Abstract
Objective
This review aims to present an updated overview of cardiac disease-induced trauma and stress-related disorders such as acute stress disorder (ASD), adjustment disorder (AjD), and posttraumatic stress disorder (PTSD). First, the prevalence of these disorders, their diagnostic criteria, and their differences from other trauma-related disorders are described. Special challenges in diagnosis and treatment are identified, with various screening tools being evaluated for symptom assessment. Additionally, the risk factors studied so far for the development of symptoms of cardiac-induced posttraumatic stress disorder and the bidirectional relationship between posttraumatic stress disorder and cardiovascular diseases are summarized. Various therapeutic interventions, including pharmacological approaches, are also discussed. Finally, various areas for future research are outlined.
Background
Experiencing a cardiovascular disease, particularly a life-threatening cardiac event, can potentially lead to stress-related disorders such as ASD, AjD, and cardiac disease-induced PTSD (CDI-PTSD). If left untreated, these disorders are associated with a worsening cardiac prognosis and higher mortality rates. Approaching treatment through a trauma-focused lens may be beneficial for managing CDI-PTSD and stress-related disorders.
Conclusion
Future research should explore treatment options for both the patients and the caregivers as well as investigate the long-term effects of trauma-focused interventions on physical and mental health outcomes.
Zusammenfassung
Ziel der Arbeit
Ziel der vorliegenden Übersichtsarbeit ist es, einen aktuellen Überblick über traumatische Ereignisse und stressbedingte Störungen im Zusammenhang mit Herzerkrankungen zu geben, mit Fokus auf akuter Belastungsstörung, Anpassungsstörung und posttraumatischer Belastungsstörung. Zuerst wird die Häufigkeit dieser Störungen, ihre diagnostischen Kriterien sowie ihre Unterschiede zu anderen traumaassoziierten Störungen beschrieben. Besondere Herausforderungen in der Diagnose und Behandlung werden identifiziert, wobei verschiedene Screening-Tools zur Bewertung der Symptome evaluiert werden. Darüber hinaus werden die bisher untersuchten Risikofaktoren für die Entwicklung von Symptomen der kardial induzierten posttraumatischen Belastungsstörung und die bidirektionale Beziehung zwischen posttraumatischer Belastungsstörung und kardiovaskulären Erkrankungen zusammengefasst. Auch verschiedene therapeutische Interventionen, einschließlich pharmakologischer Ansätze, werden diskutiert. Abschließend werden verschiedene Bereiche für zukünftige Forschung skizziert.
Hintergrund
Das Erleben einer Herz-Kreislauf-Erkrankung, insbesondere eines lebensbedrohlichen kardialen Ereignisses, kann zu stressbedingten Störungen wie akuter Belastungsstörung, Anpassungsstörung und kardial induzierter posttraumatischer Belastungsstörung führen. Unbehandelt können diese Störungen den Verlauf und die Prognose der kardialen Erkrankung verschlechtern und zu höheren Sterberaten beitragen. Ein auf das Trauma fokussierter Behandlungsansatz könnte sich als nützlich erweisen, um stressbedingte Störungen zu bewältigen.
Schlussfolgerung
Zukünftige Studien sollten effektive und effiziente Behandlungsmöglichkeiten für Patienten und Behandler untersuchen und die langfristigen Folgen von Interventionen mit Fokus auf Traumata für die körperliche und psychische Gesundheit genauer evaluieren.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Cardiovascular diseases (CVD) and acute cardiac events such as acute coronary syndrome (ACS) continue to be the leading cause of morbidity and mortality worldwide [1]. Although hospitalization rates and mortality from CVD have declined in recent years due to improvements in medical care and the management of risk factors, demographic shifts have resulted in a rise in the incidence of CVD, presenting substantial medical and economic challenges for the healthcare system [2].
A sudden acute cardiac event carries an imminent risk of death and can evoke feelings of anxiety, loss of control, and helplessness, which can potentially be traumatic [3]. Patients suffering from these symptoms may qualify for a formal diagnosis of acute stress disorder (ASD) occurring within 1 month of the cardiac event. Generally, an episode of ASD fades quickly, most often without need for treatment. However, in a substantial number of cases, adjustment disorder (AjD) and/or cardiac disease induced (CDI-) posttraumatic stress disorder (CDI-PTSD) may occur.
Cardiac disease induced-induced PTSD is defined by the presence of multiple clusters of psychological, behavioral, and physiological symptoms, including intrusive thoughts (intrusions), avoidance, negative changes in cognition and mood, as well as increased arousal and stress reactivity [4]. Trauma-related disorders caused by cardiac diseases not only significantly impair quality of life [5] but are also associated with an increased risk of another cardiac event and increased mortality in the first 3 years following the initial event [6].
