Abstract
The diagnosis and therapy of heart failure with preserved ejection fraction (HFpEF) remain challenging. Currently, there are ongoing discussions on whether the diagnosis of HFpEF should be based solely on left ventricular ejection fraction, which may not account for the heterogeneity of HFpEF syndrome. This aspect has been addressed by the recently proposed HFA-PEFF and the H2FPEF algorithms, which take numerous diagnostic modalities into account to establish the diagnosis of HFpEF. Moreover, this review focuses on the adequate treatment of comorbidities and risk factors in HFpEF that should be an essential part of any HFpEF therapy. Furthermore, the management of fluid level in HFpEF patients is pointed out, as it plays an important role in symptom control. In addition, the value of LCZ696 therapy in HFpEF is discussed. Although LCZ696 had neutral effects in the large PARAGON-HF trial, it had previously been granted an extended indication by the Food and Drug Administration. Since the publication of the EMPEROR-Preserved trial, empagliflozin now represents the first drug to significantly improve the prognosis of HFpEF patients. Therefore, the role of SGLT2 inhibitors in HFpEF management is highlighted. Overall, this review aims to enhance the knowledge on the diagnostic processes and best treatments available for HFpEF patients.
Zusammenfassung
Bis heute stellen Diagnose und Therapie der Herzinsuffizienz mit erhaltener linksventrikulärer Ejektionsfraktion (HFpEF) eine Herausforderung dar. Aufgrund der Heterogenität des HFpEF-Syndroms wird aktuell zunehmend kritisch darüber diskutiert, ob die Diagnose ausschließlich auf der linksventrikulären Ejektionsfraktion beruhen sollte. Dieser Aspekt wurde durch die kürzlich vorgeschlagenen HFA-PEFF- und H2FPEF-Diagnosealgorithmen aufgegriffen, die verschiedene Untersuchungsverfahren bei der HFpEF-Diagnose berücksichtigen. Darüber hinaus konzentriert sich diese Übersicht auf die adäquate Behandlung von Komorbiditäten und Risikofaktoren bei Patienten mit HFpEF, die eine Grundlage jeder HFpEF-Therapie darstellen sollte. Außerdem wird auf das Management des Volumenhaushalts bei HFpEF-Patienten eingegangen, durch das Symptome reduziert werden können. Zudem wird der Wert der LCZ696-Therapie bei HFpEF diskutiert. Obwohl LCZ696 in der großen PARAGON-HF-Studie nur einen neutralen Effekt aufwies, wurde die Zulassung in den USA erst kürzlich von der Food and Drug Administration (FDA) angepasst und erweitert. Seit der Veröffentlichung der EMPEROR-Preserved-Studie ist Empagliflozin nun das erste Medikament, das die Prognose bei HFpEF-Patienten nachweislich signifikant verbessert. Daher wird die Rolle der SGLT2-Hemmer bei der Behandlung von Patienten mit HFpEF genauer beschrieben. Das Ziel dieser Übersicht besteht darin, Kenntnisse über eine optimale Diagnostik sowie eine bestmögliche Therapie für HFpEF-Patienten zu vermitteln.
Similar content being viewed by others
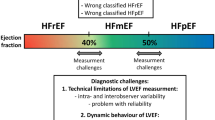
According to the 2021 European Society of Cardiology (ESC) guidelines [1], heart failure (HF) should be differentiated into three different forms depending on left ventricular ejection fraction (LVEF): heart failure with preserved ejection fraction (HFpEF, LVEF ≥ 50%), heart failure with reduced ejection fraction (HFrEF, LVEF ≤ 40%), and heart failure with mildly reduced ejection fraction (HFmrEF, LVEF 41–49%). Despite the latest breakthroughs in medical treatment, the diagnosis, as well as the therapy of the syndrome HFpEF, remains challenging. This review focuses on patient management strategies in HFpEF to accelerate and to enhance the diagnostic process and to provide the patients with the best treatment possible.
The heterogeneity of heart failure with preserved ejection fraction
As pointed out by the 2021 ESC guidelines [1], the potential causes of HFpEF are numerous. Typically, patients suffering from HFpEF are older and more often female compared with patients who have HFrEF and HFmrEF [2, 3]. Moreover, HFpEF patients commonly exhibit various comorbidities and cardiovascular risk factors such as chronic kidney disease, diabetes, hypertension, obesity, and deconditioning [4]. Furthermore, specific diseases may result in HFpEF. These comprise, for instance, primary cardiomyopathies, storage diseases such as Fabry’s disease and amyloidosis, or pericardial diseases such as constrictive pericarditis. Thus, rather than a single clinical diagnosis, the term “HFpEF” describes a clinical syndrome with different underlying etiologies that require distinct therapies [5]. As a result, there are ongoing discussions on whether the definition of HFpEF should be based solely on LVEF [6]. To address this issue, two algorithms have been proposed recently—H2FPEF [7] and HFA-PEFF [8]—that consider numerous findings (noninvasive as well as invasive) besides LVEF to establish the diagnosis of HFpEF.
