Abstract
Purpose
Acidification by bacterial biofilms at the bracket/tooth interface is one of the most common problems in fixed orthodontic treatments, which can lead to white spot lesions (WSL) and caries. As lingual brackets were shown to exhibit reduced WSL formation clinically, the aim of this in situ study was to compare initial intraoral biofilm formation and acidification on bracket-like specimens placed buccally and palatally in the upper jaw as a possible cause for this observation.
Methods
Intraoral biofilm was collected from splints equipped with buccally and palatally exposed test specimens, which were worn by 12 volunteers for a total of 48 h. The test specimens consisted of standard bracket material cylinders on top of a hydroxyapatite disc to represent the bracket/tooth interface. They were analyzed for three-dimensional biofilm volume and live/dead distribution by fluorescence staining and confocal laser scanning microscopy as well as for acidification by fluorescence-based pH ratiometry.
Results
Similar general biofilm morphology with regard to volume and viability could be detected for buccally and palatally exposed specimens. For pH values, biofilms from both positions showed increased acidification at the bottom layer. Interestingly, the pH value at the top layers of the biofilms was slightly lower on palatally than on buccally exposed specimens, which may likely be due to anatomic conditions.
Conclusion
Based on the results of this study, initial intraoral biofilm formation and acidification is almost similar on the bracket material/biomimetic tooth interface when placed buccally or palatally in the upper jaw. As lingual brackets were shown to exhibit reduced WSL formation clinically, future studies should investigate further factors like bracket geometry.
Zusammenfassung
Zielsetzung
Die durch bakterielle Biofilme verursachte Ansäuerung an der Bracket/Zahn-Grenzfläche ist eines der häufigsten Probleme während der festsitzenden kieferorthopädischen Behandlung, das zu White-Spot-Läsionen (WSL) und Karies führen kann. Da linguale Multibracketapparaturen klinisch eine verminderte WSL-Bildung aufweisen, war das Ziel dieser In-situ-Studie, die initiale intraorale Biofilmbildung und Ansäuerung an bukkal und palatinal im Oberkiefer platzierten Bracket-ähnlichen Probekörpern als mögliche Ursache zu analysieren.
Methoden
Mit Probekörpern bestückte Miniplastschienen dienten der intraoralen Biofilmgewinnung in 12 Probanden für insgesamt 48 h. Die Probekörper wurden bukkal und palatinal platziert und bestanden aus Standard-Bracketmaterialzylindern, welche auf Hydroxylapatitscheiben befestigt wurden, sodass die Bracket/Zahn-Grenzfläche imitiert werden konnte. Die Analyse des dreidimensionalen Biofilmvolumens und der Lebend/tot-Verteilung erfolgte durch Fluoreszenzfärbung und konfokale Laserscanningmikroskopie. Die Auswertung der Ansäuerung erfolgte durch fluoreszenzbasierte pH-Ratiometrie.
Ergebnisse
In Bezug auf das Volumen und die Viabilität konnte für bukkal und palatinal exponierte Probekörper eine allgemein ähnliche Biofilmmorphologie nachgewiesen werden. An beiden Positionen war eine erhöhte Ansäuerung in den unteren Schichten des Biofilms zu detektieren. Interessanterweise war der pH-Wert in den obersten Schichten der Biofilme bei palatinal positionierten Probekörpern etwas niedriger als bei bukkal positionierten Probekörpern, was vermutlich durch anatomische Gegebenheiten bedingt ist.
Schlussfolgerung
Basierend auf den Ergebnissen dieser Studie ist die initiale intraorale Biofilmbildung und Ansäuerung an der Grenzfläche zwischen Bracketmaterial und biomimetischem Zahn bei bukkaler bzw. palatinaler Platzierung im Oberkieferbereich ähnlich. Da linguale Multibracketapparaturen klinisch eine reduzierte WSL-Bildung aufweisen, sollten zukünftige Studien weitere Faktoren wie die Bracketgeometrie untersuchen.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Biofilms are structured microbial communities that are attached to a surface and surrounded by an extracellular matrix. In the mouth, they are responsible for many diseases, like caries and periodontal diseases, the two most prevalent medical threats in industrialized societies [10, 18, 43]. Dental caries is defined as a multifactorial, biofilm-mediated, diet-modulated, noncommunicable, dynamic disease resulting in mineral loss of dental hard tissues [21, 41, 48].
Biofilm formation begins shortly after the tooth surface has been cleaned. A pellicle composed of salivary proteins forms. This pellicle serves oral bacteria as attachment point to colonize the tooth surface [30, 39, 54]. When further bacteria colonize, the plaque grows into a three-dimensional structure surrounded by a matrix of self-produced extracellular polysaccharides [28]. In dental biofilms, the pH value of the extracellular matrix is the main virulence factor for the development of caries [57]. In order to gain energy, microorganisms in the plaque metabolize low-molecular-weight carbohydrates, thereby creating organic acids [10, 67]. This lowers the pH value, and minerals of the enamel such as calcium and phosphate can be dissolved. For tooth enamel, the critical pH value is 5.2–5.7 [28].
Enamel demineralization is also a significant risk factor and one of the greatest challenges during fixed orthodontic treatment [65]. The insertion of brackets, bands and arches complicates oral hygiene and promotes the accumulation of plaque [19].
The local acidification can subsequently lead to white spot lesions (WSL), which represent the first stage of caries formation [40]. WSL are milky white opacities of the enamel surface without cavity formation [59], which can already occur one month after the start of orthodontic treatment [46, 47]. The incidence of WSL is given in the literature up to 72.9% [53]. A 2015 meta-analysis concluded that the incidence of WSL during orthodontic treatment was 45.8% and the prevalence was 68.4% [59].
A significant reduction in the occurrence of WSL during orthodontic treatment was observed with a completely customized lingual multibracket appliance. The global incidence of new WSL for this treatment was determined to be only 3.19% for the entire dentition (teeth 17–47) [69]. When focusing on the upper incisors, it was shown that the subject-related incidence was 9.59% and the teeth-related incidence was 4.1% [36]. A comparison with previous studies on WSL incidence following conventional buccal appliances indicated a reduction by a factor 6.35 for the subject-related and a reduction by a factor 14 for the teeth-related WSL incidence [36]. Another study comparing WSL between lingual and buccal multibracket appliances found that the number of newly developing or progressive WSL was 4.8 times lower lingually than buccally [66]. In addition, the integrated fluorescence loss, measured using the quantitative light-induced fluorescence, was 10.6 times lower for lingual than for buccal surfaces [66].
