Abstract
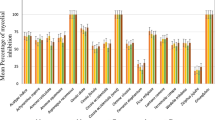
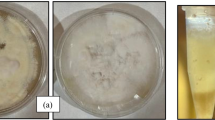
Dermatomycoses are infections caused by fungi and yeasts and the drug treatment is considered expensive and extensive. Researchers are synthesizing new organic compounds in order to obtain more effective molecules that provide reduced adverse effects. Our research group has synthesized and evaluated the biological activities of aminoalcohol and diamine derivatives, which were considered active against human pathogenic fungi. Therefore, the objective of this study was to evaluate the in vitro antifungal activity of aminoalcohols and diamine derivatives against fungi and yeasts that cause dermatomycoses. The minimum inhibitory concentrations (MICs) and the minimum fungicidal concentration (MFC) of aminoalcohol (1–4) and diamine (5–13) derivatives was determined against Trichophyton mentagrophytes, T. rubrum, Epidermophyton floccosum, and Candida albicans according to protocols from the Clinical and Laboratory Standards Institute. All molecules exhibited fungicidal activity against the evaluated fungal strains, with the MIC and MFC ranging between 0.12 and 1000 μg/mL for filamentous fungi and 0.6 and 1250 μg/mL for yeasts. The best activity was attributed to diamines compared to aminoalcohols, with an emphasis on molecules 6 and 7. These results demonstrate the antifungal potential of the evaluated aminoalcohols and diamines against the four primary fungal species that cause dermatomycoses.


Similar content being viewed by others
References
Achterman RR, White TC. Dermatophytes. Curr Biol. 2013;23:551–2. https://doi.org/10.1016/j.cub.2013.03.026.
Chen J, Yi J, Liu L, Yin S, Chen R, Li M, et al. Substrate adaptation of Trichophyton rubrum secreted endoproteases. J Micro Path. 2010;48:57–61. https://doi.org/10.1016/j.micpath.2009.12.001.
Sadeghi-Nejad B, Rezaei-Matehkolaei A, Naanaie SY. Isolation and antifungal activity evaluation of Satureja khuzestanica Jamzad extract against some clinically important dermatophytes. J Myco Med. 2017;27:554–60. https://doi.org/10.1016/j.mycmed.2017.08.002.
Trocoli Drakensjö I, Vassilaki I, Bradley MM. Granuloma caused by Trichophyton mentagrophytes in 2 immunocompetent patients. Actas Dermo-Sifiliogr. 2017;108:e6–8. https://doi.org/10.1016/j.ad.2015.05.020.
Zhang J, Tan J, He Y. Tacrolimus, not triamcinolone acetonide, interacts synergistically with itraconazole, terbinafine, bifonazole, and amorolfine against clinical dermatophyte isolates. J Med Mycol. 2018;28:612–6. https://doi.org/10.1016/j.mycmed.2018.09.003.
Silva-Rocha WP, De Azevedo MF, Chaves GM. Epidemiology and fungal species distribution of superficial mycoses in Northeast Brazil. J Med Mycol. 2017;27:57–64. https://doi.org/10.1016/j.mycmed.2016.08.009.
Achterman RR, White TC. A foot in the door for dermatophyte research. PLoS Pathog. 2012;8:6–9. https://doi.org/10.1371/journal.ppat.1002564.
Silva RAC, Da Silva CR, Neto JBA, Da Silva AR, Campos RS, Sampaio LS, et al. In-vitro anti-Candida activity of selective serotonin reuptake inhibitors against fluconazole-resistant strains and their activity against biofilm-forming isolates. J Micro Path. 2017;107:341–8. https://doi.org/10.1016/j.micpath.2017.04.008.
Wiebusch L, Almeida-Apolonio AA, Rodrigues LMC, Bicudo BP, Silva DBS, Lonchiati DF, et al. Candida albicans isolated from urine: phenotypic and molecular identification, virulence factors and antifungal susceptibility. Asian Pac J Trop Biomed. 2017;7:624–8. https://doi.org/10.1016/j.apjtb.2017.06.006.
Millsop JW, Fazel N. Oral candidiasis. Clin Dermatol. 2016;34:487–94. https://doi.org/10.1016/j.clindermatol.2016.02.022.
Carmello JC, Alves F, Mima EGO, Jorge JH, Bagnato VS, Pavarina AC. Photoinactivation of single and mixed biofilms of Candida albicans and non-albicans Candida species using Phorodithazine®. Photodiagnosis Photodyn Ther. 2017;17:194–9. https://doi.org/10.1016/j.pdpdt.2016.11.013.
Rehman S, Gunday ST, Alsalem ZH, Bozkurt A. Synthesis and characterization of novel azole functionalized poly(glycidyl methacrylate)s for antibacterial and anticandidal activity. Curr Org Synth. 2019;16:1002–9. https://doi.org/10.2174/1385272823666190828112113.