Diagnosis of HFpEF
Introduced by the Heart Failure Association (HFA) of the ESC, the HFA-PEFF score suggests a step-wise diagnostic approach to standardize and enhance the diagnosis of HFpEF [8]. The first step (P =pre-test assessment) can be performed in the ambulatory setting and takes into account clinical characteristics (HF symptoms and signs, prevalence of comorbidities) as well as standard diagnostic tests including natriuretic peptides, electrocardiogram, X‑ray, and echocardiography. If positive, the authors recommend a risk stratification by natriuretic peptide levels and sophisticated echocardiographic work-up into three different groups: low, intermediate, and high risk (step E). While the diagnosis of HFpEF is confirmed in patients at high risk and is excluded in patients at low risk, patients at intermediate risk should undergo echo stress tests or, if those are inconclusive, invasive hemodynamic measurements in step 3 (F1). Lastly, in all patients confirmed with HFpEF, an etiological work-up should be pursued aimed at identifying specific causes of HFpEF (step F2). However, as acknowledged by the ESC guidelines, the broad application of this score is limited since some of the proposed tests can only be performed in specialized centers [1]. Therefore, the guidelines suggest a simplified algorithm for physicians with no access to this kind of expertise. In accordance with the HFA-PEFF algorithm, the first step of the simplified approach is to determine the pre-test probability according to the following three points: (1) symptoms and signs of HF, (2) LVEF ≥ 50%, and (3) objective evidence indicating the presence of LV diastolic dysfunction or raised LV filling pressures (summarized in Table 1; [1]). In the case of diagnostic uncertainty, a diastolic stress test is recommended. Although invasive hemodynamic exercise testing remains the confirmatory test for the diagnosis of HFpEF, its routine performance is not encouraged by the guidelines, in particular, due to its rather low availability worldwide and the risk of potential complications [1].
Therapy of HFpEF
Treatment of comorbidities and risk factors
Patients with HFpEF exhibit numerous comorbidities and risk factors that have been associated with increased morbidity and mortality [9, 10]. Therefore, the systematic screening and adequate treatment of these comorbidities and risk factors should represent a cornerstone of any HFpEF management strategy [11], as they have an important impact on patient prognosis (Fig. 1); this is also currently studied in the OPTIMIZE-HFpEF trial (NCT02425371).
Proposed algorithm for the therapy of patients with heart failure with preserved ejection fraction. ACEi angiotensin-converting enzyme inhibitor, ARB angiotensin receptor blocker, CAD coronary artery disease, CCB calcium channel blocker, iv intravenous, MRA mineralocorticoid receptor antagonist, PDE5i phosphodiesterase type 5 inhibitor, sGC soluble guanylate cyclase, SGLT2i sodium-glucose cotransporter 2 inhibitor
Obesity and deconditioning are frequently present in HFpEF patients. In a post hoc analysis of the I‑PRESERVE trial, the majority of the 4109 patients included were overweight or obese according to their body mass index (BMI) of ≥ 26.5 kg/m2 [12]. Interestingly, patients with higher BMI were younger, more likely to be female, hypertensive as well as diabetic, and had higher LVEF. Moreover, besides a low BMI of < 23.5 kg/m2, the risk for the primary endpoint (death from any cause or hospitalization for HF, myocardial infarction, unstable angina, arrhythmia, or stroke) was significantly increased in obese HFpEF patients with a BMI of ≥ 35 kg/m2 [12]. Accordingly, in a pooled analysis with a total of 96,424 HF patients (59,263 with HFpEF and 37,161 with HFrEF), the association between BMI and all-cause mortality was found to be U‑shaped for both HFpEF and HFrEF patients, with a similar nadir of risk at a BMI of 32–33 kg/m2 [13]. Thus, treating physicians should emphasize the importance of physical activity as well as a hypocaloric diet, which both have been shown to be beneficial in HFpEF. For instance, according to a sub-analysis of the TOPCAT trial, high physical activity led to a significantly decreased risk of the composite primary endpoint (HF hospitalization, cardiovascular mortality, or aborted cardiac arrest) in HFpEF patients [14]. Furthermore, physical activity in HFpEF has been assessed by the prospective, randomized controlled Ex-DHF pilot trial [15]. Compared to usual care, supervised exercise training reduced diastolic dysfunction in terms of E/e′ and improved exercise capacity, regardless of chronotropic competence. However, as recently shown in the OptimEx-Clin trial, advising HFpEF patients to be physically active is more important than creating mandatory training programs and permanent supervision of physical activity, which may be difficult to realize in clinical practice [16]. Accordingly, one-time advice on physical activity as recommended by the guidelines resulted in a similar increase in peak oxygen consumption (peak VO2) as opposed to high-intensity interval training (3 × 38 min/week) and moderate continuous training (5 × 40 min/week) among 180 HFpEF patients. To date, the data on caloric restriction in HFpEF patients are rather sparse and are mainly derived from a single study. In this randomized, prospective trial with 100 obese HFpEF patients, a 20-week hypocaloric diet led to a 7% decrease in body weight and an improvement in peak VO2 of 1.3 ml/kg/min [17]. In patients that additionally were assigned to perform supervised exercise training, body weight was decreased by even 10% and peak VO2 increased by 2.5 ml/kg/min.