Prevalence rates
A significant proportion of CVD patients have stress-related disorders. Table 1 gives an overview of prevalence rates for the three disorders (ASD, AjD, and PTSD). Notably, prevalence rates vary widely across different CVD events [7].
Diagnostic criteria
Table 2 provides an overview of the symptoms for ASD, AjD, and PTSD based on the tenth revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10; [4]).
Differences from other trauma-related disorders
Post-traumatic stress disorder (PTSD) induced by a medical event can exhibit several pertinent differences from other trauma-related disorders [17]:
-
1.
Source of threat: Cardiac trauma-related disorders stem from internal threats originating from within one’s own body, such as heart-related events, unlike traditional trauma that typically involves external causes like accidents, assaults, or disasters.
-
2.
Nature of intrusive symptoms: Intrusive symptoms in cardiac trauma-related disorders can manifest as present or future-oriented intrusions, often referred to as “flashforward intrusions.” These typically revolve around fears of experiencing another cardiac event or concerns about mortality due to heart-related issues. By contrast, traditional trauma-related disorders may involve intrusions related to the traumatic event itself, typically in the form of flashback intrusions.
-
3.
Avoidance behaviors: Patients with cardiac trauma-related disorders may exhibit avoidance behaviors toward health-promoting activities like physical exercise, medical appointments, or medication adherence due to fear of exacerbating their condition. This avoidance may result in heightened anxiety and guilt. In traditional trauma-related disorders, avoidance behaviors may be more focused on avoiding reminders or triggers of the traumatic event.
-
4.
Interpretation of physical symptoms: Individuals with cardiac trauma-related disorders may misinterpret physical sensations such as increased heart rate or shortness of breath as signs of impending cardiac issues, leading to heightened anxiety and hyperarousal. This contrasts with traditional trauma-related disorders where physical symptoms may be more directly associated with triggers or reminders of the traumatic event.
Challenges in diagnosis and treatment
Distinguishing between physical symptoms of cardiac trauma-related disorders and symptoms of actual heart disease can be challenging for both the patients and the clinicians, potentially leading to prolonged anxiety and difficulty in initiating appropriate treatment. Tailored interventions that address the unique challenges of cardiac trauma-related disorders may be necessary for effective management. These differences highlight the distinct nature of trauma-related disorders stemming from cardiac events compared to those arising from traditional traumatic experiences, necessitating specialized approaches in diagnosis and treatment [18].
Screening tools
ICD-11 and the “Adjustment Disorder–New Module”
The diagnosis of AjD typically depends on the clinical judgment of a professional, as there is no established gold standard for standardized assessment. The new ICD-11 diagnostic criteria for AjD support a uni-faceted approach with core symptoms and additional features, resulting in a clearer diagnostic concept [19]. Central symptoms include preoccupation with the stressor and an inability to adapt. Signs of preoccupation encompass recurrence, distressing thoughts, or persistent rumination about the stressful event. Failure-to-adapt symptoms may manifest as sleep disturbances or difficulties in concentration. In accordance with this revised understanding of AjD, a self-reported assessment tool called the “Adjustment Disorder–New Module” (ADNM) was validated. So far, only a few studies have used the new ICD-11 criteria for AjD in cardiac patients, concluding that the new questionnaire is effective and recommending it for use in future studies [20, 21].
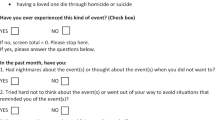
Primary Care PTSD Checklist
Screening for and diagnosing PTSD in cardiac patients can be challenging due to the unique symptomatology, such as intrusive thoughts about future cardiac events. Presently, there is no dedicated diagnostic tool designed for evaluating CDI-induced PTSD symptoms. International and scientific clinical guidelines advocate for the screening of all cardiac patients for psychological distress following such an event [22]. Early recognition and intervention can significantly improve outcomes for these patients [22]. The Primary Care PTSD Checklist (PC-PTSD) can be used to screen for PTSD in cardiac patients [23]. The PC-PTSD‑5 is effectual in identifying potential PTSD symptoms on an individual basis. The questions about the individual symptoms of PTSD should refer to the cardiac event as the traumatic experience. Patients who test positive on the screening require further assessment, ideally conducted through structured interviews.