Almeida AM, Oliveira BA, Castro PP, Mendonça CC, Furtado RA, Nicolella HD, et al. Lipophilic gold (I) complexes with 1, 3, 4-oxadiazol-2-thione or 1, 3-thiazolidine-2-thione moieties: synthesis and their cytotoxic and antimicrobial activities. Biometals. 2017;30:841–57. https://doi.org/10.1007/s10534-017-0046-6.
Coimbra ES, Santos JÁ, Lima LL, Machado PA, Campos DL, Pavan FR, et al. Synthesis, antitubercular and leishmanicidal evaluation of resveratrol analogues. J Braz Chem Soc. 2016;27:2161–9. https://doi.org/10.5935/0103-5053.20160107.
Rezende CO Jr, Le Hyaric M, Da Costa CF, Corrêa TA, Taveira AF, Araújo DP, et al. Preparation and antitubercular activity of lipophilic diamines and amino alcohols. Mem do Inst Oswaldo Cruz. 2009;104:703–5. https://doi.org/10.1590/S0074-02762009000500006.
Rezende CO Jr, Alves RO, Rezende CAM, Da Costa CF, Silva H, Le Hyaric M, et al. Trypanocidal activity of lipophilic diamines and amino alcohols. Biomed Pharmacother. 2010;64:624–6. https://doi.org/10.1016/j.biopha.2010.06.002.
Giordani RB, De Almeida MV, Fernandes E, Costa CF, De Carli GA, Tasca T, et al. Anti-Trichomonas vaginalis activity of synthetic lipophilic diamine and amino alcohol derivatives. Biomed Pharmacother. 2009;63:613–7. https://doi.org/10.1016/j.biopha.2008.10.002.
Popadyuk II, Markov AV, Babich VO, Salomatina OV, Logashenko EB, Zenkova MA, et al. Novel derivatives of deoxycholic acid bearing aliphatic or cyclic diamine moieties at the C-3 position: synthesis and evaluation of anti-proliferative activity. Bioorg Med Chem Lett. 2017;27:3755–9. https://doi.org/10.1016/j.bmcl.2017.06.072.
Taveira AF, Le Hyaric M, Reis EFC, Araújo DP, Ferreira AP, De Souza MA, et al. Preparation and antitubercular activities of alkylated amino alcohols and their glycosylated derivatives. Bioorg Med Chem Lett. 2007;15:7789–94. https://doi.org/10.1016/j.bmc.2007.08.045.
Wang D, Liu W, Tang M, Yu N, Yang X. Atroposelective synthesis of biaryl diamines and amino alcohols via chiral phosphoric acid catalyzed para-aminations of anilines and phenols. iScience. 2019;22:195–205. https://doi.org/10.1016/j.isci.2019.11.024.
Fernandes FS, Fernandes TS, Silveira LS, Caneschi W, Lourenço MCS, Diniz CG, et al. Synthesis and evaluation of antibacterial and antitumor activities of new galactopyranosylated amino alcohols. Eur J med Chem. 2016;108:203–10. https://doi.org/10.1016/j.ejmech.2015.11.037.
Rigo GV, Trein MR, Trentin DS, Macedo AJ, De Olivera BA, De Almeida AM, et al. Diamine derivative anti-Trichomonas vaginalis and anti-Tritrichomonas foetus activities by effect on polyamine metabolism. Biomed Pharmacother. 2017;95:847–55. https://doi.org/10.1016/j.biopha.2017.09.007.
De Almeida AM, Nascimento T, Ferreira BS, Castro PP, Silva VL, Diniz CG, et al. Synthesis and antimicrobial activity of novel amphiphilic aromatic amino alcohols.Bioorg Med Chem Lett. 2013;23:2883–7. https://doi.org/10.1016/j.bmcl.2013.03.078.
Caneschi CA, Almeida AM, Martins FJ, Le Hyaric M, Oliveira MME, Macedo GC, et al. In vitro antifungal activity of organic compounds derived from amino alcohols against onychomycosis. Braz J Microbiol. 2017;48:476–82. https://doi.org/10.1016/j.bjm.2016.12.008.
Sales PA Jr, Júnior COR, Le Hyaric M, De Almeida MV, Romanha AJ. The in vitro activity of fatty diamines and amino alcohols against mixed amastigote and trypomastigote Trypanosoma cruzi forms. Mem do Inst Oswaldo Cruz. 2014;109:362–4. https://doi.org/10.1590/0074-0276130496.
Du P, Viswanathan UM, Xu Z, Ebrahimnejad H, Hanf B, Burkholz T, et al. Synthesis of amphiphilic seleninic acid derivatives with considerable activity against cellular membranes and certain pathogenic microbes. J Hazard Mater. 2014;269:74–82. https://doi.org/10.1016/j.jhazmat.2014.01.014.
Schreier S, Malheiros SVP, De Paula E. Surface active drugs: self-association and interaction with membranes and surfactants. Physicochemical and biological aspects. Biochim et Biophys Acta. 2000;1508:210–34. https://doi.org/10.1016/s0304-4157(00)00012-5.
