Abstract
Objective
To detect connections between parameters of ventilation and outcomes of cardiac intensive care patients.
Design and setting
Noninterventional study. Between 05/11 and 05/12 all patients with acute heart failure and post cardiopulmonary resuscitation were registered. Lung protective ventilation was defined as peak inspiratory pressure (PIP) < 30 mmHg and tidal volume (Vt) < = 6 ml/kg.
Results
In total, 129 patients were included in the study, 68.2 % male, age 67.9 ± 13.4 years, weight 71.4 ± 37.2 kg, predictive body weight 66.9 ± 8.8 kg, mortality 47.3 %. Lung protective ventilated patients at day 1: 17.3 % with a significant difference between surviving and nonsurviving patients (24.1 % vs. 9.6 %; p < 0.05). Logistic regression models showed a strong connection between PIP and survival (odds ratio 1.13; p < 0.05). Vt showed no significant influence on survival.
Conclusion
Our data recommends a strict observance of a low PIP for cardiac intensive care patients, whereas Vt seems to be of secondary importance.
Zusammenfassung
Zielstellung
In dieser Studie sollen Zusammenhänge zwischen Beatmungsparametern und der Krankenhaussterblichkeit kardiologischer Intensivpatienten untersucht werden. Bislang gibt es nur wenige Empfehlungen zur Beatmung kardiologischer Intensivpatienten. Häufig wird auf Leitlinien zurückgegriffen, die für Patienten mit Acute Respiratory Distress Syndrome (ARDS) etabliert wurden. Diese Praxis soll überprüft werden.
Methoden
Alle beatmeten Patienten der internistischen Intensivstation (ITS) des Universitätsklinikum Halle (Saale) mit akuter Herzinsuffizienz (AHF) oder nach kardiopulmonaler Reanimation (CPR) zwischen 05/2011-05/2012 sind in die Beobachtungsstudie eingeschlossen. Als „lungenprotektiv beatmet“ gelten Patienten, die bei kontrolliertem Beatmungsmodus folgende Grenzwerte einhalten: PIP < 30 mmHg und Vt ≤ 6 ml/kg. Logistische Regressionen werden genutzt, um Korrelationen zwischen Beatmungsparametern und der Krankenhaussterblichkeit zu identifizieren.
Ergebnisse
Erfasst sind 129 Patienten, (68 % männlich; Alter 67,9 ± 13,4 Jahre; Körpergewicht (KG) 71,4 ± 37,2 kg, prädiktives KG 66,9 ± 8,8 kg, Krankenhaussterblichkeit 47,3 %). Lungenprotektiv beatmet sind an Tag 1 17,3 % der Patienten. 73,7 % der lungenprotektiv beatmeten und nur 48,4 % der nicht-lungenprotektiv beatmeten Patienten überleben (p < 0,05). Einen relevanten Zusammenhang mit der Mortalität zeigen außerdem die Parameter Beatmungsdruck (PIP) mit einer Odds Ratio (OR) von 1,15 (p = 0,001), FiO2 (OR: 1,03; p < 0,001), Horowitz-Index (OR: 0,97; p = 0,015), AaDO2 (OR: 1,03; p < 0,001) und driving pressure (OR: 1,11; p = 0,006).
Schlussfolgerung
Eine lungenprotektive Beatmung ist in dieser Studie mit einem Überlebensvorteil für die untersuchten kardiologischen Intensivpatienten assoziiert. Insbesondere die Einhaltung eines niedrigen PIP ist in dieser Studie prognostisch günstig, wohingegen der Einfluss des körpergewichts-bezogenen Tidalvolumens von untergeordneter Bedeutung erscheint.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Due to the paucity of clinical data, evidence-based recommendations for mechanical ventilation in cardiac intensive care patients are lacking. Therefore, it is a common practice to apply the guidelines that are established for patients suffering from acute respiratory distress syndrome (ARDS) [1] also to those patients with acute heart failure (AHF) and cardiogenic shock which are on mechanical ventilation [2].
