Abstract
Purpose
There has been increasing use of external beam radiotherapy for localized treatment of hepatocellular carcinoma (HCC) with both palliative and curative intent. Quality control of target delineation in primary HCC is essential to deliver adequate doses of radiation to the primary tumor while preserving adjacent healthy organs. We analyzed interobserver variability in gross tumor volume (GTV) delineation for HCC.
Patients and methods
Twelve radiation oncologists specializing in liver malignancy participated in a multi-institutional contouring dummy-run study of nine HCC cases and independently delineated GTV on the same set of provided computed tomography images. Quantitative analysis was performed using an expectation maximization algorithm for simultaneous truth and performance level estimation (STAPLE) with kappa statistics calculating agreement between physicians. To quantify the interobserver variability of GTV delineations, the ratio of the actual delineated volume to the estimated consensus volume (STAPLE), the ratio of the common and encompassing volumes, and the coefficient of variation were calculated.
Results
The median kappa agreement level was 0.71 (range 0.28–0.86). The ratio of the actual delineated volume to the estimated consensus volume ranged from 0.19 to 1.93 (median 0.94) for all cases. The ratio of the common and encompassing volumes ranged from 0.001 to 0.56 (median 0.25). The coefficient of variation for GTV delineation ranged from 8 to 57 % (median 26 %).
Conclusion
The interobserver variability in target delineation of HCC GTV in this study is noteworthy. Multi-institution studies involving radiotherapy for HCC require appropriate quality assurance programs for target delineation.
Zusammenfassung
Ziel
Die externe kurative Strahlentherapie ist zunehmend bei der lokalisierten Behandlung hepatozellulärer Karzinome (HCC) in palliativer und kurativer Absicht in Gebrauch. Eine Qualitätskontrolle der Zielabgrenzung beim primären HCC ist entscheidend, um die passende Dosis für die Primärtumorbestrahlung zuzuführen und gesunde benachbarte Organe zu schonen. Wir analysierten die Interobservervariabilität in Abgrenzung zum makroskopischen Tumorvolumen (GTV) beim HCC.
Patienten und Methoden
In einer institutsübergreifenden konturierenden Teststudie mit 9 HCC-Fällen beschrieben 12 Strahlentherapeuten das GTV anhand des gleichen Satzes von zur Verfügung gestellten Computertomogrammen. Die quantitative Analyse wurde unter Verwendung eines Expectation-Maximization-Algorithmus für die „Simultaneous Truth and Performance Level Estimation“ (STAPLE) in Verbindung mit einer zwischen den Ärzten vereinbarten Berechnung von Kappa-Statistiken durchgeführt. Um die Interobservervariabilität der GTV-Abgrenzung zu bestimmen, wurden das Verhältnis des tatsächlich abgegrenzten Volumens zum geschätzten Konsensvolumen (STAPLE), das Verhältnis des gemeinsamen Volumens zum umfassenden Volumen sowie der Variationskoeffizient berechnet.
Ergebnisse
Das mediane Kappa-Agreement-Level betrug 0,71 (Spanne 0,28–0,86). Das Verhältnis des tatsächlich abgegrenzten Volumens zum geschätzten Konsensvolumen lag in sämtlichen Fällen zwischen 0,19 und 1,93 (Mittelwert 0,94). Das Verhältnis des gemeinsamen Volumens zum umfassenden Volumen lag zwischen 0,001 und 0,56 (Mittelwert 0,25). Der Variationskoeffizient für die GTV-Abgrenzung lag im Bereich von 8–57 % (Mittelwert 26 %).
Schlussfolgerung
Die Interobservervariabilität in der Zielabgrenzung des HCC-GTV ist in dieser Studie bemerkenswert. Institutsübergreifende Studien für eine HCC-Strahlentherapie erfordern geeignete Qualitätssicherungsprogramme für die Zielabgrenzung.



