Abstract
Background
For patients with a maxillary transversal deficiency (MTD), various treatment options are available, partly based on the practitioner’s experience. This study aimed to determine a cut-off age for decision making between surgically assisted rapid palatal expansion (SARPE) over orthodontic rapid palatal expansion (ORPE) based on skeletal maturation in a female population.
Methods
A total of 100 cone beam computed tomography (CBCT) images of young females were analyzed on maturation of the pterygomaxillary (PMS), zygomaticomaxillary (ZMS), transpalatal (TPS), and midpalatal (MPS) sutures. Based on the maturation of these four junctions, four independent observers had to determine whether they would prefer ORPE or SARPE to widen the maxilla.
Results
For the PMS, the results show a closure of 83–100% from 13 to 17 years. As for the TPS, a closure of 78–85% was observed from 15 years of age. For the 15- to 17-year-old females, a closed ZMS was present in 32–47%. Regarding MPS, closed sutures presented in 61% (stages D and E) of the 15-year-old females. The cut-off age at which SARPE was recommended was 15.1 years for the orthodontist observers and 14.8 years for the maxillofacial surgeon observers.
Conclusions
Significant maturation of MPS was reached at the age of 15 in a female population. The PMS, TPS, MPS, and ZMS closed sequentially. A comprehensive diagnostic approach is necessary for choosing the appropriate treatment. When in doubt, age could assist decision making in a female population, with a cut-off age of 15 years in favor of SARPE based on this study.
Zusammenfassung
Hintergrund
Für Patienten mit einem transversalen Oberkieferdefizit (MTD) stehen verschiedene Behandlungsoptionen zur Verfügung, die zum Teil auf der Erfahrung des behandelnden Arztes beruhen. Ziel dieser Studie war es, ein Cut-off-Alter für die Entscheidung zwischen einer chirurgisch assistierten schnellen Gaumennahterweiterung (SARPE) und einer kieferorthopädischen schnellen Gaumennahterweiterung (ORPE) auf der Grundlage der skelettalen Reifung in einem weiblichen Kollektiv zu bestimmen.
Methoden
Insgesamt 100 DVT-Aufnahmen von Mädchen wurden hinsichtlich der Reifung der Sutura pterygomaxillaris (PMS), der Sutura zygomaticomaxillaris (ZMS), der Sutura palatina transversa (TPS) und der Sutura palatina mediana (MPS) analysiert. Anhand der Reifung dieser 4 Nahtstellen mussten 4 unabhängige Beobachter entscheiden, ob sie sich eher für eine ORPE oder für eine SARPE zur Oberkieferverbreiterung entscheiden würden.
Ergebnisse
Für die PMS zeigen die Ergebnisse einen Verschluss von 83–100% im Alter von 13–17 Jahren. Bei der TPS wurde ab einem Alter von 15 Jahren ein Verschluss von 78–85% beobachtet. Bei den 15- bis 17-jährigen Frauen lag eine geschlossene ZMS in 32–47% vor. Bei der MPS wurden bei 61% (Stadien D und E) der 15-jährigen Mädchen geschlossene Nähte festgestellt. Das Cut-off-Alter, ab dem eine SARPE empfohlen wurde, lag bei den kieferorthopädischen Beobachtern bei 15,1, bei den Mund-Kiefer-Gesichts-Chirurgen bei 14,8 Jahren.
Schlussfolgerungen
Eine signifikante Reifung der MPS wurde im Alter von 15 Jahren in einem weiblichen Kollektiv erreicht. PMS, TPS, MPS und ZMS schlossen sich aufeinanderfolgend. Für die Wahl der geeigneten Behandlung ist ein umfassender diagnostischer Ansatz erforderlich. Im Zweifelsfall könnte das Alter bei der Entscheidungsfindung in einem weiblichen Kollektiv hilfreich sein, wobei ein Grenzalter von 15 Jahren auf der Grundlage dieser Studie zugunsten einer SARPE ausfällt.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients with a maxillary transversal deficiency (MTD) typically present with crowded teeth, buccal corridors, narrowed dental arches, and uni- or bilateral crossbites. To improve the occlusion, maxillary expansion is necessary. Whether orthodontic or surgical maxillary widening is preferred depends on the presumed efficacy of expansion based on the timing of treatment and the practitioner’s experience and training [1].
