Abstract
Type 2 diabetes mellitus (T2DM) remains a major global health threat, claiming millions of lives annually. Despite recent advancements in managing T2DM, the need for innovative treatment options persists. Sodium-glucose cotransporter 2 (SGLT2) inhibition has proven to be an effective therapeutic strategy against T2DM, offering benefits in lowering hemoglobin A1c (HbA1c) and plasma glucose levels as well as treatment for patients with diabetes who develop chronic kidney disease (CKD). Bexagliflozin is a recently approved, orally administered SGLT2 inhibitor for treating T2DM and exhibits promise in combating CKD stages 3a and 3b. Structurally, bexagliflozin differs from other SGLT2 inhibitors in that it has a cyclopropyloxyethoxy group at the para position of the peripheral phenyl ring. This review article provides an overview of bexagliflozin’s discovery, mechanism of action, binding site interactions, metabolism, pharmacokinetics, and clinical applications. Emphasis is placed on the significant contribution of SGLT2 inhibitors, particularly bexagliflozin in glycemic control and treating associated comorbidities such as heart failure and chronic kidney disease in T2DM patients.

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Type 2 diabetes mellitus (T2DM) is a metabolic disease in which the body’s ability to produce or respond to insulin is impaired. T2DM is characterized by decreased cellular insulin sensitivity, resulting in unresponsiveness to insulin signals, and progressively diminishing pancreatic production of insulin. This causes a decrease in cellular uptake of glucose which increases the overall blood glucose level. If blood glucose levels are not managed properly, they can cause severe long-term complications throughout the body such as diabetic retinopathy, nerve and kidney damage, and cardiovascular disease [1,2,3]. T2DM is characterized by a hemoglobin A1C (HbA1C) level equal to or above 6.5%, a fasting plasma glucose level equal to or above 126 mg/dL, or a two-hour plasma glucose equal to or greater than 200 mg/dL during an oral glucose tolerance test with a loading dose of 75 g [4]. The swift escalation in obesity rates is partly accountable for the parallel surge in T2DM, affecting nearly 10.5% of the global populace [5]. In 2021, T2DM was responsible for more than 6.7 million deaths among individuals aged 20–79, comprising 12.2% of global deaths in this age group [6].
There are currently several therapeutic approaches to glycemic control in patients with T2DM such as insulin, metformin, thiazolidinediones, sulfonylureas, dipeptidyl peptidase-4 (DPP-4) inhibitors, glucagon-like peptide 1 (GLP-1) receptor agonists, gastric inhibitory peptide receptor agonists and SGLT2 inhibitors. Each of these medications has its own set of benefits and potential side effects [4]. Regardless of the effect, the rising cost of essential medications is a growing concern in the United States. Between 2015 and 2017, it was calculated that the overall expenditure on glucose-lowering medications at the national level surged by 240% (from $16.9 billion to $57.6 billion annually, adjusted to 2017 dollars) compared to 2005 to 2007 [7, 8]. Some additional calculations proved spending on insulin increased by 610% while other drugs such as SGLT2 inhibitors, GLP-1 RAs, and DPP-4 inhibitors increased by 1730% [7, 8]. Specifically, the average out-of-pocket cost per 30-day supply of currently available SGLT2 inhibitors is approximately $416.12 [9, 10].
Current SGLT2 inhibitors on the US market include canagliflozin (Invokana®), dapagliflozin (Farxiga®), empagliflozin (Jardiance®), ertugliflozin (SteglatroTM), and now Bexagliflozin (Brenzavvy®). Bexagliflozin, (2S,3R,4R,5S,6R)-2-[4-chloro-3-[[4-(2-cyclopropyloxyethoxy)phenyl]methyl]phenyl]-6-(hydroxymethyl)oxane-3,4,5-triol)) developed and marketed by TheracosBio, LLC, has been approved by the Food and Drug Administration (FDA) for the treatment of T2DM as highlighted in Table 1 [1]. SGLT2 inhibition lowers overall glucose reabsorption in the renal proximal tubule, thus increasing the urinary excretion of glucose and lowering overall blood glucose levels [11]. Patients with long-term T2DM can benefit more from the unique mechanism of SGLT2 inhibitors such as bexagliflozin. SGLT2 inhibitors lower glucose independent of insulin secretion from beta cells that are exhausted in the late stages of T2DM [11, 12]. SGLT2 inhibition does not affect pancreatic insulin secretion. In addition, bexagliflozin is highly associated with weight loss and antihypertensive effects, though its most common adverse reactions are female genital mycotic infections, urinary tract infections, and increased urination [11]. Other less specific reactions seen in all SGLT2 inhibitors are necrotizing fasciitis, diabetic ketoacidosis, and an increase in nontraumatic lower limb amputations [13]. In geriatric and/or populations with renal conditions, it is found that volume depletion is possible [13, 14]. During carcinogenicity testing in mice and rats, the highest doses of bexagliflozin were administered to each animal and were not associated with neoplastic results [2, 14, 15]. It was found that bexagliflozin was neither mutagenic nor clastogenic through in vitro and in vivo studies [2, 14, 15]. There were no effects on mating or early embryogenesis in female and male rats and no effects on ovulation in female rats at a dosage of up to 200 mg/kg/day [2, 14, 15]. This dose is equivalent to 280 times the recommended dose for males and 439 times the recommended dose for females [2, 14, 15].
The recommended dose of bexagliflozin is 20 mg once daily in the morning, with or without food, and does not require adjustment for patients with renal function abnormalities [9, 11]. The cost of bexagliflozin is approximately $50 per 30-day supply, which is on average about $360 less expensive than other SGLT2 inhibitors [9, 10]. An SGLT2 inhibitor being sold at this price out of pocket carrying such high efficacy for the treatment of T2DM was since now unheard of. Although bexagliflozin is not indicated for chronic kidney disease (CKD), it was still seen to be highly effective for the management of CKD in clinical trials.
Clinical importance of bexagliflozin as a T2DM medication
There are a variety of different SGLT2 inhibitors currently on the market that have been approved before Bexagliflozin. Most glucose-lowering therapies do not address inevitable chronic kidney disease in T2DM [16]. SGLT2 inhibitors can help lower blood glucose levels while managing CKD. However, their efficacy diminishes as continuing kidney function declines [16]. Unlike other drugs in its class, bexagliflozin was found to exhibit its effect in patients with CKD 3a and CKD 3b [15,16,17,18]. To the best of our knowledge, no recent reports or studies of other drugs in its class showed significantly lower HbA1c in patients with diabetes and CKD 3b [16, 19, 20]. Bexagliflozin proved to be a highly suitable SGLT2 inhibitor due to its high selectivity to the SGLT2 channel over the SGLT1 which can be considered a major advantage in the treatment of hyperglycemia [11, 21,22,23]. However, bexagliflozin is contraindicated for patients on dialysis whose kidneys have deteriorated [18].
In one meta-analysis of separate clinical trials where bexagliflozin was compared to other SGLT2 inhibitors, it was seen that bexagliflozin most significantly decreased the estimated glomerular filtration rate (eGFR) [24]. Bexagliflozin causes a significant decrease in eGFR due to its vasoconstrictive effect on the afferent renal arteriole, leading to a reduction in glomerular pressure and decreased hyperfiltration, protecting the kidney [24,25,26]. Under normal conditions, the kidneys perceive a state of hyperglycemia as a lack of blood flow and trigger tubuloglomerular feedback, which dilates the afferent arteriole and increases glomerular pressure, leading to kidney damage [25, 26]. The only other SGLT2 inhibitor approaching this level of renal protection is luseogliflozin (10), which is approved for use in Japan but not approved in the United States [24].