In the ARDS guidelines, the parameters of lung protective ventilation (LPV) are well-established and is defined as ventilation mode with tidal volume (Vt) < 6 ml/kg predicted body weight (pBW) and a peak inspiratory pressure (PIP) < 30 mmHg [3].
This concept is mainly based on the ARDS-Network study, published in 2000, which had questioned the common practice of using higher Vts [1]. Before that study, Vts of 10–15 ml/kgBW were the standard of care because otherwise normal values of arterial carbon dioxide and pH value could often not be reached. The ARDS-Network study was the logical consequence of different experiments in animals which showed that high Vts are damaging the pulmonary endothelium and epithelium and increase the risk of hypoxemia, atelectasis, and increased release of inflammatory mediators [4]. It finally turned out that patients who were ventilated with low Vts showed a significant better survival [5]. Furthermore, the number of days without ventilation was increased and the inflammatory marker interleukin-6 was also found to be decreased within this group with LPV [4]. Additionally, Agnjen Gajic et al. [6] found an association between the use of high tidal volumina (> 6 ml/kg pBW) and the increase of acute lung injury while mechanical ventilation. Unlike for ARDS, there are much less findings regarding the best ventilation strategy in the patients suffering from cardiac disease. However, the clinical outcomes in these patients that are in need of mechanical ventilation are very unsatisfactory [7].
Based on the paucity of available data, even the related guidelines can give only restrained advice about the optimal ventilation strategy in cardiac intensive care [2]. It is emphasized that noninvasive ventilation (NIV) can improve physiological parameters (e.g., oxygen saturation) in patients with acute lung edema. Nevertheless, so far it has not been conclusively shown that mortality or intubation rate in these patients is significantly decreased by NIV [8].
According to the ESC guidelines on heart failure [9], endotracheal intubation and mechanical ventilation are indicated in patients with AHF in the case of respiratory failure, hypercapnia, hypoxia, or acidosis [9].
The aim of our study was to describe how patients with severe AHF or after cardiopulmonary resuscitation (CPR) are ventilated in everyday clinical practice and to identify correlations between ventilator settings and clinical outcomes in these patients.
Methods
During a period of 12 months (01-MAY-2011 until 30-APR-2012), all mechanically ventilated patients at the medical intensive care unit (ICU; 13 beds) of the University Hospital of Halle (Saale), Germany, were included in the study if ICU admission was primarily due to cardiac disease. All patients were observed in a prospective way. Overall, 129 patients were included in the study. Among these, there were 79 patients with AHF and 50 patients after successful CPR. The 79 patients with AHF consisted of 23 (29 %) patients with cardiogenic shock, 27 (34 %) patients with lung edema, 14 (18 %) patients with ST-segment elevation myocardial infarction, and 15 (19 %) patients with non-ST elevation myocardial infarction.
After admission to the ICU, the following parameters were recorded: medical history, height, body weight, pBW, body mass index (BMI), and APACHE II-score. Furthermore, the following parameters of ventilation were documented immediately after ICU-admission and thereafter on a daily basis at 06:00 am: mode of ventilation, PIP, positive end-expiratory pressure (PEEP), respiratory rate, fraction of inspired oxygen (FiO2), Vt, minute volume, Horowitz-Index (HI, calculated as follows: HI = paO2/FiO2), arterio-alveolar oxygen-pressure difference (AaDO2, calculated as follows: 103,8 * FiO2– paCO2– paO2) and driving pressure (driving pressure = PIP –PEEP). Additionally, parameters of blood gas analysis and the following outcome parameters were prospectively recorded: need for tracheotomy, need of renal replacement therapy, in-hospital mortality, length of hospital stay.
In accordance with the ARDS network guidelines [1], a patient who was in a pressure-controlled mode of ventilation (BIPAP or PC) was considered to be treated with “LPV” if the following ventilator settings were chosen: PIP < 30 mmHg and Vt < = 6 ml/kg pBW (calculated for men: 50 + 0,91 [body size (cm)—152,4] and women: 45,5 + 0,91 [body size (cm)—152,4] [2]). All clinical parameters were collected every day at 6:00 am for the first 7 days under mechanical ventilation. The primary endpoint of the study was hospital mortality.
