Abstract
Purpose
To determine the influence of different medical physicists, photon energies, treatment planning systems and treatment machines on the resulting external beam radiotherapy dose distribution for a sample prostate cancer case.
Methods
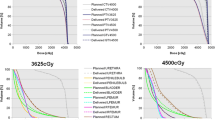
A pre-contoured computed tomography (CT) dataset containing planning target volume 1 (PTV1) prostate and seminal vesicles (single dose [SD] 1.8 Gy, total dose [TD] 59.4 Gy), PTV2 prostate (simultaneously integrated boost [SIB], SD 2.0 Gy, TD 66 Gy), PTV3 prostate and seminal vesicles approach (SD 1.8 Gy, TD 73.8 Gy/80.4 Gy SIB) as well as organs at risk (OAR: rectum, bladder, femoral heads, bowel, anus) was offered to the members of the task group IMRT (intensity-modulated radiation therapy) of the German Society for Medical Physics. The purpose was to calculate one combined treatment plan (TP) for PTV1 and PTV2, as well as a separate one for PTV3. Dose volume histograms (DVH), different dose values, conformity index (CI), homogeneity index (HI), gradient index (GI) and a new “better than average score” were used to analyse the dose distributions.
Results
Altogether 44 institutions took part in this study and submitted acceptable dose distributions for the PTVs. However, there were statistically significant differences, especially for the doses administered to the OAR, such as rectum, bladder and femoral heads. Differences between the treatment plans were not easily detectable by visual inspection of the isodose distribution. Dose maxima may occur outside the PTV. Even though scoring indices are already published, the new “better than average score” was needed to identify a plan that minimises dose to all OAR simultaneously.
Conclusion
Different medical physicists or dosimetrists, photon energies, treatment planning systems, and treatment machines have an impact on the resulting dose distribution. However, the differences only become apparent when comparing DVH, analysing dose values, comparing CI, HI, GI, as well as reviewing the dose distribution in every single plane. A new score was introduced to identify treatment plans that simultaneously deliver a low dose to all OAR. Such inter- and intra-institutional comparison studies are needed to explore different treatment planning strategies; however, there is still no automatic solution for an “optimal” treatment plan.
Zusammenfassung
Zielsetzung
Es sollten die Einflüsse unterschiedlicher Planer, der Photonenenergie sowie der Bestrahlungsplanungssysteme und Therapiegeräte auf die resultierende Dosisverteilung für einen exemplarischen Prostata-Bestrahlungsfall untersucht werden.
Methoden
Ein vorkonturierter Computertomographiedatensatz mit den Planungszielvolumina 1 (PTV1) Prostata und Samenblasen (Einzeldosis [SD] 1,8 Gy, Gesamtdosis [TD] 59,4 Gy), PTV2 Prostata (simultan integrierter Boost [SIB], SD 2,0 Gy, TD 66 Gy) und PTV3 Prostata und Samenblasenansatz (SD 1,8 Gy, TD 73,8 Gy/80,4 Gy im SIB) sowie den Risikoorganen Rektum, Blase, Anus, Darm und Femurköpfe wurde über den Arbeitskreis IMRT (intensitätsmodulierte Radiotherapie) der Deutschen Gesellschaft für Medizinische Physik allen interessierten strahlentherapeutischen Einrichtungen im deutschsprachigen Raum angeboten. Es war die Aufgabe, einen gemeinsamen Plan für PTV1 und PTV2 als auch einen weiteren für PTV3 zu berechnen. Es wurden Dosis-Volumen-Histogramme (DVH), unterschiedliche Dosiswerte, der Konformitätsindex (CI), Homogenitätsindex (HI) und Gradientenindex (GI) sowie ein neuer „Besser-als-der-Durchschnitt-Score“ miteinander verglichen sowie die Dosisverteilungen in jeder Schicht analysiert.
Ergebnisse
Insgesamt 44 strahlentherapeutische Einrichtungen nahmen an der Studie teil und sandten akzeptable Bestrahlungspläne für die PTV ein. Es fanden sich statistisch signifikante Unterschiede in den Therapieplänen, insbesondere in den Risikoorgandosen, etwa für Rektum, Blase und Hüftköpfe. Diese Unterschiede lassen sich allein anhand des Isodosenverlaufs nur schwer erkennen. Es können Dosismaxima außerhalb des PTV auftreten. Obwohl bereits mehrere Scores zur Bewertung von Therapieplänen publiziert wurden, wurde ein weiterer Score benötigt, um einen Plan mit gleichzeitig geringer Dosisbelastung für alle Risikoorgane zu identifizieren.