Compared to sulfonylureas, SGLT2 inhibitors increase renal glucose excretion which reduces the chance of hypoglycemia [11, 12]. In a 96-week study evaluating bexagliflozin versus glimepiride in conjunction with metformin, it was shown that bexagliflozin 20 mg once daily had 35% fewer subjects experiencing hypoglycemia compared to glimepiride with metformin [23]. In addition, bexagliflozin reduced HbA1c levels up to 0.8% in the short term, and 0.6% by the end of the study [23]. Although numerous monotherapy studies have been conducted, there are currently no head-to-head studies of bexagliflozin and the other SGLT2 inhibitors on the market. Through separate studies, it is shown that bexagliflozin has demonstrated comparable safety and efficacy to other SGLT2 inhibitors with reductions in fasting plasma glucose levels, HbA1c, and mean weight, as shown in Table 2 [21, 27,28,29,30,31]. In general, bexagliflozin, canagliflozin, dapagliflozin, empagliflozin, and ertugliflozin caused similar adverse events such as diabetic ketoacidosis, urinary tract infections, minor volume depletion, and female genital myotic infections [21, 27,28,29,30,31].
Cardio protective nature of SGLT2 inhibitors
Recent studies have shown how SGLT2 inhibitors not only provide valuable clinical effects on reducing hyperglycemia but also heart failure benefits independent of their glucose-lowering effects [32, 33]. It was discovered that the use of SGLT2 inhibitors contributed to sympathetic nervous system activity suppression and lowered cardiac pre- and afterload [32,33,34]. The cardioprotective effects rely mainly on the role of free fatty acid receptor 3 (FFAR3). FFAR3 is present in sympathetic neurons, and when activated, stimulates sympathetic neuronal firing by inducing a signaling cascade that stimulates the myocardium through norepinephrine release [34, 35]. SGLT2 inhibitors can prevent this myocardial stimulation by increasing the amount of β-hydroxybutyrate [34, 35]. β-hydroxybutyrate is found at high levels in the body during starvation and is highly expressed during treatment with SGLT2 inhibitors [34,35,36]. Dapagliflozin has been the primary SGLT2 inhibitor studied for its cardioprotective nature. However, an increasing number of studies are finding that this is a general factor among the class of drugs as they cause an increase in ketone bodies [32, 34, 35].
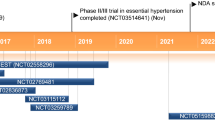
Currently, unlike other marketed SGLT2 inhibitors, bexagliflozin is not yet indicated for the treatment of cardiovascular disease or heart failure. However, recent clinical studies found that bexagliflozin shows clinically meaningful and statistically significant enhancements for cardiovascular health and glycemic control compared to metformin alone [13, 37]. The study demonstrated this effect by using systolic blood pressure as a secondary endpoint compared to the placebo and found that bexagliflozin lowers systolic blood pressure [37]. Results from the Bexagliflozin Efficacy and Safety Trial (BEST) demonstrated that bexagliflozin can improve cardiovascular health by reducing systolic blood pressure in high-risk patients [38]. Bexagliflozin is still being evaluated for its potential beneficial effects in cardiovascular protection.
Target validation
As research and development continue, SGLT has become a major drug target for the treatment of T2DM. SGLT uses a sodium concentration gradient to transport glucose into cells which regulates overall glucose levels in the body [39,40,41,42,43,44]. SGLT1 is found in the kidney, small intestine, the heart to regulate cardiac glucose transport, and the lateral S3 segment of the proximal renal tubule in the kidney [45]. Approximately 10% of all plasma glucose reabsorption is regulated by the SGLT1 [42, 45, 46]. SGLT2 is found in the early S1 segment of the proximal tubule of the nephrons where the transporter intakes plasma glucose into the cell [43, 47]. The approximant glucose reabsorption from SGLT2 is 90% [43, 47]. SGLT2 regulates kidney glucose reabsorption while SGLT1 regulates small intestine glucose reabsorption [42, 43, 48]. SGLT1 transports one sodium ion for two glucose molecules, whereas SGLT2 transports one sodium ion for one glucose molecule [42, 43, 48]. The receptors themselves have different affinities and capacities. SGLT2 has a high capacity, but low affinity for glucose while SGLT1 has a low capacity and high affinity for glucose [39, 48].
SGLT2’s impact on the body’s glucose levels and regulation quickly gave rise to its validity as a drug target for diabetes mellitus. By inhibiting SGLT2’s action in the kidney, SGLT2 inhibitors prevent the reabsorption of glucose in the renal proximal tubule. This causes an increase in glucose clearance in urine due to glucosuria resulting from a lowered renal threshold for glucose [11, 15, 40, 49]. This pharmacological mechanism paved the way for the introduction of several SGLT2 inhibitors to treat T2DM. SGLT2 inhibitors have also been found to cause weight loss and antihypertensive effects [12]. Compared to sulfonylureas and insulin, SGLT2 inhibitors have a lower hypoglycemic risk [12]. In addition to their ability to control blood glucose levels, SGLT2 inhibitors have been found to possess cardioprotective effects in preventing heart failure among T2DM patients with or without cardiovascular disease [15, 49]. This is an additional benefit of SGLT2 inhibitors compared to other antihyperglycemic therapies.
Structural modifications of SGLT2 inhibitors
All currently known SGLT2 inhibitors are derived from phlorizin, a natural product isolated from the bark of apple roots [42, 50]. Originally, phlorizin (Fig. 1) was used for its antipyretic effects to treat fevers and malaria [46, 51]. In 1886, von Mering discovered that the use of phlorizin caused glycosuria [46, 48]. Centuries later, the study of phlorizin’s mechanism of action led to the discovery of SGLT2 inhibitors [46, 48]. It was proven that phlorizin increased insulin sensitivity in tissues and lowered blood glucose [52, 53]. Although phlorizin was shown to reduce elevated blood glucose levels, it could not be used as a hypoglycemic for various pharmacological concerns. As a nonselective SGLT2 inhibitor, meaning it can also inhibit SGLT1, gastrointestinal side effects such as diarrhea and dehydration were prominent [42, 44]. Another setback from the use of phlorizin was its poor metabolic stability after oral administration as an O-glucoside (Fig. 1) which made it easily degraded by beta-glucosidase [50]. To overcome this obstacle of metabolism, the O-glucoside was replaced with N or C-glucosides which created improved metabolic stability [42, 45, 50]. This critical change in structure resulted in the discovery of the current class of SGLT2 inhibitors, all of which have a C-glycosidic linkage between the central phenyl group and the glucose motif.