Lima MIO, Medeiros ACA, Silva KVS, Cardoso GN, Lima EO, Pereira FO. Investigation of the antifungal potential of linalool against clinical isolates of fluconazole resistant Trichophyton rubrum. J Mycol Med. 2017;27:195–202. https://doi.org/10.1016/j.mycmed.2017.01.011.
Peres NT, Maranhão FCA, Rossi A, Martinz-Rossi NM. Dermatófitos: Interação patógeno-hospedeiro e resistência a antifúngicos. Bras Dermatol. 2010;85:657–67. https://doi.org/10.1590/S0365-05962010000500009.
Krauss J, Muller C, Kiebling J, Richter S, Staudacher V, Bracher F. Synthesis and biological evaluation of novel N-alkyl tetra- and decahydroisoquinolines: novel antifungals that target ergosterol biosynthesis. Arch Pharm. 2014;347:283–90. https://doi.org/10.1002/ardp.201300338.
Tang H, Wu J, Zhang W, Zhao L, Zhang Y, Shen C. Design, synthesis and biological evaluation of novel non-azole derivatives as potential antifungal agents. Chin Chem Lett. 2015;26:2–6. https://doi.org/10.1016/j.cclet.2015.04.030.
Clinical and Laboratory Standards Institute (CLSI). Reference method for broth dilution antifungal susceptibility testing of filamentous fungi: approved standard. 2nd edn. (M38-A2). Wayne, PA, USA: Clinical and Laboratory Standards Institute; 2008. p. 1–35.
Ouf SA, Abu Taleb AM, Tharwat NA, Geweely NS. Efficacy of some synthesized thiazoles against dermatophytes. J Mycol Med. 2013;23:230–23. https://doi.org/10.1016/j.mycmed.2013.07.056.
Miron D, Battisti F, Silva FK, Lana AD, Pippi B, Casanova B, et al. Antifungal activity and mechanism of action of monoterpenes against dermatophytes and yeasts. Braz J Pharmacogn. 2014;24:660–7. https://doi.org/10.1016/j.bjp.2014.10.014.
Szczepaniak J, Cieslik W, Romanowicz A, Musiol R, Krasowska A. Blocking and dislocation of Candida albicans Cdr1p transporter by styrylquinolines. Int J Antimicrob Agents. 2017;50:171–6. https://doi.org/10.1016/j.ijantimicag.2017.01.044.
Bisha B, Kim HJ, Brehm-Stecher BF. Improved DNA-FISH for cytometric detection of Candida spp. J Appl Microbiol. 2011;110:881–92. https://doi.org/10.1111/j.1365-2672.2011.04936.x.
Rivas L, Mühlhauser M. Complejo Trichophyton mentagrophytes. Rev Chil Infect. 2015;32:319–20. https://doi.org/10.4067/S0716-10182015000400009.
Clinical and Laboratory Standards Institute (CLSI). Reference method for broth dilution antifungal susceptibility testing of yeasts; Third informational supplement. CLSI document M27-S3. Wayne, PA, USA: Clinical and Laboratory Standards Institute; 2008.
Clinical and Laboratory Standards Institute (CLSI). Reference method for broth dilution antifungal susceptibility testing of yeast; fourth informational supplement. CLSI document M27-S4. Wayne, PA, USA: Clinical and Laboratory Standards Institute; 2012.
Falahati M, Nozari S, Makhdoomi A, Ghasemi Z, Nami S, Assadi M. Comparison of antifungal effect of nanosilver particles alone and in combination with current drugs on candida species isolated from women with recurrent vulvovaginal candidiasis. Eur J Exp Biol. 2014;4:77–82.
Magagnin CM, Stopiglia CDO, Vieira FJ, Daiane H, Machado M, Vetoratto G, et al. Perfil de suscetibilidade a antifúngicos de dermatófitos isolados de pacientes com insuficiência renal crônica. Bras Dermatol. 2011;86:694–701. https://doi.org/10.1590/S0365-05962011000400011.
Espinel-Ingroff A, Fothergill A, Peter J, Rinaldi MG, Walsh TJ. Testing conditions for determination of minimum fungicidal concentrations of new and established antifungal agents for Aspergillus spp.: NCCLS Collaborative Study. J Clin Microbiol. 2002;40:3204–8. https://doi.org/10.1128/jcm.40.9.3204-3208.2002.
Acknowledgements
This research was supported by Coordination for the Improvement of Higher Education Personnel (CAPES), National Council for Scientific and Technological Development (CNPq), Research Support Foundation of the State of Minas Gerais (FAPEMIG), Carlos Chagas Filho Foundation for Research Support of the State of Rio de Janeiro (FAPERJ-E-26/202.447/2019), and Pro-Rectorate of Graduate Studies and Research at the Federal University of Juiz de Fora (PROPESQ/UFJF).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Caneschi, C.A., de Oliveira, B.A., de Almeida, A.M. et al. Antifungal activity of aminoalcohols and diamines against dermatophytes and yeast. Med Chem Res 29, 2164–2169 (2020). https://doi.org/10.1007/s00044-020-02636-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00044-020-02636-y