Risk factors for the development of CDI-PTSD
Numerous studies indicate that risk factors for CDI-PTSD following a cardiac event encompass various domains. These include sociodemographic factors (such as female gender, younger age, and potentially ethnic minority status and low education), psychological characteristics (including prior psychological issues, high intrusion symptoms, and severity of ASD and depression symptoms), and aspects related to the cardiac event itself (such as perception of life threat, history of referral to a psychologist, and the context of care during the event; [24, 25]). Of particular importance is an individual’s perception of illness following a cardiac event, which consistently influences the development of CDI-PTSD symptoms [26]. Specifically, intense pain, fear, and helplessness in response to the ACS significantly heighten the likelihood of PTSD development [27]. Contradictory results have been reported with the use of benzodiazepines, as sedation in the initial phase of resuscitation reduced the risk of developing PTSD [28]. However, patients with an ACS and benzodiazepines had an increased risk of PTSD [29]. Additional risk factors for the development of these symptoms include environmental and treatment-related factors (e.g., chaotic hospital admissions, treatment complications, staff statements; [29]), personality traits (Type D, neuroticism, hostility, alexithymia; [11]), and a patient’s biopsychosocial history (stressful life events, prior heart disease, other somatic conditions; [30]). Cardiac patients treated during emergency department overcrowding, hallway care, and perceived inadequate clinician–patient communication also appear to be at greater risk for subsequent PTSD [31]. Interestingly, objective indicators of cardiac injury, such as troponin T levels in ACS, show little correlation with subsequent PTSD symptoms [27]. Conversely, social support and resilience factors (such as internal control beliefs, humor, patience, and repressive coping strategies immediately after the traumatic event) have been shown to have a protective effect against the development of CDI-PTSD symptoms [24].
The bidirectional association between PTSD and CVD
The bidirectional association between PTSD and CDI-PTSD has long been linked to an increased risk of CVD, although the precise reciprocal relationship between PTSD and CVD remains not fully understood [32]. Several physiological mechanisms have been investigated to elucidate the link between PTSD and CVD, including autonomic dysfunction, disruptions in neuroendocrine regulation, and inflammatory processes (for details, refer to [33]). Various neurobiological underpinnings may be involved, consistent with the conceptualization of PTSD as a disorder characterized by altered formation and/or extinction of emotional memories, along with dysregulated responses to threat and stress [34]. These encompass alterations in the functioning and connectivity of specific brain regions crucial for emotional processing and cognition, notably the amygdala, insula, dorsal anterior cingulate, and ventromedial prefrontal cortex [34].
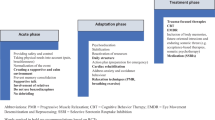
Therapeutic interventions
Preventing cardiac-induced stress-related disorders involves addressing both the physical and psychological aspects of cardiac events. Since not all cardiac events can be prevented, it is important to note that several strategies can help reduce the risk and mitigate the impact of traumatic experiences related to these events. Given that the personal experience of stress and discomfort is more important than the severity of the cardiac condition [7], establishing a sense of safety and control is essential.
An immediate one-time trauma-specific counseling shows no beneficial long-term effect on preventing posttraumatic stress compared with one session of general stress counseling [35, 36]. However, trauma-specific counseling was more effective in patients who perceived an increased level of social support [37]. After a cardiac event, there are several starting points for preventive interventions based on the aforementioned risk factors. Providing patients and their families with information and education about cardiac conditions, treatment options, and coping strategies could help reduce anxiety, fear, and distress. A multidisciplinary approach has been emphasized to support ICD patients with shock experience and provide detailed and practice-friendly psychoeducation [38]. Furthermore, web-based cognitive behavioral therapy (CBT) has been recommended as a low-threshold alternative to in-person treatments for centers lacking comprehensive cardiac psychology services.
This goes in line with therapeutic options for AjD. Interventions usually aim at three factors: (a) elimination or mitigation of stress (e.g., treatment of underlying CVD); (b) improvement of coping and adaptation (e.g., taking up activities); and (c) symptom reduction and behavioral change (e.g., CBT for anxiety/depression; [39]). As AjD is by definition transient, the authors propose a stepped approach with level 1 watchful waiting, which could be accomplished during cardiac rehabilitation. Level 2 consists of low-intensity psychological interventions such as web-based programs. For those patients who do not benefit sufficiently, level 3 recommends individual psycho- and/or pharmacotherapy. Level 4 includes inpatient treatment for people with severe AjD with, for instance, suicidal tendencies [39]. A recent review and meta-analysis reported web-based interventions for AjD areas to be effective [40]. One example is the Internet-based modular program Brief Adjustment Disorder Intervention (BADI) for ICD-11-AjD [41]. The BADI is a CBT-based program and consists of four modules: relaxation, time management, mindfulness, and strengthening relationships. It showed promising effects on AjD when used at least once in 30 days [42]. Therapeutic support did not enhance its effectiveness [43]. Participation in cardiac rehabilitation following a cardiac event can help individuals recover physically and emotionally. These programs typically encompass supervised exercise training, educational sessions promoting heart-healthy lifestyle modifications, and counseling or support groups to address psychological concerns. However, individuals with PTSD or AjD exhibit reduced participation in physical activity and tend to avoid their physical limits [21, 44]. As the occurrence of somatic symptoms such as chest tightness or heartbeat symptoms can increase post-traumatic stress [45], this could culminate in a self-perpetuating cycle of avoidance with mutually reinforcing factors. Exercise, however, has a beneficial effect on PTSD, whether used alone or as a complement to conventional therapy [46].