Moreover, hypertension as well as diabetes are common comorbidities and risk factors in patients with HFpEF [5, 11]. Particularly since the publication of the EMPEROR-Preserved trial [18], the SGLT2-inhibitor empagliflozin should be the primary treatment option for diabetes in HFpEF patients. In March 2022, the European Commission granted an indication of empagliflozin for all adults with symptomatic chronic HF, which includes patients across the full spectrum of LVEF [19]. The EMPEROR-Preserved trial [18] and the value of SGLT2-inhibitors in HFpEF patients are discussed in greater detail in Sect. “Sodium glucose cotransporter 2 inhibitors”. As hypertension may lead to cardiac decompensation [20] and mainly contributes to the development of HFpEF, an adequate hypertension treatment represents an essential part of any HFpEF therapy. Although there is uncertainty about the optimal hypertensive therapy in HFpEF patients, the 2021 ESC guidelines recommend considering the same treatment strategy as in patients with HFrEF [1]. In a meta-analysis including 75 prospective, randomized comparative studies, beta-blockers or diuretics caused less LV mass regression than angiotensin receptor blockers (ARBs), angiotensin-converting enzyme inhibitors (ACEi), and calcium channel blockers (CCBs; [21]).
Furthermore, iron deficiency is commonly present in patients with HFpEF. According to a small study with 190 symptomatic HFpEF patients, severe diastolic dysfunction was more likely to be found in iron-deficient patients [22]. Also, the presence of iron deficiency correlated with reduced exercise capacity and quality of life (QOL). The effects of intravenous iron administration in HFpEF are currently unknown, while it has been shown to have beneficial effects on symptoms and QOL in HFrEF [23]. However, therapy with intravenously administered iron in HFpEF is being evaluated in the two ongoing randomized controlled trials: FAIR-HFpEF (NCT03074591) and PREFER-HF (NCT03833336).
Angiotensin receptor neprilysin inhibitor (LCZ696)
Besides the inhibition of the angiotensin II receptor type 1, LCZ696 inhibits the metalloprotease neprilysin, which results in increased levels of natriuretic peptides, and thus causes vasodilatation and increased diuresis [11]. Moreover, inhibition of neprilysin promotes the formation of cGMP, therefore interfering with the NO-cGMP-PKG (“nitric oxide–-cyclic guanosine monophosphate–protein kinase”) axis, which is thought to play an essential part in the pathophysiology of HFpEF [24, 25].
However, in the randomized controlled PARAGON-HF trial [26] with 4822 HFpEF patients included (LVEF of at least 45%), treatment with LCZ696 failed to significantly reduce the risk of the primary endpoint of total HF hospitalizations or CV death.
Interestingly, data from a retrospective analysis question the pathophysiological rationale for neprilysin inhibition in HFpEF. Accordingly, in 144 HFpEF patients, increased neprilysin levels were not associated with a greater rate of HF hospitalizations or death [27]. By contrast, in patients with HFrEF, elevated neprilysin levels correlated with an unfavorable prognosis. In 1069 HFrEF patients, the risk of the combined endpoint of HF hospitalization and CV death was increased by 20% if the neprilysin serum level was above the median [28].
Nevertheless, a nonsignificant but nominal risk reduction of 13% was observed in the treatment arm of the PARAGON-HF study [26]. This was initially attributed to a more efficient blood pressure reduction with LCZ696, which is approximately twice as high as with valsartan [29]. However, a post hoc analysis of the PARAGON-HF trial showed that the aforementioned nominal risk reduction in the primary endpoint did not result from the greater decrease in systolic blood pressure with LCZ696 therapy [30].
Furthermore, in the PARAGON-HF study [26], the definition of HFpEF and thus the criteria for study inclusion were primarily based on the recorded LVEF, which had to be at least 45%. In addition, patients did not have to receive a mandatory etiological work-up prior to enrolment to exclude specific causes of HFpEF such as amyloidosis and Fabry’s disease, which could be resistant to treatment with LCZ696. Therefore, the inclusion criteria of the PARAGON-HF study did not allow for the heterogeneity of the HFpEF syndrome, representing a potential limitation.
