Abstract
Background
Radiotherapy using the deep inspiration breath-hold (DIBH) technique compared with free breathing (FB) can achieve substantial reduction of heart and lung doses in left-sided breast cancer cases. The anatomical organ movement in deep inspiration also cause unintended exposure of locoregional lymph nodes to the irradiation field.
Methods
From 2017–2020, 148 patients with left-sided breast cancer underwent breast conserving surgery (BCS) or mastectomy (ME) with axillary lymph node staging, followed by adjuvant irradiation in DIBH technique. Neoadjuvant or adjuvant systemic therapy was administered depending on hormone receptor and HER2-status.
CT scans in FB and DIBH position with individual coaching and determination of the breathing amplitude during the radiation planning CT were performed for all patients. Intrafractional 3D position monitoring of the patient surface in deep inspiration and gating was performed using Sentinel and Catalyst HD 3D surface scanning systems (C-RAD, Catalyst, C-RAD AB, Uppsala, Sweden). Three-dimensional treatment planning was performed using standard tangential treatment portals (6 or 18 MV). The delineation of ipsilateral locoregional lymph nodes was done on the FB and the DIBH CT-scan according to the RTOG recommendations.
Results
The mean doses (Dmean) in axillary lymph node (AL) level I, II and III in DIBH were 32.28 Gy (range 2.87–51.7), 20.1 Gy (range 0.44–53.84) and 3.84 Gy (range 0.25–39.23) vs. 34.93 Gy (range 10.52–50.40), 16.40 Gy (range 0.38–52.40) and 3.06 Gy (range 0.21–40.48) in FB (p < 0.0001). Accordingly, in DIBH the Dmean for AL level I were reduced by 7.59%, whereas for AL level II and III increased by 22.56% and 25.49%, respectively.
The Dmean for the supraclavicular lymph nodes (SC) in DIBH was 0.82 Gy (range 0.23–4.11), as compared to 0.84 Gy (range 0.22–10.80) with FB (p = 0.002). This results in a mean dose reduction of 2.38% in DIBH.
The Dmean for internal mammary lymph nodes (IM) was 12.77 Gy (range 1.45–39.09) in DIBH vs. 11.17 Gy (range 1.34–44.24) in FB (p = 0.005). This yields a mean dose increase of 14.32% in DIBH.
Conclusions
The DIBH technique may result in changes in the incidental dose exposure of regional lymph node areas.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Incidental irradiation of cardiac structures in left-sided breast cancer increases the risk of subsequent ischaemic cardiac events [1]. Notably, any Gy increase in mean cardiac dose correlates linearly with a 7.4% increase in non-threshold cardiac events [2]. Different absorbed doses and irradiated volumes result in a variety of pathophysiologic events: macrovascular damage to the coronary vessels such as atherosclerosis and myocardial infarction, or microvascular damage with valvular heart disease and heart failure [3, 4]. Disturbingly, breast cancer patients who developed cardiac disease after initial cancer diagnosis have a higher risk of recurrence and cancer-specific death [5]. In particular, dose-dependent vulnerability of the left ventricle and all coronary segments justifies more rigorous dose reduction [6,7,8,9].
Currently, deep inspiration breath hold technique (DIBH) in the supine position allows reproducible cardiac shift from the irradiation field. Therefore, it is a widely used protective heart approach [10]. DIBH can be performed by tangential 3D-conformal radiotherapy (3DRT) or rotational/multiangle intensity-modulated radiotherapy (IMRT/VMAT) [11].
Tangential 3DRT of the mammary gland tissue often unintentionally includes the locoregional lymph nodes in the radiation fields with therapeutic dose. This dose may be sufficient for the eradication of microscopic tumor residues. This hypothesis is supported by the results of the ACOSOG Z0011 study, where patients with 1–2 involved sentinel lymph nodes upon sentinel lymph node dissection had similar axillary recurrence rates whether they received secondary axillary lymph node dissection or not [12]. However, a retrospective review revealed that high tangents and supraclavicular irradiation were used in a significant proportion of patients [13].
We propose that DIBH may lead to differences in the incidental radiation dose of the axillary, supraclavicular and internal mammary lymph nodes due to changes in their position [14, 15] in relation to the tangential radiation portals.
