Abstract
Background
Non-small-cell lung cancer (NSCLC) is a major cause of cancer-related death globally. Endothelial PAS domain-containing protein 1 (EPAS1) is a homolog of the hypoxia-inducible factor 1α and has been reported to confer tyrosine kinase inhibitor (TKI) resistance in NSCLC, but its role in peritoneal carcinomatosis of NSCLC is unknown.
Methods
PC14HM, a high metastatic potential subline of NSCLC cell line PC14, was derived. Stable shRNA knockdown of EPAS1 was then established in PC14HM cells and subjected to assessment regarding the effects on proliferation and viability, xenograft tumor growth, metastatic potential, mesothelial–mesenchymal transition (MMT)-related characteristics and peritoneal carcinomatosis in a mouse model.
Results
EPAS1 expression was elevated in PC14HM cells. Knockdown of EPAS1 inhibited the proliferation and viability of PC14HM cells in vitro and suppressed tumorigenesis in vivo. In addition, the metastatic features and in vitro productions of MMT-inducing factors in PC14HM cells was also associated with EPAS1. More importantly, knockdown of EPAS1 drastically suppressed peritoneal carcinomatosis of PC14HM cells in vivo.
Conclusion
EPAS1 promotes peritoneal carcinomatosis of NSCLC through enhancement of MMT and could therefore serve as a prognostic marker or a therapeutic target in treating NSCLC, particularly in patients with peritoneal carcinomatosis.







Similar content being viewed by others
Abbreviations
- EGFR:
-
Epidermal growth factor receptor
- ELISA:
-
Enzyme-linked immunosorbent assay
- EPAS1:
-
Endothelial PAS domain-containing protein 1
- HGF:
-
Hepatocyte growth factor
- IL:
-
Interleukin
- MET:
-
Hepatocyte growth factor receptor
- MMT:
-
Mesothelial–mesenchymal transition
- NSCLC:
-
Non-small-cell lung cancer
- PCI:
-
Peritoneal carcinomatosis index
- PCR:
-
Polymerase chain reaction
- SCLC:
-
Small-cell lung cancer
- SD:
-
Standard deviation
- TGF-β1:
-
Transforming growth factor-β1
- TKI:
-
Tyrosine kinase inhibitor
- TNF‑α:
-
Tumour necrosis factor‑α
References
Molina JR, Yang P, Cassivi SD, Schild SE, Adjei AA (2008) Non-small cell lung cancer: epidemiology, risk factors, treatment, and survivorship. Mayo Clin Proc 83:584–594. https://doi.org/10.4065/83.5.584
Duma N, Santana-Davila R, Molina JR (2019) Non-small cell lung cancer: epidemiology, screening, diagnosis, and treatment. Mayo Clin Proc 94:1623–1640. https://doi.org/10.1016/j.mayocp.2019.01.013
Yang P, Allen MS, Aubry MC, Wampfler JA, Marks RS, Edell ES, Thibodeau S, Adjei AA, Jett J, Deschamps C (2005) Clinical features of 5,628 primary lung cancer patients: experience at Mayo Clinic from 1997 to 2003. Chest 128:452–462. https://doi.org/10.1378/chest.128.1.452
Harjes U (2017) Non-small cell lung cancer: where there’s smoke. Nat Rev Cancer 17:634–635. https://doi.org/10.1038/nrc.2017.95
Herbst RS, Morgensztern D, Boshoff C (2018) The biology and management of non-small cell lung cancer. Nature 553:446–454. https://doi.org/10.1038/nature25183
Wang Y, Chen Z (2020) Mutation detection and molecular targeted tumor therapies. STEMedicine 1:e11. https://doi.org/10.37175/stemedicine.v1i1.11
Saintigny P, Burger JA (2012) Recent advances in non-small cell lung cancer biology and clinical management. Discov Med 13:287–297