Orthodontic rapid palatal expansion (ORPE), also known as rapid maxillary expansion (RME), is indicated for the treatment of transversal hypoplasia of the maxilla in young patients. For adolescents and skeletally mature patients, surgically assisted rapid palatal expansion (SARPE), also known as surgically assisted rapid maxillary expansion (SARME), is the gold standard because of the fusion of the sutures [2].
The current literature has a great overlap for the choice between the ORPE and SARPE procedures which prevents a clear cut-off. Depending on the source, the cut-off age recommended for starting SARPE procedures ranges from 14 to 25 years [3,4,5,6,7], while the cut-off age to stop with ORPE procedures ranges from 12 to 25 years [3,4,5,6,7]. Table 1 shows the cut-off for ORPE and SARPE extracted from different articles.
Most of these statements are based on earlier data derived from skeletal maturation on two-dimensional (2D) imaging and lower resolution techniques. Yet, nowadays, low-dose cone beam computed tomography (CBCT) imaging might help to assist the decision process for or against a surgical intervention. Angelieri et al. [8] suggested classification based on CBCT imaging for a patient-specific assessment before maxillary expansion, with a patient-specific decision based on the maturation of the midpalatal suture (MPS) [9]. Yet, some authors debate on the justified use of CBCT in young patients considering the increased radiation sensitivity of children [10].
In the literature, variable ways of research to determine the maturation of the MPS. Franchi et al. [11] used a CT to check the bone density in Hounsfield units (HU), while ultrasonography via a semi-quantitative bone fill score was used by Sumer et al. [12]. Kwak et al. [13] evaluated the correlation between fractal patterning and ossification of the palatal suture via CBCT in combination with the Angelieri classification. Melsen et al. [14] performed a combined histologic microradiographic study and showed that the transverse growth of the MPS continued up to the age of 16 but argued that interdigitation in adolescence is already so severe that separation of the two halves of the maxilla would not be possible without fracturing the interdigitated processes. They also suggested that the pterygomaxillary suture (PMS) is a possible hinge around which posterior rotation of the maxilla halves occurs as a result of an ORPE treatment [15].
Several studies demonstrated that chronological age is not a good indicator for choosing ORPE vs SARPE since palatal suture fusion is poorly correlated with patient age [16,17,18,19,20]. These studies were solely based on the maturation of the MPS. Isfeld et al. [21] pointed out in their systematic review that the maturity of other maxillary sutures has to be taken into account. Another paper checked the MPS, the zygomaticomaxillary suture (ZMS) and the internasal sutures in an ex vivo study after bone- or dental-borne rapid palatal expansion and identified a high level of strain in the ZMS which emphasizes the complexity of the issue [22]. Kinzinger et al. [23] investigated the MPS as well as the transpalatal suture (TPS) and concluded that the main resistance for expansion lies in the complex connections surrounding the maxilla rather than in the MPS itself. With age, the center of rotation shifts ventrally as a result of the dorsocranially shifting of the resistance, resulting in a V shaped opening in the course of ORPE.
To provide better insight into suture maturation in females (13–17 years of age) and to better assist the decision making for surgical intervention, the present study aimed to determine a cut-off age when to opt for SARPE vs. ORPE based on skeletal maturation in a female population.
Materials and methods
This study complies with the Declaration of Helsinki “Ethical Principles for Medical Research Involving Human Subjects”. Ethical approval was obtained from the Ethical Review Board of the University Hospitals Leuven (S62686).
A retrospective cohort study was performed on 100 CBCTs of females ranging from 13 to 17 years of age. The images were randomly selected from healthy patients presenting at the Dentomaxillofacial Imaging Center at our hospital from January 2016 to July 2019. All images were obtained for diagnostic indications other than orthodontic decision making for palatal expansion (e.g., impacted canines).
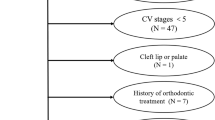
All ages were represented by 20 patients each to create an equilibrium between the age groups. Exclusion criteria were patients with a cleft, a poor-quality scan and previous orthodontic treatment. Only CBCT images of females were included because the patients who came for diagnostic imaging happened to be mostly women. Luckily, they present the largest group in the orthodontic–orthognathic population [24, 25].