The chemical structure of an SGLT2 inhibitor has 4 major components including a glycone moiety, an aglycone moiety, a central phenyl ring, and a peripheral phenyl (Fig. 2) [44, 45, 54]. Chemical modifications to the peripheral and central phenyl ring substituents and the glycone moiety will affect drug potency, receptor affinity, and selectivity to one receptor type over another [44, 45, 54]. As previously stated, the glycone and aglycone moieties are connected by a C-glycosidic linkage, which is much more metabolically favored than an O-glycosidic linkage [50]. However, further changes in potency and selectivity are found based on ring substitutions at R1 and R2 on the aglycone moiety [42]. The glycone moiety, which is generally unmodified, is responsible for binding to the receptor in the SGLT2 glucose binding pocket, to block its function [44]. Exceptions include some SGLT2 inhibitors whose glycone structure possesses sulfur instead of oxygen as seen in luseogliflozin (10). The thiol ether significantly boosts the receptors’ inhibition [42]. R1 substitutions on the aglycone moiety can meaningfully alter the potency and selectivity of the SGLT2 inhibitor [42, 50, 55]. The R1 moiety is suggested to be a small halogenated or alkyl group since larger groups attached to the ring tend to show a decreasing trend in SGLT2 inhibitor activity [42, 55]. A chlorine group at the R1 position on the central phenyl ring was found to be the strongest and most essential for SGLT2 inhibitor potency as compared to other moieties placed at the same position [56].
The link between the two phenyl rings plays a role in the activity of the drug as shortening or lengthening the bond will decrease activity [42, 51, 55]. The optimum length of the link between phenyl rings is a single carbon link [42]. Any changes to the peripheral phenyl ring itself will modify the drug’s inhibitory potential [42, 57]. As an example, the replacement of the peripheral phenyl ring with thiophene as seen in canagliflozin (6) will increase both the selectivity towards SGLT2 and potency [42, 57]. Ipragliflozin (8), which is not yet FDA-approved in the US, uses a benzothiophene group instead of the peripheral phenyl ring which led to a lowered potency but an increase in selectivity toward SGLT2 [42, 57]. Based on these two observations, it can loosely be concluded that sulfur heterocycles in place of the phenyl ring show an overall increase in activity [42]. The R2 position is responsible for the difference in potency of the SGLT2 inhibitor drugs, exhibiting the strongest activity when bearing lipophilic strong electron-withdrawing groups including halogens, or weak electron-donating groups such as the cyclopropyloxyethoxy group seen in bexagliflozin [42, 55]. By increasing the chain length of R2, the drug increases its inhibitory potency, however it loses selectivity over SGLT1 [42].
Variance in moieties of bexagliflozin
Bexagliflozin is considered a derivative of a previously approved SLGT2 inhibitor, dapagliflozin (2) (Fig. 1) with the primary difference involving the R2 group on the peripheral phenyl ring. Dapagliflozin has an ethoxy group (11) attached to carbon 4 on the peripheral phenyl ring, whereas bexagliflozin has a cyclopropyloxyethoxy group (12) [51, 58]. Table 3 summarizes the SGLT1 and SGLT2 IC50 values of analogs with various R2 tail variations. The table also displays the selectivity level of SGLT2 compared to SGLT1 [57, 59]. The analog bearing the cyclopropyloxyethoxy (12) group has excellent SGLT2 potency and selectivity over SGLT1. The cyclobutyloxyethoxy derivative (13) also showed a highly similar spectrum of potency and selectivity given practically the same IC50 [57]. As seen in Table 3, increasing the ring size of the cycloalkyl group, reduced potency. Studies have shown that by increasing the ring size of the cycloalkyl group, there was a general decrease in potency, leaving (12) to be the most potent inhibitor and most selective towards SGLT2 out of the compounds tested [51, 57]. The size of the cyclopropyl resulted in the ideal positioning for a balance of selectivity and inhibitory potency.
The R1 substituent in bexagliflozin (1) is a lipophilic electron-withdrawing substituent that has been established to increase the inhibitory potency [42]. The lipophilic electron-withdrawing group is essential for inhibition of the SGLT2 although it has a negligible effect on the selectivity between SGLT1 and SGLT2 [42, 51, 57]. Selectivity and potency comparisons between many currently available SGLT2 inhibitors to bexagliflozin (1) will demonstrate their functionality differences. Bexagliflozin (1) (Fig. 1) has an SGLT2 selectivity of approximately 2400-fold, whereas according to Faille and Jean-Luc, phlorizin (5) has a significantly lower selectivity of SGLT2 over SGLT1 of about 6-14-fold [48, 60,61,62,63,64,65,66]. Many of the other medications have similar selectivity levels with dapagliflozin (2) containing a different R2 group but the same halogen at R1 (Fig. 2) being about 1170-1240-fold. Empagliflozin (3) contains the same halogen atom at R1 but a completely different cycloalkyloxy group at R2 (Fig. 2) yields a selectivity of 2677-fold, and tofogliflozin (4-Japan only) is about 2000–3000-fold [48, 60,61,62,63,64,65,66]. While the selectivity of these compounds is similar, the potency at the SGLT2 is also a key factor. It was proven that the IC50 of bexagliflozin (1) is on average 2.3 (1.3–3.9) nM [48, 60,61,62,63,64,65,66]. Meanwhile, phlorizin (5) is less active at the hSGLT2 which has an IC50 of 21–34.6 nM [48, 60,61,62,63,64,65,66]. Overall, the remaining SGLT2 inhibitors possess similar potency. Dapagliflozin (2), empagliflozin (3), and tofogliflozin (4) have an IC50 of 1.12–1 nM, 3.1 nM, and 2.9–6.4 nM respectively [48, 60,61,62,63,64,65,66]. Of the other SGLT2 inhibitors studied, canagliflozin (6) seems to be a potent yet not very selective SGLT2 inhibitor. Its SGLT2 IC50 of 2.7–4.4 nM shows it is potent while only having a selectivity of 155–263 fold, a tenfold decrease in potency towards SGLT2 compared to bexagliflozin [48, 60,61,62,63,64,65,66].
Synthesis of bexagliflozin
TheracosBio, LLC. filed a product patent in 2010 that displayed information about the discovery and synthesis of bexagliflozin. The synthesis outlined in patent US7838499B2 includes 5 steps to achieving a yield of 10% (Fig. 3) [67, 68]. The synthesis starts by creating 2-cyclo-propoxyethanol (18) by reacting 2-(2-bromoethyl)-1,3-dioxolane (16) with magnesium and dibromoethane (17) in tetrahydrofuran (THF). The compound 2-cyclo-propoxyethanol (18) which results from the prior reaction, is then tosylated to form molecule 19. The aglycone moiety (20) is then used in a Br/Li exchange reaction and added to the glycone moiety (22). Then, mesylation of the hydroxyl group of the intermediate from the reaction with the glycone moiety will form compound 23. The last step removes the methoxy group from 23 by utilizing the reducing agent Et3SiH and BF3×Et2O which forms bexagliflozin (1) after treatment with L-proline. High-performance liquid chromatography (HPLC) results show an achieved purity of 99.2% of bexagliflozin (1) [43, 44]. A major disadvantage of using this route for synthesis is the requirement of the correct stereoisomer for molecule 23 by using a preparative HPLC strategy which decreases the overall product yield [67].
The synthesis of bexagliflozin as outlined in Patent US7838499B2 [68]
Mechanistic binding of bexagliflozin
Glucose reabsorption in kidney nephrons is a key mechanism to understanding the action of SGLT2 inhibitors. SGLT2 inhibitors are quickly absorbed from the gastrointestinal tract to the blood [44]. They are then filtered from the glomerulus in the kidneys where they enter the lumen and bind to the luminal membrane in the proximal tubule [41, 44, 69]. Sodium binding to SGLT2 is needed before SGLT2 inhibitors can bind [41, 44, 69]. This binding blocks the reabsorption of glucose by mimicking its reabsorption process [41, 44, 69]. This is a unique mechanistic class feature that requires filtration by the kidneys before they can elicit their pharmacological effect at the active site.