Despite the undeniable indication for therapeutic intervention, a study reported only 30–40% of patients with diagnosed CDI-PTSD received some form of treatment, whether medication or counseling [47]. Trauma-focused psychotherapy is more beneficial than non-trauma-focused therapies in reducing PTSD severity [48]. Meta-analyses have demonstrated encouraging findings regarding the efficacy and long-term impact of exposure-based therapies such as prolonged exposure (PE), trauma-focused CBT, cognitive therapy (CT), and eye movement desensitization and reprocessing (EMDR; [49]) as well as narrative exposure therapy (NET; [50]). Imaginal exposure therapy (IET) proved safe, as evidenced by the absence of significant changes in blood pressure and heart rate during exposures [51]. Promising approaches extend beyond traditional psychotherapeutic interventions. Innovative therapies such as biofeedback may serve as a variation of exposure therapy [52].
Pharmacotherapy
In addition to psychotherapy, psychotropic drugs are another option for treatment of severe PTSD. Selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRIs) are the drugs of choice [53]. Of the SSRI group, sertraline and citalopram seem safe for patients with CVD [54]. Tricyclics should be avoided in patients with CVD [15]. Furthermore, clinicians should monitor possible cardiometabolic side effects (e.g., weight gain) and discuss the risks and benefits of the medication with patients before and throughout the treatment [53]. Benzodiazepines exhibit a short-term anxiolytic effect, yet they increase the risk of developing PTSD symptoms after an ACS, making it advisable to use them with caution [29]. An important contraindication arises concerning patients with heart failure, as antidepressants have been associated with an increased risk of all-cause mortality [55]. Antidepressants, i.e., SSRIs, should therefore be avoided in favor of psychotherapy [56]. There is only limited research on pharmacotherapy for AjD, but studies suggest caution against the use of benzodiazepines [57].
Future research
Future research should aim to better identify early signs of CDI-induced distress with screening for ASD, especially in patients with a history of mental illness, as they seem most vulnerable to additional stress [58]. Clinician–patient communication is a critical factor that can influence the development of PTSD symptoms [59]. As the perception of a hectic hospital environment and crowded emergency department are associated with an increased risk for ASD and PTSD and can lead to a higher re-admission rate [60, 61], interventions should go beyond individual care and address structural factors, too. Future research on effective interventions for ASD should aim to help patients with cardiac disease mitigate their distress and perceived threat while concurrently preventing the emergence of long-term cardiac trauma and stress-related disorders such as AjD and PTSD. Not all patients benefit from the same intervention [37].
Further research is needed to identify specific risk factors, enabling more personalized interventions that effectively target the most vulnerable patients and those who benefit the most. A promising differentiation has been offered in a recent study of ACS patients that identified three clusters associated with posttraumatic stress and depression [62]: (a) low-risk cluster with the highest resilience, task-oriented coping, positive affect, and social support; (b) a lonely cluster with the lowest social support and resilience; and (c) avoidant cluster with the lowest task-oriented coping and positive affect. Future research is needed to assess whether addressing these factors may yield protective benefits. Research on early intervention after a traumatically experienced medical event to prevent PTSD is promising, albeit preliminary and limited [63], but is even more sparse regarding AjD. One barrier is the unclear defined criteria and the lack of assessment methods for AjD [64]. The ICD-11 introduced a major change in the definition of AjD with two core symptoms: preoccupation and failure to adapt [65]. Increasing evidence supports the concept [66] and the assessment tool (ADNM; [19]). With the establishment of standardized criteria and assessment tools, future studies can more reliably assess the efficacy of preventive and early intervention programs for AjD.
