Abstract
Purpose
Aim of the present analysis was to evaluate the movement and dose variability of the different lymph node levels of node-positive breast cancer patients during adjuvant radiotherapy (RT) with regional nodal irradiation (RNI) in deep-inspiration breath hold (DIBH).
Methods
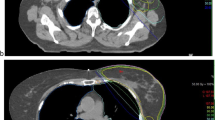
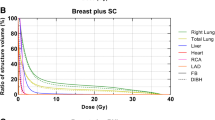
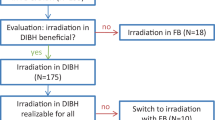
Thirty-five consecutive node-positive breast cancer patients treated from October 2016 to February 2018 receiving postoperative RT of the breast or chest wall including RNI of the supra-/infraclavicular lymph node levels (corresponding to levels IV, III, Rotter LN (interpectoral), and some parts of level II) were analyzed. To evaluate the lymph node level movement, a center of volume (COV) was obtained for each lymph node level for free-breathing (FB) and DIBH plans. Geometric shifts and dose differences between FB and DIBH were analyzed.
Results
A significant movement of the COV in anterior (y) and cranial (z) dimensions was observed for lymph node levels I–II and Rotter lymph nodes (p < 0.001) due to DIBH. Only minor changes in the lateral dimension (x axis) were observed, without reaching significance for levels III, IV, and internal mammary. There was a significant difference in the mean dose of level I (DIBH vs. FB: 38.2 Gy/41.3 Gy, p < 0.001) and level II (DIBH vs. FB: 45.9 Gy/47.2 Gy, p < 0.001), while there was no significant difference in level III (p = 0.298), level IV (p = 0.476), or internal mammary nodes (p = 0.471).
Conclusion
A significant movement of the axillary lymph node levels was observed during DIBH in anterior and cranial directions for node-positive breast cancer patients in comparison to FB. The movement leads to a significant dose reduction in level I and level II.
Zusammenfassung
Fragestellung
Ziel der vorliegenden Analyse war es, die Bewegungs- und Dosisvariabilität der verschiedenen Lymphknotenstationen nodalpositiver Brustkrebspatientinnen während der adjuvanten Bestrahlung inklusive regionaler Lymphabflussbestrahlung (RNI) in tiefer Inspiration („deep inspiration breath hold“, DIBH) zu bewerten.
Methoden
Von Oktober 2016 bis Februar 2018 wurden 35 nodalpositive Brustkrebspatientinnen mit postoperativer RT der Brust oder Brustwand einschließlich RNI der supra-/infraklavikulären Lymphknotenregionen (entsprechend Level IV, III, Rotter-Lymphknoten interpektoral und Anteile von Level II) untersucht. Zur Beurteilung der Bewegung der Lymphknotenstationen wurde für jedes Lymphknotenlevel der geometrische Volumenmittelpunkt („center of volume“, COV) in freier Atmung („free breathing“, FB) und DIBH ermittelt. Die räumlichen Bewegungen und Dosisunterschiede zwischen FB und DIBH wurden analysiert.
Ergebnisse
Eine signifikante Bewegung des COV in anteriorer (y) und kranialer (z) Richtung wurde für die Lymphknotenlevel I–II sowie für die Rotter-Lymphknoten (p < 0,001) in DIBH beobachtet. Es wurden nur geringe Veränderungen im Bereich der lateralen Dimension (x-Achse) beobachtet, welche für die Level III, IV und die Mammaria-interna-Lymphknoten nicht signifikant waren. Es zeigten sich außerdem signifikante Dosisunterschiede für das Lymphknotenlevel I (DIBH vs. FB: 38,2 Gy/41,3 Gy; p < 0,001) und II (DIBH vs. FB: 45,9 Gy/47,2 Gy; p < 0,001), während es keinen signifikanten Unterschied für das Level III (p = 0,298), IV (p = 0,476) und Mammaria interna (p = 0,471) gab.
Schlussfolgerungen
Eine signifikante Bewegung der axillären Lymphknotenstationen während DIBH wurde vorwiegend in anteriorer und kranialer Richtung im Vergleich zu FB beobachtet. Die Bewegung führte zu einer signifikanten Dosisreduktion innerhalb der Lymphknotenlevel I und II.