Since all SGLT2 inhibitors are composed of glycone and aglycone moieties, their binding to the SGLT2 receptor is very similar, if not identical. Studies that have examined structural models such as vSGLT, have given insight into the inhibitor binding properties [44, 70]. The glycone moiety binds tightly to the glucose binding site at the SGLT2 receptor, mimicking the binding of a glucose molecule [44, 50, 71]. This glycone moiety stacks with the aromatic side chain of the residue Y290 found at the inner gate at the glucose binding site [50]. The hydroxyl groups found on the glycone moiety will form hydrogen bonds with the surrounding residues on SGLT2 including side chains of N75, H80, E99, S287, W291, K321, and Q457 as well as the main chain carbonyl group on residue F98 [44, 50]. All the glucose binding site residues in SGLT1 are conserved in SGLT2 and the functional importance of the residues have been confirmed in cysteine mutant studies [44, 72,73,74,75]. Molecular docking studies have identified the inhibitor binding site in the structural models of SGLT1 and SGLT2 [44, 76].
An in vitro study on the selectivity of bexagliflozin was performed in 2011. In this functional SGLT2 uptake assay, the researchers measured the sodium-dependent methyl-α-glucopyranoside (AMG) uptake in cells expressing recombinant human SGLT2 [2, 77]. They found that bexagliflozin was shown to inhibit the uptake of AMG into the cells in a dose-dependent manner [2, 77]. By demonstrating activity in SGLT2-expressing cells, they could assess the functionality/activity of bexagliflozin in vitro, before demonstrating on rats in vivo. Assays were also used in vivo on both rats and dogs in the same study. Both animals were administered bexagliflozin, at a variety of doses, orally after overnight fasting. An hour after administering bexagliflozin, the animals were given a glucose solution 2 g/kg via oral gavage [77]. Blood glucose concentrations were measured before dosing with glucose and 15-, 30-, 60-, and 120-min post-glucose dosing [77]. Urine was also collected from 0 to 4 h, 4 to 8 h, and 8 to 24 h to measure glucose as well as electrolyte analysis. In both animals, it was concluded that bexagliflozin was able to lower glucose blood levels after a 2 g/kg glucose administration in healthy subjects[77]. In rats, bexagliflozin was found to be more effective in lowering glucose levels and in both animals, glucosuria was prominent [77].
Dapagliflozin (2) (Fig. 1) binding exhibits the glucose moiety binding to the glycose site as well as having its aglycone moiety facing the outer side of the vestibule [44]. In comparison to phlorizin, however, dapagliflozin was shown to lie deeper in the binding pocket [44]. Variability in the moieties on aglycone and glycone contributes to the selectivity of SGLT2 over SGLT1. For example, dapagliflozin and bexagliflozin have a hydroxyl group at the carbon 6 of the glycone moiety, which differs from sotagliflozin (9) which has a sulfide group on carbon 5. This group on sotagliflozin (9) allows the drug to be a dual inhibitor of SGLT1 and SGLT2 since the effect of hydrophobic interaction is stronger in the smaller pocket of SGLT1 generated by the sulfide group [42, 50, 78].
SGLT2 inhibitors are competitive inhibitors with a high affinity to the SGLT2 but are only active from the extracellular surface of the SGLT when sodium is bound [41, 44]. The inhibition of these receptors by SGLT2 inhibitors is reversible however they have slower off-time constants due to the strong interaction of the aglycone moiety and the vestibule of the SGLT2 [44, 79]. When the bexagliflozin enters the SGLT2 the glycone moiety will approach the glucose binding site in the SGLT2. Once bound, SGLT2 inhibitors like bexagliflozin will lock the transporter in the outward-facing conformation [44].
Molecular docking studies were performed using a molecular operating environment (MOE, Amarel Desktop, v.2022.02), to find the most probable conformation in the receptor pocket. The amino acid residues and interactions with bexagliflozin are shown in Fig. 4a, b. As expected, the glycone moiety inserts itself into the glucose binding site in the SGLT2 and creates hydrogen bonding interactions with the amino acid residues. The docking also showed various interactions with water molecules in the binding site of bexagliflozin. Figure 4c shows the crystal structure of bexagliflozin inside the receptor binding pocket in the SGLT2 generated by MOE. The bexagliflozin molecule shown in green in Fig. 4c, is the most probable conformation as determined by MOE.
The binding mechanism of bexagliflozin. After sodium binds first, the glycone moiety will bind to the SGLT2 receptor at the glucose binding site. The blue residues interact with the glycone moiety. The dashed lines represent bonding interactions between the drug molecule and amino acid residues at the SGLT2 binding site. Molecular docking studies are presented in a. The interactions were confirmed by Molecular Operating Environment (MOE) studies by docking bexagliflozin to the SGLT2 active site at the optimized conformation. The crystal structure of bexagliflozin bound to SGLT2 active site, generated using MOE docking, is presented in b. Bexagliflozin is shown in green, positioned in the binding pocket in the ribbon structure. This was generated using MOE (c)
Metabolism
Zhang et al. conducted in vitro and in vivo studies to identify the main metabolites of bexagliflozin [77]. They used HPLC coupled with mass spectrometry to analyze samples from humans and animals taking bexagliflozin. The results revealed that metabolism pathways involve glucuronidation and oxidation. In addition, in vitro testing with different recombinant enzymes showed that the primary enzymes acting on bexagliflozin are CYP3A4 and UGT1A9. Across all species studied, metabolite 25 was found to be the major metabolite [1, 2, 77]. Furthermore, they assessed the pharmacologic activity of each metabolite by measuring the sodium-dependent uptake of AMG by cells expressing recombinant human SGLT2 treated with each metabolite [1, 2, 77]. Their findings showed that all metabolites studied exhibited less than 10% of the activity seen in the parent compound bexagliflozin [1, 77].
Bexagliflozin has six primary metabolites, three coming from glucuronidation and three from oxidation [1, 2]. These metabolites have less than 10% activity providing no glucose-lowering activity in the body [1, 2]. Metabolite 27 was seen to have an IC50 value that has glucose-lowering effects (17.9 nM), yet it is not present in high enough concentrations to be clinically relevant [13]. Studies also reported metabolite excretion in the urine, feces, and bile [3, 4]. Pathways of bexagliflozin metabolism are highlighted in Fig. 5 with corresponding enzymes. The primary metabolite excreted in the urine is EGT0002149 (29), created by the isoenzyme UDP-glucuronosyltransferase 1A9 (UGT1A9), found primarily in the kidneys [2]. This major metabolite is a 3-O-glucuronide that is excreted by various organic anion transporters [1]. Metabolite 29 is the only metabolite near the concentration maximum (Cmax) of bexagliflozin, being 0.243 ng/L and 0.727 ng/L respectively which shows how 29 is the primary molecule released from bexagliflozin’s metabolism [2]. The other three main metabolites are formed through the process of oxidation by the cytochrome P450 3A4 (CYP3A4) isoenzyme [1, 2]. These oxidative metabolites are not very potent and minimally circulating, while also being excreted mainly in the feces with the parent compound [2]. Metabolite (S)-EGT0001663 (27) has a 7-fold increase in IC50 and a Cmax of 0.0149 ng/L, while the next closest metabolite is EGT0001494 (25) with a 40-fold increase in IC50 and a Cmax of 0.0298 ng/L, the remaining are all well over 100-1000-fold increases with relatively low Cmax ranging from 0.00525 to 0.0368 ng/L [2]. Most of the metabolites are not potent nor circulate in high concentrations in the blood.