CBCT images were acquired according to the following variables: field of view maximum of 230 × 260 to 240 × 190 mm2 depending on indication, 96–110 kV, slice thickness 0.3–0.6 mm with a Planmeca Promax 3D Max (Planmeca, Helsinki, Finland) or a NewTom VGi-evo (NewTom, Verona, Italy) scanner and keeping the as low as reasonably achievable (ALARA) principle in mind [10, 26]. Each scan was taken based on a standardized protocol for the positioning as it was suggested by Angelieri et al. with the patient in a natural head position in all three planes (the head in an upright posture, the eyes focused on a point in the distance at eye level, which implies that the visual axis is horizontal) [27].
Screening of 100 CBCTs was performed randomly and independently by two oral and maxillofacial surgery residents (OMFS) and two orthodontists by assessing the sutures in the maxilla. All CBCT images were anonymized and randomly screened without any knowledge of the patients’ age. The TPS, PMS, and ZMS were analyzed to determine closure, while the level of maturation of the MPS was categorized based on the Angelieri classification [8]. All sutures were assessed in the coronal plane. Figs. 1, 2, and 3 show an open and a closed suture of the TPS, PMS, and ZMS, respectively. The used subdivision of the midpalatal classification is shown in Fig. 4 with exemplary radiographic CBCT images. Stage A appears as an almost straight high-density line, stage B demonstrates a scalloped high-density line, while stage C is characterized as two parallel, scalloped high-density lines. Fusion in the palatine bone of MPS can be visualized in stage D and at stage E, the midpalatal suture is additionally fused in a portion of the maxilla. All stages together represent a gradual transition from an open to a fused suture. Further details on this classification can be found in the study of Angelieri et al. [8]. Based on the results of these four sutures, the observers had also to decide if they would opt for an ORPE or SARPE as the preferred treatment option if the treatment plan would include widening of the maxilla. A subdivision was made based on the training of the examiners (orthodontics or maxillofacial surgery).
Cone-beam computed tomography (CBCT) images corresponding to the maturation stages by the Angelieri classification [8] of the midpalatal suture (MPS). a Stage A: almost straight high-density line; b stage B: scalloped high-density line; c stage C: two parallel, scalloped high-density lines; d stage D: fusion of the MPS only in the palatine bone; e stage E: fusion of the MPS in a portion of the maxilla
Digitale Volumentomographie (DVT) entsprechend den Reifungsstadien nach der Angelieri-Klassifikation [8] der Sutura palatina mediana (MPS). a Stadium A: fast gerade Linie mit hoher Dichte; b Stadium B: gewellte Linie mit hoher Dichte; c Stadium C: 2 parallele, gewellte Linien mit hoher Dichte; d Stadium D: Fusion der MPS nur im Os palatinum; e Stadium E: Fusion der MPS in einem Teil des Oberkiefers
A priori sample size analysis (G*Power 3.1, Heinrich-Heine-Universität, Düsseldorf, Germany) was performed based on a similar study [28]. Power analysis calculated that a sample size of minimum of 20 patients per age category would give an 80% probability of identifying a significant difference concerning suture maturation related to patient age at a significance level of 5%. Correlation of suture assessment between the observers was determined using Kendall’s tau (κ). A p-value of <0.05 indicated a concordant evaluation of the sutures between the observers.
For assessing the relation between suture evaluation and the suggested intervention, a generalized linear mixed model with patients and observers as random factors and the intervention as fixed factor for binary outcomes with a logit link was fit. For assessing the relation between suture evaluation and age, a similar model with age as fixed continuous factor was fit. For the MPS, the two lowest ranked outcome classes were considered as one group (A–B, C–D) for further outcome analysis. This outcome parameter was associated with age outcome for each observer group. To compare the closure of the left and right sutures for the PMS and ZMS, a Fischer’s exact test was performed. A P-value of < 0.05 was considered significant.
To determine a cut-off age for the choice between ORPE and SARPE, a generalized linear mixed model was built between age as a continuous fixed factor and the choice of intervention. Patient and observer were modelled as a random factor. The inflection point of the sigmoidal curve that draws the relation between age and choice was taken as the threshold age.