In the absence of published data in this regard from randomized trials of DIBH vs free breathing (FB) RT in the supine position, reporting institutional experiences is necessary. The goal of this single-institutional retrospective study was to investigate dosimetric differences of incidental locoregional lymph nodes irradiation between DIBH and FB for left-sided breast cancer patients.
Materials and methods
Patient selection and treatment planning
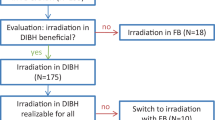
From December 2017 to July 2020, 148 out of 247 patients with left-sided or bilateral breast cancer which were screened for irradiation in DIBH technique were included in this analysis. The majority of patients (131 patients, 88.5%) received 3DRT in DIBH. The remaining 17 (11.5%) patients received RT in FB either due to suboptimal compliance or lack of dosimetric benefits of DIBH.
BCS or mastectomy with axillary lymph node staging was performed according to institutional protocols. Systemic therapy was administered according to current guidelines [16] and individual recommendations of the multidisciplinary tumor board. A tumor bed boost was administered for all premenopausal patients or for postmenopausal patients with additional risk factors (tumor stage ≥ T2, extensive intraductal component, grade 3, HER2-positive or triple-negative tumors).
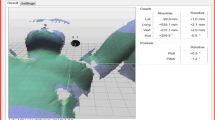
All patients received coaching for DIBH in the CT room using a Surface Image Guided RT (SGRT) system (C-RAD, Catalyst, C-RAD AB, Uppsala, Sweden). The patients were asked to take a deep breath and hold it for a duration of 20 s. The width of the gating window was set to 5 mm. All patients received two CT scans with a slice thickness of 2 mm (Brilliance, CT Big Bore, Philips, Cleveland, OH) in FB and DIBH. Treatment planning (Oncentra MasterPlan, Nucletron, Veenendaal, The Netherlands and/or Eclipse™ planning systems (Varian Medical Systems)) was carried out using standard tangential treatment portals (6 or 18 MV; Synergy; Elekta, Crawley, United Kingdom).
Adjuvant WBI or thoracic wall RT was delivered using either moderate hypofractionation (40.05 Gy in 15 fractions) or conventional fractionation (50.00–50.40 Gy in 25–28 fractions). Boost irradiation was delivered sequentially (10–16 Gy in 5–8 fractions), with simultaneous integrated boost (58.80–61.60 Gy in 25–28 fractions) or IORT (single dose of 20 Gy with 50-kV photons [17]).
During follow up, all patients were examined every three to six months for the first two years in the radiation oncology department, followed by annual visits thereafter. Breast ultrasound was performed every 6 months for the first three years. Mammograms were obtained six months after WBI, and yearly after the first mammography. Suspected recurrences were biopsy confirmed.
Statistical analysis
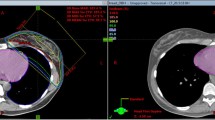
For the planned dosimetric evaluation, lymph nodes levels of interest (axillary lymph node levels I, II, III, supraclavicular (SC) and internal mammary (IM) lymph nodes) as well as the contralateral breast were retrospectively delineated (Fig. 1). The delineation was done on both the FB and the DIBH scan according to the RTOG recommendations [18]. DVH parameters were then extracted for all delineated structures (volume, Dmean, D50%, Dmax, Dmin, V30, V40).
Delineation of locoregional lymph nodes and isodose distribution. a-c: Delineation of the supraclavicular (green), axillary lymph levels I (yellow) and II (light blue axillary lymph nodes in level III (blue), internal mammary (orange). a + c: CT scan in DIBH; b + d: CT scan in FB; a-d: Visualization of isodose distribution in DIBH and FB
Data are reported as a mean, median (range), and frequencies. For all dosimetric parameters, mean values and their corresponding ranges as well as the relative dose reduction were determined. DVH parameters of the FB vs. DIBH plans were compared using a Wilcoxon signed-rank test. P-values < 0.05 were considered statistically significant. Effect size was assessed according to Cohen (1988) [19]. Analysis was performed using SPSS version 27 (IBM, Armonk, NY, USA).