According to these results, one could hypothesize that there is less biofilm formation on lingual than on buccal orthodontic brackets. As a consequence, acidification would be lower and fewer WSLs would occur. However, studies comparing biofilm formation and acidification lingually/palatally and buccally at the bracket–tooth interface have not yet been carried out.
Therefore, the objective of this in situ study was the three-dimensional investigation of initial intraoral biofilm formation and pH values on buccal and palatal bracket material. For this purpose, splints equipped with test specimens were exposed to the oral cavity of 12 volunteers for a total of 48 h. To quantify biofilm volume and live/dead distribution, the specimens were fluorescently stained and examined by confocal laser scanning microscopy (CLSM). The pH value within the biofilms was measured using pH ratiometry by the pH-sensitive ratiometric dye seminaphthorhodafluor-4F 5‑(and -6)-carboxylic acid (C-SNARF-4). Depending on the protonation, the dye shows a shift in its fluorescence emission detected by CLSM and can, thus, measure the extracellular pH value in the range from 4.5 to 7.0.
By combining the results of biofilm volume and pH value quantification, biofilm formation and acidification on buccally and palatally exposed bracket materials in the upper jaw were compared.
Materials and methods
Subject selection
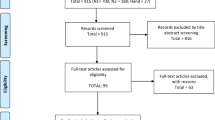
The present study was approved by the ethical committee of the Hannover Medical School (amendment to ethic vote no. 8570_BO_S2019). Twelve individuals (6 women and 6 men) aged between 23 and 36 years (mean 27.6 years) participated in this study. Their healthy periodontal condition was assured by an initial periodontal screening including the probing depths (PD), the modified sulcus bleeding index according to Lange (SBI) and the modified approximal plaque index according to Lange (API) [28].
Exclusion criteria were general diseases, antibiotic treatment 6 weeks before participation, smoking, removable dentures, and pregnancy. All participants were informed about the objectives and interventional processes of the study and signed a consent form. The collected data were anonymized.
Test specimen preparation
To mimic the bracket/teeth boundary, the test specimens consisted of standard bracket material cylinders on top of a hydroxyapatite disc (Figs. 1a and 2). The cylinders were provided by FORESTADENT® -Bernhard Förster GmbH (Pforzheim, Germany) and had a diameter of 3.5 mm and a height of 1.7 mm.
a Schematic representation of the test specimen setup with the investigated pH levels at the biofilm–hydroxyapatite bracket material interface. b Scanning electron microscopy images of the hydroxyapatite disc at different magnifications: scale bars corresponding to b 200 µm, c 20 µm
a Schematische Darstellung des Probekörperaufbaues mit Kenntlichmachung der untersuchten Ebenen zur Bestimmung des pH-Wertes an der Biofilm-Hydroxylapatit-Bracketmaterial-Grenzfläche. b Rasterelektronenmikroskopische Aufnahme des Hydroxylapatit-Probekörpers bei unterschiedlichen Vergrößerungen: „scale bars“ entsprechend b 200 µm, c 20 µm
a Occlusal splint design: Occlusal splints with fixed specimens in the molar and premolar region on both the buccal and palatal sides of the first and second quadrants on a plaster model and c examined positions of the fixed specimen consisting of a hydroxyapatite specimen with bonded bracket-material. b, d Intraoral photos of the integrated occlusal splint (b occlusal view, d front view)
a Konstruktion der Okklusionsschiene: Okklusionsschienen mit im Prämolaren- und Molarenbereich sowohl palatinal als auch vestibulär in den ersten und zweiten Quadranten befestigten Probekörpern auf einem Gipsmodell und c untersuchte Positionen der befestigten Probekörper, bestehend aus einem mit Bracketmaterial bestückten Hydroxylapatit-Probekörper. b, d Intraorale Ansichten der eingesetzten Okklusionsschiene (b okklusale Ansicht, d frontale Ansicht)
The hydroxyapatite discs were custom-made from hydroxyapatite powder with a particle size of 10 µm (Sigma–Aldrich, St. Louis, MO USA). The powder was processed to a mash with modelling liquid (VITA Zahnfabrik H. Rauter GmbH & Co. KG, Bad Säckingen, Germany) and filled into a silicon template of the required disc shape. Using a vacuum pump, the liquid was withdrawn through an ash-free filter (Rotilabo® round filter, Typ 13A, Carl Roth GmbH & Co. KG, Karlsruhe, Germany). The resulting filter cake was then sintered in a sintering furnace (sintering process: in 15 min up to 95 °C, maintain this temperature for 1 h, in 3 h up to 1500 °C, maintain this temperature for 2 h, in 2 h down to 1000 °C, maintain this temperature for 1 h and in 5 h down to 40 °C). The resulting hydroxyapatite discs had a diameter of 6 mm and a height of 1.5 mm. To test for basic biocompatibility, normal adhesion and growth of human fibroblasts on the discs was verified microscopically in preliminary experiments. The bracket cylinders were bonded directly on the hydroxyapatite discs with light cure adhesive paste (Transbond™ XT, 3M Unitek, Neuss, Germany), without prior etching with phosphoric acid to avoid impact of the hydroxyapatite surface quality.
Splint design and in situ examination period
An upper jaw impression of every participant was taken with alginate (Alginoplast®, Kulzer GmbH, Hanau, Germany) and a plaster model was subsequently produced (SHERAALPIN gelb, Hartgips Typ 3, DIN EN 6873, Shera Werkstoff-Technologie GmbH & Co. KG, Lemförde, Germany). A thermoplastic deep drawing procedure (Erkodur, Erkodent® Erich Kopp GmbH, Pfalzgrafenweiler, Germany) was used to manufacture the occlusal splints.
The test specimens were placed buccally and palatally in the premolar and molar region in the first and second quadrants with flowable composite (Tetric EvoFlow A2, Ivoclar Vivadent AG, Schaan, Lichtenstein) on the occlusal splints (Fig. 2). In order to improve the adhesive bond, the desired areas were sandblasted with aluminum oxide (150 µm) beforehand (Sheraaluminiumoxid, SHERA Werkstoff-Technologie GmbH & Co. KG, Lemförde, Germany).
