Abstract
Purpose
Theophylline has been suggested to have a neuroprotective effect in ischemic stroke; however, results from animal stroke models and clinical trials in humans are controversial. The aim of this study was to assess the effect of theophylline on the cerebral perfusion with multiparametric magnetic resonance imaging (MRI).
Methods
The relative cerebral blood flow (rCBF), relative cerebral blood volume (rCBV), and relative mean transit time (rMTT) in the infarct core, penumbra, and unaffected tissue were measured using multi-parametric MRI at baseline and 3‑h follow-up in patients treated with theophylline or placebo as an add-on to thrombolytic therapy.
Results
No significant differences in mean rCBF, rCBV, and rMTT was found in the penumbra and unaffected tissue between the theophylline group and the control group between baseline and 3‑h follow-up. In the infarct core, mean rCBV increased on average by 0.05 in the theophylline group and decreased by 0.14 in the control group (p < 0.04). Mean rCBF and mean rMTT in the infarct core were similar between the two treatment groups.
Conclusion
The results indicate that theophylline does not change the perfusion in potentially salvageable penumbral tissue but only affects the rCBV in the infarct core. In contrast to the penumbra, the infarct core is unlikely to be salvageable, which might explain why theophylline failed in clinical trials.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The neuroprotective effect of theophylline is controversial with conflicting results in animal ischemic stroke models and previous clinical trials in humans. Animal stroke models have demonstrated reduced ischemic brain damage, reduced perifocal edema, and reduced mortality by preconditioning or perconditioning with theophylline [1,2,3]; however, previous randomized clinical trials failed to demonstrate improved clinical outcome in humans [4, 5].1
Theophylline acts as a phosphodiesterase inhibitor and competitive adenosine receptor antagonist with well-documented effects in the respiratory system [6]; however, the vasoactive effect of theophylline on ischemic brain tissue is not fully understood. Inhibition of phosphodiesterase increases cyclic adenosine monophosphate that subsequently activates calcium-activated potassium channels and adenosine triphosphate-sensitive potassium channels, which causes vasodilatation [7]; however, inhibition of adenosine receptor causes cerebral vasoconstriction [8, 9]. This vasoconstriction was previously found in cortical tissue in animal stroke models and humans, but not in ischemic tissue [10, 11]. Regional cerebral blood flow (CBF) measured using the Xenon-133 arterial injection technique demonstrated that theophylline decreases regional CBF in areas of normal brain tissue and increases regional CBF in areas of stroke, a phenomenon described as inverse intracerebral steal [12].
In contrast to the previous studies, dynamic susceptibility contrast-enhanced magnet resonance imaging (MRI) allows not only the cerebral blood flow, cerebral blood volume (CBV), and mean transit time (MTT) [13] to be quantified but also to differentiate between the infarct core and the penumbra in patients with acute ischemic stroke [14]; however, this imaging technique has not been used to investigate potential effects of theophylline on the regional cerebral perfusion.
The aim of this study was to investigate the effect of theophylline on perfusion in the infarct core and penumbra in patients with acute ischemic stroke.
Material and Methods
Study Objective
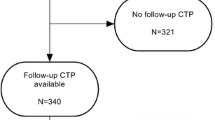
This subgroup study is based on the theophylline in acute ischemic stroke trial, a proof-of-concept, randomized, double-blinded, placebo-controlled trial that assessed the neuroprotective effect of theophylline as an add-on to thrombolytic therapy (EudraCT number 2013-001989-42). The trial protocol was approved by the Danish Health and Medicines Authorities (ref. no. 2013050908) and the Regional Scientific Ethics Committee (ref.-no. N‑20130034) [15]. The main inclusion criteria were MRI verified moderate to severe stroke symptoms (National Institutes of Health Stroke Scale [NIHSS] ≥4), eligibility for thrombolytic therapy within 4.5 h of symptom onset and written informed consent. The trial was terminated early due to slow recruitment. The co-primary endpoints, early clinical improvement and infarct growth at 24 h follow-up, were without significant difference after correction for multiplicity [16].
This preplanned sub-group analysis included all patients with multiparametric MRI including perfusion-weighted imaging available at baseline and 3–4 h follow-up (in the following referred as 3‑h follow-up). This interval was chosen for follow-up imaging as theophylline is expected to be still active (half-life 3–9 h) at this time.