Zhen Q, Liu JF, Liu JB, Wang RF, Chu WW, Zhang YX, Tan GL, Zhao XJ, Lv BL (2015) Endothelial PAS domain-containing protein 1 confers TKI-resistance by mediating EGFR and MET pathways in non-small cell lung cancer cells. Cancer Biol Ther 16:549–557. https://doi.org/10.1080/15384047.2015.1016689
Cui J, Duan B, Zhao X, Chen Y, Sun S, Deng W, Zhang Y, Du J, Chen Y, Gu L (2016) MBD3 mediates epigenetic regulation on EPAS1 promoter in cancer. Tumour Biol 37:13455–13467. https://doi.org/10.1007/s13277-016-5237-1
Pan X, Zhu Q, Sun Y, Li L, Zhu Y, Zhao Z, Zuo J, Fang W, Li K (2015) PLGA/poloxamer nanoparticles loaded with EPAS1 siRNA for the treatment of pancreatic cancer in vitro and in vivo. Int J Mol Med 35:995–1002. https://doi.org/10.3892/ijmm.2015.2096
Rawluszko-Wieczorek AA, Horbacka K, Krokowicz P, Misztal M, Jagodzinski PP (2014) Prognostic potential of DNA methylation and transcript levels of HIF1A and EPAS1 in colorectal cancer. Mol Cancer Res 12:1112–1127. https://doi.org/10.1158/1541-7786.MCR-14-0054
Patil T, Aisner DL, Noonan SA, Bunn PA, Purcell WT, Carr LL, Camidge DR, Doebele RC (2016) Malignant pleural disease is highly associated with subsequent peritoneal metastasis in patients with stage IV non-small cell lung cancer independent of oncogene status. Cancer Treat Res 96:27–32. https://doi.org/10.1016/j.lungcan.2016.03.007
Doebele RC, Lu X, Sumey C, Maxson DA, Weickhardt AJ, Oton AB, Bunn PA Jr., Baron AE, Franklin WA, Aisner DL, Varella-Garcia M, Camidge DR (2012) Oncogene status predicts patterns of metastatic spread in treatment-naive nonsmall cell lung cancer. Cancer 118:4502–4511. https://doi.org/10.1002/cncr.27409
Su HT, Tsai CM, Perng RP (2008) Peritoneal carcinomatosis in lung cancer. Respirology 13:465–467. https://doi.org/10.1111/j.1440-1843.2008.01268.x
Kurishima K, Miyazaki K, Tamura T, Ohara G, Kagohashi K, Kawaguchi M, Satoh H (2013) Peritoneal and meningeal relapse from lung adenocarcinoma after a response to gefitinib: a case report. Mol Clin Oncol 1:785–787. https://doi.org/10.3892/mco.2013.122
Satoh H, Kagohashi K, Kurishima K (2013) Peritoneal relapse from lung adenocarcinoma after a response to EGFR-TKI. Tuberk Toraks 61:346–347. https://doi.org/10.5578/tt.6534
Nakano T, Shimizu K, Kawashima O, Kamiyoshihara M, Kakegawa S, Sugano M, Ibe T, Nagashima T, Kaira K, Sunaga N, Ohtaki Y, Atsumi J, Takeyoshi I (2012) Establishment of a human lung cancer cell line with high metastatic potential to multiple organs: gene expression associated with metastatic potential in human lung cancer. Oncol Rep 28:1727–1735. https://doi.org/10.3892/or.2012.1972
Otto J, Jansen PL, Lucas S, Schumpelick V, Jansen M (2007) Reduction of peritoneal carcinomatosis by intraperitoneal administration of phospholipids in rats. BMC Cancer 7:104. https://doi.org/10.1186/1471-2407-7-104
Yanez-Mo M, Lara-Pezzi E, Selgas R, Ramirez-Huesca M, Dominguez-Jimenez C, Jimenez-Heffernan JA, Aguilera A, Sanchez-Tomero JA, Bajo MA, Alvarez V, Castro MA, del Peso G, Cirujeda A, Gamallo C, Sanchez-Madrid F, Lopez-Cabrera M (2003) Peritoneal dialysis and epithelial-to-mesenchymal transition of mesothelial cells. N Engl J Med 348:403–413. https://doi.org/10.1056/NEJMoa020809
