Abstract
Purpose
To evaluate alterations in pulmonary function indices after helical tomotherapy and explore potential associations with biologically corrected dosimetric parameters.
Patients and methods
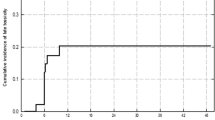
In 64 patients with inoperable locally advanced non-small cell lung cancer, pulmonary function tests before and within 6 months after radiotherapy were evaluated retrospectively. In the case of concurrent chemotherapy a total dose of 67.2 Gy was delivered, otherwise 70.5 Gy was provided. In 44 patients, late pulmonary function changes (≥6 months after radiotherapy) could also be assessed.
Results
In the entire patient group, there were significant declines in forced expiratory volume in 1s (FEV1) (average change −4.1% predicted; P = 0.007), in forced vital capacity (FVC) (−4.9% predicted; P = 0.002), total lung capacity (TLC) (−5.8% predicted; P = 0.0016) and DLCO (diffusing capacity of the lung for carbon monoxide corrected for hemoglobin level) (−8.6% predicted; P < 0.001) during the first 6 months. Corresponding FEV1, FVC, TLC and DLCO declines in the subgroup with late measurements (after 11.3 months on average) were −5.7, −7.4, −7.0, −9.8% predicted. A multivariate analysis including V5 Gy, V10 Gy, V20 Gy, V40 Gy, V60 Gy, mean lung dose (MLD), gross tumor volume (GTV) and planning target volume (PTV) as potential covariates showed that GTV was the most consistent contributor, being significant for ∆FEV1 (P = 0.003), ∆FVC (P = 0.003), ∆TLC (P = 0.001) and ∆DLCO (P = 0.01). V5 Gy or V10 Gy did not contribute to any of the lung function changes.
Conclusions
The decline in pulmonary function indices after helical tomotherapy was of similar magnitude to that observed in studies reporting the effect of conformal radiotherapy on lung function. Diffusion capacity was the parameter showing the largest decrease following radiation therapy as compared to baseline and correlated with gross tumor volume. None of the alterations in pulmonary function tests were associated with the lung volume receiving low-dose radiation.
Zusammenfassung
Zielsetzung
Evaluation von Veränderungen von Lungenfunktionsparametern nach helikaler Tomotherapie und Untersuchung möglicher Zusammenhänge mit dosimetrischen Parametern nach strahlenbiologischer Korrektur.
Patienten und Methoden
Bei 64 Patienten mit inoperablem lokal fortgeschrittenem nicht-kleinzelligem Lungenkarzinom wurden vor der Strahlentherapie und innerhalb der ersten 6 Monate nach Behandlung Lungenfunktionsprüfungen durchgeführt und ausgewertet. Im Fall von konkomitant applizierter Chemotherapie wurde eine Gesamtdosis von 67,2 Gy vorgeschrieben, anderenfalls 70,5 Gy. Bei 44 der 64 Patienten konnten auch längerfristige funktionelle Veränderungen (≥6 Monate nach Strahlentherapie) ermittelt werden.
Ergebnisse
Im gesamten Patientenkollektiv wurden innerhalb der ersten 6 Monate signifikante Verminderungen der Einsekundenkapazität (FEV1) (durchschnittliche Änderung −4,1%/%Sollwert; P = 0,007), in forcierte Vitalkapazität (FVC) (−4,9%/%Sollwert; P = 0,002), totale Lungenkapazität (TLC) (−5,8%/%Sollwert; P = 0,0016) und DLCO (Diffusionskapazität) (−8,6%/%Sollwert; P < 0,001) gemessen. Die entsprechende Verminderung von FEV1, FVC, TLC und DLCO in der Gruppe mit späteren Messungen (im Durschnitt 11,3 Monate) waren −5,7, −7,4, −7,0, −9,8%/%Sollwert. Die Multivarianzanalyse unter Berücksichtigung von V5 Gy, V10 Gy, V20 Gy, V40 Gy, V60 Gy, mittlere Lungendichte (MLD), makroskopische Tumorvolumen (GTV) und Planungszielvolumen (PTV) als mögliche Kovariablen zeigte, dass das GTV den stärksten Einfluss hatte. Auch ∆FEV1 (P = 0,003), ∆FVC (P = 0,003), ∆TLC (P = 0,001) und ∆DLCO (P = 0,01) erreichten Signifikanzniveau. V5 Gy und V10 Gy trugen nicht zur Verschlechterung der Lungenfunktion bei.