Results
Altogether, 148 patients with 296 CT scans were analyzed. Baseline characteristics are shown in Table 1. Most patients had T1 (67.6%, n = 100) and N0 stage (87.8%, n = 130) with positive estrogen and progesterone receptor status. Poor differentiation (G3) and Ki-67 > 20% were present in 25.7% and 41.9 of patients, respectively. A minority of patients required re-resection to achieve clear margins (12.8%). Only four patients received mastectomy (2.7%). About 23% of patients received hypofractionated radiotherapy.
Axillary lymph node levels I, II and III
The DVH parameters for levels I-III, SC and IM are summarized in Table 2.
The mean dose (Dmean) in level I, II and III in DIBH were 32.28 Gy (range 2.87–51.7), 20.10 Gy (range 0.44–53.84) and 3.84 Gy (range 0.25–39.23) vs. 34.93 Gy (range 10.52–50.40), 16.40 Gy (range 0.38–52.40) and 3.06 Gy (range 0.21–40.48) in the FB group (p < 0.0001 for all) (Fig. 2). In comparison to FB, Dmean for level I was reduced by 7.59% (effect size, r = 0.38) and increased for level II and III by 22.56% (r = 0.45), and 25.49% (r = 0.47).
The D50% in level I, II, and III in DIBH were 35.42 Gy (range 1.64–53.35), 19.65 Gy (range 0.44–52.32) and 3.23 Gy (range 0.25–44.97) vs. 39.02 Gy (range 2.75–52.05), 15.29 Gy (range 0.38–52.37) and 2.38 Gy (range 0.21–47.19) in the FB group (p < 0.0001 for all) (Table 2). Thus, in comparison to FB D50% for level I was reduced by 9.23% (r = 0.39), whereas it was increased for level II and III D50% by 28.52% (r = 0.42), and 35.71% (r = 0.46) (Table 2).
The mean values of V30Gy, and V40Gy for level I in the DIBH cohort were decreased by 9.23% and 11.13% (p < 0.0001 for both, r = 0.38 and r = 0.32), respectively. There was an increase in the mean values of V30, and V40 for level II in DIBH 27.88% (p < 0.0001, r = 0.41) and 29.31% (p < 0.0001, r = 0.44) respectively. There was a non-significant increase in the mean values of V30Gy and V40Gy for level III with DIBH (Table 2).
The mean volumes of the lymph node levels were assessed in FB and DIBH. There were small, but significant volume decreases in DIBH for level III by 3.83% (p < 0.0001) but not for level II by 1.28% (p = 0.062).
Supraclavicular and internal mammary region and contralateral breast
The Dmean for the SC in DIBH was 0.82 Gy (range 0.23–4.11), as compared to 0.84 Gy (range 0.22–10.80) with FB (p = 0.002). This results in a Dmean reduction of 2.38% (r = 0.26) in DIBH (Fig. 3). The mean volumes of the SC in FB were 27.2 cm3 (range 15.2–38.5) vs. DIBH: 26 cm3 (range 13–37.3). This resulted with moderate volume decrease in DIBH for SC by 2.4% (p < 0.0001).
The Dmean for IM was 12.77 Gy (range 1.45–39.09) in DIBH vs. 11.17 Gy (range 1.34–44.24) in FB (p = 0.005). This yields a Dmean increase of 14.32% (r = 0.23) in DIBH (Fig. 4). The mean of V30Gy, and V40Gy for IM in DIBH were by 29.47% (p = 0.019, r = 0.19) and 33.54% (p = 0.02, r = 0.19) (Table 2). The mean volume of the IM in FB was 7.6 cm3 (range 3.80–9.5) compared to 7.5 cm3 (range 3.7–9.5) in DIBH. This corresponded to a small, but significant decrease in volume in DIBH for IM by 1.3% (p < 0.0001).
Mean values for right (contralateral) breast were 795.5 cm3 (range 128–2762.7) for FB and 801.2 cm3 (range 121.80–2759.1) for DIBH. The mean relative difference between DIBH and FB was small (relative increase of 0.72%), but statistically significant (p = 0.023).
Discussion
In this retrospective single-center analysis, we could demonstrate that the use of DIBH leads to significant changes in dose-volume parameters for patients with left-sided breast cancer treated with tangential 3DRT. For level I, DIBH lead to a decrease in incidental dose whereas DIBH was associated with increased doses for level II-III, supraclavicular and internal mammary lymph nodes.
