Abstract
Posaconazole (PSZ, SCH 56592), is a new generation of orally active triazole antifungal agent with a tetrahydrofuran center, derived from itraconazole (ITZ). This drug has a broader spectrum of activity respect to the dioxolane-based triazoles. Structurally, PSZ molecule with four chiral centers and long side chain has a complicated structure. In this review, we describe general aspects of PSZ, including chemistry, pharmacological properties, mechanism of action, synthetic strategies, synthesis of key intermediates, structure-antifungal activity relationships, and the design of its prodrugs. Finally, the non-classical properties of PSZ including antitrypanosomal, antileishmanial and hedgehog (Hh) signaling pathway inhibitory activities will be discussed. By highlighting the information and experiences gained with PSZ, we can better move toward newer compounds of this generation.

Graphical abstract

























Similar content being viewed by others
Abbreviations
- 9-BBN:
-
9-Borabicyclo[3,3,1]nonane
- BCC:
-
Basal cell carcinoma
- BINAP:
-
2,2′-Bis(diary1phosphino)-1,l′-binaphthyl
- BOB:
-
Benzyloxybutyrate
- BSA:
-
Bovine serum albumin
- CD:
-
Chagas disease
- DBCP:
-
Dibenzylchlorophosphate
- DCM:
-
Dichloromethane
- DIBAL-H:
-
Diisobutylaluminum hydride
- DIPEA:
-
Diisopropylethylamine
- DMAP:
-
N′,N′-(dimethylamino)pyridine
- DMF:
-
N,N-dimethylformamide
- DMSO:
-
Dimethyl sulfoxide
- FLZ:
-
Fluconazole
- GVHD:
-
Graft versus host disease
- HATU:
-
1-[Bis(dimethylamino)methylene]-1H-1,2,3-triazolo[4,5b]pyridinium 3-oxide hexafluorophosphate
- Hh:
-
Hedgehog
- HSGT:
-
Hematopoietic stem cell transplantation
- ITZ:
-
Itraconazole
- LAH:
-
Lithium aluminum hydride
- LT:
-
Long-tail
- MB:
-
Medulloblastoma
- MD:
-
Molecular dynamic
- MTBE:
-
Methyl tertiary-butyl ether
- NBS:
-
N-Bromosuccinimide
- NMM:
-
N-Methylmorpholine
- OXZ:
-
(4R)-(+)-4-benzyl-2-oxazolidinone
- PSZ:
-
Posaconazole
- SAR:
-
Structure-activity relationship
- SOB:
-
4-Silyloxybutyrates
- SMO:
-
Smoothened
- ST:
-
Short-tail
- TBAF:
-
Tetrabutylammonium fluoride
- TBSCl:
-
tert-Butyldimethylsilyl chloride
- TEA:
-
Triethylamine
- THF:
-
Tetrahydrofuran
- VRZ:
-
Voriconazole
References
Nagaraj S, Manivannan S, Narayan S. Potent antifungal agents and use of nanocarriers to improve delivery to the infected site: a systematic review. J Basic Microbiol. 2021;61:849–73.
Panagopoulou P, Roilides E. Evaluating posaconazole, its pharmacology, efficacy and safety for the prophylaxis and treatment of fungal infections. Expert Opin Pharmacother. 2022;23:175–99.
Czyrski A, Resztak M, Świderski P, Brylak J, Główka FK. The Overview on the Pharmacokinetic and Pharmacodynamic Interactions of Triazoles. Pharmaceutics. 2021;13:1961.
Schiller DS, Fung HB. Posaconazole: an extended-spectrum triazole antifungal agent. Clin Ther. 2007;29:1862–86.
Nomeir AA, Pramanik BN, Heimark L, Bennett F, Veals J, Bartner P, et al. Posaconazole (Noxafil, SCH 56592), a new azole antifungal drug, was a discovery based on the isolation and mass spectral characterization of a circulating metabolite of an earlier lead (SCH 51048). J Mass Spectrom. 2008;43:509–17.
Bennett F, Saksena AK, Lovey RG, Liu Y-T, Patel NM, Pinto P, et al. Hydroxylated analogues of the orally active broad spectrum antifungal, Sch 51048 (1), and the discovery of posaconazole [Sch 56592; 2 or (S, S)-5]. Bioorg Med Chem Lett. 2006;16:186–90.