The specimen-equipped splints were worn in situ for 48 h by the participants. During this time, oral hygiene was suspended. The splints could only be removed for eating (stored in humid environment), but not longer than 40 min. After the examination period, the specimens were carefully removed from the splint without damaging the integrity of the biofilm and placed in phosphate-buffered saline (PBS, Sigma–Aldrich). The specimens were assigned to either a pH group or a live/dead staining group, based on predefined block randomization to exclude effects of the oral quadrant or the specific location.
Live/dead fluorescence staining and biofilm volume quantification
In situ grown biofilms were fluorescent labeled using the LIVE/DEADTM BacLight™ Bacterial Viability Kit (Thermo Fisher Scientific, Braunschweig, Germany). The fluorescent dyes Syto9® and propidium iodide were simultaneously applied as 1:4000 dilution in PBS according to the manufacturer’s recommendations. Specimens were fixed with 2.5% glutaraldehyde (Carl Roth GmbH + Co. KG) and placed in PBS for microscopy. Using the TCS SP8 confocal laser-scanning microscope (CLSM, Leica Microsystems GmbH, Wetzlar, Germany) three-dimensional images with a 400× magnification and a z-step-size of 5 µm were taken at four defined positions per specimen (Fig. 2c). The laser lines 488 nm and 552 nm as well as emission spectra of 500–550 nm and 650–750 nm were used to detect Syto9 and propidium iodide, respectively. The Imaris software package (Imaris 8.4, Bitplane AG, Zurich, Switzerland) was used to quantify biofilm volume and live/dead distribution.
Microscopic biofilm pH analysis
Analysis of the biofilm pH was based on the protocol by Schlafer and Dige [57] using a pH-sensitive ratiometric dye. The biofilm covered specimens were immersed in 50 mM HEPES buffer pH 7.0 (Thermo Fisher Scientific) containing 7.5 µM SNARF®-4F 5‑(and-6)-carboxylic acid (Thermo Fisher Scientific) and 0.4% glucose (Carl Roth GmbH & Co. KG) and incubated for 45 min in 5% CO2 at 37 °C. Subsequently, fluorescence was recorded by CLSM (TCS SP8, Leica Microsystems GmbH) using a 488 nm laser line and detecting emission at 485–490 nm (surface reflection), 576–608 nm (green proportion), and 629–661 nm (red proportion). Three-dimensional images with 20 steps were taken at four defined positions on the specimens (Fig. 2c) at a magnification of 400×. To quantify the green/red ratio in different biofilm layers, tagged image file format (TIFF) files of four levels per position were exported using the Leica LAS X Core software (Leica Microsystems GmbH). Level 1 was defined as bottom layer with maximum surface reflection and level 4 as top layer of the biofilm. Levels 2 and 3 were evenly distributed in between (Fig. 1a). The software daime (digital image analysis in microbial ecology; University of Vienna, Vienna, Austria) [13] was used to delete bacterial and cellular biomass from the images. For every level, the green/red ratio of the remaining biofilm matrix was calculated with the ImageJ software (ImageJ 1.53e, Wayne Rasband, National Institutes of Health, Bethesda, MD, USA, http://imagej.nih.gov/ij/) according to the protocol by Schlafer and Dige [57].
To link green/red ratios to pH values a calibration experiment was performed. SNARF® (7.5 µM) was added to HEPES buffer with pH values ranging from 4.0 to 8.0 in steps of 0.2. Five images were taken per pH value by CLSM and processes as described above. Calibration was done using the GraphPad Prism software 8.4 (GraphPad Software, Inc., La Jolla, CA, USA) by interpolating a sigmoidal, 4PL, standard curve with logarithmic x‑axis.
Statistical analysis
Sensitivity analysis of the experimental design was done using G*Power software 3.1.9.7 [20] for one-way analysis of variance (AVOVA) fixed effects, with the given total sample size of 48 (respectively 44) distributed in two groups, α = 0.05 and a statistical power of 0.8. Statistical comparison of biofilm morphology and pH was carried out with the GraphPad Prism software 8.4. Position effect of specimens on each splint did not have to be taken into account due to block randomization. Position effect within each specimen (Fig. 2c) was assessed by two-way ANOVA (biofilm volume and live/dead distribution) or by restricted maximum limitation (REML) mixed-effects model (pH) with Bonferroni’s multiple comparison correction. As the effect could be excluded, values for all positions on one specimen were averaged and used for further analysis. D’Agostino & Pearson omnibus test was performed to assess normal distribution of biofilm volume and live/dead distribution. Subsequently, Wilcoxon matched-pairs signed rank test was used to test for significant differences between palatal and buccal samples. To test for significant differences in pH values between palatal and buccal samples as well as between the different levels within one sample, REML mixed-effects model with Bonferroni’s multiple comparison correction was used. For all analyses, significance level was set to α = 0.05.
Results
To analyze bacterial biofilm pH at the orthodontic bracket/tooth interface, test specimens consisting of cylindric bracket material on a hydroxyapatite disc were exposed in the upper jaw of 12 participants. To verify healthy oral conditions, initial periodontal screening was performed and revealed the following: PD of 1.5 ± 0.12 mm, SBI of 1 ± 0.02%, and API of 10.64 ± 0.03%. After 48 h of in situ biofilm growth, test specimen of 11/12 subjects (one subject withdrew from the study due to an acute temporomandibular disorder [TMD]) could be included in the study and were stained and analyzed by CLSM. With this experimental design, effects with an effect size >0.4 could be detected ensuring a statistical power of 0.8.
