oncology group (RTOG) and the European organization for research and treatment of cancer (EORTC). Int J Radiat Oncol Biol Phys 31:1341–1346
Cookson MS et al (2007) Variation in the definition of biochemical recurrence in patients treated for localized prostate cancer: the American urological association prostate guidelines for localized prostate cancer update panel report and recommendations for a standard in the re. J Urol 177:540–545
Hwang WL et al (2018) Comparison between adjuvant and early-salvage postprostatectomy radiotherapy for prostate cancer with adverse pathological features. JAMA Oncol 4:1–8
Ost P, De Troyer B, Fonteyne V, Oosterlinck W, De Meerleer G (2011) A matched control analysis of adjuvant and salvage high-dose postoperative intensity-modulated radiotherapy for prostate cancer. Int J Radiat Oncol Biol Phys 80:1316–1322
Katayama S et al (2014) Hypofractionated IMRT of the prostate bed after radical prostatectomy: acute toxicity in the PRIAMOS‑1 trial. Int J Radiat Oncol Biol Phys 90:926–933
Waldstein C, Dörr W, Pötter R, Widder J, Goldner G (2018) Postoperative radiotherapy for prostate cancer: morbidity of local-only or local-plus-pelvic radiotherapy. Strahlenther Onkol 194:23–30
Murthy V et al (2020) Late toxicity and quality of life with prostate only or whole pelvic radiation therapy in high risk prostate cancer (POP-RT): a randomised trial. Radiother Oncol 145:71–80
Sujenthiran A et al (2018) Treatment-related toxicity in men who received intensity-modulated versus 3D-conformal radiotherapy after radical prostatectomy: a national population-based study. Radiother Oncol 128:357–363
Acknowledgements
Special thanks to Marion Moll for English language editing.
Funding
Open access funding provided by Medical University of Vienna.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M. Moll, D. D’Andrea, A. Zaharie, B. Grubmüller, C. Paschen, S. Zehetmayer, S.F. Shariat, J. Widder and G. Goldner declare that they have no competing interests.
Appendix
Appendix
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Moll, M., D’Andrea, D., Zaharie, A. et al. Comparative effectiveness of moderate hypofractionation with volumetric modulated arc therapy versus conventional 3D-radiotherapy after radical prostatectomy. Strahlenther Onkol 198, 719–726 (2022). https://doi.org/10.1007/s00066-022-01909-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-022-01909-2