Beredaki M-I, Arendrup MC, Andes D, Mouton JW, Meletiadis J. The role of new posaconazole formulations in the treatment of Candida albicans infections: data from an in vitro pharmacokinetic-pharmacodynamic model. Antimicrobial Agents Chemother. 2021;65:e01292–01220.
Pfaller MA, Carvalhaes CG, Messer SA, Rhomberg PR, Castanheira M. In vitro activity of posaconazole and comparators versus opportunistic filamentous fungal pathogens globally collected during 8 years. Diagnostic Microbiol Infect Dis. 2021;101:115473.
Yang M, Cheng L, Dai Q, Yang B, Yuan Q, Yu M, et al. A novel cryptococcal meningitis therapy: the combination of amphotericin B and posaconazole promotes the distribution of amphotericin B in the brain tissue. BioMed Res Int. 2020;2020:8878158.
Szekalska M, Wróblewska M, Trofimiuk M, Basa A, Winnicka K. Alginate oligosaccharides affect mechanical properties and antifungal activity of alginate buccal films with posaconazole. Mar Drugs. 2019;17:692.
González GM, Fothergill AW, Sutton DA, Rinaldi MG, Loebenberg D. In vitro activities of new and established triazoles against opportunistic filamentous and dimorphic fungi. Med Mycol. 2005;43:281–4.
Diekema D, Messer S, Hollis R, Jones R, Pfaller M. Activities of caspofungin, itraconazole, posaconazole, ravuconazole, voriconazole, and amphotericin B against 448 recent clinical isolates of filamentous fungi. J Clin Microbiol. 2003;41:3623–6.
Munayyer HK, Mann PA, Chau AS, Yarosh-Tomaine T, Greene JR, Hare RS, et al. Posaconazole is a potent inhibitor of sterol 14α-demethylation in yeasts and molds. Antimicrobial Agents Chemother. 2004;48:3690–6.
Gonzalez-Lara MF, Ostrosky-Zeichner L. Fungal Infections of the brain, in: Neurological Complications of Infectious Diseases, Springer, Switzerland; 2021. p. 201–24.
Góralska K, Blaszkowska J, Dzikowiec M. Neuroinfections caused by fungi. Infection. 2018;46:443–59.
Stewart AG, Lane S. Just as good but better tolerated: Posaconazole as first-line therapy for invasive aspergillosis. Hematologist. 2021;18.
Grau S, Cámara R, Jurado M, Sanz J, Aragón B, Gozalbo I. Cost-effectiveness of posaconazole tablets versus fluconazole as prophylaxis for invasive fungal diseases in patients with graft-versus-host disease after allogeneic hematopoietic stem cell transplantation. Eur J Health Econ. 2018;19:627–36.
Zhang S, Zhang P, Wang Z, Liu L, He Y, Jiang E, et al. Posaconazole oral suspension as salvage therapy for invasive fungal disease in patients with hematological diseases. Future Microbiol. 2019;14:477–88.
Maertens JA, Rahav G, Lee DG, Ponce-de-León A, Ramírez Sánchez IC, Klimko N, et al. Posaconazole versus voriconazole for primary treatment of invasive aspergillosis: a phase 3, randomised, controlled, non-inferiority trial. Lancet. 2021;397:499–509.
Clark NM, Grim SA, Lynch JP III. Posaconazole: use in the prophylaxis and treatment of fungal infections. Semin Respir Crit Care Med. 2015;36:767–85.
Chen L, Krekels EH, Verweij PE, Buil JB, Knibbe CA, Brüggemann RJ. Pharmacokinetics and pharmacodynamics of posaconazole. Drugs. 2020;80:671–95.
Shafiei M, Peyton L, Hashemzadeh M, Foroumadi A. History of the development of antifungal azoles: a review on structures, SAR, and mechanism of action. Bioorganic Chem. 2020;104:104240.
Irannejad H, Emami S, Mirzaei H, Hashemi SM. In silico prediction of ATTAF-1 and ATTAF-2 selectivity towards human/fungal lanosterol 14α-demethylase using molecular dynamic simulation and docking approaches. Inform Med Unlocked. 2020;20:100366.
Irannejad H, Emami S, Mirzaei H, Hashemi SM. Data on molecular docking of tautomers and enantiomers of ATTAF-1 and ATTAF-2 selectivty to the human/fungal lanosterol-14α-demethylase. Data Brief. 2020;31:105942.