Conclusion
The development of targeted interventions for the unique challenges posed by trauma-related disorders in the context of cardiac events, including adjustment disorder and cardiac disease-induced posttraumatic stress disorder, is crucial. These interventions should aim to address the specific symptomatology, risk factors, and barriers to treatment engagement associated with cardiac trauma-related disorders, thus improving patient outcomes and quality of life. The integration of psychological support into standard cardiac care pathways, such as cardiac rehabilitation programs, may help ensure that patients receive timely and appropriate interventions to address their psychological needs alongside their physical recovery.
References
Ahmad FB, Anderson RN (2021) The leading causes of death in the US for 2020. JAMA 325(18):1829–1830. https://doi.org/10.1001/jama.2021.5469
Kumar A, Siddharth V, Singh SI, Narang R (2022) Cost analysis of treating cardiovascular diseases in a super-specialty hospital. PLoS ONE 17(1):e262190. https://doi.org/10.1371/journal.pone.0262190
Wu M, Wang W, Zhang X, Li J (2022) The prevalence of acute stress disorder after acute myocardial infarction and its psychosocial risk factors among young and middle-aged patients. Sci Rep 12(1):7675. https://doi.org/10.1038/s41598-022-11855-9
World Health Organization (2016) International statistical classification of diseases and related health problems, 10th edn. World Health Organization, Geneva, Switzerland
Lui JNM, Williams C, Keng MJ et al (2023) Impact of new cardiovascular events on quality of life and hospital costs in people with cardiovascular disease in the united kingdom and United States. JAHA 12(19):e30766. https://doi.org/10.1161/JAHA.123.030766
Agarwal S, Presciutti A, Cornelius T et al (2019) Cardiac arrest and subsequent hospitalization-induced posttraumatic stress is associated with 1‑year risk of major adverse cardiovascular events and all-cause mortality. Crit Care Med 47(6):e502–e505. https://doi.org/10.1097/CCM.0000000000003713
Vilchinsky N, Ginzburg K, Fait K, Foa EB (2017) Cardiac-disease-induced PTSD (CDI-PTSD): a systematic review. Clin Psychol Rev 55:92–106. https://doi.org/10.1016/j.cpr.2017.04.009
Sumner JA, Kronish IM, Chang BP et al (2017) Acute stress disorder symptoms after evaluation for acute coronary syndrome predict 30-day readmission. Int J Cardiol 240:87–89. https://doi.org/10.1016/j.ijcard.2017.03.102
Ginzburg K, Kutz I, Koifman B et al (2016) Acute stress disorder symptoms predict all-cause mortality among myocardial infarction patients: a 15-year longitudinal study. Ann Behav Med 50(2):177–186. https://doi.org/10.1007/s12160-015-9744-x
Armand S, Wagner MK, Ozenne B et al (2022) Acute Traumatic Stress Screening Can Identify Patients and Their Partners at Risk for Posttraumatic Stress Disorder Symptoms After a Cardiac Arrest: A Multicenter Prospective Cohort Study. J Cardiovasc Nurs 37(4):394–401. https://doi.org/10.1097/JCN.0000000000000829
Ledermann K, von Känel R, Barth J et al (2020) Myocardial infarction-induced acute stress and post-traumatic stress symptoms: the moderating role of an alexithymia trait—difficulties identifying feelings. Eur J Psychotraumatol 11(1):1804119. https://doi.org/10.1080/20008198.2020.1804119
Dew MA, Kormos RL, DiMartini AF et al (2001) Prevalence and risk of depression and anxiety-related disorders during the first three years after heart transplantation. Psychosomatics 42(4):300–313. https://doi.org/10.1176/appi.psy.42.4.300
Latal B, Helfricht S, Fischer JE et al (2009) Psychological adjustment and quality of life in children and adolescents following open-heart surgery for congenital heart disease: a systematic review. BMC Pediatr 9:6. https://doi.org/10.1186/1471-2431-9-6
Rea KE, McCormick AM, Lim HM, Cousino MK (2021) Psychosocial outcomes in pediatric patients with ventricular assist devices and their families: a systematic review. Pediatr Transplant 25(4):e14001. https://doi.org/10.1111/petr.14001
Princip M, Ledermann K, von Känel R (2023) Posttraumatic stress disorder as a consequence of acute cardiovascular disease. Curr Cardiol Rep 25(6):455–465. https://doi.org/10.1007/s11886-023-01870-1