This aspect appears to be further underlined by the results of the subgroup analyses of the PARAGON-HF study. Whereas women appeared to benefit significantly from the LCZ696 therapy, particularly through a reduction in HF hospitalizations, this was not the case in men [31]. Moreover, in patients with an LVEF between 45% and 57%, the risk of the primary endpoint was significantly decreased by 22% through LCZ696 compared with valsartan only. By contrast, in patients with an LVEF above the median of 57%, there were no significant differences regarding the primary endpoint between the intervention and the control arm [26]. Recently, data from PARAGON-HF and PARADIGM-HF were pooled in order to examine LCZ696 treatment effects across the spectrum of LVEF. In this analysis, the administration of LCZ696 led to a significant decrease of the primary endpoint up to an LVEF of 55% ([32]; Fig. 1). Similar results were obtained from post hoc analyses of other large HFpEF studies, suggesting that candesartan (CHARM-Preserved, [33]) and spironolactone (TOPCAT, [34]) have a significant treatment benefit for patients with an LVEF below 55% [35]. Furthermore, positive therapeutic effects have been demonstrated for beta-blocker therapy, up to an LVEF of < 50% [36]. However, it should be noted that the LVEF range of 45–55% according to the ESC definition includes not only patients with HFpEF, but also those with HFmrEF ([1]; Fig. 2).
Range of left ventricular ejection fraction, in which candesartan, beta-blockers, spironolactone, LCZ696, and empagliflozin significantly reduce the risk of HF hospitalization and/or CV death for all heart failure patients (original trials indicated in brackets). CV cardiovascular, HF heart failure, HFmrEF heart failure with mildly-reduced ejection fraction, HFpEF heart failure with preserved ejection fraction, HFrEF heart failure with reduced ejection fraction, LVEF left ventricular ejection fraction
In February 2021, the US Food and Drug Administration (FDA) granted an expanded indication to LCZ696 for patients with LVEF below normal (< 50%) [37]. However, the FDA also pointed out that, “LVEF is a variable measure and the use of clinical judgment is essential in deciding whom to treat.” At the present time, the authors believe that therapy with LCZ696 may be beneficial in selected individuals. The decision, however, should not only include the reported LVEF, but should be based on as many diagnostic modalities as possible, such as those included in the HFA-PEFF [8] or H2FPEF [7] score.
Sodium glucose cotransporter 2 inhibitors
Gliflozines, such as empagliflozin, canagliflozin, or dapagliflozin, inhibit the sodium-glucose cotransporter 2 (SGLT2) of the proximal renal tubules, thereby reducing glucose reabsorption from the primary urine, and ultimately causing renal glucosuria. Thus, a decrease in blood glucose levels can be achieved. Consequently, these SGLT2-inhibitors (SGLT2i) have been initially studied as anti-diabetic drugs. As recently shown in two large randomized trials, treatment with either empagliflozin (EMPEROR-Reduced, [38]) or dapagliflozin (DAPA-HF, [39]) is associated with a significant decrease in morbidity and mortality in patients suffering from HFrEF, irrespective of diabetes status. The underlying mechanisms remain the subject of ongoing discussions within the scientific community. These include an improvement in cardiac energetics through increased ketone body production and a decrease in preload and afterload [40, 41]. In 2021, the EMPEROR-Preserved trial investigated the effects of empagliflozin in 5988 symptomatic (NYHA stadium III–IV) HFpEF patients (LVEF ≥ 40%), regardless of the presence or absence of diabetes [18]. Compared to placebo, therapy with empagliflozin resulted in a significant reduction of the primary endpoint (composite of CV death or HF hospitalization). According to the sub-analyses, the treatment effects were similar in HFpEF patients with and without diabetes. Furthermore, health-related QOL measured by the KCCQ score was significantly improved in the intervention arm. Of note, this effect was documented early on and was sustained for 1 year or longer [42]. In March 2022, the European Commission approved treatment with empagliflozin for all patients with symptomatic chronic HF, including patients across the full spectrum of LVEF [19]. Currently, there is another large randomized controlled trial (DELIVER; NCT03619213) studying the effects of dapagliflozin on a composite primary endpoint (CV death, HF hospitalization, urgent HF visit) in HFpEF patients (LVEF ≥ 40%).
To date, empagliflozin represents the first drug to significantly improve outcomes in HFpEF. It will be exciting to see whether these effects apply equally to other SGLT2i, in particular dapagliflozin, which will be clarified in the DELIVER trial [58]. Overall, the authors are convinced that empagliflozin should be the cornerstone of any HFpEF medical treatment, especially due to the lack of other evidence-based options.