Shi N, Zheng Q, Zhang H. Molecular dynamics investigations of binding mechanism for triazoles inhibitors to CYP51. Front Mol Biosci. 2020;7:266.
Hargrove TY, Friggeri L, Wawrzak Z, Qi A, Hoekstra WJ, Schotzinger RJ, et al. Structural analyses of Candida albicans sterol 14α-demethylase complexed with azole drugs address the molecular basis of azole-mediated inhibition of fungal sterol biosynthesis. J Biol Chem. 2017;292:6728–43.
Fischer A, Don CG, Smiesko M. Molecular dynamics simulations reveal structural differences among allelic variants of membrane-anchored cytochrome P450 2D6. J Chem Inf Modeling. 2018;58:1962–75.
Emami S, Ghobadi E, Saednia S, Hashemi SM. Current advances of triazole alcohols derived from fluconazole: Design, in vitro and in silico studies. Eur J Med Chem. 2019;170:173–94.
Keniya MV, Sabherwal M, Wilson RK, Woods MA, Sagatova AA, Tyndall JD, et al. Crystal structures of full-length lanosterol 14α-demethylases of prominent fungal pathogens Candida albicans and Candida glabrata provide tools for antifungal discovery. Antimicrobial Agents Chemother. 2018;62:e01134–18.
Ezzet F, Wexler D, Courtney R, Krishna G, Lim J, Laughlin M. Oral bioavailability of posaconazole in fasted healthy subjects. Clin Pharmacokinetics. 2005;44:211–20.
Herbrecht R. Posaconazole: a potent, extended‐spectrum triazole anti‐fungal for the treatment of serious fungal infections. Int J Clin Pract. 2004;58:612–24.
Courtney R, Radwanski E, Lim J, Laughlin M. Pharmacokinetics of posaconazole coadministered with antacid in fasting or nonfasting healthy men. Antimicrobial Agents Chemother. 2004;48:804–8.
Li Y, Theuretzbacher U, Clancy CJ, Nguyen MH, Derendorf H. Pharmacokinetic/pharmacodynamic profile of posaconazole. Clin Pharmacokinetics. 2010;49:379–96.
Keating GM. Posaconazole. Drugs. 2005;65:1553–67.
Sabatelli F, Patel R, Mann P, Mendrick C, Norris C, Hare R, et al. In vitro activities of posaconazole, fluconazole, itraconazole, voriconazole, and amphotericin B against a large collection of clinically important molds and yeasts. Antimicrobial Agents Chemother. 2006;50:2009–15.
Suh HJ, Kim I, Cho J-Y, Park S-I, Yoon SH, Hwang J-H, et al. Early therapeutic drug monitoring of Posaconazole Oral suspension in patients with hematologic malignancies. Therapeutic Drug Monit. 2018;40:115–9.
Courtney R, Pai S, Laughlin M, Lim J, Batra V. Pharmacokinetics, safety, and tolerability of oral posaconazole administered in single and multiple doses in healthy adults. Antimicrobial Agents Chemother. 2003;47:2788–95.
Shalini K, Kumar N, Drabu S, Sharma PK. Advances in synthetic approach to and antifungal activity of triazoles. Beilstein J Org Chem. 2011;7:668–77.
Torres HA, Hachem RY, Chemaly RF, Kontoyiannis DP, Raad II. Posaconazole: a broad-spectrum triazole antifungal. Lancet Infect Dis. 2005;5:775–85.
Groll AH, Walsh TJ. Posaconazole: clinical pharmacology and potential for management of fungal infections. Expert Rev Anti-infective Ther. 2005;3:467–87.
Walsh TJ, Raad I, Patterson TF, Chandrasekar P, Donowitz GR, Graybill R, et al. Treatment of invasive aspergillosis with posaconazole in patients who are refractory to or intolerant of conventional therapy: an externally controlled trial. Clin Infect Dis. 2007;44:2–12.
Wiederhold NP. Pharmacokinetics and safety of posaconazole delayed-release tablets for invasive fungal infections. Clin Pharmacol: Adv Appl. 2016;8:1.
Leelawattanachai P, Montakantikul P, Nosoongnoen W, Chayakulkeeree M. Pharmacokinetic/pharmacodynamic study of posaconazole delayed-release tablet in a patient with coexisting invasive aspergillosis and mucormycosis. Therapeutics Clin Risk Manag. 2019;15:589.