Meentken MG, van Beynum IM, Legerstee JS et al (2017) Medically related post-traumatic stress in children and adolescents with congenital heart defects. Front Pediatr 5:20. https://doi.org/10.3389/fped.2017.00020
Edmondson D (2014) An enduring somatic threat model of posttraumatic stress disorder due to acute life-threatening medical events. Soc Personal Psychol Compass 8(3):118–134. https://doi.org/10.1111/spc3.12089
Mundy E, Baum A (2004) Medical disorders as a cause of psychological trauma and posttraumatic stress disorder. Curr Opin Psychiatry 17(2):123–127. https://doi.org/10.1097/00001504-200403000-00009
Glaesmer H, Romppel M, Brähler E et al (2015) Adjustment disorder as proposed for ICD-11: Dimensionality and symptom differentiation. Psychiatry Res 229(3):940–948. https://doi.org/10.1016/j.psychres.2015.07.010
Maercker A, Einsle F, Kollner V (2007) Adjustment disorders as stress response syndromes: a new diagnostic concept and its exploration in a medical sample. Psychopathology 40(3):135–146. https://doi.org/10.1159/000099290
Bermudez T, Maercker A, Bierbauer W et al (2023) The role of daily adjustment disorder, depression and anxiety symptoms for the physical activity of cardiac patients. Psychol Med 53(13):5992–6001. https://doi.org/10.1017/S0033291722003154
Douma MJ, Graham TAD, Ali S et al (2021) What are the care needs of families experiencing cardiac arrest?: a survivor and family led scoping review. Resuscitation 168:119–141. https://doi.org/10.1016/j.resuscitation.2021.09.019
Prins A, Bovin MJ, Smolenski DJ et al (2016) The primary care PTSD screen for DSM‑5 (PC-PTSD-5): development and evaluation within a veteran primary care sample. J Gen Intern Med 31(10):1206–1211. https://doi.org/10.1007/s11606-016-3703-5
Edmondson D, Kronish IM, Shaffer JA et al (2013) Posttraumatic stress disorder and risk for coronary heart disease: a meta-analytic review. Am Heart J 166(5):806–814. https://doi.org/10.1016/j.ahj.2013.07.031
Roberge MA, Dupuis G, Marchand A (2010) Post-traumatic stress disorder following myocardial infarction: prevalence and risk factors. Can J Cardiol 26(5):e170–e175. https://doi.org/10.1016/s0828-282x(10)70386-x
Princip M, Gattlen C, Meister-Langraf RE et al (2018) The role of illness perception and its association with posttraumatic stress at 3 months following acute myocardial infarction. Front Psychol 9:941. https://doi.org/10.3389/fpsyg.2018.00941
Guler E, Schmid JP, Wiedemar L et al (2009) Clinical diagnosis of posttraumatic stress disorder after myocardial infarction. Clin Cardiol 32(3):125–129. https://doi.org/10.1002/clc.20384
Ladwig KH, Schoefinius A, Dammann G et al (1999) Long-acting psychotraumatic properties of a cardiac arrest experience. Am J Psychiatry 156(6):912–919. https://doi.org/10.1176/ajp.156.6.912
von Känel R, Schmid JP, Meister-Langraf RE et al (2021) Pharmacotherapy in the management of anxiety and pain during acute coronary syndromes and the risk of developing symptoms of posttraumatic stress disorder. J Am Heart Assoc 10(2):e18762–19. https://doi.org/10.1161/JAHA.120.018762
Kronish IM, Edmondson D, Moise N et al (2018) Posttraumatic stress disorder in patients who rule out versus rule in for acute coronary syndrome. Gen Hosp Psychiatry 53:101–107. https://doi.org/10.1016/j.genhosppsych.2018.02.007
Musey PI Jr, Schultebraucks K, Chang BP (2020) Stressing out about the heart: a narrative review of the role of psychological stress in acute cardiovascular events. Acad Emerg Med 27(1):71–79. https://doi.org/10.1111/acem.13882
Maddox SA, Hartmann J, Ross RA, Ressler KJ (2019) Deconstructing the gestalt: mechanisms of fear, threat, and trauma memory encoding. Neuron 102(1):60–74. https://doi.org/10.1016/j.neuron.2019.03.017
Seligowski AV, Webber TK, Marvar PJ et al (2022) Involvement of the brain-heart axis in the link between PTSD and cardiovascular disease. Depress Anxiety 39(10):663–674. https://doi.org/10.1002/da.23271
Wilson MA, Liberzon I, Lindsey ML et al (2019) Common pathways and communication between the brain and heart: connecting post-traumatic stress disorder and heart failure. Stress 22(5):530–547. https://doi.org/10.1080/10253890.2019.1621283
von Känel R, Barth J, Princip M et al (2018) Early psychological counseling for the prevention of posttraumatic stress induced by acute coronary syndrome: the MI-SPRINT randomized controlled trial. Psychother Psychosom 87(2):75–84. https://doi.org/10.1159/000486099