Sandoval P, Jimenez-Heffernan JA, Rynne-Vidal A, Perez-Lozano ML, Gilsanz A, Ruiz-Carpio V, Reyes R, Garcia-Bordas J, Stamatakis K, Dotor J, Majano PL, Fresno M, Cabanas C, Lopez-Cabrera M (2013) Carcinoma-associated fibroblasts derive from mesothelial cells via mesothelial-to-mesenchymal transition in peritoneal metastasis. J Pathol 231:517–531. https://doi.org/10.1002/path.4281
Abrams HL, Spiro R, Goldstein N (1950) Metastases in carcinoma; analysis of 1000 autopsied cases. Cancer 3:74–85
Warren S, Gates O (1964) Lung cancer and metastasis. Arch Pathol 78:467–473
McNeill PM, Wagman LD, Neifeld JP (1987) Small bowel metastases from primary carcinoma of the lung. Cancer 59:1486–1489
Satoh H, Ishikawa H, Yamashita YT, Kurishima K, Ohtsuka M, Sekizawa K (2001) Peritoneal carcinomatosis in lung cancer patients. Oncol Rep 8:1305–1307. https://doi.org/10.3892/or.8.6.1305
Niu FY, Zhou Q, Yang JJ, Zhong WZ, Chen ZH, Deng W, He YY, Chen HJ, Zeng Z, Ke EE, Zhao N, Zhang N, Sun HW, Zhang QY, Xie Z, Zhang XC, Wu YL (2016) Distribution and prognosis of uncommon metastases from non-small cell lung cancer. BMC Cancer 16:149. https://doi.org/10.1186/s12885-016-2169-5
Nassereddine H, Sannier A, Brosseau S, Rodier JM, Khalil A, Msika S, Danel C, Couvelard A, Theou-Anton N, Cazes A (2019) Clinicopathological and molecular study of peritoneal carcinomatosis associated with non-small cell lung carcinoma. Pathol Oncol Res. https://doi.org/10.1007/s12253-019-00713-1
Putra AC, Eguchi H, Lee KL, Yamane Y, Gustine E, Isobe T, Nishiyama M, Hiyama K, Poellinger L, Tanimoto K (2015) The A allele at rs13419896 of EPAS1 is associated with enhanced expression and poor prognosis for non-small cell lung cancer. PLoS ONE 10:e134496. https://doi.org/10.1371/journal.pone.0134496
Yu S, Ren H, Li Y, Liang X, Ning Q, Chen X, Chen M, Hu T (2018) HOXA4-dependent transcriptional activation of AXL promotes cisplatin-resistance in lung adenocarcinoma cells. Anticancer Agents Med Chem 18:2062–2067. https://doi.org/10.2174/1871520619666181203110835
Wang Z, Wei Y, Zhang R, Su L, Gogarten SM, Liu G, Brennan P, Field JK, McKay JD, Lissowska J, Swiatkowska B, Janout V, Bolca C, Kontic M, Scelo G, Zaridze D, Laurie CC, Doheny KF, Pugh EK, Marosy BA, Hetrick KN, Xiao X, Pikielny C, Hung RJ, Amos CI, Lin X, Christiani DC (2018) Multi-omics analysis reveals a HIF network and hub gene EPAS1 associated with lung adenocarcinoma. EBioMedicine 32:93–101. https://doi.org/10.1016/j.ebiom.2018.05.024
Xu XH, Bao Y, Wang X, Yan F, Guo S, Ma Y, Xu D, Jin L, Xu J, Wang J (2018) Hypoxic-stabilized EPAS1 proteins transactivate DNMT1 and cause promoter hypermethylation and transcription inhibition of EPAS1 in non-small cell lung cancer. FASEB J. https://doi.org/10.1096/fj.201700715
Yuan S, Xiang Y, Wang G, Zhou M, Meng G, Liu Q, Hu Z, Li C, Xie W, Wu N, Wu L, Cai T, Ma X, Zhang Y, Yu Z, Bai L, Li Y (2019) Hypoxia-sensitive LINC01436 is regulated by E2F6 and acts as an oncogene by targeting miR-30a-3p in non-small cell lung cancer. Mol Oncol 13:840–856. https://doi.org/10.1002/1878-0261.12437
Tan DS, Agarwal R, Kaye SB (2006) Mechanisms of transcoelomic metastasis in ovarian cancer. Lancet Oncol 7:925–934. https://doi.org/10.1016/S1470-2045(06)70939-1