Image Acquisition
Multiparametric MRI was performed with the same field strength (1.5 or 3.0 T) at baseline and at 3‑h follow-up including diffusion-weighted MRI (DWI), perfusion-weighted MRI (PWI) with intravenous gadolinium (0.1 mmol per kg body weight, 5 ml/s bolus injection), circle of Willis time-of-flight MR angiography (TOF MRA), and fluid-attenuated inversion recovery (FLAIR) MRI. The thrombolysis in myocardial infarction (TIMI) grading was used to grade arterial obstruction [17]. Large vessel occlusion was defined as TIMI 0–1 at baseline and conversion from TIMI 0–1 at baseline to 2–3 at 3‑h follow-up was defined as revascularization.
Imaging Post-Processing
Image analysis of the DWI and PWI MRI datasets was performed using the semi-automatic software tool AnToNIa [18]. In brief, the b0 and b1000 mm2/s DWI datasets were used to calculate an apparent diffusion (ADC) dataset. A semi-automatic volume growing approach with a rather conservative upper ADC threshold of 550 × 10−6 mm2/s, in accordance with previous stroke studies [19], was used to segment the infarct core region of interest (ROI). This threshold was used to ensure that no penumbra tissue is part of the infarct core. The PWI dataset was automatically motion corrected and the arterial input function was manually identified from the internal carotid artery and middle cerebral artery (M1 segment). After this, a block-circulant deconvolution-based perfusion analysis with a threshold of 0.15 was applied to calculate the CBF, CBV, MTT, and time to maximum (Tmax) of the residual function. After this, relative perfusion maps (rCBF, rCBV, rMTT, and rTmax) were computed using mean values from contralateral brain tissue, excluding cerebrospinal fluid, and registered to the ADC dataset. More precisely, subtraction was used for the temporal parameters (rMTT and rTmax), while division was used for calculation of the rCBV and rCBF maps. The rTmax map was then used to segment the hyperperfused tissue applying a semiautomatic volume growing approach with a lower Tmax threshold of 6 s [20]. The penumbra ROI was computed by subtracting the infarct core ROI from the hypoperfusion ROI (perfusion-diffusion mismatch). The unaffected tissue ROI was computed by subtracting infarct core and penumbra ROIs from the brain segmentation in the affected hemisphere. The mean rCBV, rCBF, and rMTT values were calculated for the infarct core ROI, penumbra ROI, and unaffected tissue ROI using the baseline relative perfusion parameter maps. The same baseline ROIs were applied to calculate the average perfusion parameters in the 3‑h follow-up PWI dataset registered to the acute ADC dataset (Fig. 1).
Axial section of the brain using multi-parametric MRI with semiautomatic imaging post-processing: a T-max map; b apparent diffussion (ADC) map; c ADC map with cerebrospinal fluid (CSF) segmentation; d infarct core region of interest (ROI) (red), e infarct core ROI (red) and penumbra ROI (bright green); f infarct core ROI (red), penumbra ROI (bright green), unaffected tissue ROI (light green)
Thus, ADC, rCBF, rCBV, and rMTT values were available for the infarct core, penumbra, and the unaffected tissue at baseline and 3‑h follow-up.
Clinical Assessment
Clinical improvement was described in several case series and non-randomized clinical trials immediately after administration of theophylline. For that reason, healthcare professionals blinded to the allocation of the study medication assessed the clinical improvement defined as improvement in the National Institute of Health Stroke Scale (NIHSS) score by ≥4 points from baseline to 3‑h follow-up. Furthermore, blood pressure and heart rate were measured at baseline and 3‑h follow-up to assess the positive inotropic and chronotropic effect of theophylline.
Theophylline Concentration Assessment
A blood sample was taken to assess the blood serum concentration of theophylline at 3‑h follow-up.
Statistical Analyses
Baseline characteristics were summarized by mean and standard deviation (SD) for continuous data and counts and percentages for categorical data. Continuous data were compared with a two-sided t‑test or Wilcoxon’s rank sum test and categorical data were compared using Fisher’s exact test.
A Wilcoxon’s rank sum test was used to compare baseline and follow-up rCBF, rCBV, and rMTT within the infarct core, penumbra, and unaffected tissue. A two-sided t‑test with equal variances was used to compare the differences in relative perfusion parameters from baseline to follow-up. All tests were applied as post hoc analyses as the preplanned substudy analysis was omitted due to slow recruitment and early termination of the trial. A two-sided alpha level of 0.05 without correction for multiple comparisons was applied for this explorative analysis. Stata/MP version 16.1 (Stata Corp LLC, College Station, TX, USA) was used for the statistical analysis.