At the ICU, the following ventilators were used: Evita Infinity® V500 (Draeger), Evita Infinity® C500 (Draeger), Evita XL® (Drager), Servo Ventilator® 300A (Siemens).
The analysis of the data was performed with SPSS Statistics 20.0 (SPSS Inc. Chicago, IL, USA). All data were recorded in an anonymous way. The study was performed according to the regulations of the ethics committee of the Martin Luther University Halle-Wittenberg.
Results
During the period of observation, 129 patients with cardiovascular disease requiring mechanical ventilation were included into the study. The demographic data, the medical history, and the outcome parameters are shown in Tab. 1. As expected, mortality was significantly higher in patients after CPR in comparison to patients with AHF.
Ventilator settings and the derived parameters during the course of ventilation are given in Tab. 2. As seen in the table, the percentage of patients with augmented spontaneous breathing was only 20 % on day 1 but subsequently rose up to 80 % on day 7. In parallel, mean PIP showed a clear decrease from day 1 to day three and remained stable thereafter. Vt was kept at a relatively constant level over the analyzed period of time.
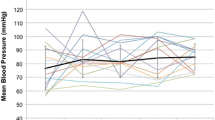
Within the 129 patients, only 17.3 % received LPV on day 1 (AHF: 13 pat. = 18.8 %; CPR: 6 pat. = 14.6 %). However, the early establishment of LPV was associated with an improved survival as seen from Fig. 1.
Tab. 3 shows in more detail which percentage of patients reached the two different ventilation goals (PIP; Vt) that together determine LPV. Obviously, the cutoff for PIP was maintained in a high percentage of patients throughout the whole observational period whereas the Vt exceeded 6 ml/kgBW in the vast majority of patients throughout the study.
For more precise information about the impact of PIP or Vt on hospital mortality, two binary logistic regression models were established (Tab. 4). All patients receiving pressure controlled respiratory modes (PC, BIPAP) were included in this model. First, the individual parameters were analyzed in a univariante way. Additionally, the analysis was repeated in a multivariate manner were the potential confounders age, BMI, APACHE II score on admission and application of catecholamines were taken into consideration. The parameters age and body mass index were chosen linked to their influence in prior morbidity. As markers for the severity of disease, APACHE II score and the use of catecholamines were selected. APACHE II score lines out the severity of disease after admission on the ICU and the use of catecholamines the severity of cardiogenic shock.
It turns out that both in the univariante as well as in the multivariate model PIP is closely linked to mortality whereas, however, such a correlation cannot be found for Vt.
Discussion
Both patients with AHF and patients post CPR are mostly critically ill and have poor outcomes—especially if they are in need of mechanical ventilation. There are different theories why respiratory failure and the use of mechanical ventilation increase the mortality of patients with AHF. One of the reasons could be that these patients often already suffer from cardiogenic shock and subsequent systemic hypoperfusion [10]. Another explanation is that the ventilation-induced increase in intrathoracic pressure has a complex influence on left and right heart function. For an instance, it has been shown that small changes in the intrathoracic pressure can result in large changes in stroke volume [10].
The outcomes in patients after CPR remain poor, even though many efforts have been made to increase the survival of these patients. In an analysis of 12,000 patients treated by emergency medical services (EMS) in Seattle, the percentage of patients that were discharged alive from hospital after cardiac arrest did not differ significantly between 1998–2001 and 1977–1981 (15.7 vs. 17.5 %) [11]. This study also tried to find reasons for the overall poor survival of these patients but was not able to determine specific causes which could be potentially influenced by therapeutic strategies [11]. These results underline the need for further attempts to improve the survival of critically ill patients with cardiac disease.