Management of fluid level in HFpEF patients
Fluid overload may rapidly lead to signs and symptoms of congestion in HFpEF patients. Thus, diuretics remain an essential part of any HFpEF management. However, the monitoring of patients’ fluid status can be challenging and is often limited to traditional assessment tools such as daily weight controls [43, 44, 45]. Some telemonitoring devices on the other hand allow for the detection of impending cardiac decompensation at an early stage, and can therefore help to avoid HF hospitalizations. For instance, telemonitoring of the pulmonary arterial pressure using the CardioMEMS device has proven to be an effective therapeutic measure. After the convincing results of the U.S. CHAMPION study [46], the method was evaluated in Europe in the MEMS-HF trial [47]. This was a prospective, but not placebo-controlled, study in which 234 symptomatic HF patients were included. Of note, the study inclusion was independent of LVEF. Consequently, patients with HFrEF (LVEF < 40%) as well as HFmrEF and HFpEF (LVEF ≥ 40%) were included. Hospitalization rates due to HF were reduced by 62% after implantation of the CardioMEMS device [47]. In addition, an improvement in QOL was demonstrated after the initiation of CardioMEMS-guided therapy, which was objectively measured using the KCCQ score. Complications from CardioMEMS implantation and sensor failure were documented in only four patients (1.7%) and did not result in death. For further evaluation of hemodynamic-guided HF management, the randomized, placebo-controlled GUIDE-HF trial was initiated [48]. In this trial, 1022 symptomatic HF patients (NYHA II–IV) with either a recent HF hospitalization or elevated natriuretic peptides were enrolled. Surprisingly, CardioMEMS-guided HF management did not decrease the risk of the primary endpoint, which was a composite of all-cause mortality and total HF events (HF hospitalizations and urgent HF hospital visits) at 12 months [48]. However, these results may have been influenced considerably by the COVID-19 pandemic, thus representing an important limitation of the GUIDE-HF trial. Accordingly, in a pre-COVID-19 impact analysis, the risk of the primary endpoint was significantly lower in the intervention arm compared with usual care. This was primarily driven by the reduction of HF hospitalizations. During the COVID-19 pandemic, the primary event rate in the control arm decreased by 21%, while it did not change significantly in the intervention arm. As a result, the pre-COVID-19 treatment effects diminished [48]. Of note, these differences cannot be explained by changes in provider- or disease-dependent factors [49]. Thus, the outcomes in GUIDE-HF were most likely affected by changes in patient-dependent factors due to COVID-19, such as changes in behavioral patterns. Therefore, the impact of hemodynamic-guided HF management needs to be investigated in further trials.
Assumably, telemonitoring of fluid status to guide diuretic treatment in HF patients (HFpEF, HFmrEF, and HFrEF) will become increasingly important in the future. The authors encourage the implementation of home monitoring in current HFpEF management strategies, if available.
Interventional therapy of HFpEF
There are various interventional approaches to improve HFpEF therapy, which comprise, for instance, the implementation of atrial shunt devices (ASD), cardiac contractility modulation (CCM), cardiac resynchronization therapy (CRT), and the catheter-based denervation of renal sympathetic nerves [5]. Of these, the implementation of ASDs to decrease left atrial pressure by generating artificial left–right shunts has been the most promising. In the REDUCE LAP-HF I trial, this method has been shown to significantly reduce left atrial pressure during exercise [50] and to be safe [51]. However, just recently, the results of the REDUCE LAP-HF II trial [52] were published. In this randomized, multicenter, sham-controlled trial, a total of 626 symptomatic HFpEF patients (LVEF ≥ 40%) with increased pulmonary capillary wedge pressure (PCWP) during exercise (≥ 25 mm Hg) were enrolled. The primary endpoint was a hierarchical composite of CV death or non-fatal ischemic stroke at 12 months, rate of total HF events up to 24 months, and change in KCCQ overall summary score at 12 months. Compared with sham-control, the intervention did not have any significant therapeutic effects, neither on the primary composite endpoint nor on its individual components [52].
Management of atrial fibrillation in HFpEF
Atrial fibrillation (AF) is a common and prognostically unfavorable concomitant disease in patients with HFpEF [1]. In a post hoc analysis of the TOPCAT trial, the occurrence of AF was independently associated with an increased risk of CV events (CV mortality, aborted cardiac arrest, or HF hospitalization; [53]).
Catheter-based pulmonary vein isolation (PVI) in patients with HFrEF has emerged as a cornerstone in AF therapy and improves clinical outcomes compared to medical treatment [54]. However, it is currently unclear whether patients with HFpEF can benefit equally from catheter ablation. Interestingly, data from the German ablation registry suggest that PVI for rhythm control is frequently performed in HFpEF patients [55]. Thus, randomized trials are desperately needed to clarify the role of PVI in patients suffering from HFpEF.
According to the ESC guidelines [56], if no further therapeutic attempts are made to preserve sinus rhythm and both the treating physician and the patient accept the presence of AF by consensus, so-called permanent AF is present. In this case, the primary objective of AF therapy is the control of ventricular heart rate, which should not exceed 110 bpm. In patients with HF, beta-blockers and digitalis glycosides are available for this purpose. The RATE-AF study [57] randomly compared the effects of bisoprolol and digoxin in patients with permanent AF and HF (defined as NYHA stage II–IV). The study included mostly patients with HFpEF (LVEF ≥ 50%), whereas only about 19% of patients had LVEF < 50%. With regard to the primary endpoint (increase in QOL objectified by the 36-item Short Form Health Survey physical component summary score), no significant differences were demonstrated in either treatment group. However, a decrease in NT-pro-BNP levels as well as serious clinical events (death, unplanned hospitalizations, treatment-related adverse events, primary care visits) was observed in patients treated with digoxin [57].