Anonymized data that support the findings of this study are available from the corresponding author upon reasonable request.
Results
Study Population
An MRI at 3‑h follow-up was acquired and available in 24 out of 64 patients included in the theophylline as an add-on to thrombolytic therapy trial. Of the patients 13 were treated with theophylline and 11 patients were treated with placebo. Baseline patient characteristics, including baseline imaging parameters, process measures, and main follow-up characteristics were not significantly different between the two groups (Table 1). The change in heart rate from baseline to 3‑h follow-up was significantly different (p < 0.05) in the theophylline group (mean increase by 11 beats per minute, SD 26) compared to the control group (mean decrease by 9 beats per minute, SD 14). The change in systolic blood pressure (−12 mm Hg, SD 14 versus −8 mm Hg, SD 25; p = 0.62) and the diastolic blood pressure (−9 mm Hg, SD 8 versus −12 mm Hg, SD 12; p = 0.51) from baseline to 3‑h follow-up was similar in the theophylline group and the control group. Clinical improvement at 3‑h follow-up was present in 1 (8%) patient in the theophylline group and 2 patients (18%) in the control group (p = 1.0). Large vessel occlusion (LVO) at baseline was identified by TOF MRA in 11 patients. Recanalization was found in 7 of 7 patients with LVO in the theophylline group and in 2 of 4 in the control group (p = 0.11). The mean theophylline concentration in the theophylline group was 4.9 mg/l (SD 1.5) at 3‑h follow-up.
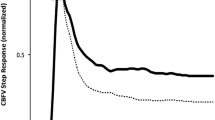
Infarct Core
The mean rCBF values in the infarct core at baseline and follow-up as well as the change from baseline to 3‑h follow-up were similar in the theophylline group and the control group (p = 0.47). The mean rCBV was similar at baseline (p = 0.34) but significantly higher at 3‑h follow-up in the theophylline group (p < 0.01). Likewise, there was a statistically significant difference (p < 0.04) regarding the mean rCBV change from baseline to 3‑h follow-up in the theophylline group (mean = 0.05; SD = 0.18) compared to the control group (mean = −0.14; SD = 0.24; Table 2). The mean ADC and rMTT values at baseline and 3‑h follow-up, and the corresponding changes from baseline to 3‑h follow-up were similar between the two groups (Fig. 2).
Penumbra
No significant differences were found comparing the mean ADC, rCBF, rCBV, and rMTT values at baseline and 3‑h follow-up in the penumbra between the theophylline group and the control group (Table 2; Fig. 2).
Unaffected Tissue
Likewise, the mean ADC, rCBF, rCBV, and rMTT values in the unaffected tissue at baseline and 3‑h follow-up were similar between the theophylline group and the control group (Table 2; Fig. 2).
Discussion
Our data suggest that theophylline, as an add-on to thrombolytic therapy in acute ischemic stroke, does not significantly affect the rCBF, rCBV, or rMTT in the penumbra or the unaffected tissue. The only significant difference found between the two groups was the change in rCBV from baseline to 3‑h follow-up in the infarct core with higher values in the theophylline group and lower values in the control group. The rCBF and rMTT in the infarct core were unaffected.