While there are a number of profound studies regarding mechanical ventilation in ARDS patients, nearly no high-quality evidence exists on mechanical ventilation in cardiac intensive care patients. Therefore, the optimal ventilation strategy for AHF patients is unknown and the recommendations regarding mechanical ventilation in AHF-patients are mainly based on the ARDS-studies [2], as the guideline Cardiogenic Shock Due to Myocardial Infarction recommends [2].
As something like a first step on the way to evidence-based ventilation strategies in cardiac intensive care patients, our study presented here tried to describe how patients suffering from AHF or survived sudden cardiac death are ventilated in everyday clinical practice.
In our study, 89 % of the patients were ventilated with a PIPof less than 30 mmHg on the first day after initiation of ventilation with a further increase of this number within the next days. However, only 22.4 % of these patients received ventilation using low Vts with Vt < 6 ml/kgBW. Accordingly, the percentage of patients receiving “LPV” defined as the combination of both low Vt and PIP was even lower (17.3 %).
Although these numbers are certainly far away from our treatment goals, they are in line with previous reports showing that in everyday practice the adherence to ventilation guidelines is still limited. An analysis from 2004 of 10 ICUs in Europe showed that only 8 % of the included patients were ventilated using Vt < 6 ml/kgKG [12]. This is of note because already in 2000 it had been conclusively shown that the application of low Vts is indeed beneficial for patients with ARDS: the ARDS-network found a mortality rate of 39.8 % in the patients treated with traditional Vts that was significantly reduced to 31.0 % in patients ventilated with lower Vts. Similar to the study of Brun-Buisson et al. [12] the reason for the low percentage of lung protected ventilated patients in this study remain unclear.
These finding can also be seen in our study with cardiac intensive care patients: these patients show a better survival if the LPV was applied early. In our analysis, 73.7 % of the patients treated with LPV survived, whereas only 48.4 % patients of the patients ventilated in a non-lung-protective could be discharged alive. This result indicates that the early use of LPV as established for ARDS is also reasonable in patients with AHF and post CPR.
In our study, different parameters of ventilation were linked to the prognosis of cardiac intensive care patients, whereas other parameters seemed to be of less importance. As expected, both FiO2, HI as well as AaDO2 which all can be considered as markers of the severity of gas exchange disturbance were significantly linked to mortality (both univariate and multivariate logistic regression model).
Most of these parameters are also known to be of prognostic importance in ARDS patients from earlier studies [13].
These parameters mentioned above reflect the disturbance of the pulmonary gas exchange. However, our logistic regression analyses also revealed that there are ventilator settings which are directly tuned by the treating physicians that seem to have a significant influence on mortality in cardiac intensive care patients. Unexpectedly, our analysis suggests that in cardiac intensive care patients the limitation of PIP seems to be of much more importance than the adherence to a Vt of 6 ml/kg. This is contrary to the results of the studies in ARDS-patients that suggest both parameters to be important for the clinical outcome [3].
The ALKK registry had previously shown that the main ventilation mode in patients suffering from acute myocardial infarction was BIPAP and CPPV (continous positive pressure ventilation). There was a significant increase in mortality in patients with CPPV-use [7]. This connection could not be shown in our study because only patients with pressure controlled modes were included in the regression analysis.
It is noteworthy that in our study, the influence of the different parameters of mechanical ventilation on clinical outcomes was found for the whole cohort of cardiac intensive care patients whereas statistical significance got lost in the two subgroups of patients suffering from acute heart failure and after cardiopulmonal resuscitation. This might be explained by the limited number of AHF and CPR patients within the study. Furthermore, the low percentage of lung protective ventilated patients in this study could influence the results. Future studies with larger numbers of patients will have to deepen the influence on these two groups.
Conclusion
In summary, the results of the study presented here suggest that a lung protective way of ventilation with a limitation of both PIP as well as Vt as it has become standard of care for patients suffering from ARDS might also be advantageous for cardiac ICU patients. Especially the strict reduction of PIP seems to be of prognostic importance and might be even more relevant than the limitation of Vt.