Since publication of the ACOSOG Z0011-trial, there has been a controversial discussion regarding the radiation dose required for control of subclinical disease in the axilla [20]. Although the trial protocol mandated standard tangential irradiation, a subsequent retrospective analysis of 228 patients showed that more than half of the patients were treated with high tangents and 15% received supraclavicular irradiation [13]. A meta-analysis of prospective partial breast irradiation-trials demonstrated an increased risk of axillary recurrences with an odds ratio of 1.75 (95%-confidence interval 1.07–2.88), further suggesting that incidental axillary irradiation might contribute to locoregional control [21].
A recent systematic review identified 13 retrospective studies with a total of 475 patients which analyzed dosimetric parameters of axillary lymph node levels for patients planned for adjuvant whole breast radiotherapy [22]. There was considerable variation in axillary doses depending on the use of high tangents and radiation technique. For patients treated with standard tangential 3DRT, median dose in axillary levels I-III ranged from 22 to 43.5 Gy, 3 to 35.6 Gy, and 1 to 20.5 Gy, respectively [22]. In addition to these retrospective studies, Hildebrandt et al. recently published prospective data from the quality assurance program of the INSEMA-trial [23]. Incidental axillary doses were analyzed for 234 patients who underwent central plan review. Axillary level I and II were treated with a median of 72.8% and 39.9% of the prescribed dose in the breast, respectively. Level III only received a median dose of 16.4% of the breast dose. More than 25% of patients were treated with a median dose ≥ 95% of the breast dose in level I. Patients with a body mass index (BMI) ≥ 30 kg/m2 had significantly higher median doses in level I-III. Most patients received 3DRT (76.1%), while DIBH was only used in 1 patient [23].
DIBH is a standard technique for patients with left sided breast cancer due to a significant dose reduction of cardiac structures [24,25,26]. In 2019, the breast cancer expert panel of the German Society for Radiation Oncology (DEGRO) recommended the use of DIBH for the treatment of patients with left sided breast cancer [10]. However, DIBH is not only associated with a change in the position of the heart and lungs but also with changes in the chest wall and surrounding soft tissue [14, 15]. This may affect the incidental dose to axillary lymph node levels as well as the supraclavicular and internal mammary lymph nodes.
Borm et al. contoured axillary lymph node levels according to the RTOG atlas for 32 patients and compared incidental doses during DIBH and FB [15]. They demonstrated an overall three-dimensional movement of the axillary lymph node levels of 1.5 to 1.6 cm. The use of DIBH lead to a significant decrease in the incidental dose to level I and numerical, but mostly non-significant increases in the dose to level II and III [15].
Pazos et al. analyzed the influence of DIBH on doses to level I-III, supraclavicular and internal mammary nodes for 35 patients planned for radiotherapy of the breast or chest wall and the regional lymph nodes. Three-dimensional movement was between 0.79 cm for level I and 1.44 cm for internal mammary nodes. DIBH led to a significant decrease in the dose to level I and II compared to FB, however there were no significant differences for the other regions of interest [14].
In our analysis, the largest absolute changes were observed for level I with a decrease of 2.65 Gy (from 34.93 Gy to 32.28 Gy) and for level II with an increase of 3.7 Gy (from 16.40 Gy to 20.10 Gy). However, the clinical relevance may be more adequately addressed by comparing exposure to higher doses, such as V40Gy and V30Gy. While only small amounts of level II were exposed to these doses, DIBH led to an absolute decrease in the V40Gy and V30Gy of 6.3% and 5.9% for Level I, respectively. Level III as well as the supraclavicular and the internal mammary nodes were only minimally exposed to incidental irradiation. The observed changes, though in some cases statistically significant, may not be clinically relevant due to relatively small absolute differences. Compared to the analysis by Borm et al. [15], the changes in Dmean and V40Gy and V30Gy are somewhat smaller in magnitude. Contrary to their findings, we saw an increase in all dosimetric parameters for level II as well as Dmean to level III, but nor for V40Gy and V30Gy for level III. We observed considerably lower doses to level II and III, for example for Dmean of level II: 16.40 Gy (FB) and 20.10 Gy (DIBH) in our analysis compared to 23.7 Gy (FB) and 24.1 Gy (DIBH) for Borm et al. [15]. This may be related to differences in treatment planning and DIBH-technique. While we used a surface scanning-approach with a pre-defined gating window of 5 mm, the real-time position management system (RPM, Varian Medical Systems, Palo Alto, CA) was used by Borm et al. [15]. No details regarding the gating window were provided.