The perfusion parameters CBF, CBV, and MTT are established parameters to define the infarct core and penumbra in acute ischemic stroke patients [21,22,23]; however, the applied thresholds to distinguish infarct core from penumbra and the prediction of outcome and final infarct volume vary across different studies [24,25,26]. The interpretation of the different parameters can be difficult, especially as the calculation of the perfusion parameters is complex and different methods are used in studies [23]. In ischemic lesions, uncoupling of CBV and CBF can occur in parts of the lesion with regionally reduced or increased CBV and CBF values [27]. The initial response of brain tissue to a decrease of cerebral perfusion pressure is to dilate the vessels in the ischemic area to maintain the CBF [21]. Our data showed significant changes in mean rCBV in the infarct core at 3‑h follow-up with higher values in the theophylline group. At this point, it remains speculative whether the increased rCBV in the infarct core in the theophylline group is due to the positive chronotropic and inotropic effect of theophylline; however, this theory might be supported by our finding of a significant difference in heart rate with higher values in the theophylline group, which could be an indicator for increased cardiac output with subsequent increased mean arterial pressure, increased cerebral perfusion pressure, and finally increased rCBV. Another explanation might be the inverse intracerebral steal (the so-called Robin Hood phenomenon) with vasoconstriction and decreased CBF in healthy brain tissue and increased CBF in ischemic tissue previously described by Skinhøj and Paulson, which might also have an effect of CBV [11, 12]; however, our results do not really support this explanation, as no significant rCBF change in the infarct core, and especially no decrease of rCBF in the unaffected tissue, was observed from baseline to 3‑h follow-up. Even more important, the rCBF, rCBV, and rMTT in the penumbra was not significantly different between the theophylline group and control group. The lack of improved perfusion in the salvageable penumbra might explain absence of a clinical effect and failure to reduce the final infarct volume by theophylline [16] as the infarct core was the only region which showed significant differences in rCBV but is commonly assumed to be non-salvageable. It should also be mentioned that there is experimental evidence that adenosine released by astrocytes during ischemia might have a protective effect on neurons [28] and microcirculation [9]. Thus, the inhibition of the adenosine receptor by theophylline might have a counterproductive effect.
A comparison of our data with previous studies is difficult, as patient selection, trial medication application, and imaging techniques are substantially different. These studies demonstrated intracerebral vasoconstriction and decreased CBF when theophylline was applied as bolus injection into the internal carotid artery [11] or intravenously [12], whereas a short intravenous infusion of theophylline over 15 min was used in our study. The previous studies measured the CBF almost immediately after administration of theophylline in contrast to our measurements after 3–4 h; however, the average serum theophylline concentration of 4.9 mg/l in our trial is comparable with the concentration found in the study of Magnussen et al. [29]. The authors reported a serum theophylline concentration of about 5 mg/l and a 22% reduced global CBF 45 min after bolus injection of 250 mg of theophylline. Thus, it remains uncertain if the different types of theophylline administrations and/or the timing of the CBF measurements can explain the controversial results.
The strength of our study compared to previous studies is a dataset from a randomized, placebo-controlled trial design with MRI-verified ischemic stroke patients. The main limitation of our analysis is the small number of patients included in this secondary study caused by the early termination of the main trial due to slow recruitment. Thus, the varying infarct core and penumbra volumes, with and without large vessel occlusion, and with and without revascularization at follow-up is a limitation. Another limitation might be our definition of the infarct core and the penumbra. Spreading depolarization, often a single terminal event that mediates neuronal death in the infarct core, causes cytotoxic edema with restricted diffusion in the intracellular and extracellular spaces that decrease the signal in the ADC maps [30]; however, a normalization of the ADC lesion can be seen in cases of tissue reperfusion, especially within 3 h after stroke onset [31]. Thus, due to the dynamics of the ADC lesion, the infarct core definition in this study might limit the interpretability of the perfusion changes in the infarct core; however, our data did not show perfusion changes in the penumbra and unaffected brain tissue, which contradicts the hypothesis of the inverse intracerebral steal, namely vasoconstriction of the healthy tissue in favor for the salvageable penumbra (Robin Hood phenomenon). These findings might explain the lack of clinical improvement after 3‑h follow-up in this study, lack of early clinical improvement or reduced infarct growth at 24‑h follow-up in the main trial [16] and lack of clinical improvement in previous clinical trials [4, 5].
In conclusion, our results indicate that theophylline does not change the perfusion in potentially salvageable penumbra in acute ischemic stroke, but only affects the rCBV in the infarct core. In contrast to penumbral tissue, the infarct core is unlikely to be salvageable, which might explain why theophylline fails to reduce the final infarct volume and fails to improve the clinical outcome.
References
Kogure K, Scheinberg P, Busto R, Reinmuth OM. An effect of aminophylline in experimental cerebral ischemia. Trans Am Neurol Assoc. 1975;100:77–80.
Seida M, Wagner HG, Vass K, Klatzo I. Effect of aminophylline on postischemic edema and brain damage in cats. Stroke. 1988;19:1275–82.
Bona E, Ådén U, Gilland E, Fredholm BB, Hagberg H. Neonatal cerebral hypoxia-ischemia: the effect of adenosine receptor antagonists. Neuropharmacology. 1997;36:1327–38.
Geismar P, Marquardsen J, Sylvest J. Controlled trial of intravenous aminophylline in acute cerebral infarction. Acta Neurol Scand. 1976;54:173–80.