Pharmacokinetics and pharmacodynamics of bexagliflozin in humans
Bexagliflozin can increase the urinary excretion of glucose and urinary volume in a dose-dependent manner [13]. The recommended daily oral dose of 20 mg was found to maintain therapeutic plasma levels after multiple administrations [13]. As mentioned previously, bexagliflozin is effective in patients with normal renal function, reduced renal function, and CKD 3a/3b. However, its efficacy decreases with decreasing renal function [13, 16]. The basic pharmacokinetic parameters of bexagliflozin were within similar ranges as many other SGLT2 inhibitors. It exhibits a bioavailability of about 78% with a half-life of 12 h as determined in the clinical trials [32]. Two clinical studies in humans have shown that bexagliflozin exhibits a half-life of 12 h and a total clearance of 19.1 L/h with the parent compound alone being 28.7% excreted via feces and 1.5% renally [9, 13]. Both the parent compound and associated metabolites together are excreted 51.1% via feces and 40.5% renally [13]. The time to max concentration (Tmax) was between 2 and 4 h without food [9, 13]. With food, the Tmax increased to 5 h with the maximum concentration also increased by 31% [9, 13]. Bexagliflozin is slightly soluble in aqueous environments and does not readily absorb moisture from the environment [2, 14]. Protein binding is 93% with a high volume of distribution of 262 liters. In comparison, dapagliflozin has a protein binding of 91% and a volume of distribution of 118 liters [13, 80].
Discussion
The field of medicinal chemistry has played a crucial role in the development of more effective drugs for treating T2DM. Bexagliflozin not only helps in treating hyperglycemia but also other medical conditions that occur in T2DM such as CKD stages 3a/3b and cardiovascular disease. Bexagliflozin is a similar analog of dapagliflozin with the cyclopropoxyethoxy instead of the ethoxy group. Due to bexagliflozin’s relatively recent FDA approval and short time on the market, very limited mechanistic structure-activity relationship studies are available to date. As shown in Table 3 and Fig. 1, structural variations of the R2 tail result in different measurements of IC50 and selectivity, but no common pattern between structure-activity relationships can be found. As drug design technology becomes robust, the future development of more effective anti-glycemic drugs may rely on the importance of the R2 tail. Based on clinical studies and pharmacological descriptions, bexagliflozin’s selectivity and lowering of the mean weight, fasting plasma glucose, and HbA1c indicate a role for its use in managing T2DM similar to current SGLT2 inhibitors on the market. Head-to-head clinical studies including bexagliflozin against other SGLT2 inhibitors were not found. However, initial positive results regarding the potential to also assist in managing CKD and cardiovascular disease support further evaluation. In the future, further structure-activity relationships should be evaluated including true conformation of bexagliflozin in the SGLT2 binding site, for many SGLT2 inhibitors including bexagliflozin, further studies on the mechanism(s) of action related to blood pressure reduction, weight loss, and albuminuria are warranted.
Conclusion
T2DM, a metabolic disease characterized by hyperglycemia due to impaired insulin sensitivity and/or insulin production, has been the cause of considerable mortality and morbidity across the globe. The development of SGLT2 inhibitors has been a revolutionary weapon against the continuous battle to find treatments for T2DM. Bexagliflozin, a new SGLT2 inhibitor, has proven to be effective in decreasing blood glucose concentration. Many studies have shown SGLT2 inhibitors being used in the treatment of heart disease and slowing of progression in CKD 3b/3a although not yet indicated. Bexagliflozin can lower eGFR, lower systolic blood pressure, and cause albuminuria on top of its antihyperglycemic effects. As marketed now, bexagliflozin may be viewed as a promising option based on cost, efficacy, and safety.
Abbreviations
- AMG:
-
Methyl-α-glucopyranoside
- CKD:
-
Chronic kidney disease
- CKD 3a:
-
Chronic kidney disease stage 3a
- CKD 3b:
-
Chronic kidney disease stage 3b
- Cmax:
-
Concentration maximum
- CYP3A4C:
-
Cytochrome P450 3A4
- DM:
-
Diabetes mellitus
- eGFR:
-
Estimated glomerular filtration rate
- FDA:
-
Food and Drug Administration
- GLP-1:
-
Glucagon-like peptide 1
- HbA1c:
-
Hemoglobin A1c
- HPLC:
-
High-performance liquid chromatography
- hSGLT2:
-
Human sodium glucose cotransporter 2
- MOE:
-
Molecular operating environment
- PDB:
-
Protein Data Bank
- SGLT:
-
Sodium glucose cotransporter
- SGLT1:
-
Sodium glucose cotransporter 1
- SGLT2:
-
Sodium-glucose cotransporter 2
- Tmax:
-
Time to max concentration
- T2DM:
-
Type 2 diabetes mellitus
- UGT1A9:
-
UDP-glucuronosyltransferase 1A9
- vSGLT:
-
Vibrio parahaemolyticus sodium/galactose symporter
References
Gumieniczek A, Berecka-Rycerz A. Metabolism and Chemical Degradation of New Antidiabetic Drugs: A Review of Analytical Approaches for Analysis of Glutides and Gliflozins. Biomedicines. 2023;11:2127 https://doi.org/10.3390/biomedicines11082127.
Zhang W, Li X, Ding H, Lu Y, Stilwell GE, Halvorsen Y-D, et al. Metabolism and disposition of the SGLT2 inhibitor bexagliflozin in rats, monkeys and humans. Xenobiotica. 2020;50:559–69. https://doi.org/10.1080/00498254.2019.1654634.
Quattrin T, Mastrandrea LD, Walker LSK. Type 1 diabetes. Lancet. 2023;401:2149–62. https://doi.org/10.1016/s0140-6736(23)00223-4.
Karnchanasorn R, Huang J, Ou H-Y, Feng W, Chuang L-M, Chiu KC, et al. Comparison of the Current Diagnostic Criterion of HbA1c with Fasting and 2-Hour Plasma Glucose Concentration. J Diab Res. 2016;2016:1–11. https://doi.org/10.1155/2016/6195494.
Ruze R, Liu T, Zou X, Song J, Chen Y, Xu R, et al. Obesity and type 2 diabetes mellitus: connections in epidemiology, pathogenesis, and treatments. Front Endocrinol. 2023;14:1161521 https://doi.org/10.3389/fendo.2023.1161521.
El-Kebbi IM, Bidikian NH, Hneiny L, Nasrallah MP. Epidemiology of type 2 diabetes in the Middle East and North Africa: Challenges and call for action. World J Diab. 2021;12:1401–25. https://doi.org/10.4239/wjd.v12.i9.1401.
Zhou X, Shrestha SS, Shao H, Zhang P. Factors Contributing to the Rising National Cost of Glucose-Lowering Medicines for Diabetes During 2005–2007 and 2015–2017. Diab Care. 2020;43:2396–402. https://doi.org/10.2337/dc19-2273.
Taylor SI. The High Cost of Diabetes Drugs: Disparate Impact on the Most Vulnerable Patients. Diab Care. 2020;43:2330–2. https://doi.org/10.2337/dci20-0039.