Half of the specimens were analyzed for biofilm volume and live/dead distribution at the bracket/hydroxyapatite disc interface. Representative reconstructions of the biofilms are shown in Fig. 3a, b. They exhibited three-dimensional morphology and consisted of bacterial as well as human cells. As a specific position effect (Fig. 2c) could be excluded by statistical analysis, average values for buccally and palatally exposed specimens were compared. The average buccal biofilm volume was 8.79 × 105 ± 3.31 × 105 μm3 and the average palatal biofilm volume was 8.32 × 105 ± 2.73 × 105 μm3 (Fig. 3c). No statistically significant difference could be detected. The live/dead distribution was also almost similar between buccally and palatally exposed specimens with approximately 54% living and 45% dead cells (Fig. 3d).
a Three-dimensional (3D) image reconstructions of confocal laser scanning microscopy (CLSM) data; magnification 400×. Scale bars: 50 µm. a buccal b palatal. Quantification of biofilm formation. Box-plot diagram of c biofilm volume and d live/dead distribution
a Dreidimensionale Bildrekonstruktionen der durch CLSM (konfokale Laserscanningmikroskopie) gewonnenen Daten, Vergr. 400:1. „Scale bars“: 50 µm, a vestibulär b palatinal. Quantifizierung der Biofilmbildung c Box-Plot-Diagramm des Biofilmvolumens und d der Lebend/tot-Verteilung
The other specimens were analyzed for pH values at different biofilm layers (Fig. 1a). For each position on the specimen (Fig. 2c), three-dimensional images of the biofilm were taken. From these images, four levels were selected for pH analysis (Fig. 4a). Level 1 was defined as bottom layer and level 4 as top layer of the biofilm. Level 2 and 3 were evenly distributed in between. As for biofilm volume a position specific effect (Fig. 2c) of the pH value could be excluded by statistical analysis, average values per level were calculated (Fig. 4b).
a Biofilm pH imaging of confocal laser scanning microscopy (CLSM); magnification 400×. b Box-plot diagram of pH values in different layers of the biofilms
a pH-Wert Darstellungen innerhalb des Biofilmes mittels CLSM (konfokale Laserscanningmikroskopie), Vergr. 400:1. b Box-Plot-Diagramm der pH-Werte in den verschiedenen Ebenen der Biofilme
For buccally exposed specimens, the pH value steadily increased from pH 6.46 at the bottom layer (level 1) to pH 6.89 at the top layer (level 4). In contrast, for palatally exposed specimens, the pH was 6.40 at the bottom layer, increased up to pH 6.74 at level 3 and slightly reduced to pH 6.68 at level 4.
For biofilms grown on both oral positions, the pH value at the bottom layer was significantly lower compared to all other layers. When comparing both bottom layers (1 and 2) between buccal and palatal specimens, no differences could be detected. In contrast, the pH values of the top layers (3 and 4) were significantly lower palatally than buccally.
Discussion
Common complications of orthodontic treatment are local demineralizations of the enamel that could lead to the formation of white spot lesions (WSL) and caries. They are caused by acid production of increased amounts of dental plaque around the brackets, due to inadequate oral hygiene during orthodontic treatment [7, 8, 59]. Interestingly, it has been shown that biofilm growth depends on intraoral location [5, 58]. In line with this, WSL showed a decreased clinical prevalence for lingual brackets [66, 69]. Therefore, the hypothesis of this study was that there is a difference in initial intraoral biofilm formation on buccally and palatally bonded brackets, resulting in different acidification. To address this hypothesis, this study quantified volume, live/dead distribution and pH value of initial biofilms formed on buccally and palatally exposed test specimens in the upper jaw of volunteers.
Prior to the study, healthy periodontal conditions of each participant were assured by an initial periodontal screening including probing depths (PD), modified sulcus bleeding index (SBI), and modified approximal plaque index (API) [28]. All values were within the normal range. Further risk factors influencing oral microflora, such as general diseases, antibiotic treatment 6 weeks before participation, alcohol consumption, smoking or pregnancy were also excluded [3, 9, 12, 24, 31, 49, 52, 55]. The selected sample size was set to 12 participants with specimens for each analysis in duplicates, which corresponds to studies with a similar study design and allows for the detection of large effect sizes >0.4 [4, 5, 27, 44, 61]. As the clinically observed lingual and buccal WSL formation upon orthodontic treatment differs by more than 60% [59], this experimental setup was considered sufficient. For biofilm collection, individual occlusal splints of the upper jaw were equipped with test specimens. The test specimens were placed buccally and palatally in the premolar and molar region in the first and second quadrants. This ensured an increased wearing comfort compared to the lower jaw and no impairment of aesthetics and phonetics for this initial study, but needs to be taken into account when evaluating the data. To avoid additional oral position-specific effects [4, 5], specimens were block-wise randomly assigned to the different evaluation groups. Instead of real brackets with geometries varying between different companies and especially between lingual and buccal appliances, uniform cylindric shaped bracket material was used. This ensures a higher reproducibility and comparability between the different positions. The test specimens were also not directly fixed to the splints, but to discs made of pure hydroxyapatite. This mineral is the main component of human enamel [15, 50] and the discs, thus, could be considered biomimetic alloplastic. The advantages of this construction are that it provided a standardized and uniform shape according to the desired dimensions, allowed for the analysis of the bracket/tooth interface, but avoided the use of allogeneic [35, 64, 67, 70] or xenogeneic material [2, 25, 33, 62]. This reduced ethical concerns regarding the study and increased participants acceptance. The decision not to use shielding in the area of biofilm collection—as was done in previous studies [16, 44, 63]—was based on the idea of simulating clinical reality as precisely as possible, i.e., allowing shear forces of the tongue and cheeks. Taken together, this splint design ensured almost natural biofilm formation that was close to the clinical orthodontic situation and, thus, can serve as the basis for further studies.
The splints were worn for 48 h by the participants. This time was set as other studies have demonstrated that it was appropriate for in situ biofilm growth [4, 5, 27, 35, 44, 51, 61, 64]. Due to the fact that oral hygiene was suspended, accumulation of biofilm formation was increased but it still should be considered as an initial biofilm. Even if the study design was not directly comparable with multiyear orthodontic treatment, it was sufficient for an initial study. However, it would be important for future studies to analyze the obtaining findings over the entire period of orthodontic treatment.
For the final analysis, half of the specimens were live/dead fluorescent stained and CLSM was used to quantify biofilm volume and live/dead distribution at the bracket/hydroxyapatite disc interface. This method is well established and allows for biofilm quantification with almost native morphology [17, 22, 29, 45, 60].
The detected biofilm consisted of bacterial and also human cells. These cells were most likely human gingival epithelial cells that are integrated into the biofilm through bacterial colonization, as has been demonstrated in various studies [16, 44, 63].
Compared to other studies, the biofilm volume was low in this study [16, 44]. This is most probably due to a different splint design in which the specimens were exposed to the natural conditions of the oral cavity, including shear forces by cheek and tongue, and were not protected by shield-like structures. However, the live/dead distribution was almost similar [44, 62].