Results
The CBCTs of 20 patients per age group ranging from 13 to 17 years were analyzed.
The interrater agreement is presented in Table 2. Both the MPS and TPS suture evaluation showed a significant agreement for the orthodontist (P = 0.0059 and P < 0.001, respectively) and maxillofacial surgeon (P = 0.0032 and P < 0.001, respectively) observers. Orthodontists also evaluated the left ZMS with high concordance (P = 0.0465). PMS assessment resulted in a nonsignificant correlation both for orthodontist (P = 1.00) and maxillofacial surgeon (P = 1.00) evaluation.
Closure of TPS increased progressively from age 13 to 15 going from 54% to 85%. After this, closure remains stable with 78% to 85%. In Fig. 5, the prevalence of open and closed TPS is shown in percentages per age group, respectively.
For the PMS, the results show a closure of 83 to 100% (Fig. 6). The percentages of open and closed PMS are presented per age group, respectively.
The ZMS demonstrated a closure of 9 to 47% depending on the age group. For the 13- and 14-year-old females, a closed ZMS was present in 9 to 16%, while for the 15-, 16- and 17-year-old females a closed ZMS was present in 32 to 47% (Fig. 7).
The Fischer’s exact test to compare the left and right sides of the sutures showed a significant (p < 0.001), parallel development of both the PMS and ZMS.
The average results for the MPS analysis are shown in Fig. 8, where the colors indicate the percentages of stages A–E. The percentages per age group and per stage can be found in supplementary Table 1. The frequency of stages A, B, and C decreased over the age groups as the age increased. A transition was taking place, where stages D and E presented more often with increasing age.
Percentage (%) of midpalatal sutures classified as stage A (dark green), B (light green), C (orange), D (bright red), and E (dark red), presented per age group. y years
Prozentsatz (%) der als Stadium A (dunkelgrün), B (hellgrün), C (orange), D (hellrot), and E (dunkelrot) klassifizierten Suturae palatinae medianae entsprechend der Altersgruppe. y Jahre
Table 3 depicts the relation between age and suture evaluation and between suture evaluation and the preference of the doctors for ORPE vs SARPE. These statistical analyses were performed for both orthodontist and maxillofacial surgeon observers. Maxillofacial surgeons reported the MPS and TPS to be significantly correlated with age. Orthodontists reported that MPS, TPS, ZMS, and PMS sutures were significantly more closed with increasing age. Maxillofacial surgeons significantly preferred SARPE intervention with increasing closure of the MPS, TPS, ZMS, and PMS sutures. Orthodontists preferred SARPE intervention when MPS, TPS, and ZMS were more matured. PMS did not significantly influence the orthodontist’s choice for SARPE (P = 0.9993). The cut-off age at which SARPE was suggested, based on the evaluation of the sutures, was 15.1 years for the orthodontist observers and 14.8 years for the maxillofacial surgeon observers (Table 4). Figs. 9 and 10 show the average of the observers’ choice of treatment for ORPE versus SARPE for orthodontists and maxillofacial surgeons, respectively.
The average of the observers’ indication of treatment between orthodontic rapid palatal expansion (ORPE, green) versus surgically assisted rapid palatal expansion (SARPE, red) for orthodontists, presented per age group. y years
Durchschnitt der durch die Beobachter gestellten Behandlungsindikation zwischen kieferorthopädischer schneller Gaumennahterweiterung (ORPE, grün) und chirurgisch assistierter schneller Gaumennahterweiterung (SARPE, rot) für Kieferorthopäden, dargestellt nach Altersgruppen. y Jahre
The average of the observers’ indication of treatment between orthodontic rapid palatal expansion (ORPE, green) versus surgically assisted rapid palatal expansion (SARPE, red) for maxillofacial surgeons, presented per age group. y years
Durchschnitt der durch die Beobachter gestellten Behandlungsindikation zwischen kieferorthopädischer schneller Gaumennahterweiterung (ORPE, grün) und chirurgisch assistierter schneller Gaumennahterweiterung (SARPE, rot) für Mund-Kiefer-Gesichts-Chirurgen, dargestellt nach Altersgruppen. y Jahre
Discussion
This study aimed to determine a cut-off age at which significant maturation of the MPS, TPS, ZMS, and PMS is reached, to be used as a key indicator in the decision about which treatment to choose to widen a narrow maxilla: ORPE or SARPE.