Bexagliflozin (Brenzavvy) - A fifth SGLT2 inhibitor for type 2 diabetes. Med Lett Drugs Ther. 2023;65:130–2. https://doi.org/10.58347/tml.2023.1683b.
Aggarwal R, Vaduganathan M, Chiu N, Bhatt DL. Out-of-Pocket Costs for SGLT-2 (Sodium-Glucose Transport Protein-2) Inhibitors in the United States. Circulation: Heart Fail. 2022;15. https://doi.org/10.1161/circheartfailure.121.009099.
Hoy SM. Bexagliflozin: First Approval. Drugs. 2023;83:447–53. https://doi.org/10.1007/s40265-023-01848-x.
Hsia DS, Grove O, Cefalu WT. An update on sodium-glucose co-transporter-2 inhibitors for the treatment of diabetes mellitus. Curr Opin Endocrinol Diab Obes. 2017;24:73–9. https://doi.org/10.1097/med.0000000000000311.
Cowart K, Coon S, Carris NW. A Review of the Safety and Efficacy of Bexagliflozin for the Management of Type 2 Diabetes. Ann Pharmacotherapy. 2023. https://doi.org/10.1177/10600280231190443.
Dalal D, Kant R, Attri K, Kapoor G, Nagarajan K, Bhutani R, et al. A Systematic Overview of Bexagliflozin: A Type 2 Diabetic Drug. Asian J Pharmaceutical Res Health Care. 2023;15:109–14.
Azzam O, Carnagarin R, Lugo-Gavidia LM, Nolde J, Matthews VB, Schlaich MP. Bexagliflozin for type 2 diabetes: an overview of the data. Expert Opin Pharmacother. 2021;22:2095–103. https://doi.org/10.1080/14656566.2021.1959915.
Allegretti AS, Zhang W, Zhou W, Thurber TK, Rigby SP, Bowman-Stroud C, et al. Safety and Effectiveness of Bexagliflozin in Patients With Type 2 Diabetes Mellitus and Stage 3a/3b CKD. Am J Kidney Dis. 2019;74:328–37. https://doi.org/10.1053/j.ajkd.2019.03.417.
Dholariya S, Dutta S, Singh R, Parchwani D, Sonagra A, Kaliya M. Bexagliflozin, a sodium-glucose cotransporter 2 (SGLT2) inhibitor, for improvement of glycemia in type 2 diabetes mellitus: a systematic review and meta-analysis. Expert Opin Pharmacotherapy. 2023. https://doi.org/10.1080/14656566.2023.2269854.
Frak W, Hajdys J, Radzioch E, Szlagor M, Mlynarska E, Rysz J, et al. Cardiovascular Diseases: Therapeutic Potential of SGLT-2 Inhibitors. Biomedicines. 2023;11. https://doi.org/10.3390/biomedicines11072085.
Neal B, Perkovic V, Mahaffey KW, De Zeeuw D, Fulcher G, Erondu N, et al. Canagliflozin and Cardiovascular and Renal Events in Type 2 Diabetes. N Engl J Med. 2017;377:644–57. https://doi.org/10.1056/nejmoa1611925.
Wanner C, Inzucchi SE, Lachin JM, Fitchett D, Von Eynatten M, Mattheus M, et al. Empagliflozin and Progression of Kidney Disease in Type 2 Diabetes. N Engl J Med. 2016;375:323–34. https://doi.org/10.1056/nejmoa1515920.
Halvorsen Y-D, Walford G, Thurber T, Russell H, Massaro M, Freeman MW. A 12-week, randomized, double-blind, placebo-controlled, four-arm dose-finding phase 2 study evaluating bexagliflozin as monotherapy for adults with type 2 diabetes. Diab Obes Metab. 2020;22:566–73. https://doi.org/10.1111/dom.13928.
Halvorsen Y-D, Lock JP, Zhou W, Zhu F, Freeman MW. A 24-week, randomized, double-blind, active-controlled clinical trial comparing bexagliflozin with sitagliptin as an adjunct to metformin for the treatment of type 2 diabetes in adults. Diab Obes Metab. 2019;21:2248–56. https://doi.org/10.1111/dom.13801.
Halvorsen YD, Lock JP, Frias JP, Tinahones FJ, Dahl D, Conery AL, et al. A 96-week, double-blind, randomized controlled trial comparing bexagliflozin to glimepiride as an adjunct to metformin for the treatment of type 2 diabetes in adults. Diab Obes Metab. 2023;25:293–301. https://doi.org/10.1111/dom.14875.
Lin J, Wang S, Wen T, Zhang X. Renal protective effect and safety of sodium-glucose cotransporter-2 inhibitors in patients with chronic kidney disease and type 2 diabetes mellitus: a network meta-analysis and systematic review. Int Urol Nephrol. 2022;54:2305–16. https://doi.org/10.1007/s11255-022-03117-4.
Garcia-Ropero A, Badimon JJ, Santos-Gallego CG. The pharmacokinetics and pharmacodynamics of SGLT2 inhibitors for type 2 diabetes mellitus: the latest developments. Expert Opin Drug Metab Toxicol. 2018;14:1287–302. https://doi.org/10.1080/17425255.2018.1551877.
Sen T, Heerspink HJL. A kidney perspective on the mechanism of action of sodium glucose co-transporter 2 inhibitors. Cell Metab. 2021;33:732–9. https://doi.org/10.1016/j.cmet.2021.02.016.
Feng M, Lv H, Xu X, Wang J, Lyu W, Fu S. Efficacy and safety of dapagliflozin as monotherapy in patients with type 2 diabetes mellitus: A meta-analysis of randomized controlled trials. Medicine. 2019;98:e16575 https://doi.org/10.1097/md.0000000000016575.
Roden M, Merker L, Christiansen AV, Roux F, Salsali A, Kim G, et al. Safety, tolerability and effects on cardiometabolic risk factors of empagliflozin monotherapy in drug-naïve patients with type 2 diabetes: a double-blind extension of a Phase III randomized controlled trial. Cardiovasc Diabetol. 2015;14 https://doi.org/10.1186/s12933-015-0314-0.
Roden M, Weng J, Eilbracht J, Delafont B, Kim G, Woerle HJ, et al. Empagliflozin monotherapy with sitagliptin as an active comparator in patients with type 2 diabetes: a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Diab Endocrinol. 2013;1:208–19. https://doi.org/10.1016/S2213-8587(13)70084-6.
Stenlöf K, Cefalu WT, Kim KA, Alba M, Usiskin K, Tong C, et al. Efficacy and safety of canagliflozin monotherapy in subjects with type 2 diabetes mellitus inadequately controlled with diet and exercise. Diab, Obes Metab. 2013;15:372–82. https://doi.org/10.1111/dom.12054.
Terra SG, Focht K, Davies M, Frias J, Derosa G, Darekar A, et al. Phase III, efficacy and safety study of ertugliflozin monotherapy in people with type 2 diabetes mellitus inadequately controlled with diet and exercise alone. Diab, Obes Metab. 2017;19:721–8. https://doi.org/10.1111/dom.12888.
Basak D, Gamez D, Deb S. SGLT2 Inhibitors as Potential Anticancer Agents. Biomedicines. 2023;11:1867 https://doi.org/10.3390/biomedicines11071867.