Conclusion
Heart failure with preserved ejection fraction (HFpEF) is a heterogeneous syndrome and a diagnosis based solely on LVEF may be insufficient. The diagnostic process should ideally use the recently introduced H2FPEF and HFA-PEFF algorithms. HFpEF therapy must include the adequate treatment of comorbidities and risk factors, as they influence prognosis. Avoiding fluid overload by diuretic treatment to increase quality of life is an essential part of HFpEF therapy. If available, telemonitoring should be incorporated into HFpEF management to detect fluid overload before signs and symptoms of congestion. LCZ696 has been granted an expanded indication for patients with LVEF < 50% by the FDA. Empagliflozin is the first drug to significantly reduce morbidity and mortality in HFpEF patients and should be the cornerstone of any HFpEF treatment. The DELIVER trial will investigate whether this also applies to dapagliflozin. Further research is needed to enhance our understanding of the complex syndrome of HFpEF and help improve HFpEF management.
References
McDonagh TA, Metra M, Adamo M et al (2021) 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J 42(36):3599–3726
Chen X, Savarese G, Dahlstrom U et al (2019) Age-dependent differences in clinical phenotype and prognosis in heart failure with mid-range ejection compared with heart failure with reduced or preserved ejection fraction. Clin Res Cardiol 108(12):1394–1405
Fonarow GC, Stough WG, Abraham WT et al (2007) Characteristics, treatments, and outcomes of patients with preserved systolic function hospitalized for heart failure: a report from the OPTIMIZE-HF registry. J Am Coll Cardiol 50(8):768–777
Lam CSP, Donal E, Kraigher-Krainer E, Vasan RS (2011) Epidemiology and clinical course of heart failure with preserved ejection fraction. Eur J Heart Fail 13(1):18–28
Wintrich J, Kindermann I, Ukena C et al (2020) Therapeutic approaches in heart failure with preserved ejection fraction: past, present, and future. Clin Res Cardiol 109(9):1079–1098
Triposkiadis F, Butler J, Abboud FM et al (2019) The continuous heart failure spectrum: moving beyond an ejection fraction classification. Eur Heart J 40(26):2155–2163
Reddy YNV, Carter RE, Obokata M et al (2018) A simple, evidence-based approach to help guide diagnosis of heart failure with preserved ejection fraction. Circulation 138(9):861–870
Pieske B, Tschöpe C, de Boer RA et al (2019) How to diagnose heart failure with preserved ejection fraction: the HFA-PEFF diagnostic algorithm: a consensus recommendation from the heart failure association (HFA) of the European society of cardiology (ESC). Eur Heart J 40(40):3297–3317
Dunlay SM, Roger VL, Redfield MM (2017) Epidemiology of heart failure with preserved ejection fraction. Nat Rev Cardiol 14(10):591–602
Riedel O, Ohlmeier C, Enders D et al (2018) The contribution of comorbidities to mortality in hospitalized patients with heart failure. Clin Res Cardiol 107(6):487–497
Tschöpe C, Birner C, Böhm M et al (2018) Heart failure with preserved ejection fraction: current management and future strategies : expert opinion on the behalf of the nucleus of the “heart failure working group” of the German society of cardiology (DKG). Clin Res Cardiol 107(1):1–19
Haass M, Kitzman DW, Anand IS et al (2011) Body mass index and adverse cardiovascular outcomes in heart failure patients with preserved ejection fraction: results from the irbesartan in heart failure with preserved ejection fraction (I-PRESERVE) trial. Circ Heart Fail 4(3):324–331
Zhang J, Begley A, Jackson R et al (2019) Body mass index and all-cause mortality in heart failure patients with normal and reduced ventricular ejection fraction: a dose-response meta-analysis. Clin Res Cardiol 108(2):119–132
Hegde SM, Claggett B, Shah AM et al (2017) Physical activity and prognosis in the TOPCAT trial (treatment of preserved cardiac function heart failure with an aldosterone antagonist). Circulation 136(11):982–992
Edelmann F, Gelbrich G, Dungen H‑D et al (2011) Exercise training improves exercise capacity and diastolic function in patients with heart failure with preserved ejection fraction: results of the Ex-DHF (exercise training in diastolic heart failure) pilot study. J Am Coll Cardiol 58(17):1780–1791
Mueller S, Winzer EB, Duvinage A et al (2021) Effect of high-intensity interval training, moderate continuous training, or guideline-based physical activity advice on peak oxygen consumption in patients with heart failure with preserved ejection fraction: a randomized clinical trial. JAMA 325(6):542–551
Kitzman DW, Brubaker P, Morgan T et al (2016) Effect of caloric restriction or aerobic exercise training on peak oxygen consumption and quality of life in obese older patients with heart failure with preserved ejection fraction: a randomized clinical trial. JAMA 315(1):36–46