From 13 to 15 years, closure of the TPS gradually increased. From the age of 15 years, closure was arrested at about 80% (range 78–85%). On the basis of CBCT studies Kinzinger et al. [23] reported that a complete open TPS was demonstrable only up to the age of 12 years. In cases older than 12 years, only partially open or closed TPS could be identified. They further stated, based on their subgroups, that ORPE occurred in a triangular fashion from 12 years of age onward with a V-shaped change of the palate. It can be argued that this finding should encourage the preference of SARPE if parallel widening is deemed necessary. Thus, when making the choice about treatment, the amount of widening and the shape of widening (parallel or V‑shaped) should be taken into account. The PMS was classified as closed in 83 to 100%. This means that the PMS may be already closed in a large proportion of patients of a younger age than that investigated in this study. Based on CBCT analysis, Ghoneima et al. confirmed that forces provoked by ORPE affected primarily the anterior sutures [29] Thus, one can reason that early closure of the PMS should affect the orthodontic widening of the maxilla. As already indicated, the main point of resistance moves dorsocranial with the development which can compromise ORPE [23]. Thus, our results seem to support the findings of Laudemann et al. [30] that greater posterior expansion is achieved if pterygomaxillary disjunction is performed. However, the systematic review by Hamedi et al. was inconclusive on this topic [31].
In the groups of 13- and 14-year-olds, 84–91% of the ZMS was classified as open bilaterally. Even in the group of 17-year-old females, around 60% of the ZMS was still open. The analysis of CBCTs in this study has shown great heterogeneity in the timing of closure of the different maxillary sutures. It can be concluded that the PMS, TPS, MPS, and ZMS close sequentially and therefore a comprehensive diagnostic approach is necessary for the choice of treatment. The Fischer’s exact test showed a significant result (p < 0.001) for PMS and ZMS between the left and right sides. This means that an open left suture is significantly associated with an open right suture. One can conclude that suture closure happens symmetrically.
Maturation of the MPS occurs gradually starting from stage A to stage E with an increase over the age groups. Histological findings of the midpalatal suture support the five maturational stages of the Angelieri classification identified on CBCTs [9]. The prepubertal stages A and B represent a broad suture and the beginning of interdigitation, respectively. The fusion process of the MPS starts in stage C with bone spicules and acellular tissue ‘islands’ [8, 17, 18, 20, 32]. Further maturation takes place in stages D and E with sutural fusion starting in the posterior region and subsequently progresses toward the anterior [16, 17]. Stage C is critical since it is the turning point between the open (A and B) and the closed stages (D and E). In the present study, stages A and B together are represented by 42% and 35% in the age groups of 13 and 14 years, respectively. A turning point is present at the age of 15 years since stages D and E are represented by 61%, 66%, and 75% at the ages of 15, 16, and 17 years, respectively. The orthodontist and maxillofacial surgeon observers suggested SARPE from age 15.1 and 14.8 years; hence, based on our detailed suture maturation analysis, one could state that 15 years is a valuable cut-off age to indicate SARPE.
The answer to the question of the best choice of treatment was based on the comprehensive view of all four sutures (TPS, PMS, ZMS, and MPS). These percentages may be higher than the sutures separately considering the observer’s opinion is based on the combination of all sutures. In this comprehensive approach, the early closure of the PMS obviously pushed the observers to the SARPE procedure, since it is known that fusion of this suture compromises ORPE [1, 15]. It is also proven that the fulcrum of maxillary expansion tends to be located more inferior in adolescents which may be attributed to the increased resistance due to ossification of other maxillary sutures and hereby can adversely affect ORPE treatment [33].