When comparing the biofilms formed buccally and palatally, interestingly no statistically significant differences in volume or the live/dead distribution in this initial intraoral biofilm could be detected. This is in contrast to the study of Auschill et al. [5], which revealed a lower palatal biofilm thickness compared to the examined buccal locations. However, in their study the specimens were differently positioned buccally and palatally. Unlike the buccal specimens, the palatal specimens were placed in the area of the palatal mucosa at a greater distance from the teeth and the dental plaque. Other studies, which did not include palatal or lingual specimens, have shown similar vitality patterns at different locations on the buccal side of the upper and the lower jaw [4]. Taken together, there might be differences in biofilm formation capability at different locations in the oral cavity. However, for bracket-like specimens placed buccally and palatally in the upper jaw, the biofilm formed within the initial period seemed to be similar regarding its general morphology.
To gain deeper insight into acidification properties of biofilms, an analysis of the biofilm pH was carried out with a pH-sensitive ratiometric dye, followed by CLSM and digital image analysis software based on the protocol by Schlafer and Dige [57]. This quantitative fluorescence microscopic examination enables the determination of vertical and horizontal pH gradients in microscopic images without changing the biofilm mechanically, for example, with microelectrodes [57]. The pH was analyzed in different layers of the biofilm, due to the fact that the distribution of nutrients and metabolites in the biofilm is not even [57]. The heterogeneous biofilm has diffusion-modifying properties that cause chemical/nutrient gradients, which lead to microenvironments within the biofilm. Thereby, niches with different pathogenic potentials, such as pH, redox, and nutrient availability can develop [10, 23].
In line with this, in both oral positions the lowest pH value could be detected at the bottom layer. Buccally as well as palatally, the pH dropped likewise from 7.0 to approximately 6.45. The exact value strongly depends on the incubation conditions and the biofilm maturation state. The biofilm in this study was comparable young and incubated only for 45 min and with 0.4% glucose as sole nutrient source. This is most probably the reason for the likewise small drop in pH. An increase in specimen exposure time in the oral cavity, incubation time in glucose solution or additional nutrients available would most probably result in different outcomes. An increased biofilm volume and metabolism would lead to an increase in acid metabolic products that in turn would cause lower pH values, reaching the critical pH value for tooth enamel demineralization [1, 56]. Even though the biofilms in both oral positions showed similar pH values at the bottom layer, statistically significant differences could be observed between the pH values in the top layers 3 and 4. The biofilm grown on palatally exposed specimens showed a lower pH value than that grown buccally, which indicates stronger acidification by the bacteria present. With regard to the aforementioned results, this could not be due to greater palatal biofilm volume or higher viability. Most probably, the buffering effect of saliva from the parotid gland was responsible for the lower acidification buccally [42]. The excretory duct of the parotid gland enters the oral cavity opposite the second upper molar [38] and, thus, in closer proximity to the buccally placed specimens than to the palatal ones. A repetition of this study in the lower jaw could confirm the influence of salivary flow due to the different anatomical conditions. The excretory ducts of the sublingual gland are located close to the incisors and could potentially create a buffering effect that could lead to lower pH values buccally compared to lingually. Other studies have shown that WSL more frequently occurred in the maxillary than in the mandible arch [32, 34]. Gorelick et al. observed that WSL did not occur even after prolonged use of mandibular canine-to-canine bonded retainer and suggested salivary flow as a possible cause [26].
Another reason to consider for the lower acidification detected on the buccal side could be a different bacterial composition between the biofilms of the two oral positions. A consequence of different bacterial composition could be different metabolic activities and products and, thus, to differences in acidification [56]. To address this in more detail, future approaches should quantify bacterial metabolic activity buccally and palatally and identify specific species composition by genomic sequencing.
Regarding the initial hypothesis, it could be shown that the initial oral biofilms form similarly on bracket-like specimens if exposed buccally or palatally in the upper jaw. At both oral positions, the lowest pH value could be detected at the bottom layer of the biofilm, accordingly at the bracket/tooth interface. However, differences were determined at higher levels of the biofilm, which might be due to the specific position in the oral cavity. Further studies should address whether these observations can be confirmed also in the lower jaw with different anatomic properties and, most importantly, over longer periods of time close to the duration of orthodontic treatment. Changing the duration of the specimens in the oral cavity would most likely also result in different, lower pH values that would reach the critical pH for enamel demineralization [1, 56]. Another possibility to study especially the biofilm pH-caused demineralization in more detail would be to use the splint design of this study with bovine enamel instead of hydroxyapatite discs. Here, demineralization could be examined directly using digital transverse microradiography (TMR), a highly appropriate method for validating mineral losses [14]. Furthermore, previous etching of enamel, which is routinely done to increase surface energy, surface area, and porosity for efficient bracket adhesion [6, 11], could influence biofilm accumulation and should be considered in further studies. For example, Knösel et al. have shown that surplus etching of the entire labial surface results in a higher likelihood of developing WSL [37]. Therefore, the design and setup of this study could serve as a blueprint for multiple further analyses to examine pH development at the tooth–bracket interface in more detail.
Regarding site specific effects of demineralization, within the limitations of this study, there is no evidence for an intrinsic reduced biofilm formation capability at the palatal position. Therefore, further factors should also be considered for the clinically observed reduced WSL prevalence in lingual orthodontic treatment. For example, due to the custom-made manufacturing process [68], lingual brackets have a different geometry and the advantage of fitting precisely on the tooth surface [66]. In addition, they have a large base, which almost covers the entire lingual/palatal surface, thereby creating an inherent seal [66]. The specific effect of bracket geometry could be analyzed in further studies.
Conclusion
In this study, a successful comparison between initial biofilm formation on palatally and buccally placed bracket-like material in the upper jaw with regard to acidification, biofilm volume, and live/dead distribution could be achieved. It could be shown that there were no differences in the general biofilm morphology regarding volume and viability. Interestingly, in biofilms from both positions a similarly decreased pH value at the deeper layers of the biofilm could be detected. Towards the top layers of the biofilms, the pH value increased at both positions. Only for palatally exposed specimens did the pH value slightly decrease from level 3 to level 4. Overall, a gradient from low pH values at the bottom layer to higher pH values at the top layer was discernible. Based on the results of this study, initial biofilm formation and acidification is similar on buccally and palatally placed bracket material in the upper jaw. As lingual brackets exhibit reduced WSL formation clinically, future studies should investigate further factors like bracket geometry.