Anker SD, Butler J, Filippatos G et al (2021) Empagliflozin in heart failure with a preserved ejection fraction. N Engl J Med 385(16):1451–1461
https://www.boehringer-ingelheim.com/human-health/heart-diseases/heart-failure/preserved-heart-failure-treatment-approval-europe. Accessed 31.3.22
Beckett NS, Peters R, Fletcher AE et al (2008) Treatment of hypertension in patients 80 years of age or older. N Engl J Med 358(18):1887–1898
Fagard RH, Celis H, Thijs L, Wouters S (2009) Regression of left ventricular mass by antihypertensive treatment: a meta-analysis of randomized comparative studies. Hypertension 54(5):1084–1091
Bekfani T, Pellicori P, Morris D et al (2019) Iron deficiency in patients with heart failure with preserved ejection fraction and its association with reduced exercise capacity, muscle strength and quality of life. Clin Res Cardiol 108(2):203–211
Anker SD, Kirwan BA, van Veldhuisen DJ et al (2018) Effects of ferric carboxymaltose on hospitalisations and mortality rates in iron-deficient heart failure patients: an individual patient data meta-analysis. Eur J Heart Fail 20(1):125–133
Paulus WJ, Tschöpe C, Sanderson JE et al (2007) How to diagnose diastolic heart failure: a consensus statement on the diagnosis of heart failure with normal left ventricular ejection fraction by the heart failure and echocardiography associations of the European society of cardiology. Eur Heart J 28(20):2539–2550
Tschöpe C, Van Linthout S (2014) New insights in (inter)cellular mechanisms by heart failure with preserved ejection fraction. Curr Heart Fail Rep 11(4):436–444
Solomon SD, McMurray JJV, Anand IS et al (2019) Angiotensin-neprilysin inhibition in heart failure with preserved ejection fraction. N Engl J Med 381(17):1609–1620
Goliasch G, Pavo N, Zotter-Tufaro C et al (2016) Soluble neprilysin does not correlate with outcome in heart failure with preserved ejection fraction. Eur J Heart Fail 18(1):89–93
Bayes-Genis A, Barallat J, Galan A et al (2015) Soluble neprilysin is predictive of cardiovascular death and heart failure hospitalization in heart failure patients. J Am Coll Cardiol 65(7):657–665
Ruilope LM, Dukat A, Böhm M et al (2010) Blood-pressure reduction with LCZ696, a novel dual-acting inhibitor of the angiotensin II receptor and neprilysin: a randomised, double-blind, placebo-controlled, active comparator study. Lancet 375(9722):1255–1266
Selvaraj S, Claggett BL, Böhm M et al (2020) Systolic blood pressure in heart failure with preserved ejection fraction treated with sacubitril/valsartan. J Am Coll Cardiol 75(14):1644–1656
McMurray JJV, Jackson AM, Lam CSP et al (2020) Effects of sacubitril-valsartan, versus valsartan, in women compared to men with heart failure and preserved ejection fraction: insights from PARAGON-HF. Circulation 141(5):338–351
Solomon SD, Vaduganathan M, Claggett BL et al (2020) Sacubitril/valsartan across the spectrum of ejection fraction in heart failure. Circulation 141(5):352–361
Yusuf S, Pfeffer MA, Swedberg K et al (2003) Effects of candesartan in patients with chronic heart failure and preserved left-ventricular ejection fraction: the CHARM-preserved trial. Lancet 362(9386):777–781
Pitt B, Pfeffer MA, Assmann SF et al (2014) Spironolactone for heart failure with preserved ejection fraction. N Engl J Med 370(15):1383–1392
Böhm M, Bewarder Y, Kindermann I (2020) Ejection fraction in heart failure revisited—where does the evidence start? Eur Heart J 41(25):2363–2365
Cleland JGF, Bunting KV, Flather MD et al (2018) Beta-blockers for heart failure with reduced, mid-range, and preserved ejection fraction: an individual patient-level analysis of double-blind randomized trials. Eur Heart J 39(1):26–35
Novartis (2021) Novartis Entresto® granted expanded indication in chronic heart failure by FDA. https://www.novartis.com/news/media-releases/novartis-entresto-granted-expanded-indication-chronic-heart-failure-fda. Accessed 31.3.22
Packer M, Anker SD, Butler J et al (2020) Cardiovascular and renal outcomes with empagliflozin in heart failure. N Engl J Med 383(15):1413–1424
McMurray JJV, Solomon SD, Inzucchi SE et al (2019) Dapagliflozin in patients with heart failure and reduced ejection fraction. N Engl J Med 381(21):1995–2008
Maack C, Lehrke M, Backs J et al (2018) Heart failure and diabetes: metabolic alterations and therapeutic interventions: a state-of-the-art review from the translational research committee of the heart failure association-European society of cardiology. Eur Heart J 39(48):4243–4254
Verma S, McMurray JJV, Cherney DZI (2017) The metabolodiuretic promise of sodium-dependent glucose cotransporter 2 inhibition: the search for the sweet spot in heart failure. JAMA Cardiol 2(9):939–940