Our analysis represents the largest cohort both in terms of dosimetric analysis in FB and in DIBH. We included intraindividual comparisons based on CT-scans in FB and DIBH for each patient. To exclude confounding by different radiotherapy techniques, only tangential 3DRT-plans were analyzed. It has been previously shown that IMRT or VMAT can also significantly impact incidental dose to the axilla [27,28,29]. Thus, our data cannot be extrapolated to patients receiving a combination of DIBH and IMRT/VMAT. Interindividual differences in anatomy may be responsible in part for dosimetric variability. Furthermore, compliance with breath hold as well as the quality of coaching for DIBH and the depth of inspiration may have an impact on anatomical changes and the position of lymph node areas in DIBH. Unfortunately, information on BMI was not available from the patient charts and could thus not be analyzed. The subgroup of patients with mastectomy was too small to provide reliable estimates for statistical comparisons. About 23% of patients in our analysis received hypofractionated radiotherapy, which in itself may lead to a decreased biologically effective dose to the unintentionally exposed axilla [30].
In conclusion, we could demonstrate a significant variability in incidental dose exposure to regional lymph node areas in patients with left-sided breast cancer by the use of DIBH. Further studies are needed to determine the clinical significance of these findings and to establish predictors of dosimetric changes based on patient-related factors.
Availability of data and materials
The data used in this analysis are available with the authors’ permission.
Abbreviations
- AL:
-
Axillary lymph nodes
- ALND:
-
Axillary lymph node dissection
- BCS:
-
Breast conservation surgery
- CI:
-
Confidence interval
- 3DRT:
-
3D-conformal radiotherapy
- DVH:
-
Dose-volume histogram
- DIBH:
-
Deep inspiration breath hold
- ER:
-
Estrogen receptor
- FB:
-
Free breathing
- HER2:
-
Human epidermal growth factor receptor 2
- IM:
-
Internal mammary lymph nodes
- IMRT:
-
Intensity-modulated radiotherapy
- IORT:
-
Intraoperative radiotherapy
- MV:
-
Megavolt
- OS:
-
Overall survival
- PR:
-
Progesterone receptor
- RT:
-
Radiotherapy
- SC:
-
Supraclavicular lymph nodes
- SGRT:
-
Surface image guided radiotherapy
- SIB:
-
Simultaneous integrated boost
- SLND:
-
Sentinel lymph node dissection
- TNBC:
-
Triple-negative breast cancer
- VMAT:
-
Volumetric modulated arc therapy
- WBI:
-
Whole breast irradiation
References
Harris EE, Correa C, Hwang WT, Liao J, Litt HI, Ferrari VA, et al. Late cardiac mortality and morbidity in early-stage breast cancer patients after breast-conservation treatment. J Clin Oncol. 2006;24(25):4100–6.
Darby SC, Ewertz M, McGale P, Bennet AM, Blom-Goldman U, Bronnum D, et al. Risk of ischemic heart disease in women after radiotherapy for breast cancer. N Engl J Med. 2013;368(11):987–98.
Stewart FA, Seemann I, Hoving S, Russell NS. Understanding radiation-induced cardiovascular damage and strategies for intervention. Clin Oncol (R Coll Radiol). 2013;25(10):617–24.
Yang EH, Marmagkiolis K, Balanescu DV, Hakeem A, Donisan T, Finch W, et al. Radiation-induced vascular disease-a state-of-the-art review. Front Cardiovasc Med. 2021;8: 652761.
Koelwyn GJ, Newman AAC, Afonso MS, van Solingen C, Corr EM, Brown EJ, et al. Myocardial infarction accelerates breast cancer via innate immune reprogramming. Nat Med. 2020;26(9):1452–8.