References
Agnello M, Cen L, Tran NC, Shi W, McLean JS, He X (2017) Arginine improves pH homeostasis via metabolism and microbiome modulation. J Dent Res 96:924–930. https://doi.org/10.1177/0022034517707512
Al-Ahmad A, Follo M, Selzer AC, Hellwig E, Hannig M, Hannig C (2009) Bacterial colonization of enamel in situ investigated using fluorescence in situ hybridization. J Med Microbiol 58:1359–1366. https://doi.org/10.1099/jmm.0.011213-0
Amir M, Brown JA, Rager SL, Sanidad KZ, Ananthanarayanan A, Zeng MY (2020) Maternal microbiome and infections in pregnancy. Microorganisms. https://doi.org/10.3390/microorganisms8121996
Arweiler NB, Hellwig E, Sculean A, Hein N, Auschill TM (2004) Individual vitality pattern of in situ dental biofilms at different locations in the oral cavity. Caries Res 38:442–447. https://doi.org/10.1159/000079625
Auschill T, Hellwig E, Sculean A, Hein N, Arweiler N (2004) Impact of the intraoral location on the rate of biofilm growth. Clin Oral Invest 8:97–101. https://doi.org/10.1007/s00784-004-0255-6
Beech DR, Jalaly T (1980) Bonding of polymers to enamel: influence of deposits formed during etching, etching time and period of water immersion. J Dent Res 59:1156–1162
Beerens MW, Boekitwetan F, van der Veen MH, ten Cate JM (2014) White spot lesions after orthodontic treatment assessed by clinical photographs and by quantitative light-induced fluorescence imaging; a retrospective study. Acta Odontol Scand 73:441–446. https://doi.org/10.3109/00016357.2014.980846
Bishara SE, Ostby AW (2008) White spot lesions: formation, prevention, and treatment. Semin Orthod 14:174–182. https://doi.org/10.1053/j.sodo.2008.03.002
Borgo PV, Rodrigues VA, Feitosa AC, Xavier KC, Avila-Campos MJ (2014) Association between periodontal condition and subgingival microbiota in women during pregnancy: a longitudinal study. J Appl Oral Sci 22:528–533. https://doi.org/10.1590/1678-775720140164
Bowen WH, Burne RA, Wu H, Koo H (2018) Oral biofilms: pathogens, matrix, and polymicrobial interactions in microenvironments. Trends Microbiol 26:229–242. https://doi.org/10.1016/j.tim.2017.09.008
Cerci BB, Roman LS, Guariza-Filho O, Camargo ES, Tanaka OM (2012) Dental enamel roughness with different acid etching times: atomic force microscopy study. Eur J Gen Dent 1:187–191
Coretti L, Cuomo M, Florio E, Palumbo D, Keller S, Pero R, Chiariotti L, Lembo F, Cafiero C (2017) Subgingival dysbiosis in smoker and nonsmoker patients with chronic periodontitis. Mol Med Rep 15:2007–2014. https://doi.org/10.3892/mmr.2017.6269
Daims H, Lucker S, Wagner M (2006) Daime, a novel image analysis program for microbial ecology and biofilm research. Environ Microbiol 8:200–213
Darling CL, Le CQ, Featherstone JDB, Fried D (2009) An automated digital microradiography system for assessing tooth demineralization. Proc SPIE Int Soc Opt Eng. https://doi.org/10.1117/12.816868
Dawes C, Pedersen AM, Villa A, Ekstrom J, Proctor GB, Vissink A, Aframian D, McGowan R, Aliko A, Narayana N, Sia YW, Joshi RK, Jensen SB, Kerr AR, Wolff A (2015) The functions of human saliva: a review sponsored by the world workshop on oral medicine VI. Arch Oral Biol 60:863–874. https://doi.org/10.1016/j.archoralbio.2015.03.004
Desch A, Freifrau von Maltzahn N, Stumpp N, Dalton M, Yang I, Stiesch M (2020) Biofilm formation on zirconia and titanium over time—an in vivo model study. Clin Oral Implants Res 31:865–880. https://doi.org/10.1111/clr.13632
Doll K, Jongsthaphongpun KL, Stumpp NS, Winkel A, Stiesch M (2016) Quantifying implant-associated biofilms: comparison of microscopic, microbiologic and biochemical methods. J Microbiol Methods 130:61–68
Donlan RM, Costerton JW (2002) Biofilms: survival mechanisms of clinically relevant microorganisms. Clin Microbiol Rev 15:167–193. https://doi.org/10.1128/CMR.15.2.167-193.2002
Enaia M, Bock N, Ruf S (2011) White-spot lesions during multibracket appliance treatment: a challenge for clinical excellence. Am J Orthod Dentofacial Orthop 140:17. https://doi.org/10.1016/j.ajodo.2010.12.016
Faul F, Erdfelder E, Lang A, Buchner A (2007) G* power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res 39:175–191
Fejerskov O (1997) Concepts of dental caries and their consequences for understanding the disease. Community Dent Oral Epidemiol 25:5–12. https://doi.org/10.1111/j.1600-0528.1997.tb00894.x
Flach N, Bottcher DE, Parolo CC, Firmino LB, Malt M, Lammers ML, Grecca FS (2016) Confocal microscopy evaluation of the effect of irrigants on enterococcus faecalis biofilm: an in vitro study. Scanning 38:57–62. https://doi.org/10.1002/sca.21241
Flemming HC, Wingender J, Szewzyk U, Steinberg P, Rice SA, Kjelleberg S (2016) Biofilms: an emergent form of bacterial life. Nat Rev Microbiol 14:563–575. https://doi.org/10.1038/nrmicro.2016.94
Freitag-Wolf S, Munz M, Wiehe R, Junge O, Graetz C, Jockel-Schneider Y, Staufenbiel I, Bruckmann C, Lieb W, Franke A, Loos BG, Jepsen S, Dommisch H, Schaefer AS (2019) Smoking modifies the genetic risk for early-onset periodontitis. J Dent Res 98:1332–1339. https://doi.org/10.1177/0022034519875443
Giertsen E, Guggenheim B, Thurnheer T, Gmur R (2000) Microbiological aspects of an in situ model to study effects of antimicrobial agents on dental plaque ecology. Eur J Oral Sci 108:403–411. https://doi.org/10.1034/j.1600-0722.2000.108005403.x
Gorelick L, Geiger AM, Gwinnett AJ (1982) Incidence of white spot formation after bonding and banding. Am J Orthod 81:93–98. https://doi.org/10.1016/0002-9416(82)90032-x