de Cuba EM, Kwakman R, van Egmond M, Bosch LJ, Bonjer HJ, Meijer GA, te Velde EA (2012) Understanding molecular mechanisms in peritoneal dissemination of colorectal cancer : future possibilities for personalised treatment by use of biomarkers. Virchows Arch 461:231–243. https://doi.org/10.1007/s00428-012-1287-y
Aroeira LS, Aguilera A, Sanchez-Tomero JA, Bajo MA, del Peso G, Jimenez-Heffernan JA, Selgas R, Lopez-Cabrera M (2007) Epithelial to mesenchymal transition and peritoneal membrane failure in peritoneal dialysis patients: pathologic significance and potential therapeutic interventions. J Am Soc Nephrol 18:2004–2013. https://doi.org/10.1681/ASN.2006111292
Sandoval P, Loureiro J, Gonzalez-Mateo G, Perez-Lozano ML, Maldonado-Rodriguez A, Sanchez-Tomero JA, Mendoza L, Santamaria B, Ortiz A, Ruiz-Ortega M, Selgas R, Martin P, Sanchez-Madrid F, Aguilera A, Lopez-Cabrera M (2010) PPAR-gamma agonist rosiglitazone protects peritoneal membrane from dialysis fluid-induced damage. Lab Invest 90:1517–1532. https://doi.org/10.1038/labinvest.2010.111
Loureiro J, Aguilera A, Selgas R, Sandoval P, Albar-Vizcaino P, Perez-Lozano ML, Ruiz-Carpio V, Majano PL, Lamas S, Rodriguez-Pascual F, Borras-Cuesta F, Dotor J, Lopez-Cabrera M (2011) Blocking TGF-beta1 protects the peritoneal membrane from dialysate-induced damage. J Am Soc Nephrol 22:1682–1695. https://doi.org/10.1681/ASN.2010111197
Mubarak KK, Montes-Worboys A, Regev D, Nasreen N, Mohammed KA, Faruqi I, Hensel E, Baz MA, Akindipe OA, Fernandez-Bussy S, Nathan SD, Antony VB (2012) Parenchymal trafficking of pleural mesothelial cells in idiopathic pulmonary fibrosis. Eur Respir J 39:133–140. https://doi.org/10.1183/09031936.00141010
Li Y, Wang J, Asahina K (2013) Mesothelial cells give rise to hepatic stellate cells and myofibroblasts via mesothelial-mesenchymal transition in liver injury. Proc Natl Acad Sci USA 110:2324–2329. https://doi.org/10.1073/pnas.1214136110
Perez-Lozano ML, Sandoval P, Rynne-Vidal A, Aguilera A, Jimenez-Heffernan JA, Albar-Vizcaino P, Majano PL, Sanchez-Tomero JA, Selgas R, Lopez-Cabrera M (2013) Functional relevance of the switch of VEGF receptors/co-receptors during peritoneal dialysis-induced mesothelial to mesenchymal transition. PLoS One 8:e60776. https://doi.org/10.1371/journal.pone.0060776
Funding
This work was funded by the Natural Science Foundation of Hebei Province (H2019106033).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Q. Zhen, Y. Zhang, L. Gao, R. Wang, W. Chu, X. Zhao, Z. Li, H. Li, B. Zhang, B. Lv, and J. Liu declare that they have no competing interests.
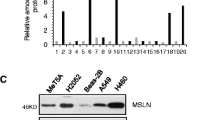
Caption Electronic Supplementary Material
Figure S1. HIF1α expression is unchanged between PC14 and PC14HM cell lines.
Expression levels of (A) HIF1α mRNA and (B) protein were examined in PC14 and PC14HM cells, respectively. Values were mean ± SD from at least three biological replicates. n p > 0.05, PC14 vs PC14HM
Rights and permissions
About this article
Cite this article
Zhen, Q., Zhang, Y., Gao, L. et al. EPAS1 promotes peritoneal carcinomatosis of non-small-cell lung cancer by enhancing mesothelial–mesenchymal transition. Strahlenther Onkol 197, 141–149 (2021). https://doi.org/10.1007/s00066-020-01665-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-020-01665-1