Two biases can be identified for the current study. A selection bias is present because the population selected in this study does not represent patients with MTD. It may be that the MPS in patients with MTD closes earlier or later than in the general population. Thus, further research on this topic is necessary. Furthermore, decision-making is biased by the experience, preference and education of the observer (observer bias). In the present study, we opted to have both maxillofacial surgeons and orthodontists to independently make a decision based on the clinical information and the CBCT images. In practice, the indication for both ORPE and SARPE is most often determined by orthodontists. Adding two OMFSs as observers may have reduced the observer bias but they may have a more surgical preference for treating MTD. In this study, OMFSs were more radical in their decision for ORPE in younger ages and SARPE in older ages. For OMFSs, this may be due to a lack of orthodontic education and the general experience to make direct decisions in everyday practice compared to orthodontists.
This study is further limited by its focus on the indication rather than comparing pre- and postexpansion results. The preference of the observers based on suture maturation on CBCT images is presented instead of actual results postexpansion in patients being treated with an ORPE or SARPE procedure, subdivided into stages of the midpalatal suture maturation. Reliability testing of the classification of Angelieri et al. performed by Isfeld et al. [34] did not match the original study [8]. They stated that the methodology is nonintuitive, requires significant operator calibration, and is heavily influenced by the degree of image sharpness and clarity [34]. A recent study indicated that 81% of the females who were 16 years and older demonstrated a stage D midpalatal suture [35]. This is in line with our results and confirms the idea of the possibility of an age-related treatment choice. This view is also supported by studies that proved that females show less variability in open midpalatal sutures than men and that the midpalatal maturation in females generally occurs earlier than in men [9, 35].
Practitioners should consider all maxillary sutures in the decision-making process regarding ORPE vs SARPE for MTD [21] and also realize that the current classification, presented by Angelieri et al. [8], has its limitations [34]. Nevertheless, in combination with the analysis of all maxillary sutures, the classification is a decent guideline for the choice of treatment between ORPE vs SARPE. It should be remembered that each case is patient-specific. There is the possibility that SARPE may be necessary at an even earlier age, but also that ORPE may be possible in adults [36]. One should also keep in mind the amount of widening as the indication when choosing ORPE over SARPE or vice versa. A CBCT will assist in the decision-making process. However, in the absence of imaging, this study can also provide support in making a treatment choice. More research on the maturation of all maxillary sutures is necessary as this will facilitate the decision of the preferred treatment since other sutures will also affect the postexpansion results.
Conclusion
Based on cone-beam computed tomography (CBCT) analysis of the maturation of the pterygomaxillary (PMS), transpalatal (TPS), midpalatal (PMS), and zygomaticomaxillary (ZMS) sutures, this study showed that there is a significant maturation of MPS and TPS in a female population of 15 years and older. One could consider 15 years as a possible cut-off age for orthodontic rapid palatal expansion (ORPE) versus surgically assisted rapid palatal expansion (SARPE), but one should keep the amount of widening and indication in mind. When in doubt, individual assessment of circummaxillary suture maturation can be useful for decision-making in ORPE vs SARPE. The classification of Angelieri et al. is a decent guideline in the choice of treatment but all maxillary sutures have to be taken into account.
References
Baccetti T, Franchi L, Cameron CG, McNamara JA (2001) Treatment timing for rapid maxillary expansion. Angle Orthod 71:343–350