Gu H, Fan D, Gao J, Zou W, Peng Z, Zhao Z, Ling J, LeGeros RZ (2012) Effect of ZnCl2 on plaque growth and biofilm vitality. Arch Oral Biol 57:369–375. https://doi.org/10.1016/j.archoralbio.2011.10.001
Hellwig E, Klimek J, Attin T (2013) Einführung in die Zahnerhaltung. Dt. Zahnärzte-Verl, Köln
Hohscheidt GL, Bottcher DE, Fatturi Parolo CC, Montagner F, Grecca FS (2013) Response of E. faecalis biofilms to different associations of auxiliary substances during root canal preparation: a confocal laser microscopy analysis. Microsc Res Tech 76:658–662. https://doi.org/10.1002/jemt.22215
Hojo K, Nagaoka S, Ohshima T, Maeda N (2009) Bacterial interactions in dental biofilm development. J Dent Res 88:982–990. https://doi.org/10.1177/0022034509346811
Jiang Y, Zhou X, Cheng L, Li M (2020) The impact of smoking on subgingival microflora: from periodontal health to disease. Front Microbiol 11:66. https://doi.org/10.3389/fmicb.2020.00066
Julien KC, Buschang PH, Campbell PM (2013) Prevalence of white spot lesion formation during orthodontic treatment. Angle Orthod 83:641–647. https://doi.org/10.2319/071712-584.1
Jung DJ, Al-Ahmad A, Follo M, Spitzmuller B, Hoth-Hannig W, Hannig M, Hannig C (2010) Visualization of initial bacterial colonization on dentine and enamel in situ. J Microbiol Methods 81:166–174. https://doi.org/10.1016/j.mimet.2010.03.002
Khalaf K (2014) Factors affecting the formation, severity and location of white spot lesions during orthodontic treatment with fixed appliances. J Oral Maxillofac Res 5:e4. https://doi.org/10.5037/jomr.2014.5104
Klug B, Santigli E, Westendorf C, Tangl S, Wimmer G, Grube M (2016) From mouth to model: combining in vivo and in vitro oral biofilm growth. Front Microbiol 7:1448. https://doi.org/10.3389/fmicb.2016.01448
Knösel M, Klang E, Helms H, Wiechmann D (2016) Occurrence and severity of enamel decalcification adjacent to bracket bases and sub-bracket lesions during orthodontic treatment with two different lingual appliances. Eur J Orthod 38:485–492. https://doi.org/10.1093/ejo/cjv069
Knösel M, Bojes M, Jung K, Ziebolz D (2012) Increased susceptibility for white spot lesions by surplus orthodontic etching exceeding bracket base area. Am J Orthod Dentofac Orthop 141:574–582. https://doi.org/10.1016/j.ajodo.2011.11.017
Kochhar A, Larian B, Azizzadeh B (2016) Facial nerve and parotid gland anatomy. Otolaryngol Clin North Am 49:273–284. https://doi.org/10.1016/j.otc.2015.10.002
Kolenbrander PE, Andersen RN, Blehert DS, Egland PG, Foster JS, Palmer RJ (2002) Communication among oral bacteria. Microbiol Mol Biol Rev 66:486–505. https://doi.org/10.1128/mmbr.66.3.486-505.2002
Lucchese A, Gherlone E (2012) Prevalence of white-spot lesions before and during orthodontic treatment with fixed appliances. Eur J Orthod 35:664–668. https://doi.org/10.1093/ejo/cjs070
Machiulskiene V, Campus G, Carvalho JC, Dige I, Ekstrand KR, Jablonski-Momeni A, Maltz M, Manton DJ, Martignon S, Martinez-Mier EA, Pitts NB, Schulte AG, Splieth CH, Tenuta LMA, Ferreira Zandona A, Nyvad B (2020) Terminology of dental caries and dental caries management: consensus report of a workshop organized by ORCA and cariology research group of IADR. Caries Res 54:7–14. https://doi.org/10.1159/000503309
Marsh PD, Do T, Beighton D, Devine DA (2016) Influence of saliva on the oral microbiota. Periodontol 2000 70:80–92. https://doi.org/10.1111/prd.12098
Marsh PD (2003) Are dental diseases examples of ecological catastrophes? Microbiology 149:279–294. https://doi.org/10.1099/mic.0.26082-0
Meyer-Kobbe V, Doll K, Stiesch M, Schwestka-Polly R, Demling A (2018) Comparison of intraoral biofilm reduction on silver-coated and silver ion-implanted stainless steel bracket material. J Orofac Orthop 80:32–43. https://doi.org/10.1007/s00056-018-00165-3
Netuschil L, Reich E, Unteregger G, Sculean A, Brecx M (1998) A pilot study of confocal laser scanning microscopy for the assessment of undisturbed dental plaque vitality and topography. Arch Oral Biol 43:277–285. https://doi.org/10.1016/S0003-9969(97)00121-0
Ogaard B, Rolla G, Arends J (1988) Orthodontic appliances and enamel demineralization. part 1. lesion development. Am J Orthod Dentofacial Orthop 94:68–73
O’Reilly MM, Featherstone JD (1987) Demineralization and remineralization around orthodontic appliances: an in vivo study. Am J Orthod Dentofacial Orthop 92:33–40
Pitts NB, Zero DT, Marsh PD, Ekstrand K, Weintraub JA, Ramos-Gomez F, Tagami J, Twetman S, Tsakos G, Ismail A (2017) Dental caries. Nat Rev Dis Primers 3:17030. https://doi.org/10.1038/nrdp.2017.30
Pulikkotil SJ, Nath S et al (2020) Alcohol consumption is associated with periodontitis. A systematic review and meta-analysis of observational studies. Community Dent Health 37:12–21. https://doi.org/10.1922/CDH_4569Pulikkotil10
Qamar Z, Haji Abdul Rahim ZB, Chew HP, Fatima T (2017) Influence of trace elements on dental enamel properties: a review. J Pak Med Assoc 67:116–120
Quintas V, Prada-Lopez I, Carreira MJ, Suarez-Quintanilla D, Balsa-Castro C, Tomas I (2017) In situ antibacterial activity of essential oils with and without alcohol on oral biofilm: a randomized clinical trial. Front Microbiol 8:2162. https://doi.org/10.3389/fmicb.2017.02162