Schönbeck C, Gaardahl K, Houston B. Drug solubilization by mixtures of cyclodextrins: additive and synergistic effects. Mol Pharm. 2019;16:648–54.
Ma S-X, Chen W, Yang X-D, Zhang N, Wang S-J, Liu L, et al. Alpinetin/hydroxypropyl-β-cyclodextrin host–guest system: Preparation, characterization, inclusion mode, solubilization and stability. J Pharm Biomed Anal. 2012;67:193–200.
Tang P, Li S, Wang L, Yang H, Yan J, Li H. Inclusion complexes of chlorzoxazone with β-and hydroxypropyl-β-cyclodextrin: characterization, dissolution, and cytotoxicity. Carbohydr Polym. 2015;131:297–305.
Tang P, Ma X, Wu D, Li S, Xu K, Tang B, et al. Posaconazole/hydroxypropyl-β-cyclodextrin host–guest system: improving dissolution while maintaining antifungal activity. Carbohydr Polym. 2016;142:16–23.
Xu F, Xu Y, Liu G, Zhang M, Qiang S, Kang J. Separation of twelve posaconazole related stereoisomers by multiple heart-cutting chiral–chiral two-dimensional liquid chromatography. J Chromatogr A. 2020;1618:460845.
Chen Y, Huang Y, Zhao X, Li Z. Concise synthesis of 1, 3-diacetoxy-2-[2′-(2′′, 4′′-difluorophenyl) prop-2′-en-1′-yl]propane: An Intermediate for Posaconazole. Synthetic Commun. 2015;45:734–40.
Saksena AK, Girijavallabhan VM, Lovey RG, Pike RE, Desai JA, Ganguly AK, et al. Enantioselective synthesis of the optical isomers of broad-spectrum orally active antifungal azoles, Sch 42538 and Sch 45012. Bioorg Med Chem Lett. 1994;4:2023–8.
Lovey RG, Saksena AK, Girijavallabhan VM, Blundell P, Guzik H, Loebenberg D, et al. Synthesis and antifungal activity of the 2, 2, 5-tetrahydrofuran regioisomers of SCH 51048. Bioorg Med Chem Lett. 2002;12:1739–42.
Noé E, Séraphin D, Zhang Q, Djaté F, Hénin J, Laronze J-Y, et al. Synthesis of the new (cyclopenta [b] pyrrolo [1, 2-d]) azepino [4, 5-b] indole ring system. Tetrahedron Lett. 1996;37:5701–4.
Tamao K, Sumitani K, Kiso Y, Zembayashi M, Fujioka A, Kodama S-I, et al. Nickel-phosphine complex-catalyzed Grignard coupling. I. Cross-coupling of alkyl, aryl, and alkenyl Grignard reagents with aryl and alkenyl halides: general scope and limitations. Bull Chem Soc Jpn. 1976;49:1958–69.
Cahiez G, Avedissian H. Highly stereo-and chemoselective iron-catalyzed alkenylation of organomagnesium compounds. Synthesis. 1998;1998:1199–205.
Dos Santos M, Franck X, Hocquemiller R, Figadere B, Peyrat J-F, Provot O, et al. Iron-catalyzed coupling reaction between 1, 1-dichloro-1-alkenes and grignard reagents. Synlett. 2004;2004:2697–700.
Saksena AK, Girijavallabhan VM, Wang H, Liu Y-T, Pike RE, Ganguly AK. Concise asymmetric routes to 2, 2, 4-trisubstituted tetrahydrofurans via chiral titanium imide enolates: Key intermediates towards synthesis of highly active azole antifungals SCH 51048 and SCH 56592. Tetrahedron Lett. 1996;37:5657–60.
Saksena AK, Girijavallabhan VM, Lovey RG, Pike RE, Wang H, Ganguly AK, et al. Highly stereoselective access to novel 2, 2, 4-trisubstituted tetrahydrofurans by halocyclization: Practical chemoenzymatic synthesis of SCH 51048, a broad-spectrum orally active antifungal agent. Tetrahedron Lett. 1995;36:1787–90.