von Känel R, Meister-Langraf RE, Barth J et al (2021) Course, moderators, and predictors of acute coronary syndrome-induced post-traumatic stress: a secondary analysis from the myocardial infarction-stress prevention intervention randomized controlled trial. Front Psychiatry 12:621284. https://doi.org/10.3389/fpsyt.2021.621284
von Känel R, Meister-Langraf RE, Barth J et al (2022) Early trauma-focused counseling for the prevention of acute coronary syndrome-induced posttraumatic stress: social and health care resources matter. J Clin Med 11(7):1993. https://doi.org/10.3390/jcm11071993
Sears SF, Harrell R, Sorrell A et al (2023) Addressing PTSD in implantable cardioverter defibrillator patients: state-of-the-art management of ICD shock and PTSD. Curr Cardiol Rep 25:1029–1039. https://doi.org/10.1007/s11886-023-01924-4
Baumeister H, Bachem R, Domhardt M (2022) Therapy of the adjustment disorder. In: Maercker A (ed) Trauma Sequelae. Springer, Berlin, Heidelberg https://doi.org/10.1007/978-3-662-64057-9_21
Fernández-Buendía S, Miguel C, Dumarkaite A et al (2024) Technology-supported treatments for adjustment disorder: a systematic review and preliminary meta-analysis. J Affect Disord 347:29–38. https://doi.org/10.1016/j.jad.2023.11.059
Skruibis P, Eimontas J, Dovydaitiene M et al (2016) Internet-based modular program BADI for adjustment disorder: protocol of a ran-domized controlled trial. Bmc Psychiatry 16:264. https://doi.org/10.1186/s12888-016-0980-9
Eimontas J, Rimsaite Z, Gegieckaite G et al (2018) Internet-based self-help intervention for ICD-11 adjustment disorder: preliminary findings. Psychiatr Q 89(2):451–460. https://doi.org/10.1007/s11126-017-9547-2
Eimontas J, Gegieckaite G, Dovydaitiene M et al (2018) The role of therapist support on effectiveness of an internet-based modular self-help intervention for adjustment disorder: a randomized controlled trial. Anxiety Stress Coping 31(2):146–158. https://doi.org/10.1080/10615806.2017.1385065
Sopek Merkaš I, Lakušić N, Sonicki Z et al (2023) Prevalence of posttraumatic stress disorder following acute coronary syndrome and clinical characteristics of patients referred to cardiac rehabilitation. World J Psychiatry 13(6):376–385. https://doi.org/10.5498/wjp.v13.i6.376
von Känel R, Meister-Langraf RE, Zuccarella-Hackl C et al (2022) Association between changes in post-hospital cardiac symptoms and changes in acute coronary syndrome-induced symptoms of post-traumatic stress. Front Cardiovasc Med 9:852710. https://doi.org/10.3389/fcvm.2022.852710
Hegberg NJ, Hayes JP, Hayes SM (2019) Exercise intervention in PTSD: a narrative review and rationale for implementation. Front Psychiatry 10:133. https://doi.org/10.3389/fpsyt.2019.00133
Sundquist K, Chang BP, Parsons F et al (2016) Treatment rates for PTSD and depression in recently hospitalized cardiac patients. J Psychosom Res 86:60–62. https://doi.org/10.1016/j.jpsychores.2016.05.007
Bisson JI, Roberts NP, Andrew M et al (2013) Psychological ther-apies for chronic post-traumatic stress disorder (PTSD) in adults. Cochrane Database Syst Rev 2013(12):CD3388. https://doi.org/10.1002/14651858.CD003388.pub4
Kline AC, Cooper AA, Rytwinksi NK, Feeny NC (2018) Long-term efficacy of psychotherapy for posttraumatic stress disorder: a meta-analysis of randomized controlled trials. Clin Psychol Rev 59:30–40. https://doi.org/10.1016/j.cpr.2017.10.009
Cusack K, Jonas DE, Forneris CA et al (2016) Psycho-logical treatments for adults with posttraumatic stress disorder: a systematic review and meta-analysis. Clin Psychol Rev 43:128–141. https://doi.org/10.1016/j.cpr.2015.10.003
Shemesh E, Annunziato RA, Weatherley BD et al (2011) A randomized controlled trial of the safety and promise of cognitive-behavioral therapy using imaginal exposure in patients with posttraumatic stress disorder resulting from cardiovascular illness. J Clin Psychia-try 72(2):168–174. https://doi.org/10.4088/JCP.09m05116blu
Meli L, Birk J, Edmondson D, Bonanno GA (2020) Trajectories of posttraumatic stress in patients with confirmed and rule-out acute coronary syndrome. Gen Hosp Psychiatry 62:37–42. https://doi.org/10.1016/j.genhosppsych.2019.11.006