Saisho Y. SGLT2 Inhibitors: the Star in the Treatment of Type 2 Diabetes? Diseases. 2020;8 https://doi.org/10.3390/diseases8020014.
Lymperopoulos A, Borges JI, Cora N, Sizova A. Sympatholytic Mechanisms for the Beneficial Cardiovascular Effects of SGLT2 Inhibitors: A Research Hypothesis for Dapagliflozin’s Effects in the Adrenal Gland. Int J Mol Sci. 2021;22:7684 https://doi.org/10.3390/ijms22147684.
Kimura I, Inoue D, Maeda T, Hara T, Ichimura A, Miyauchi S, et al. Short-chain fatty acids and ketones directly regulate sympathetic nervous system via G protein-coupled receptor 41 (GPR41). Proc Natl Acad Sci USA. 2011;108:8030–5. https://doi.org/10.1073/pnas.1016088108.
Stanley WC, Recchia FA, Lopaschuk GD. Myocardial Substrate Metabolism in the Normal and Failing Heart. Physiological Rev. 2005;85:1093–129. https://doi.org/10.1152/physrev.00006.2004.
Halvorsen Y-DC, Lock JP, Freeman MW. 1117-P: Cardiovascular and Glycemic Benefits of Bexagliflozin as an Adjunct to Metformin for the Treatment of Type 2 Diabetes in Adults: A 24-Week, Randomized, Double-Blind, Placebo-Controlled Trial. Diabetes. 2020;69:1117-P https://doi.org/10.2337/db20-1117-P.
McMurray JJV, Freeman MW, Massaro JOE, Solomon S, Lock P, Riddle MC, et al. 32-OR: The Bexagliflozin Efficacy and Safety Trial (BEST): A Randomized, Double-Blind, Placebo-Controlled, Phase IIII, Clinical Trial. Diabetes. 2020;69:32-OR https://doi.org/10.2337/db20-32-OR.
Chao EC, Henry RR. SGLT2 inhibition — a novel strategy for diabetes treatment. Nat Rev Drug Discov. 2010;9:551–9. https://doi.org/10.1038/nrd3180.
Diamant M, Morsink LM. SGLT2 inhibitors for diabetes: turning symptoms into therapy. Lancet. 2013;382:917–8. https://doi.org/10.1016/S0140-6736(13)60902-2.
Ghezzi C, Hirayama BA, Gorraitz E, Loo DD, Liang Y, Wright EM. SGLT2 inhibitors act from the extracellular surface of the cell membrane. Physiol Rep. 2014;2 https://doi.org/10.14814/phy2.12058.
Manoj A, Das S, Kunnath Ramachandran A, Alex AT, Joseph A. SGLT2 inhibitors, an accomplished development in field of medicinal chemistry: an extensive review. Future Med Chem. 2020;12:1961–90. https://doi.org/10.4155/fmc-2020-0154.
Vallon V, Platt KA, Cunard R, Schroth J, Whaley J, Thomson SC, et al. SGLT2 mediates glucose reabsorption in the early proximal tubule. J Am Soc Nephrol. 2011;22:104–12. https://doi.org/10.1681/asn.2010030246.
Wright EM. SGLT2 Inhibitors: Physiology and Pharmacology. Kidney360. 2021;2:2027–37. https://doi.org/10.34067/kid.0002772021.
Ramani J, Shah H, Vyas VK, Sharma M. A review on the medicinal chemistry of sodium glucose co-transporter 2 inhibitors (SGLT2-I): Update from 2010 to present. Eur J Med Chem Rep. 2022;6:100074 https://doi.org/10.1016/j.ejmcr.2022.100074.
Ehrenkranz JRL, Lewis NG, Ronald Kahn C, Roth J. Phlorizin: a review. Diab/Metab Res Rev. 2005;21:31–8. https://doi.org/10.1002/dmrr.532.
Santer R, Calado J. Familial renal glucosuria and SGLT2: from a Mendelian trait to a therapeutic target. Clin J Am Soc Nephrol. 2010;5:133–41. https://doi.org/10.2215/cjn.04010609.
Faillie J-L. Pharmacological aspects of the safety of gliflozins. Pharmacol Res. 2017;118:71–81. https://doi.org/10.1016/j.phrs.2016.07.001.
Verma S, McMurray JJV. SGLT2 inhibitors and mechanisms of cardiovascular benefit: a state-of-the-art review. Diabetologia. 2018;61:2108–17. https://doi.org/10.1007/s00125-018-4670-7.
Hiraizumi M, Akashi T, Murasaki K, Kishida H, Kumanomidou T, Torimoto N, et al. Transport and inhibition mechanism of the human SGLT2–MAP17 glucose transporter. Nat Struct Mol Biol. 2024;31:159–69. https://doi.org/10.1038/s41594-023-01134-0.
Maccari R, Ottanà R. Sodium-Glucose Cotransporter Inhibitors as Antidiabetic Drugs: Current Development and Future Perspectives. J Medicinal Chem. 2022;65:10848–81. https://doi.org/10.1021/acs.jmedchem.2c00867.
Kahn BB, Shulman GI, Defronzo RA, Cushman SW, Rossetti L. Normalization of blood glucose in diabetic rats with phlorizin treatment reverses insulin-resistant glucose transport in adipose cells without restoring glucose transporter gene expression. J Clin Investig. 1991;87:561–70. https://doi.org/10.1172/jci115031.
Rossetti L, Smith D, Shulman GI, Papachristou D, Defronzo RA. Correction of hyperglycemia with phlorizin normalizes tissue sensitivity to insulin in diabetic rats. J Clin Investig. 1987;79:1510–5. https://doi.org/10.1172/jci112981.
Xu G, Xu B, Song Y, Sun X. An efficient method for synthesis of bexagliflozin and its carbon-13 labeled analogue. Tetrahedron Lett. 2016;57:4684–7. https://doi.org/10.1016/j.tetlet.2016.09.003.
Aguillón AR, Mascarello A, Segretti ND, De Azevedo HFZ, Guimaraes CRW, Miranda LSM, et al. Synthetic Strategies toward SGLT2 Inhibitors. Org Process Res Dev. 2018;22:467–88. https://doi.org/10.1021/acs.oprd.8b00017.
Bhattacharya S, Rathore A, Parwani D, Mallick C, Asati V, Agarwal S, et al. An exhaustive perspective on structural insights of SGLT2 inhibitors: A novel class of antidiabetic agent. Eur J Med Chem. 2020;204 https://doi.org/10.1016/j.ejmech.2020.112523.
Xu B, Feng Y, Cheng H, Song Y, Lv B, Wu Y, et al. C-Aryl glucosides substituted at the 4’-position as potent and selective renal sodium-dependent glucose co-transporter 2 (SGLT2) inhibitors for the treatment of type 2 diabetes. Bioorg Med Chem Lett. 2011;21:4465–70. https://doi.org/10.1016/j.bmcl.2011.06.032.
Xu G, Lv B, Roberge JY, Xu B, Du J, Dong J, et al. Design, Synthesis, and Biological Evaluation of Deuterated C-Aryl Glycoside as a Potent and Long-Acting Renal Sodium-Dependent Glucose Cotransporter 2 Inhibitor for the Treatment of Type 2 Diabetes. J Med Chem. 2014;57:1236–51. https://doi.org/10.1021/jm401780b.