Koudstaal MJ, Poort LJ, van der Wal KGH et al (2005) Surgically assisted rapid maxillary expansion (SARME): a review of the literature. Int J Oral Maxillofac Surg 34:709–714. https://doi.org/10.1016/j.ijom.2005.04.025
Epker B, Wolford L (1980) Transverse maxillary deficiency dentofacial deformities: integrated orthodontic and surgical correction. Mosby, St. Louis
Timms DJ, Vero D (1981) The relationship of rapid maxillary expansion to surgery with special reference to midpalatal synostosis. Br J Oral Surg 19:180–196. https://doi.org/10.1016/0007-117X(81)90003-2
Mossaz CF, Byloff FK, Richter M (1992) Unilateral and bilateral corticotomies for correction of maxillary transverse discrepancies. Eur J Orthod 14:110–116. https://doi.org/10.1093/ejo/14.2.110
Mommaerts MY (1999) Transpalatal distraction as a method of maxillary expansion. Br J Oral Maxillofac Surg 37:268–272. https://doi.org/10.1054/bjom.1999.0127
Alpern MC, Yurosko JJ (1987) Rapid palatal expansion in adults with and without surgery. Angle Orthod 57:245–263
Angelieri F, Cevidanes LHS, Franchi L et al (2013) Midpalatal suture maturation: classification method for individual assessment before rapid maxillary expansion. Am J Orthod Dentofacial Orthop 144:759–769. https://doi.org/10.1016/j.ajodo.2013.04.022
Angelieri F, Franchi L, Cevidanes LHS et al (2016) Prediction of rapid maxillary expansion by assessing the maturation of the midpalatal suture on cone beam CT. Dental Press J Orthod 21:115–125. https://doi.org/10.1590/2177-6709.21.6.115-125.sar
Hendee WR, Edwards F (1986) ALARA and an integrated approach to radiation protection. Semin Nucl Med 16:142–150. https://doi.org/10.1016/s0001-2998(86)80027-7
Franchi L, Baccetti T, Lione R et al (2010) Modifications of midpalatal sutural density induced by rapid maxillary expansion: a low-dose computed-tomography evaluation. Am J Orthod Dentofacial Orthop 137:486–488. https://doi.org/10.1016/j.ajodo.2009.10.028
Sumer AP, Ozer M, Sumer M et al (2012) Ultrasonography in the evaluation of midpalatal suture in surgically assisted rapid maxillary expansion. J Craniofac Surg 23:1375–1377. https://doi.org/10.1097/SCS.0b013e3182519f0a
Kwak KH, Kim SS, Kim YI, Kim YD (2016) Quantitative evaluation of midpalatal suture maturation via fractal analysis. Korean J Orthod 46:323–330. https://doi.org/10.4041/kjod.2016.46.5.323
Melsen B (1975) Palatal growth studied on human autopsy material. A histologic microradiographic study. Am J Orthod 68:42–54. https://doi.org/10.1016/0002-9416(75)90158-X
Melsen B, Melsen F (1982) The postnatal development of the palatomaxillary region studied on human autopsy material. Am J Orthod 82:329–342. https://doi.org/10.1016/0002-9416(82)90467-5
Knaup B, Yildizhan F, Wehrbein H (2004) Age-related changes in the midpalatal suture. A histomorphometric study. J Orofac Orthop 65:467–474. https://doi.org/10.1007/s00056-004-0415-y
Persson M, Thilander B (1977) Palatal suture closure in man from 15 to 35 years of age. Am J Orthod Dentofacial Orthop 72:42–52. https://doi.org/10.1016/0002-9416(77)90123-3
Korbmacher H, Schilling A, Püschel K et al (2007) Age-dependent three-dimensional microcomputed tomography analysis of the human midpalatal suture. J Orofac Orthop 68:364–376. https://doi.org/10.1007/s00056-007-0729-7
Wehrbein H, Yildizhan F (2001) The mid-palatal suture in young adults. A radiological-histological investigation. Eur J Orthod 23:105–114. https://doi.org/10.1093/ejo/23.2.105
Persson M, Magnusson BC, Thilander B (1978) Sutural closure in rabbit and man: a morphological and histochemical study. J Anat 125:313–321. https://doi.org/10.1097/00006534-197811000-00080
Isfeld D, Lagravere M, Leon-Salazar V, Flores-Mir C (2017) Novel methodologies and technologies to assess mid-palatal suture maturation: a systematic review. Head Face Med 13:13. https://doi.org/10.1186/s13005-017-0144-2
Fox GC, Jones TA, Wilson JM et al (2020) Sutural loading in bone- versus dental-borne rapid palatal expansion: an ex vivo study. Orthod Craniofac Res 23:419–426. https://doi.org/10.1111/ocr.12384
Kinzinger GSM, Hourfar J, Buschhoff C et al (2022) Age-dependent interactions of maxillary sutures during RME and their effects on palatal morphology: CBCT and dental cast analysis. J Orofac Orthop 83:412–431. https://doi.org/10.1007/s00056-022-00429-z