Schlussfolgerung
Nach helikaler Tomotherapie verschlechterten sich die Lungenfunktionsparameter in ähnlicher Weise wie in den Studien mit konformaler Strahlentherapie. Die Diffusionskapazität war der Parameter mit der größten Abnahme nach Tomotherapie und korrelierte mit dem Tumorvolumen (GTV). Keine der Veränderungen in der Lungenfunktionsprüfung war abhängig vom Lungenvolumen, das geringen Strahlendosen ausgesetzt war.


Similar content being viewed by others
References
Mirimanoff RO (1994) Concurrent chemotherapy (CT) and radiotherapy (RT) in locally advanced non-small cell lung cancer (NSCLC): a review. Cancer Treat 11:79–99
Phernambucq EC, Spoelstra FO, Verbakel WF et al (2011) Outcomes of concurrent chemoradiotherapy in patients with stage III non-small-cell lung cancer and significant comorbidity. Ann Oncol 22:132–138
Eberhardt WE, De Ruysscher D, Weder W et al (2015) 2nd ESMO Consensus Conference in lung cancer:locally advanced stage III non-small-cell lung cancer. Ann Oncol 26:1573–1588
Aupérin A, Le Péchoux C, Rolland E et al (2010) Meta-analysis of concomitant versus sequential radiochemotherapy in locally advanced non-small-cell lung cancer. J Clin Oncol 28:2181–2190
van Baardwijk A, Wanders S, Boersma L et al (2010) Mature results of an individualized radiation dose prescription study based on normal tissue constraints in stages I to III non-small-cell lung cancer. J Clin Oncol 28:1380–1386
Bradley JD, Paulus R, Komaki R et al (2015) Standard-dose versus high-dose conformal radiotherapy with concurrent and consolidation carboplatin plus paclitaxel with or without cetuximab for patients with stage IIIA or IIIB non-small-cell lung cancer (RTOG 0617): a randomised, two-by-two factorial phase 3 study. Lancet Oncol 16:187–199
Antonia SJ, Villegas A, Daniel D et al (2018) Overall survival with durvalumab after chemoradiotherapy in stage III NSCLC. N Engl J Med 379:2342–2350
Abratt RP, Willcox PA (1995) The effect of irradiation on lung function and perfusion in patients with lung cancer. Int J Radiat Oncol Biol Phys 15:915–919
Gopal R, Starkschall G, Tucker SL et al (2003) Effects of radiotherapy and chemotherapy on lung function in patients with non-small-cell lung cancer. Int J Radiat Oncol Biol Phys 56:114–120
Abratt RP, Willcox PA, Smith JA (1990) Lung cancer in patients with borderline lung functions-zonal lung perfusion scans at presentation and lung function after high dose irradiation. Radiother Oncol 19:317–322
Grills IS, Yan D, Martinez AA et al (2003) Potential for reduced toxicity and dose escalation in the treatment of inoperable non-small-cell lung cancer: a comparison of intensity-modulated radiation therapy (IMRT), 3D conformal radiation, and elective nodal irradiation. Int J Radiat Oncol Biol Phys 57:875–890
Gopal R, Tucker SL, Komaki R et al (2003) The relationship between local dose and loss of function for irradiated lung. Int J Radiat Oncol Biol Phys 56:106–113
Vogelius IS, Westerly DC, Cannon GM et al (2011) Intensity-modulated radiotherapy might increase pneumonitis risk relative to three-dimensional conformal radiotherapy in patients receiving combined chemotherapy and radiation therapy: a modeling study of dose dumping. Int J Radiat Oncol Biol Phys 80:893–899
Rosas S, Barbosa B, Couto JG (2018) Intensity-modulated radiation therapy versus volumetric-modulated arc therapy in non-small cell lung cancer: assessing the risk of radiation pneumonitis. J Radiother Pract 17:6–11