Reichert S, Schlitt A, Beschow V, Lutze A, Lischewski S, Seifert T, Dudakliewa T, Gawe R, Werdan K, Hofmann B, Schaller HG, Schulz S (2015) Use of floss/interdental brushes is associated with lower risk for new cardiovascular events among patients with coronary heart disease. J Periodontal Res 50:180–188. https://doi.org/10.1111/jre.12191
Richter AE, Arruda AO, Peters MC, Sohn W (2011) Incidence of caries lesions among patients treated with comprehensive orthodontics. Am J Orthod Dentofacial Orthop 139:657–664. https://doi.org/10.1016/j.ajodo.2009.06.037
Rogers JD, Palmer J et al (2001) Role of streptococcus gordonii amylase-binding protein A in adhesion to hydroxyapatite, starch metabolism, and biofilm formation. Infect Immun 69:7046–7056. https://doi.org/10.1128/IAI.69.11.7046-7056.2001
Saffi MA, Furtado MV, Montenegro MM, Ribeiro IW, Kampits C, Rabelo-Silva ER, Polanczyk CA, Rosing CK, Haas AN (2013) The effect of periodontal therapy on C‑reactive protein, endothelial function, lipids and proinflammatory biomarkers in patients with stable coronary artery disease: Study protocol for a randomized controlled trial. Trials 14:283–283. https://doi.org/10.1186/1745-6215-14-283
Schachtele CF, Jensen ME (1982) Comparison of methods for monitoring changes in the pH of human dental plaque. J Dent Res 61:1117–1125. https://doi.org/10.1177/00220345820610100201
Schlafer S, Dige I (2016) Ratiometric imaging of extracellular pH in dental biofilms. J Vis Exp. https://doi.org/10.3791/53622
Segata N, Haake SK, Mannon P, Lemon KP, Waldron L, Gevers D, Huttenhower C, Izard J (2012) Composition of the adult digestive tract bacterial microbiome based on seven mouth surfaces, tonsils, throat and stool samples. Genome Biol 13:R42. https://doi.org/10.1186/gb-2012-13-6-r42
Sundararaj D, Venkatachalapathy S, Tandon A, Pereira A (2015) Critical evaluation of incidence and prevalence of white spot lesions during fixed orthodontic appliance treatment: a meta-analysis. J Int Soc Prev Community Dent 5:433–439. https://doi.org/10.4103/2231-0762.167719
Takenaka S, Iwaku M, Hoshino E (2001) Artificial pseudomonas aeruginosa biofilms and confocal laser scanning microscopic analysis. J Infect Chemother 7:87–93. https://doi.org/10.1007/s101560100014
Tawakoli PN, Neu TR, Busck MM, Kuhlicke U, Schramm A, Attin T, Wiedemeier DB, Schlafer S (2017) Visualizing the dental biofilm matrix by means of fluorescence lectin-binding analysis. J Oral Microbiol 9:1345581. https://doi.org/10.1080/20002297.2017.1345581
Tawakoli PN, Al-Ahmad A, Hoth-Hannig W, Hannig M, Hannig C (2013) Comparison of different live/dead stainings for detection and quantification of adherent microorganisms in the initial oral biofilm. Clin Oral Investig 17:841–850. https://doi.org/10.1007/s00784-012-0792-3
Thurnheer T, Belibasakis GN, Bostanci N (2014) Colonisation of gingival epithelia by subgingival biofilms in vitro: role of “red complex” bacteria. Arch Oral Biol 59:977–986. https://doi.org/10.1016/j.archoralbio.2014.05.023
Tomas I, Prada-Lopez I, Quintas V, Carreira MJ, Simon-Soro A, Mira A, Balsa-Castro C (2018) In situ substrate-formed biofilms using IDODS mimic supragingival tooth-formed biofilms. J Oral Microbiol 10:1495975. https://doi.org/10.1080/20002297.2018.1495975
Tufekci E, Dixon JS, Gunsolley JC, Lindauer SJ (2011) Prevalence of white spot lesions during orthodontic treatment with fixed appliances. Angle Orthod 81:206–210. https://doi.org/10.2319/051710-262.1
Van Der Veen MH, Attin R, Schwestka-Polly R, Wiechmann D (2010) Caries outcomes after orthodontic treatment with fixed appliances: do lingual brackets make a difference? Eur J Oral Sci 118:298–303. https://doi.org/10.1111/j.1600-0722.2010.00733.x
von Ohle C, Gieseke A, Nistico L, Decker EM, DeBeer D, Stoodley P (2010) Real-time microsensor measurement of local metabolic activities in ex vivo dental biofilms exposed to sucrose and treated with chlorhexidine. Appl Environ Microbiol 76:2326–2334. https://doi.org/10.1128/AEM.02090-09
Wiechmann D, Rummel V, Thalheim A, Simon JS, Wiechmann L (2003) Customized brackets and archwires for lingual orthodontic treatment. Am J Orthod Dentofacial Orthop 124:593–599. https://doi.org/10.1016/j.ajodo.2003.08.008
Wiechmann D, Klang E, Helms H, Knösel M (2015) Lingual appliances reduce the incidence of white spot lesions during orthodontic multibracket treatment. Am J Orthod Dentofacial Orthop 148:414–422. https://doi.org/10.1016/j.ajodo.2015.05.015
Wood SR, Kirkham J, Marsh PD, Shore RC (2000) Architecture of intact natural human plaque biofilms studies by confocal laser scanning microscopy. J Dent Res 79:21
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
M.F. Loewe, K. Doll-Nikutta, M. Stiesch and R. Schwestka-Polly declare that they have no competing interests.
Ethical standards
The present study was approved by the ethical committee of the Hannover Medical School (amendment to ethic vote no. 8570_BO_S2019). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1975 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Equally contributing last authors: Meike Stiesch, Rainer Schwestka-Polly
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Loewe, M.F., Doll-Nikutta, K., Stiesch, M. et al. Biofilm volume and acidification within initial biofilms formed in situ on buccally and palatally exposed bracket material. J Orofac Orthop (2024). https://doi.org/10.1007/s00056-024-00515-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00056-024-00515-4
Keywords
- Dental plaque
- pH value
- Orthodontic bracket materials
- Confocal laser scanning microscopy
- White spot lesions