Similar content being viewed by others
References
Overgaard M, Hansen PS, Overgaard J et al (1997) Postoperative radiotherapy in high-risk premenopausal women with breast cancer who receive adjuvant chemotherapy. Danish Breast Cancer Cooperative Group 82b Trial. N Engl J Med 337:949–955
Overgaard M, Nielsen HM, Overgaard J (2007) Is the benefit of postmastectomy irradiation limited to patients with four or more positive nodes, as recommended in international consensus reports? A subgroup analysis of the DBCG 82 b&c randomized trials. Radiother Oncol 82:247–253
Ragaz J, Olivotto IA, Spinelli JJ et al (2005) Locoregional radiation therapy in patients with high-risk breast cancer receiving adjuvant chemotherapy: 20-year results of the British Columbia randomized trial. J Natl Cancer Inst 97:116–126
Offersen BV, Boersma LJ, Kirkove C et al (2015) ESTRO consensus guideline on target volume delineation for elective radiation therapy of early stage breast cancer. Radiother Oncol 114:3–10
Budach W, Bölke E, Kammers K et al (2015) Adjuvant radiation therapy of regional lymph nodes in breast cancer—a meta-analysis of randomized trials—an update. Radiat Oncol 10:1–7
Whelan TJ, Olivotto IA, Parulekar WR et al (2015) Regional nodal irradiation in early-stage breast cancer. N Engl J Med 373:307–316
Poortmans PM, Collette S, Kirkove C et al (2015) Internal mammary and medial supraclavicular irradiation in breast cancer. N Engl J Med 373:317–327
Hennequin C, Bossard N, Servagi-Vernat S et al (2013) Ten-year survival results of a randomized trial of irradiation of internal mammary nodes after mastectomy. Int J Radiat Oncol Biol Phys 86:860–866
Cuzick J, Stewart H, Rutqvist L et al (1994) Cause-specific mortality in long-term survivors of breast cancer who participated in trials of radiotherapy. J Clin Oncol 12:447–453
Darby SC, Ewertz M, Mcgale P et al (2013) Risk of ischemic heart disease in women after radiotherapy for breast cancer. N Engl J Med 368:987–998
Henson KE, Mcgale P, Taylor C et al (2013) Radiation-related mortality from heart disease and lung cancer more than 20 years after radiotherapy for breast cancer. Br J Cancer 108:179–182
Darby SC, Mcgale P, Taylor CW et al (2005) Long-term mortality from heart disease and lung cancer after radiotherapy for early breast cancer: prospective cohort study of about 300,000 women in US SEER cancer registries. Lancet Oncol 6:557–565
Schonecker S, Walter F, Freislederer P et al (2016) Treatment planning and evaluation of gated radiotherapy in left-sided breast cancer patients using the CatalystTM/SentinelTM system for deep inspiration breath-hold (DIBH). Radiat Oncol 11:143
Corradini S, Ballhausen H, Weingandt H et al (2017) Left-sided breast cancer and risks of secondary lung cancer and ischemic heart disease: effects of modern radiotherapy techniques. Strahlenther Onkol 194(3):196–205. https://doi.org/10.1007/s00066-017-1213-y
Cozzi L, Lohr F, Fogliata A et al (2017) Critical appraisal of the role of volumetric modulated arc therapy in the radiation therapy management of breast cancer. Radiat Oncol 12:200
Sachdev S, Goodman CR, Neuschler E et al (2017) Radiotherapy of MRI-detected involved internal mammary lymph nodes in breast cancer. Radiat Oncol 12:199
Becker-Schiebe M, Stockhammer M, Hoffmann W et al (2016) Does mean heart dose sufficiently reflect coronary artery exposure in left-sided breast cancer radiotherapy? Strahlenther Onkol 192:624–631
Mast ME, Heijenbrok MW, Van Kempen-Harteveld ML et al (2016) Less increase of CT-based calcium scores of the coronary arteries: effect three years after breast-conserving radiotherapy using breath-hold. Strahlenther Onkol 192:696–704
Lu HM, Cash E, Chen MH et al (2000) Reduction of cardiac volume in left-breast treatment fields by respiratory maneuvers: a CT study. Int J Radiat Oncol Biol Phys 47:895–904