Morgan B, Dodds DR, Zaks A, Andrews DR, Klesse R. Enzymatic desymmetrization of prochiral 2-substituted-1, 3-propanediols: a practical chemoenzymatic synthesis of a key precursor of SCH51048, a broad-spectrum orally active antifungal agent. J Org Chem. 1997;62:7736–43.
Morgan B, Stockwell BR, Dodds DR, Andrews DR, Sudhakar AR, Nielsen CM, et al. Chemoenzymatic approaches to SCH 56592, a new azole antifungal. J Am Oil Chemists’ Soc. 1997;74:1361–70.
Ke Z, Tan CK, Chen F, Yeung Y-Y. Catalytic asymmetric bromoetherification and desymmetrization of olefinic 1, 3-diols with C 2-symmetric sulfides. J Am Chem Soc. 2014;136:5627–30.
Gao M, Zhao Y, Zhong C, Liu S, Liu P, Yin Q, et al. General [4 + 1] cyclization approach to access 2, 2-disubstituted tetrahydrofurans enabled by electrophilic bifunctional peroxides. Org Lett. 2019;21:5679–84.
Hepperle M, Eckert J, Gala D, Shen L, Evans CA, Goodman A. Mono N-arylation of piperazine (III): metal-catalyzed N-arylation and its application to the novel preparations of the antifungal posaconazole and its advanced intermediate. Tetrahedron Lett. 2002;43:3359–63.
Lv G, Zhang D-L, Wang D, Pan L, Liu Y. Synthesis, crystal structure, anti-bone cancer activity and molecular docking investigations of the heterocyclic compound 1-((2S, 3S)-2-(benzyloxy) pentan-3-yl)-4-(4-(4-(4-hydroxyphenyl) piperazin-1-yl) phenyl)-1H-1, 2, 4-triazol-5 (4H)-one. J Struct Chem. 2019;60:1173–9.
Hoffman HL, Ernst EJ, Klepser ME. Novel triazole antifungal agents. Expert Opin Investig Drugs. 2000;9:593–605.
Kim H, Kumari P, Lin C-C, Nomeir AA. Simultaneous high-performance liquid chromatographic determination of SCH 59884 (phosphate ester prodrug of SCH 56592), SCH 207962 and SCH 56592 in dog plasma. J Pharm Biomed Anal. 2002;27:295–303.
Lee GM, Eckert J, Gala D, Schwartz M, Renton P, Pergamen E, et al. Synthesis of Injectable antifungal SCH 59884. Org Process Res Dev. 2001;5:622–9.
Renton P, Gala D, Lee G. SOB as an alternate to BOB: findings from the preparation of injectable antifungal Sch 59884. Tetrahedron Lett. 2001;42:7141–3.
Renton P, Shen L, Eckert J, Lee G, Gala D, Chen G, et al. An intramolecular silyl transfer from the carboxylate to the hydroxyl group in sodium 4-hydroxybutyrate and its application to the synthesis of injectable antifungal posaconazole derivative, Sch 59884. Org Process Res Dev. 2002;6:36–41.
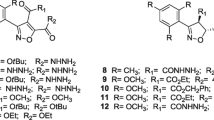
Teske KA, Dash RC, Morel SR, Chau LQ, Wechsler-Reya RJ, Hadden MK. Development of posaconazole-based analogues as hedgehog signaling pathway inhibitors. Eur J Med Chem. 2019;163:320–32.
Kim J, Tang JY, Gong R, Kim J, Lee JJ, Clemons KV, et al. Itraconazole, a commonly used antifungal that inhibits Hedgehog pathway activity and cancer growth. Cancer Cell. 2010;17:388–99.
Doheny D, Manore SG, Wong GL, Lo H-W. Hedgehog signaling and truncated GLI1 in cancer. Cells. 2020;9:2114.
Quaglio D, Infante P, Di Marcotullio L, Botta B, Mori M. Hedgehog signaling pathway inhibitors: an updated patent review (2015–present). Expert Opin Ther Pat. 2020;30:235–50.
Hadden MK. Hedgehog pathway inhibitors: a patent review (2009–present). Expert Opin Ther Pat. 2013;23:345–61.
Scales SJ, de Sauvage FJ. Mechanisms of Hedgehog pathway activation in cancer and implications for therapy. Trends Pharmacol Sci. 2009;30:303–12.
Skoda AM, Simovic D, Karin V, Kardum V, Vranic S, Serman L. The role of the Hedgehog signaling pathway in cancer: A comprehensive review. Bosn J Basic Med Sci. 2018;18:8.