Similar content being viewed by others
References
Park J, Won, Chen M et al (2015) Global patterns of hepatocellular carcinoma management from diagnosis to death: the BRIDGE Study. Liver Int 35:2155–2166
Seong J (2009) Challenge and hope in radiotherapy of hepatocellular carcinoma. Yonsei Med J 50:601–612
Hong TS, Bosch WR, Krishnan S et al (2014) Interobserver variability in target definition for hepatocellular carcinoma with and without portal vein thrombus: radiation therapy oncology group consensus guidelines. Int J Radiat Oncol Biol Phys 89:804–813
Genovesi D, CÃfaro GA, Vinciguerra A et al (2011) Interobserver variability of clinical target volume delineation in supra-diaphragmatic Hodgkin’s disease: a multi-institutional experience. Strahlenther Onkol 187:357–366
Vorwerk H, Beckmann G, Bremer M et al (2009) The delineation of target volumes for radiotherapy of lung cancer patients. Radiother Oncol 91:455–460
Cox BW, Spratt DE, Lovelock M et al (2012) International Spine Radiosurgery Consortium consensus guidelines for target volume definition in spinal stereotactic radiosurgery. Int J Radiat Oncol Biol Phys 83(e597):e605
Warfield SK, Zou KH, Wells WM (2004) Simultaneous truth and performance level estimation (STAPLE): an algorithm for the validation of image segmentation. IEEE Trans Med Imaging 23:903–921
Sim J, Wright C (2005) The kappa statistic in reliability studies: use, interpretation, and sample size requirements. Phys Ther 85:257–268
Villeirs GM, Van Vaerenbergh K, Vakaet L et al (2005) Interobserver delineation variation using CT versus combined CT + MRI in intensity-modulated radiotherapy for prostate cancer. Strahlenther Onkol 181:424–430
Weiss E, Hess CF (2003) The impact of gross tumor volume (GTV) and clinical target volume (CTV) definition on the total accuracy in radiotherapy theoretical aspects and practical experiences. Strahlenther Onkol 179:21–30
Van Hoe L, Haven F, Bellon E et al (1997) Factors influencing the accuracy of volume measurements in spiral CT: a phantom study. J Comput Assist Tomogr 21:332–338
Eriksen J, Salembier C, Rivera S et al (2014) Four years with FALCON – an ESTRO educational project: achievements and perspectives. Radiother Oncol 112:145–149
Rasch C, Barillot I, Remeijer P et al (1999) Definition of the prostate in CT and MRI: a multi-observer study. Int J Radiat Oncol Biol Phys 43:57–66
Rasch C, Keus R, Pameijer FA et al (1997) The potential impact of CT-MRI matching on tumor volume delineation in advanced head and neck cancer. Int J Radiat Oncol Biol Phys 39:841–848
Weltens C, Menten J, Feron M et al (2001) Interobserver variations in gross tumor volume delineation of brain tumors on computed tomography and impact of magnetic resonance imaging. Radiother Oncol 60:49–59
Voroney J, Brock K, Eccles C et al (2006) Prospective comparison of computed tomography and magnetic resonance imaging for liver cancer delineation using deformable image registration. Int J Radiat Oncol Biol Phys 66:780–791
Dawson LA, Guha C (2008) Hepatocellular carcinoma: radiation therapy. Cancer J 14:111–116
Xu H, Gong G, Wei H et al (2014) Feasibility and potential benefits of defining the internal gross tumor volume of hepatocellular carcinoma using contrast-enhanced 4D CT images obtained by deformable registration. Radiat Oncol 9:221
Pan T, Lee T, Rietzel E et al (2004) 4D-CT imaging of a volume influenced by respiratory motion on multi-slice CT. Med Phys 31:333–340
Hong TS, DeLaney TF, Mamon HJ et al (2014) A prospective feasibility study of respiratory-gated proton beam therapy for liver tumors. Pract Radiat Oncol 4:316–322
Beddar AS, Briere TM, Balter P et al (2008) 4D-CT imaging with synchronized intravenous contrast injection to improve delineation of liver tumors for treatment planning. Radiother Oncol 87:445–448
Acknowledgements
This work was supported by a grant (0620390) from the National R&D Program for Cancer Control, Ministry of Health and Welfare, Republic of Korea.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Y.S. Kim, J.W. Kim, W.S. Yoon, M.K. Kang, I.J. Lee, T.H. Kim, J.H. Kim, H.-S. Lee, H.C. Park, H.S. Jang, C.S. Kay, S.M. Yoon, M.-S. Kim, and J. Seong declare that they have no competing interests.
Ethical standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Additional information
Young Suk Kim and Jun Won Kim contributed equally.
Caption Electronic Supplementary Material
66_2016_1028_MOESM1_ESM.tif
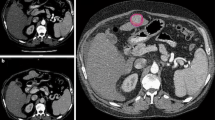
Supplementary fig. 1: Patient 1. The 95 % confidence level (S95) is shown in thicker red line. Lipiodol deposit after transarterial chemoembolization (TACE) presented with high-density nodule
66_2016_1028_MOESM2_ESM.tif
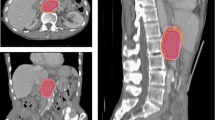
Supplementary fig. 2. Patient 2. The 95 % confidence level (S95) is shown in thicker red line. Tumor-to-parenchyma difference is minimal
Rights and permissions
About this article
Cite this article
Kim, Y.S., Kim, J.W., Yoon, W.S. et al. Interobserver variability in gross tumor volume delineation for hepatocellular carcinoma. Strahlenther Onkol 192, 714–721 (2016). https://doi.org/10.1007/s00066-016-1028-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00066-016-1028-2