Britton M, de Faire U, Helmers C, Miah K, Rane A. Lack of effect of theophylline on the outcome of acute cerebral infarction. Acta Neurol Scand. 1980;62:116–23.
Barnes PJ. Theophylline. Pharmaceuticals. 2010;3:725–47.
Brian JE, Faraci FM, Heistad DD. Recent insights into the regulation of cerebral circulation. Clin Exp Pharmacol Physiol. 1996;23:449–57.
Li J, Iadecola C. Nitric oxide and adenosine mediate vasodilation during functional activation in cerebellar cortex. Neuropharmacology. 1994;33:1453–61.
Dreier JP, Tille K, Dirnagl U. Partial antagonistic effect of adenosine on inverse coupling between spreading neuronal activation and cerebral blood flow in rats. Neurocrit Care. 2004;1:85–94.
Regli F, Yamaguhi T, Waltz AG. Responses of surface arteries and blood flow of Ischemic and nonischemic cerebral cortex to aminophylline comma ergotamine tartrate comma and Acetazolamide. Stroke. 1971;2:461–70.
Gottstein U, Paulson OB. The effect of intracarotid aminophylline infusion on the cerebral circulation. Stroke. 1972;3:560–5.
Skinhøj E, Paulson OB. The mechanism of action of aminophylline upon cerebral vascular disorders. Acta Neurol Scand. 1970;46:129–40.
Hatazawa J, Shimosegawa E, Toyoshima H, Ardekani BA, Suzuki A, Okudera T, Miura Y. Cerebral blood volume in acute brain infarction: A combined study with dynamic susceptibility contrast MRI and 99mTc-HMPAO-SPECT. Stroke. 1999;30:800–6.
Røhl L, Ostergaard L, Simonsen CZ, Vestergaard-Poulsen P, Andersen G, Sakoh M, Le Bihan D, Gyldensted C. Viability thresholds of ischemic penumbra of hyperacute stroke defined by perfusion-weighted MRI and apparent diffusion coefficient. Stroke. 2001;32:1140–6.
Modrau B, Hjort N, Østergaard L, Mouridsen K, Andersen G, Bach FW. Theophylline as an add-on to thrombolytic therapy in acute ischaemic stroke (TEA-Stroke): A randomized, double-blinded, placebo-controlled, two-centre phase II study. Eur Stroke J. 2016;1:248–54.
Modrau B, Andersen G, Mikkelsen IK, Nielsen A, Hansen MB, Johansen MB, Eskildsen HW, Povlsen JP, Yavarian Y, Mouridsen K, Østergaard L, Bach FW, Hjort N. Theophylline as an add-on to thrombolytic therapy in acute ischemic stroke: a randomized placebo-controlled trial. Stroke. 2020;51:1983–90.
Zaidat OO, Yoo AJ, Khatri P, Tomsick TA, von Kummer R, Saver JL, Marks MP, Prabhakaran S, Kallmes DF, Fitzsimmons BF, Mocco J, Wardlaw JM, Barnwell SL, Jovin TG, Linfante I, Siddiqui AH, Alexander MJ, Hirsch JA, Wintermark M, Albers G, Woo HH, Heck DV, Lev M, Aviv R, Hacke W, Warach S, Broderick J, Derdeyn CP, Furlan A, Nogueira RG, Yavagal DR, Goyal M, Demchuk AM, Bendszus M, Liebeskind DS; Cerebral Angiographic Revascularization Grading (CARG) Collaborators; STIR Revascularization working group; STIR Thrombolysis in Cerebral Infarction (TICI) Task Force. Recommendations on angiographic revascularization grading standards for acute ischemic stroke: a consensus statement. Stroke. 2013;44:2650–63.
Forkert ND, Cheng B, Kemmling A, Thomalla G, Fiehler J. ANTONIA perfusion and stroke: a software tool for the multi-purpose analysis of MR perfusion-weighted datasets and quantitative ischemic stroke assessment. Methods Inf Med. 2014;53:469–81.
Siemonsen S, Löbel U, Sedlacik J, Forkert ND, Mouridsen K, Østergaard L, Thomalla G, Fiehler J. Elevated T2-values in MRI of stroke patients shortly after symptom onset do not predict irreversible tissue infarction. Brain. 2012;135:1981–9.
Olivot JM, Mlynash M, Thijs VN, Kemp S, Lansberg MG, Wechsler L, Bammer R, Marks MP, Albers GW. Optimal Tmax threshold for predicting penumbral tissue in acute stroke. Stroke. 2009;40:469–75.