Schlussfolgerung
Unterschiedliche Planer, Photonenenergien, eingesetzte Bestrahlungsplanungssysteme und Therapiegeräte haben einen Einfluss auf die resultierende Dosisverteilung. Die Unterschiede werden aber erst durch einen Vergleich der DVH, eine numerische Analyse der Dosiswerte, die Kontrolle von CI, HI und GI sowie eine Begutachtung der Dosisverteilungen in jeder Schicht deutlich. Es wurde ein neuer Score eingeführt, um Bestrahlungspläne zu finden, die die Dosisbelastung aller Risikoorgane gleichzeitig minimieren. Solche inter- und intrainstitutionellen Planvergleichsstudien sind nötig, um unterschiedliche Bestrahlungstechniken zu bewerten. Aber weiterhin gibt es keine automatische Lösung für einen „optimalen“ Bestrahlungsplan.






Similar content being viewed by others
References
Erlay J, Ervik M, Dikshit R et al (2012) Cancer incidence and mortality worldwide: IARC CancerBase No. 11. In: GLOBOCAN 2012 v1. 0
Stewart B, Wild CP et al (2014) World cancer report 2014. CEDEX, France, Lyon
Marino C, Villaggi E, Maggi G et al (2015) A feasibility dosimetric study on prostate cancer: are we ready for a multicenter clinical trial on SBRT? Strahlenther Onkol 191:573–581
D’Amico AV, Whittington R, Malkowicz SB et al (1998) Biochemical outcome after radical prostatectomy, external beam radiation therapy, or interstitial radiation therapy for clinically localized prostate cancer. JAMA 280(11):969–974 (Epub 1998/09/28)
Frenzel T, Honecker F, Krüll A et al (2012) Tumorerfassung: Mit Erfassungsbögen und Leitlinien für die interdisziplinäre Diagnostik und Therapie, 1st edn. Thieme, Stuttgart
Partin AW, Yoo J, Carter HB et al (1993) The use of prostate specific antigen, clinical stage and Gleason score to predict pathological stage in men with localized prostate cancer. J Urol 150:110–114
International Commission on Radiation Units and Measurements (2010) ICRU report 83 prescribing, recording, and reporting photon-beam intensity-modulated radiation therapy (IMRT). J ICRU 10(1). https://doi.org/10.1093/jicru/ndq002
Feuvret L, Noël G, Mazeron J‑J, Bey P (2006) Conformity index: a review. Int J Radiat Oncol Biol Phys 64:333–342
Paddick I (2000) A simple scoring ratio to index the conformity of radiosurgical treatment plans. Technical note. J Neurosurg 93(Suppl 3):219–222
Yoon M, Park SY, Shin D et al (2007) A new homogeneity index based on statistical analysis of the dose-volume histogram. J Appl Clin Med Phys 8:9–17
Wu Q, Mohan R, Morris M et al (2003) Simultaneous integrated boost intensity-modulated radiotherapy for locally advanced head-and-neck squamous cell carcinomas. I: dosimetric results. Int J Radiat Oncol Biol Phys 56:573–585
Paddick I, Lippitz B (2006) A simple dose gradient measurement tool to complement the conformity index. J Neurosurg 105(Suppl):194–201
Park JM, Park S‑Y, Choi CH et al (2017) Treatment plan comparison between Tri-Co-60 magnetic-resonance image-guided radiation therapy and volumetric modulated arc therapy for prostate cancer. Oncotarget 8:91174–91184
Lin Y‑W, Lin K‑H, Ho H‑W et al (2014) Treatment plan comparison between stereotactic body radiation therapy techniques for prostate cancer: non-isocentric CyberKnife versus isocentric RapidArc. Phys Med 30:654–661
Quan EM, Li X, Li Y et al (2012) A comprehensive comparison of IMRT and VMAT plan quality for prostate cancer treatment. Int J Radiat Oncol Biol Phys 83:1169–1178
Moustakis C, Blanck O, Ebrahimi Tazehmahalleh F et al (2017) Planning benchmark study for SBRT of early stage NSCLC: results of the DEGRO working group Stereotactic radiotherapy. Strahlenther Onkol 193:780–790
Blanck O, Wang L, Baus W et al (2016) Inverse treatment planning for spinal robotic radiosurgery: an international multi-institutional benchmark trial. J Appl Clin Med Phys 17:313–330
Esposito M, Masi L, Zani M et al (2019) SBRT planning for spinal metastasis: indications from a large multicentric study. Strahlenther Onkol 195:226–235
Moustakis C, Chan MKH, Kim J et al (2018) Treatment planning for spinal radiosurgery: a competitive multiplatform benchmark challenge. Strahlenther Onkol 194:843–854