Taylor C, McGale P, Bronnum D, Correa C, Cutter D, Duane FK, et al. Cardiac structure injury after radiotherapy for breast cancer: cross-sectional study with individual patient data. J Clin Oncol. 2018;36(22):2288–96.
Wennstig AK, Garmo H, Isacsson U, Gagliardi G, Rintela N, Lagerqvist B, et al. The relationship between radiation doses to coronary arteries and location of coronary stenosis requiring intervention in breast cancer survivors. Radiat Oncol. 2019;14(1):40.
Nilsson G, Holmberg L, Garmo H, Duvernoy O, Sjogren I, Lagerqvist B, et al. Distribution of coronary artery stenosis after radiation for breast cancer. J Clin Oncol. 2012;30(4):380–6.
Skytta T, Tuohinen S, Boman E, Virtanen V, Raatikainen P, Kellokumpu-Lehtinen PL. Troponin T-release associates with cardiac radiation doses during adjuvant left-sided breast cancer radiotherapy. Radiat Oncol. 2015;10:141.
Duma MN, Baumann R, Budach W, Dunst J, Feyer P, Fietkau R, et al. Heart-sparing radiotherapy techniques in breast cancer patients: a recommendation of the breast cancer expert panel of the German society of radiation oncology (DEGRO). Strahlenther Onkol. 2019;195(10):861–71.
Piroth MD, Baumann R, Budach W, Dunst J, Feyer P, Fietkau R, et al. Heart toxicity from breast cancer radiotherapy : Current findings, assessment, and prevention. Strahlenther Onkol. 2019;195(1):1–12.
Giuliano AE, Ballman KV, McCall L, Beitsch PD, Brennan MB, Kelemen PR, et al. Effect of axillary dissection vs no axillary dissection on 10-year overall survival among women with invasive breast cancer and sentinel node metastasis: the ACOSOG Z0011 (Alliance) randomized clinical trial. JAMA. 2017;318(10):918–26.
Jagsi R, Chadha M, Moni J, Ballman K, Laurie F, Buchholz TA, et al. Radiation field design in the ACOSOG Z0011 (Alliance) trial. J Clin Oncol. 2014;32(32):3600–6.
Pazos M, Fiorentino A, Gaasch A, Schonecker S, Reitz D, Heinz C, et al. Dose variability in different lymph node levels during locoregional breast cancer irradiation: the impact of deep-inspiration breath hold. Strahlenther Onkol. 2019;195(1):13–20.
Borm KJ, Oechsner M, Combs SE, Duma MN. Deep-inspiration breath-hold radiation therapy in breast cancer: a word of caution on the dose to the axillary lymph node levels. Int J Radiat Oncol Biol Phys. 2018;100(1):263–9.
Ditsch N, Kolberg-Liedtke C, Friedrich M, Jackisch C, Albert US, Banys-Paluchowski M, et al. AGO recommendations for the diagnosis and treatment of patients with early breast cancer: update 2021. Breast Care (Basel). 2021;16(3):214–27.
Stoian R, Erbes T, Zamboglou C, Scholber J, Gainey M, Sachpazidis I, et al. Intraoperative radiotherapy boost as part of breast-conservation therapy for breast cancer: a single-institution retrospective analysis. Strahlenther Onkol. 2021;197(9):812–9.
Gentile MS, Usman AA, Neuschler EI, Sathiaseelan V, Hayes JP, Small W Jr. Contouring guidelines for the axillary lymph nodes for the delivery of radiation therapy in breast cancer: evaluation of the RTOG breast cancer atlas. Int J Radiat Oncol Biol Phys. 2015;93(2):257–65.
Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale: Erlbaum; 1998. ISBN 0805802835.
Haffty BG, Hunt KK, Harris JR, Buchholz TA. Positive sentinel nodes without axillary dissection: implications for the radiation oncologist. J Clin Oncol. 2011;29(34):4479–81.
Haussmann J, Budach W, Strnad V, Corradini S, Krug D, Schmidt L, et al. Comparing local and systemic control between partial- and whole-breast radiotherapy in low-risk breast cancer-a meta-analysis of randomized trials. Cancers (Basel). 2021;13(12):2967.