Khan NA, Arif H, Imran L. The FDA Has Approved a New SGLT2 Inhibitor, Bexagliflozin, Which is Showing Promising Results in the Management of Type 2 Diabetes. SN Compr Clin Med. 2023;5:217 https://doi.org/10.1007/s42399-023-01563-4.
Grempler R, Thomas L, Eckhardt M, Himmelsbach F, Sauer A, Sharp DE, et al. Empagliflozin, a novel selective sodium glucose cotransporter‐2 (SGLT‐2) inhibitor: characterisation and comparison with other SGLT‐2 inhibitors. Diab Obes Metab. 2012;14:83–90. https://doi.org/10.1111/j.1463-1326.2011.01517.x.
Han S, Hagan DL, Taylor JR, Xin L, Meng W, Biller SA, et al. Dapagliflozin, a Selective SGLT2 Inhibitor, Improves Glucose Homeostasis in Normal and Diabetic Rats. Diabetes. 2008;57:1723–9. https://doi.org/10.2337/db07-1472.
Kakinuma H, Oi T, Hashimoto-Tsuchiya Y, Arai M, Kawakita Y, Fukasawa Y, et al. (1S)-1,5-Anhydro-1-[5-(4-ethoxybenzyl)-2-methoxy-4-methylphenyl]-1-thio-d-glucitol (TS-071) is a Potent, Selective Sodium-Dependent Glucose Cotransporter 2 (SGLT2) Inhibitor for Type 2 Diabetes Treatment. J Med Chem. 2010;53:3247–61. https://doi.org/10.1021/jm901893x.
Kurosaki E, Ogasawara H. Ipragliflozin and other sodium–glucose cotransporter-2 (SGLT2) inhibitors in the treatment of type 2 diabetes: Preclinical and clinical data. Pharmacol Therapeutics. 2013;139:51–9. https://doi.org/10.1016/j.pharmthera.2013.04.003.
Liang Y, Arakawa K, Ueta K, Matsushita Y, Kuriyama C, Martin T, et al. Effect of Canagliflozin on Renal Threshold for Glucose, Glycemia, and Body Weight in Normal and Diabetic Animal Models. PLoS ONE. 2012;7:e30555 https://doi.org/10.1371/journal.pone.0030555.
Ohtake Y, Sato T, Kobayashi T, Nishimoto M, Taka N, Takano K, et al. Discovery of Tofogliflozin, a Novel C-Arylglucoside with an O-Spiroketal Ring System, as a Highly Selective Sodium Glucose Cotransporter 2 (SGLT2) Inhibitor for the Treatment of Type 2 Diabetes. J Medicinal Chem. 2012;55:7828–40. https://doi.org/10.1021/jm300884k.
Tahara A, Kurosaki E, Yokono M, Yamajuku D, Kihara R, Hayashizaki Y, et al. Pharmacological profile of ipragliflozin (ASP1941), a novel selective SGLT2 inhibitor, in vitro and in vivo. Naunyn-Schmiedeberg’s. Arch Pharmacol. 2012;385:423–36. https://doi.org/10.1007/s00210-011-0713-z.
Sasikala CVA, Nahide PD, Beesu M, Biswas S, Basu D, Achanta S, et al. Synthetic Approaches to Gliflozins: A Comprehensive Overview. Synthesis. 2024;56:906–43. https://doi.org/10.1055/s-0042-1751524.
Song Y, Chen Y, Cheng H, Li S, Wu Y, Feng Y, et al. assignee. Preparation of benzylbenzene glycoside derivatives as antidiabetic agents. Patent WO2009026537. 2009.
Eskandari S, Wright EM, Loo DDF. Kinetics of the Reverse Mode of the Na+/Glucose Cotransporter. J Membr Biol. 2005;204:23–32. https://doi.org/10.1007/s00232-005-0743-x.
Watanabe A, Choe S, Chaptal V, Rosenberg JM, Wright EM, Grabe M, et al. The mechanism of sodium and substrate release from the binding pocket of vSGLT. Nature. 2010;468:988–91. https://doi.org/10.1038/nature09580.
Wicik Z, Nowak A, Jarosz-Popek J, Wolska M, Eyileten C, Siller-Matula JM, et al. Characterization of the SGLT2 interaction network and its regulation by SGLT2 inhibitors: a bioinformatic analysis. Front Pharm. 2022;13:901340 https://doi.org/10.3389/fphar.2022.901340.
Jiang X, Loo DD, Hirayama BA, Wright EM. The importance of being aromatic: π interactions in sodium symporters. Biochemistry. 2012;51:9480–7. https://doi.org/10.1021/bi301329w.
Gorraitz E, Hirayama BA, Paz A, Wright EM, Loo DDF. Active site voltage clamp fluorometry of the sodium glucose cotransporter hSGLT1. Proc Natl Acad Sci. 2017;114:E9980–E8. https://doi.org/10.1073/pnas.1713899114.
Sala-Rabanal M, Hirayama BA, Loo DD, Chaptal V, Abramson J, Wright EM. Bridging the gap between structure and kinetics of human SGLT1. Am J Physiol Cell Physiol. 2012;302:C1293–305. https://doi.org/10.1152/ajpcell.00397.2011.
Loo DDF, Jiang X, Gorraitz E, Hirayama BA, Wright EM. Functional identification and characterization of sodium binding sites in Na symporters. Proc Natl Acad Sci. 2013;110:E4557–E66. https://doi.org/10.1073/pnas.1319218110.
Bisignano P, Ghezzi C, Jo H, Polizzi NF, Althoff T, Kalyanaraman C, et al. Inhibitor binding mode and allosteric regulation of Na+-glucose symporters. Nat Commun. 2018;9 https://doi.org/10.1038/s41467-018-07700-1.
Zhang W, Welihinda A, Mechanic J, Ding H, Zhu L, Lu Y, et al. EGT1442, a potent and selective SGLT2 inhibitor, attenuates blood glucose and HbA(1c) levels in db/db mice and prolongs the survival of stroke-prone rats. Pharm Res. 2011;63:284–93. https://doi.org/10.1016/j.phrs.2011.01.001.
Sands AT, Zambrowicz BP, Rosenstock J, Lapuerta P, Bode BW, Garg SK, et al. Sotagliflozin, a Dual SGLT1 and SGLT2 Inhibitor, as Adjunct Therapy to Insulin in Type 1 Diabetes. Diab Care. 2015;38:1181–8. https://doi.org/10.2337/dc14-2806.
Grempler R, Thomas L, Eckhardt M, Himmelsbach F, Sauer A, Sharp DE, et al. Empagliflozin, a novel selective sodium glucose cotransporter-2 (SGLT-2) inhibitor: characterisation and comparison with other SGLT-2 inhibitors. Diab Obes Metab. 2012;14:83–90. https://doi.org/10.1111/j.1463-1326.2011.01517.x.
Kasichayanula S, Liu X, Lacreta F, Griffen SC, Boulton DW. Clinical Pharmacokinetics and Pharmacodynamics of Dapagliflozin, a Selective Inhibitor of Sodium-Glucose Co-transporter Type 2. Clin Pharmacokinetics. 2014;53:17–27. https://doi.org/10.1007/s40262-013-0104-3.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bassett, R.L., Gallo, G., Le, KP.N. et al. Bexagliflozin: a comprehensive review of a recently approved SGLT2 inhibitor for the treatment of type 2 diabetes mellitus. Med Chem Res (2024). https://doi.org/10.1007/s00044-024-03274-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00044-024-03274-4