Bral S, Duchateau M, Versmessen H et al (2010) Toxicity report of a phase 1/2 dose-escalation study in patients with inoperable, locally advanced nonsmall cell lung cancer with helical tomotherapy and concurrent chemotherapy. Cancer 116:241–250
Bral S, Duchateau M, Versmessen H et al (2010) Toxicity and outcome results of a class solution with moderately hypofractionated radiotherapy in inoperable stage III non-small cell lung cancer using helical tomotherapy. Int J Radiat Oncol Biol Phys 77:1352–1359
Oh IJ, Kim KS, Kim YC et al (2013) A phase III concurrent chemoradiotherapy trial with cisplatin and paclitaxel or docetaxel or gemcitabine in unresectable non-small cell lung cancer: KASCL 0401. Cancer Chemother Pharmacol 72:1247–1254
Miller MR, Hankinson J, Brusasco V et al (2005) Standardisation of spirometry. Eur Respir J 26:319–338
Macintyre N, Crapo RO, Viegi G et al (2005) Standardisation of the single-breath determination of carbon monoxide uptake in the lung. Eur Respir J 26:720–735
Gonzalez Mangado N, Aviles Ingles MJ, Peces-Barba G et al (1987) A simple method of correcting diffusing capacity for alveolar volume reduction in restrictive lung diseases. Respiration 52:163–170
Verbanck S, Van Muylem A, Schuermans D et al (2016) Transfer factor, lung volumes, resistance and ventilation distribution in healthy adults. Eur Respir J 47:166–176
Schröder C, Engenhart-Cabillic R, Vorwerk H et al (2017) Changes in pulmonary function and influencing factors after high-dose intrathoracic radio(chemo)therapy. Strahlenther Onkol 193:125–131
Chun SG, Hu C, Choy H et al (2017) Impact of Intensity-Modulated Radiation Therapy Technique for Locally Advanced Non-Small-Cell Lung Cancer: A Secondary Analysis of the NRG Oncology RTOG 0617 Randomized Clinical Trial. J Clin Oncol 35:56–62
Ball D, Mac Manus M, Siva S et al (2017) Routine Use of Intensity-Modulated Radiotherapy for Locally Advanced Non-Small-Cell Lung Cancer Is Neither Choosing Wisely Nor Personalized Medicine. J Clin Oncol 35:1492–1493
Lopez Guerra JL, Gomez DR, Zhuang Y et al (2012) Changes in pulmonary function after three-dimensional conformal radiation therapy, intensity-modulated radiation therapy, or proton beam therapy for non-small-cell lung cancer. Int J Radiat Oncol Biol Phys 83:537–543
Brand PL, Quanjer PH, Postma DS et al (1992) Interpretation of bronchodilator response in patients with obstructive airways disease. The Dutch Chronic Non-Specific Lung Disease (CNSLD) Study Group. Thorax 47:429–436
Miller KL, Zhou SM, Barrier RC Jr et al (2003) Long-term changes in pulmonary function tests after definitive radiotherapy for lung cancer. Int J Radiat Oncol Biol Phys 56:611–615
Schröder C, Engenhart-Cabillic R, Vorwerk H et al (2016) A lot to a little or a little to a lot—which dose-volume relationship ensures the best clinical outcome in the high dose radiation therapy of thoracic tumors? A prospective approach. J Thoracic Dis 8:2053–2060
Acknowledgements
We thank Daniel Schuermans for help with assembling the lung function data from this patient population.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
K. Vekens, S. Verbanck, C. Collen, G. Storme, K. Barbé, M. De Ridder and E. Vanderhelst declare that they have no competing interests.
Caption Electronic Supplementary Material
Rights and permissions
About this article
Cite this article
Vekens, K., Verbanck, S., Collen, C. et al. Pulmonary function changes following helical tomotherapy in patients with inoperable, locally advanced non-small cell lung cancer. Strahlenther Onkol 196, 142–150 (2020). https://doi.org/10.1007/s00066-019-01489-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-019-01489-8