Schmitt M, Pin Y, Pflumio C, Mathelin C, Pivot X, Noel G. Incidental axillary dose delivery to axillary lymph node levels I-III by different techniques of whole-breast irradiation: a systematic literature review. Strahlenther Onkol. 2021;197(9):820–8.
Hildebrandt G, Stachs A, Gerber B, Potenberg J, Krug D, Wolter K, et al. Central review of radiation therapy planning among patients with breast-conserving surgery: results from a quality assurance process integrated into the INSEMA trial. Int J Radiat Oncol Biol Phys. 2020;107(4):683–93.
Pedersen AN, Korreman S, Nystrom H, Specht L. Breathing adapted radiotherapy of breast cancer: reduction of cardiac and pulmonary doses using voluntary inspiration breath-hold. Radiother Oncol. 2004;72(1):53–60.
Schonecker S, Walter F, Freislederer P, Marisch C, Scheithauer H, Harbeck N, et al. Treatment planning and evaluation of gated radiotherapy in left-sided breast cancer patients using the Catalyst(TM)/Sentinel(TM) system for deep inspiration breath-hold (DIBH). Radiat Oncol. 2016;11(1):143.
Vikstrom J, Hjelstuen MH, Wasbo E, Mjaaland I, Dybvik KI. A comparison of conventional and dynamic radiotherapy planning techniques for early-stage breast cancer utilizing deep inspiration breath-hold. Acta Oncol. 2018;57(10):1325–30.
Ahrouch I, Van Gestel D, Koshariuk O, Kirkove C, Desmet A, Philippson C, et al. Unintended dose to the lower axilla in adjuvant radiotherapy for breast cancer: Differences between tangential beam and VMAT. Radiother Oncol. 2021;164:282–8.
Lee J, Kim SW, Son SH. Dosimetric evaluation of incidental irradiation to the axilla during whole breast radiotherapy for patients with left-sided early breast cancer in the IMRT era. Medicine (Baltimore). 2016;95(26): e4036.
Song Y, Yu T, Wang W, Li J, Sun T, Qiu P, et al. Dosimetric comparison of incidental radiation to the internal mammary nodes after breast-conserving surgery using 3 techniques-inverse intensity-modulated radiotherapy, field-in-field intensity-modulated radiotherapy, and 3-dimensional conformal radiotherapy: A retrospective clinical study. Medicine (Baltimore). 2019;98(41): e17549.
Borm KJ, Oechsner M, Dusberg M, Buschner G, Wolfgang W, Combs SE, et al. Effect of hypofractionation on the incidental axilla dose during tangential field radiotherapy in breast cancer. Strahlenther Onkol. 2020;196(9):771–8.
Acknowledgements
None.
Funding
Open Access funding enabled and organized by Projekt DEAL. The authors received no specific funding for this study.
Author information
Authors and Affiliations
Contributions
T.S., J.W., N.H.N.: Study conception and study design. J.W., S.K., T.R., M.S., J.S., T.E., E.G., D.B., A-L.G., N.H.N, T.S.: Data acquisition, data analysis and data interpretation. J.W., T.R., M.S. performed DIBH coaching and treatment planning. J.W., S.K. and T.S.: Statistical analysis. D.B., V.V., D.K., I. J-B., A-L.G., N.H.N., T.S.: Manuscript editing. T.E., E.G., D.B., V.V., D.K., A-L.G., N.H.N., T.S.: Manuscript reviewed. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the institutional ethical review committee of the Albert-Ludwigs-University of Freiburg (reference no. 453/19) and was performed in accordance with the relevant guidelines and regulations. The need for patient consent was waived by the ethics committee.
Consent for publication
Not applicable.
Competing interests
D. Krug has received honoraria from Merck Sharp & Dohme and Pfizer as well as research funding from Merck KGaA outside the submitted work. T. Sprave has received honoraria from Hologic outside the submitted work. The other authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wolf, J., Kurz, S., Rothe, T. et al. Incidental irradiation of the regional lymph nodes during deep inspiration breath-hold radiation therapy in left-sided breast cancer patients: a dosimetric analysis. BMC Cancer 22, 682 (2022). https://doi.org/10.1186/s12885-022-09784-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-022-09784-x