Fecher LA, Sharfman WH. Advanced basal cell carcinoma, the hedgehog pathway, and treatment options–role of smoothened inhibitors. Biologics: Targets Ther. 2015;9:129.
Kieran MW. Targeted treatment for sonic hedgehog-dependent medulloblastoma. Neuro-Oncol. 2014;16:1037–47.
Chen B, Trang V, Lee A, Williams NS, Wilson AN, Epstein EH, et al. Posaconazole, a second-generation triazole antifungal drug, inhibits the hedgehog signaling pathway and progression of basal cell carcinoma. Mol Cancer Ther. 2016;15:866–76.
Rodrigues-dos-Santos I, Melo MF, de Castro L, Hasslocher-Moreno AM, do Brasil PEA, Silvestre de Sousa A, et al. Exploring the parasite load and molecular diversity of Trypanosoma cruzi in patients with chronic Chagas disease from different regions of Brazil. PLoS Neglected Tropical Dis. 2018;12:e0006939.
Liu Z, Ulrich vonBargen R, McCall L-I. Central role of metabolism in Trypanosoma cruzi tropism and Chagas disease pathogenesis. Curr Opin Microbiol. 2021;63:204–9.
Turabelidze G, Vasudevan A, Rojas-Moreno C, Montgomery SP, Baker M, Pratt D, et al. Autochthonous Chagas disease—Missouri, 2018. Morbidity Mortal Wkly Rep. 2020;69:193.
Santana KH, Oliveira LGR, Barros de Castro D, Pereira M. Epidemiology of Chagas disease in pregnant women and congenital transmission of Trypanosoma cruzi in the Americas: systematic review and meta-analysis. Tropical Med Int Health. 2020;25:752–63.
Villalta F, Rachakonda G. Advances in preclinical approaches to Chagas disease drug discovery. Expert Opin Drug Discov. 2019;14:1161–74.
Mazzeti AL, Gonçalves KR, Mota SL, Pereira DE, Diniz LDF, Bahia MT. Combination therapy using nitro compounds improves the efficacy of experimental Chagas disease treatment. Parasitology. 2021;148:1320–7.
Patterson S, Fairlamb AH. Current and future prospects of nitro-compounds as drugs for trypanosomiasis and leishmaniasis. Curr Med Chem. 2019;26:4454–75.
Ribeiro V, Dias N, Paiva T, Hagström-Bex L, Nitz N, Pratesi R, et al. Current trends in the pharmacological management of Chagas disease. Int J Parasitology: Drugs Drug Resistance. 2020;12:7–17.
Keenan M, Chaplin JH. A new era for Chagas disease drug discovery? Prog Med Chem. 2015;54:185–230.
Villalta F, Dobish MC, Nde PN, Kleshchenko YY, Hargrove TY, Johnson CA, et al. VNI cures acute and chronic experimental Chagas disease. J Infect Dis. 2013;208:504–11.
Andriani G, Amata E, Beatty J, Clements Z, Coffey BJ, Courtemanche G, et al. Antitrypanosomal lead discovery: identification of a ligand-efficient inhibitor of Trypanosoma cruzi CYP51 and parasite growth. J Med Chem. 2013;56:2556–67.
Lepesheva GI, Hargrove TY, Rachakonda G, Wawrzak Z, Pomel S, Cojean S, et al. VFV as a new effective CYP51 structure-derived drug candidate for Chagas disease and visceral leishmaniasis. J Infect Dis. 2015;212:1439–48.
Monteiro M, Lechuga G, Lara L, Souto B, Viganó M, Bourguignon S, et al. Synthesis, structure-activity relationship and trypanocidal activity of pyrazole-imidazoline and new pyrazole-tetrahydropyrimidine hybrids as promising chemotherapeutic agents for Chagas disease. Eur J Med Chem. 2019;182:111610.
Diniz LDF, Urbina JA, de Andrade IM, Mazzeti AL, Martins TAF, Caldas IS, et al. Benznidazole and posaconazole in experimental Chagas disease: positive interaction in concomitant and sequential treatments. PLoS Neglected Tropical Dis. 2013;7:e2367.
Benaim G, Sanders JM, Garcia-Marchán Y, Colina C, Lira R, Caldera AR, et al. Amiodarone has intrinsic anti-Trypanosoma cruzi activity and acts synergistically with posaconazole. J Med Chem. 2006;49:892–9.