Deok HL, Kang DW, Jae SA, Choong GC, Sang JK, Dae CS. Imaging of the ischemic penumbra in acute stroke. Korean J Radiol. 2005;6:64–74.
Neumann-Haefelin T, Wittsack HJ, Wenserski F, Siebler M, Seitz RJ, Mödder U, Freund HJ. Diffusion- and perfusion-weighted MRI. The DWI/PWI mismatch region in acute stroke. Stroke. 1999;30:1591–7.
Schlaug G, Benfield A, Baird AE, Siewert B, Lövblad KO, Parker RA, Edelman RR, Warach S. The ischemic penumbra: operationally defined by diffusion and perfusion MRI. Neurology. 1999;53:1528–37.
Butcher K, Parsons M, Baird T, Barber A, Donnan G, Desmond P, Tress B, Davis S. Perfusion thresholds in acute stroke thrombolysis. Stroke. 2003;34:2159–64.
Grandin CB, Duprez TP, Smith AM, Oppenheim C, Peeters A, Robert AR, Cosnard G. Which MR-derived perfusion parameters are the best predictors of infarct growth in hyperacute stroke? Comparative study between relative and quantitative measurements. Radiology. 2002;223:361–70.
Parsons MW, Yang Q, Barber PA, Darby DG, Desmond PM, Gerraty RP, Tress BM, Davis SM. Perfusion magnetic resonance imaging maps in hyperacute stroke: relative cerebral blood flow most accurately identifies tissue destined to infarct. Stroke. 2001;32:1581–7.
Parsons MW, Barber PA, Davis SM, Thijs V, Albers GW. Relationship between severity of MR perfusion deficit and DWI lesion evolution. Neurology. 2002;58:1707–1707.
Canals S, Larrosa B, Pintor J, Mena MA, Herreras O. Metabolic challenge to glia activates an adenosine-mediated safety mechanism that promotes neuronal survival by delaying the onset of spreading depression waves. J Cereb Blood Flow Metab. 2008;28:1835–44.
Magnussen I, Jakobsen P, Hoedt-Rasmussen K. Aminophylline and stroke. Acta Neurol Scan Suppl. 1977;64:168–9.
Dreier JP, Lemale CL, Kola V, Friedman A, Schoknecht K. Spreading depolarization is not an epiphenomenon but the principal mechanism of the cytotoxic edema in various gray matter structures of the brain during stroke. Neuropharmacology. 2018;134:189–207.
Fiehler J, Knudsen K, Kucinski T, Kidwell CS, Alger JR, Thomalla G, Eckert B, Wittkugel O, Weiller C, Zeumer H, Röther J. Predictors of apparent diffusion coefficient normalization in stroke patients. Stroke. 2004;35:514–9.
Funding
The study is funded by the Danish Regions (14/217), the Danish Heart Foundation (13-04-R94-A4619-22792, 14-R97-A5066-22829) and the Heart and Stroke Foundation of Canada (G-17-0018368).
Author information
Authors and Affiliations
Contributions
The study was conceived by BM. AW, BM and NF designed the study. Clinical data acquisition and management were performed by BM and NH. Image processing and analysis was performed by AW, BM, and NF. Data management and statistical analysis were performed by BM and MNJ. All authors contributed to the critical interpretation of the data. BM drafted the manuscript. All authors revised and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
B. Modrau, A. Winder, N. Hjort, M. Nygård Johansen, G. Andersen, J. Fiehler, H. Vorum and N.D. Forkert declare that they have no competing interests.
Ethical standards
This subgroup study is based on the theophylline in acute ischemic stroke trial (EudraCT number 2013-001989-42), approved by the Danish Health and Medicines Authorities (ref. no. 2013050908) and the Regional Scientific Ethic Committee (ref.-no. N‑20130034). Consent to participate: informed consent of all participants was given prior to their inclusion in the study. Consent for publication: informed consent of all participants was given prior to their inclusion in the study.
Additional information
Availability of Data and Material
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Code Availability
Not applicable.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Modrau, B., Winder, A., Hjort, N. et al. Perfusion Changes in Acute Stroke Treated with Theophylline as an Add-on to Thrombolysis. Clin Neuroradiol 32, 345–352 (2022). https://doi.org/10.1007/s00062-021-01029-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00062-021-01029-x