Govaerts D, Shaheen E, Coopman R et al (2018) Accuracy of Le Fort I osteotomy in bimaxillary splint-based orthognathic surgery: focus on posterior maxillary movements. Int J Oral Maxillofac Surg 47:1398–1404. https://doi.org/10.1016/j.ijom.2018.05.008
Larsen MK, Thygesen TH (2016) Orthognathic surgery: outcome in a facebook group. J Craniofac Surg 27:350–355. https://doi.org/10.1097/SCS.0000000000002384
Pauwels R, Beinsberger J, Collaert B et al (2012) Effective dose range for dental cone beam computed tomography scanners. Eur J Radiol 81:267–271. https://doi.org/10.1016/j.ejrad.2010.11.028
Lundström A, Lundström F, Lebret L, Moorrees C (1995) Natural head position and natural head orientation—Lundstrom. Eur J Orthod 17:111–120. https://doi.org/10.1109/IEMBS.2009.5332524
Colonna A, Cenedese S, Sartorato F et al (2021) Association of the mid-palatal suture morphology to the age and to its density: a CBCT retrospective comparative observational study. Int Orthod 19:235–242. https://doi.org/10.1016/j.ortho.2021.03.002
Ghoneima A, Abdel-Fattah E, Hartsfield J et al (2011) Effects of rapid maxillary expansion on the cranial and circummaxillary sutures. Am J Orthod Dentofacial Orthop 140:510–519. https://doi.org/10.1016/j.ajodo.2010.10.024
Laudemann K, Santo G, Revilla C et al (2011) Assessment of surgically assisted rapid maxillary expansion regarding pterygomaxillary disjunction using thin volume-rendering technique: in variance analysis and in reliability, accuracy, and validity. J Oral Maxillofac Surg 69:2631–2643. https://doi.org/10.1016/j.joms.2010.12.007
Hamedi Sangsari A, Sadr-Eshkevari P, Al-Dam A et al (2016) Surgically assisted rapid palatomaxillary expansion with or without pterygomaxillary disjunction: a systematic review and meta-analysis. J Oral Maxillofac Surg 74:338–348. https://doi.org/10.1016/j.joms.2015.06.161
Cohen M (1993) Sutural biology and the correlates of craniosynostosis. Am J Med Genet 47:581–616. https://doi.org/10.1002/ajmg.1320470507
Wertz RA (1970) Skeletal and dental changes accompanying rapid midpalatal suture opening. Am J Orthod 58:41–66. https://doi.org/10.1016/0002-9416(70)90127-2
Isfeld D, Flores-Mir C, Leon-Salazar V, Lagravère M (2019) Evaluation of a novel palatal suture maturation classification as assessed by cone-beam computed tomography imaging of a pre- and postexpansion treatment cohort. Angle Orthod 89:252–261. https://doi.org/10.2319/040518-258.1
Jimenez-Valdivia LM, Malpartida-Carrillo V, Rodríguez-Cárdenas YA et al (2019) Midpalatal suture maturation stage assessment in adolescents and young adults using cone-beam computed tomography. Prog Orthod. https://doi.org/10.1186/s40510-019-0291-z
Handelman C (2011) Palatal expansion in adults: the nonsurgical approach. Am J Orthod Dentofacial Orthop 140:462–468. https://doi.org/10.1016/j.ajodo.2011.07.002
Acknowledgements
The authors are extremely grateful to Désirée Maes, DDS, and Stefanos Vichos, DDS, of the Department of Orthodontics, University Hospitals Leuven, Leuven, Belgium for their knowledge and help in the analysis of the CBCT images.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by D. Govaerts, O. Da Costa and M. Garip. The first draft of the manuscript was written by D. Govaerts and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
D. Govaerts, O. Da Costa, M. Garip, F. Combes, R. Jacobs and C. Politis declare that they have no competing interests.
Ethical standards
This study complies with the Declaration of Helsinki “Ethical Principles for Medical Research Involving Human Subjects”. Ethical approval was obtained from the Ethical Review Board of the University Hospitals Leuven (S62686). In accordance with the ethics committee, explicit informed consent was not required as all data were coded and handled in accordance with General Data Protection Regulations (GDPR) and due to the retrospective nature of this study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Govaerts, D., Da Costa, O., Garip, M. et al. Can surgically assisted rapid palatal expansion (SARPE) be recommended over orthodontic rapid palatal expansion (ORPE) for girls above the age of 14?. J Orofac Orthop (2023). https://doi.org/10.1007/s00056-023-00487-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00056-023-00487-x