References
The Acute Respiratory Distress Syndrome Network (2000) Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The Acute Respiratory Distress Syndrome Network. N Engl J Med 342:1301–1308
Werdan K, Ruß M, Buerke M, Delle-Karth G, Geppert A, Schöndube FA (2012) Cardiogenic shock due to myocardial infarction: diagnosis, monitoring and treatment: a German-Austrian S3 Guideline. Dtsch Arztebl Int 109(19):343-351
Reinhart K, Brunkhorst FM, Bone H, Bardutzky J, Dempfle C, Forst H, Gastmeier P et al (2010) Prevention, diagnosis, therapy and follow-up care of sepsis: 1st revision of S-2k guidelines of the German Sepsis Society (Deutsche Sepsis-Gesellschaft e. V. (DSG)) and the German Interdisciplinary Association of Intensive Care and Emergency Medicine (Deutsche Interdisziplinäre Vereinigung für Intensiv- und Notfallmedizin (DIVI)). Ger Med Sci 8:Doc14
Tsuno K, Miura K, Takeya M, Kolobow T, Morioka T (1991) Histopathologic pulmonary changes from mechanical ventilation at high peak airway pressures. Am Rev Respir Dis 143:1115–1120
Biener I, Czaplik M, Bickenbach J, Rossaint R (2013) Lungenprotektive Beatmung bei ARDS. Med Klin Intensivmed Notfmed 108:578–583
Gajic O, Dara SI, Mendez JL, Adesanya AO, Festic E, Caples SM, Rana R et al (2004) Ventilator-associated lung injury in patients without acute lung injury at the onset of mechanical ventilation. Crit Care Med 32:1817–1824
Kouraki K, Schneider S, Uebis R, Tebbe U, Klein HH, Janssens U, Zahn R et al (2011) Characteristics and clinical outcome of 458 patients with acute myocardial infarction requiring mechanical ventilation. Results of the BEAT registry of the ALKK-study group. Clin Res Cardiol 100:235–239
Gray A, Goodacre S, Newby DE, Masson M, Sampson F, Nicholl J (2008) Noninvasive ventilation in acute cardiogenic pulmonary edema. N Engl J Med 359:142–151
McMurray JJV, Adamopoulos S, Anker SD, Auricchio A, Böhm M, Dickstein K, Falk V et al (2012) ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur Heart J 33:1787–1847
Oczenski W (2012) Atmen: Atemhilfen; Atemphysiologie und Beatmungstechnik. 9th ed. s.l: Georg Thieme Verlag KG, Stuttgart
Rea TD, Eisenberg MS, Becker LJ, Murray JA, Hearne T (2003) Temporal trends in sudden cardiac arrest: a 25-year emergency medical services perspective. Circulation 107:2780–2785
Brun-Buisson C, Minelli C, Bertolini G, Brazzi L, Pimentel J, Lewandowski K, Bion J et al (2004) Epidemiology and outcome of acute lung injury in European intensive care units. Results from the ALIVE study. Intensive Care Med 30:51–61
Rice TW, Wheeler AP, Bernard GR, Hayden DL, Schoenfeld DA, Ware LB (2007) Comparison of the SpO2/FIO2 ratio and the PaO2/FIO2 ratio in patients with acute lung injury or ARDS. Chest 132:410–417
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M. Schneck, K. Holder, S. Gielen, S. Nuding, J. Schröder, A.R. Tamm, K. Werdan and H. Ebelt state that there are no conflicts of interest.
All procedures followed were in accordance with the ethical standards of the ethics committee of the Martin Luther University Halle-Wittenberg.
Additional information
Redaktion
M. Buerke, Siegen
K. Holder and M. Schneck contributed equally to this work.
Rights and permissions
About this article
Cite this article
Schneck, M., Holder, K., Gielen, S. et al. Lung protective ventilation and hospital survival of cardiac intensive care patients. Med Klin Intensivmed Notfmed 111, 508–513 (2016). https://doi.org/10.1007/s00063-015-0105-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00063-015-0105-0
Keywords
- Lung protective ventilation
- Acute heart failure
- Cardiopulmonary resuscitation
- Tidal volume
- Peak inspiratory pressure
- Lung protection