Giglioli FR, Strigari L, Ragona R et al (2016) Lung stereotactic ablative body radiotherapy: a large scale multi-institutional planning comparison for interpreting results of multi-institutional studies. Phys Med 32:600–606
Schubert C, Waletzko O, Weiss C et al (2017) Intercenter validation of a knowledge based model for automated planning of volumetric modulated arc therapy for prostate cancer. The experience of the German RapidPlan Consortium. PLoS ONE 12:e178034
Kavanaugh JA, Holler S, DeWees TA et al (2019) Multi-institutional validation of a knowledge-based planning model for patients enrolled in RTOG 0617: implications for plan quality controls in cooperative group trials. Pract Radiat Oncol 9:e218–e227
Riegel AC, Vaccarelli M, Cox BW et al (2019) Impact of multi-institutional prospective peer review on target and organ-at-risk delineation in radiation therapy. Pract Radiat Oncol 9:e228–e235
Acknowledgements
The authors thank all participants of this treatment planning comparison study who sent in two treatment plans: Thomas Barthel (Würzburg), Dr. Klaus Bratengeier (Würzburg), David Büch (Nürnberg), Benjamin Bujak (Goslar), Stephan Dröge (Hemer), Dr. Jörg Eckardt (Bochum), Anke Engbert (Lüneburg), Christiane Feyrer (Heilbronn), Karsten Gerull (Lübeck), Julia Göpner (Berlin), Sascha Großmann (Mainz), Benjamin Gülden (Berlin), Laura Günther (Wuppertal), Dietmar Hahm (Bielefeld), Thomas Hauschild (Bamberg), Simon Howitz (Jena), Dr. Daniel Hummel (Stuttgart), Petra Hüttenrauch (Göttingen), Severin Kampfer (München), Jürgen Karg (Roth), Wolfgang Lechner (Wien, Österreich), Kathleen Lorenz (Chemnitz), Imke Lütjens (Hamburg), Steffen Lutz (Stuttgart), Manfred Mayr (Kaufbeuren), Tristan Mensing (Berlin), Dr. Knut Merla (Dresden), Dr. Christos Moustakis (Münster), Marcel Renz (Braunschweig), Dr. Thomas Rothe (Freiburg), Dr. Henrik Schachner (Weilheim), Dr. Nanda Schmidt-Petersen (Stade), Frank Szafinski (Düsseldorf), Michael Tartz (Hannover), Maik Teicher (Neubrandenburg), Kathleen Trombalski (Berlin), Prof. Dr. Ulrich Wolf (Leipzig), as well as five colleagues who wanted to take part anonymously.
Author information
Authors and Affiliations
Contributions
The authors of the article did the following specific work: Thorsten Frenzel: Study design, technical implementation (server, communication), evaluation of the data, presentation of the data at each community meeting (AK IMRT), drafting of the manuscript, literature search, proofreading. Dirk Albers: Technical implementation (anonymization of the CT data; import of the treatment plans), data processing, editing of the manuscript, proofreading. Maximilian Grohmann: Technical support, e.g., with Varian’s script language for the evaluation of the treatment plans, editing of the manuscript, proofreading. Andreas Krüll: Evaluation of the treatment plans, editing of the manuscript, literature search, proofreading
Corresponding author
Ethics declarations
Conflict of interest
T. Frenzel, D. Albers, M. Grohmann, and A. Krüll declare that they have no competing interests.
Ethical standards
This article is about the comparison of multiple treatment plans that were created by medical physicists in Germany and Austria. All participants gave their consent for blinded publication when sending in their treatment plan. Some participants wanted to stay anonymous in the final paper. All study participants were informed about the preliminary results and ongoing work during AK IMRT and AK Tomotherapie meetings.
Rights and permissions
About this article
Cite this article
Frenzel, T., Albers, D., Grohmann, M. et al. Results of a multicenter intensity modulated radiation therapy treatment planning comparison study for a sample prostate cancer case. Strahlenther Onkol 195, 913–922 (2019). https://doi.org/10.1007/s00066-019-01496-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-019-01496-9
Keywords
- Prostate cancer
- Intensity modulated radiation therapy
- Treatment planning
- Comparison study
- Better than average score