Algarabel M, Fernández-Rubio C, Musilova K, Peña-Guerrero J, Vacas A, Larrea E, et al. In Leishmania major, the homolog of the oncogene PES1 may play a critical role in parasite infectivity. Int J Mol Sci. 2021;22:12592.
de Almeida JV, de Souza CF, Fuzari AA, Joya CA, Valdivia HO, Bartholomeu DC, et al. Diagnosis and identification of Leishmania species in patients with cutaneous leishmaniasis in the state of Roraima, Brazil’s Amazon Region. Parasites Vectors. 2021;14:1–9.
Borborema SET, Junior JAO, Tempone AG, de Andrade Junior HF, do Nascimento N. Pharmacokinetic of meglumine antimoniate encapsulated in phosphatidylserine-liposomes in mice model: A candidate formulation for visceral leishmaniasis. Biomed Pharmacother. 2018;103:1609–16.
Pereira MB, Sydor BG, Memare KG, Verzignassi Silveira TG, Alessi Aristides SM, Dalmarco EM, et al. In vivo efficacy of meglumine antimoniate-loaded nanoparticles for cutaneous leishmaniasis: a systematic review. Nanomedicine. 2021;16:1505–18.
Soto JA, Berman JD. Miltefosine treatment of cutaneous leishmaniasis. Clin Infect Dis. 2021;73:e2463–e2464.
Sohail A, Khan RU, Khan M, Khokhar M, Ullah S, Ali A, et al. Comparative efficacy of amphotericin B-loaded chitosan nanoparticles and free amphotericin B drug against Leishmania tropica. Bull Natl Res Cent. 2021;45:1–9.
Yadagiri G, Singh PP. Chemotherapy and experimental models of visceral leishmaniasis, In: Infectious Diseases and Your Health, Springer, Singapore; 2018. p. 63–97.
Shafi MT, Bamra T, Das S, Kumar A, Abhishek K, Kumar M, et al. Mevalonate kinase of Leishmania donovani protects parasite against oxidative stress by modulating ergosterol biosynthesis. Microbiol Res. 2021;251:126837.
Yamamoto ES, de Jesus JA, Bezerra-Souza A, Brito JR, Lago JHG, Laurenti MD, et al. Tolnaftate inhibits ergosterol production and impacts cell viability of Leishmania sp. Bioorg Chem. 2020;102:104056.
Al-Abdely HM, Graybill JR, Loebenberg D, Melby PC. Efficacy of the triazole SCH 56592 against Leishmania amazonensis and Leishmania donovani in experimental murine cutaneous and visceral leishmaniases. Antimicrobial Agents Chemother. 1999;43:2910–4.
Emami S, Tavangar P, Keighobadi M. An overview of azoles targeting sterol 14α-demethylase for antileishmanial therapy. Eur J Med Chem. 2017;135:241–59.
de Macedo-Silva ST, Urbina JA, De Souza W, Rodrigues JCF. In vitro activity of the antifungal azoles itraconazole and posaconazole against Leishmania amazonensis. PloS ONE. 2013;8:e83247.
Paniz Mondolfi A, Stavropoulos C, Gelanew T, Loucas E, Perez Alvarez A, Benaim G, et al. Successful treatment of Old World cutaneous leishmaniasis caused by Leishmania infantum with posaconazole. Antimicrobial Agents Chemother. 2011;55:1774–6.
Keighobadi M, Fakhar SM, Shokri A, Mirzaei H, Hosseini Teshnizi S. Repurposing azole antifungals into antileishmanials: Novel 3-triazolylflavanones with promising in vitro antileishmanial activity against Leishmania major. Parasitol Int. 2019;69:103–9.
Shokri A, Emami S, Fakhar M, Hosseini Teshnizi S, Keighobadi M. In vitro antileishmanial activity of novel azoles (3-imidazolylflavanones) against promastigote and amastigote stages of Leishmania major. Acta Tropica. 2017;167:73–8.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dadashpour, S., Ghobadi, E. & Emami, S. Chemical and biological aspects of posaconazole as a classic antifungal agent with non-classical properties: highlighting a tetrahydrofuran-based drug toward generation of new drugs. Med Chem Res 31, 833–850 (2022). https://doi.org/10.1007/s00044-022-02901-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00044-022-02901-2