Butler J, Filippatos G, Jamal Siddiqi T et al (2022) Empagliflozin, health status, and quality of life in patients with heart failure and preserved ejection fraction: the EMPEROR-preserved trial. Circulation 145(3):184–193
Chaudhry SI, Wang Y, Concato J et al (2007) Patterns of weight change preceding hospitalization for heart failure. Circulation 116(14):1549–1554
Lewin J, Ledwidge M, O’Loughlin C et al (2005) Clinical deterioration in established heart failure: what is the value of BNP and weight gain in aiding diagnosis? Eur J Heart Fail 7(6):953–957
Stevenson LW, Perloff JK (1989) The limited reliability of physical signs for estimating hemodynamics in chronic heart failure. JAMA 261(6):884–888. https://doi.org/10.1001/jama.1989.03420060100040
Abraham WT, Stevenson LW, Bourge RC et al (2016) Sustained efficacy of pulmonary artery pressure to guide adjustment of chronic heart failure therapy: complete follow-up results from the CHAMPION randomised trial. Lancet 387(10017):453–461
Angermann CE, Assmus B, Anker SD et al (2020) Pulmonary artery pressure-guided therapy in ambulatory patients with symptomatic heart failure: the CardioMEMS European monitoring study for heart failure (MEMS-HF). Eur J Heart Fail 22(10):1891–1901
Lindenfeld J, Zile MR, Desai AS et al (2021) Haemodynamic-guided management of heart failure (GUIDE-HF): a randomised controlled trial. Lancet 398(10304):991–1001
Zile MR, Desai AS, Costanzo MR et al (2022) The GUIDE-HF trial of pulmonary artery pressure monitoring in heart failure: impact of the COVID-19 pandemic. Eur Heart J. https://doi.org/10.1093/eurheartj/ehac114
Hasenfuss G, Hayward C, Burkhoff D et al (2016) A transcatheter intracardiac shunt device for heart failure with preserved ejection fraction (REDUCE LAP-HF): a multicentre, open-label, single-arm, phase 1 trial. Lancet 387(10025):1298–1304
Shah SJ, Feldman T, Ricciardi MJ et al (2018) One-year safety and clinical outcomes of a transcatheter interatrial shunt device for the treatment of heart failure with preserved ejection fraction in the reduce elevated left atrial pressure in patients with heart failure (REDUCE LAP-HF I) trial: a randomized clinical trial. JAMA Cardiol 3(10):968–977
Shah SJ, Borlaug BA, Chung ES et al (2022) Atrial shunt device for heart failure with preserved and mildly reduced ejection fraction (REDUCE LAP-HF II): a randomised, multicentre, blinded, sham-controlled trial. Lancet 399(10330):1130–1140. https://doi.org/10.1016/S0140-6736(22)00016-2
Cikes M, Claggett B, Shah AM et al (2018) Atrial fibrillation in heart failure with preserved ejection fraction: the TOPCAT trial. JACC Heart Fail 6(8):689–697
Marrouche NF, Brachmann J, Andresen D et al (2018) Catheter ablation for atrial fibrillation with heart failure. N Engl J Med 378(5):417–427
Eitel C, Ince H, Brachmann J et al (2019) Atrial fibrillation ablation strategies and outcome in patients with heart failure: insights from the German ablation registry. Clin Res Cardiol 108(7):815–823
Hindricks G, Potpara T, Dagres N et al (2021) 2020 ESC guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European association for cardio-thoracic surgery (EACTS): the task force for the diagnosis and management of atrial fibrillation of the europe. Eur Heart J 42(5):373–498
Kotecha D, Bunting KV, Gill SK et al (2020) Effect of digoxin vs bisoprolol for heart rate control in atrial fibrillation on patient-reported quality of life: the RATE-AF randomized clinical trial. JAMA 324(24):2497–2508
Solomon SD, Vaduganathan M, Claggett BL et al (2022) Baseline characteristics of patients with HF with mildly reduced and preserved ejection fraction: DELIVER trial. JACC Heart Fail 10(3):184–197
Funding
This work has not been funded.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
J. Wintrich received speaker honoraria from Brystol Myers Squibb. M. Böhm is supported by the Deutsche Forschungsgemeinschaft (SFB TTR 219, S‑01 project number 322900939) and reports personal fees from Abbott, Amgen, Astra Zeneca, Bayer, Boehringer Ingelheim, Cytokinetics, Medtronic, Novartis, Servier and Vifor. A. Abdin declare that he has no competing interests.
For this article no studies with human participants or animals were performed by any of the authors. All studies mentioned were in accordance with the ethical standards indicated in each case.
Rights and permissions
About this article
Cite this article
Wintrich, J., Abdin, A. & Böhm, M. Management strategies in heart failure with preserved ejection fraction. Herz 47, 332–339 (2022). https://doi.org/10.1007/s00059-022-05119-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-022-05119-5