Hargrave AS, Sumner JA, Ebrahimi R, Cohen BE (2022) Posttraumatic stress disorder (PTSD) as a risk factor for cardiovascular disease: implications for future research and clinical care. Curr Cardiol Rep 24(12):2067–2079. https://doi.org/10.1007/s11886-022-01809-y
Lespérance F, Frasure-Smith N, Koszycki D et al (2007) Effects of citalopram and interpersonal psychotherapy on depression in patients with coronary artery disease: the Canadian cardiac randomized evaluation of antidepressant and psychotherapy efficacy (CREATE) trial. JAMA 297(4):367–379. https://doi.org/10.1001/jama.297.4.367
He W, Zhou Y, Ma J et al (2020) Effect of antidepressants on death in patients with heart failure: a systematic review and meta-analysis. Heart Fail Rev 25(6):919–926. https://doi.org/10.1007/s10741-019-09850-w
Ladwig KH, Baghai TC, Doyle F et al (2022) Mental health-related risk factors and interventions in patients with heart failure: a position paper endorsed by the European Association of Preventive Cardiology (EAPC). Eur J Prev Cardiol 29(7):1124–1141. https://doi.org/10.1093/eurjpc/zwac006
Hoffman J, Stein DJ (2022) What are the pharmacotherapeutic options for adjustment disorder? Expert Opin Pharmacother 23(6):643–646. https://doi.org/10.1080/14656566.2022.2033209
Edmondson D, Kronish IM, Wasson LT et al (2014) A test of the diathesis-stress model in the emergency department: who develops PTSD after an acute coronary syndrome? J Psychiatr Res 53:8–13. https://doi.org/10.1016/j.jpsychires.2014.02.009
Chang BP, Sumner JA, Haerizadeh M et al (2016) Perceived clinician-patient communication in the emergency department and subsequent post-traumatic stress symptoms in patients evaluated for acute coronary syndrome. Emerg Med J 33(9):626–631. https://doi.org/10.1136/emermed-2015-205473
Meister RE, Weber T, Princip M et al (2016) Perception of a hectic hospital environment at admission relates to acute stress disorder symptoms in myocardial infarction patients. Gen Hosp Psychiatry 39:8–14. https://doi.org/10.1016/j.genhosppsych.2015.11.004
Edmondson D, Shimbo D, Ye S et al (2013b) The association of emergency department crowding during treatment for acute coronary syndrome with subse-quent posttraumatic stress disorder symptoms. JAMA Intern Med 173(6):472–474. https://doi.org/10.1001/jamainternmed.2013.2536
Zuccarella-Hackl C, Jimenez-Gonzalo L, von Känel R et al (2023) Positive psychosocial factors and the development of symptoms of depression and post-traumatic stress symptoms following acute myocardial infarction. Front Psychol 14:1302699. https://doi.org/10.3389/fpsyg.2023.1302699
Birk JL, Sumner JA, Haerizadeh M et al (2019) Early interventions to prevent posttraumatic stress disorder symptoms in survivors of life-threatening medical events: a systematic review. J Anxiety Disord 64:24–39. https://doi.org/10.1016/j.janxdis.2019.03.003
Bachem R, Casey P (2018) Adjustment disorder: a diagnosis whose time has come. J Affect Disord 227:243–253. https://doi.org/10.1016/j.jad.2017.10.034
(2022) International classification of diseases eleventh revision (ICD-11). Geneva: World Health Organization. https://icd.who.int/browse/2024-01/mms/en
O’Donnell ML, Agathos JA, Metcalf O et al (2019) Adjustment Disorder: Current Developments and Future Directions. Int J Environ-mental Res Public Health 16(14):2537. https://doi.org/10.3390/ijerph16142537
Funding
Open access funding provided by University of Zurich
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M. Princip, K. Ledermann, R. Altwegg and R. von Känel declare that they have no competing interests.
For this article no studies with human participants or animals were performed by any of the authors. All studies mentioned were in accordance with the ethical standards indicated in each case.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Princip, M., Ledermann, K., Altwegg, R. et al. Cardiac disease-induced trauma and stress-related disorders. Herz 49, 254–260 (2024). https://doi.org/10.1007/s00059-024-05255-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-024-05255-0
Keywords
- Acute stress disorder
- Adjustment disorder
- Posttraumatic stress disorder
- Cardiovascular disease
- Cardiac-induced posttraumatic stress disorder