Shah C, Badiyan S, Berry S et al (2014) Cardiac dose sparing and avoidance techniques in breast cancer radiotherapy. Radiother Oncol 112:9–16
Chen MH, Cash EP, Danias PG et al (2002) Respiratory maneuvers decrease irradiated cardiac volume in patients with left-sided breast cancer. J Cardiovasc Magn Reson 4:265–271
Borm KJ, Oechsner M, Combs SE et al (2018) Deep-inspiration breath-hold radiation therapy in breast cancer: a word of caution on the dose to the axillary lymph node levels. Int J Radiat Oncol Biol Phys 100:263–269
Giuliano AE, Hunt KK, Ballman KV et al (2011) Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: a randomized clinical trial. JAMA 305:569–575
Alongi F, Ricchetti F, Fiorentino A et al (2014) Postoperative breast radiotherapy after neoadjuvant chemotherapy: which uncertainties still remain? Tumori 100:e212–213
Mamounas EP (2015) Impact of neoadjuvant chemotherapy on locoregional surgical treatment of breast cancer. Ann Surg Oncol 22:1425–1433
White J, Tai1 A, Arthur D, Buchholz T, MacDonald S, Marks L, Pierce L, Recht A, Rabinovitch R, Taghian A, Vicini F, Woodward W, Li XA. https://www.rtog.org/LinkClick.aspx?fileticket=vzJFhPaBipE%3d&tabid=236
Wenz F, Budach W (2017) Personalized radiotherapy for invasive breast cancer in 2017: national S3 guidelines and DEGRO and AGO recommendations. Strahlenther Onkol 193:601–603
Jagsi R, Chadha M, Moni J et al (2014) Radiation field design in the ACOSOG Z0011 (Alliance) Trial. J Clin Oncol 32:3600–3606
Mccormick B, Botnick M, Hunt M et al (2002) Are the axillary lymph nodes treated by standard tangent breast fields? J Surg Oncol 81:12–16
Aguiar A, Gomes Pereira H, Azevedo I et al (2015) Evaluation of axillary dose coverage following whole breast radiotherapy: variation with the breast volume and shape. Radiother Oncol 114:22–27
Reed DR, Lindsley SK, Mann GN et al (2005) Axillary lymph node dose with tangential breast irradiation. Int J Radiat Oncol Biol Phys 61:358–364
Russo JK, Armeson KE, Rhome R et al (2011) Dose to level I and II axillary lymph nodes and lung by tangential field radiation in patients undergoing postmastectomy radiation with tissue expander reconstruction. Radiat Oncol 6:179
Zhang L, Yang ZZ, Chen XX et al (2015) Dose coverage of axillary level I–III areas during whole breast irradiation with simplified intensity modulated radiation therapy in early stage breast cancer patients. Oncotarget 6:18183–18191
Haffty BG, Hunt KK, Harris JR et al (2011) Positive sentinel nodes without axillary dissection: implications for the radiation oncologist. J Clin Oncol 29:4479–4481
Donker M, Van Tienhoven G, Straver ME et al (2014) Radiotherapy or surgery of the axilla after a positive sentinel node in breast cancer (EORTC 10981–22023 AMAROS): a randomised, multicentre, open-label, phase 3 non-inferiority trial. Lancet Oncol 15:1303–1310
Okunieff P, Morgan D, Niemierko A et al (1995) Radiation dose-response of human tumors. Int J Radiat Oncol Biol Phys 32:1227–1237
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M. Pazos, A. Fiorentino, A. Gaasch, S. Schönecker, D. Reitz, C. Heinz, M. Niyazi, M.-N. Duma, F. Alongi, C. Belka, and S. Corradini declare that they have no competing interests.
Additional information
Montserrat Pazos and Alba Fiorentino contributed equally.
Rights and permissions
About this article
Cite this article
Pazos, M., Fiorentino, A., Gaasch, A. et al. Dose variability in different lymph node levels during locoregional breast cancer irradiation: the impact of deep-inspiration breath hold. Strahlenther Onkol 195, 13–20 (2019). https://doi.org/10.1007/s00066-018-1350-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-018-1350-y