Abstract
Objective
This study aimed at evaluating the cost-effectiveness of human papillomavirus virus (HPV) vaccination in France, using a generally applicable succinct cohort model.
Methods
A lifetime Markov cohort model, adapted to the French setting, simulate the natural history of oncogenic HPV infection towards cervical cancer (CC). Additional modules account for the effects of screening and vaccination. The girls’ cohort is vaccinated at age 12 and follows current screening. Costs and outcomes (discounted at 3 and 1.5%, respectively) were compared with a cohort receiving screening alone.
Results
The model results agreed well with real-life data. Vaccination in addition to screening would substantially reduce the incidence of and mortality from CC, compared with screening alone, at an estimated cost-effectiveness of €9,706 per quality-adjusted-life-year. Sensitivity analysis showed that the discount rate and the parameters related to the disease history have the largest impact on the results.
Conclusion
This succinct cohort model indicated that HPV vaccination would be a cost-effective policy option in France. It uses readily available data and should be generally applicable to the evaluation of HPV vaccination in a variety of countries and settings.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cervical cancer represents a substantial disease burden, with an estimated 530,000 new cases and 275,000 deaths each year worldwide (Ferlay et al. 2010). Screening techniques such as cytology and testing for human papillomavirus (HPV) infection are available and vaccination against HPV now offers a promising additional strategy for management of cervical cancer.
HPV infection is closely associated with cervical cancer (zur Hausen 1996; Walboomers et al. 1999; Bosch et al. 2002). One hundred and twenty types of HPV have been identified (Trottier and Franco 2006), classified into high-risk (oncogenic) types that can lead to pre cervical cancer lesions [low-grade intraepithelial neoplasia (CIN) lesions (CIN 1) and high-grade CIN (CIN2/3)] and cervical cancer and low-risk (non-oncogenic) types that can produce genital warts or CIN 1 but not CIN 2/3 nor cervical cancer (Munoz et al. 2006). Two oncogenic HPV types, HPV-16 and HPV-18, are responsible for 70% of detected cervical cancer cases worldwide (WHO/ICO 2010). Clinical studies have shown that the currently available bivalent vaccine targeting HPV 16/18 is effective against these types but also even beyond these and well tolerated in preventing infections and cervical intraepithelial neoplasia (CIN) (Harper et al. 2006; Paavonen et al. 2009). Addition of HPV vaccination at an early age (12 years) to screening offers a potentially cost-effective method of reducing cervical cancer incidence (Kim et al. 2008; Marra et al. 2009).
As the clinical benefits of vaccination accrue in the future, long-term clinical data will take some decades to collect. In the meantime, modelling studies can integrate currently available clinical data with country-specific epidemiological data to evaluate the potential long-term impact of adding vaccination to screening. Models can also test different scenarios to investigate the effect of uncertainty around some of the input parameters. Several models of HPV vaccination have been published, with varying degrees of complexity and transparency (Kim et al. 2008). In general, sophisticated models lead to more accurate results but are likely to be more difficult to understand. Moreover, detailed input data are not available for all countries, and simpler models may be more widely applicable (Debicki et al. 2008). We developed a succinct model, based on an existing model (Goldie et al. 2004) and close to the one developed by Kulsingam and Myers (2003) that allows transparent estimation of the cost-effectiveness of HPV vaccination using a data set that is easily accessible for most countries. It can be used to provide a rapid preliminary assessment of various vaccination and screening scenarios, such as vaccination with or without screening (opportunistic or organised), at various ages and with or without catch-up vaccination. The model has been described in detail and its performance compared with a more complex modelling approach elsewhere (Debicki et al. 2008). In the present paper we describe its application to evaluating the cost-effectiveness of HPV vaccination in a specific country, France.
Methods
Model design
The model is a lifetime Markov cohort model developed in Microsoft Excel, based on a previously published model (Debicki et al. 2008) with some simplifications to facilitate its transposition to different settings (Debicki et al. 2008). The model consists of three modules.
-
Natural history, with nine health states (no HPV, oncogenic HPV, CIN stage 1, CIN stage 2/3, persistent CIN stage 2/3, cervical cancer, cancer cured, cervical cancer death, death from other cause)
-
Screening, with two additional health states (detected CIN stage 1, detected CIN stage 2/3)
-
Vaccination, which alters the transition probability for moving from the ‘no HPV’ health state to the ‘oncogenic HPV’ health state, based on vaccine efficacy data
The screening module allows the modelling of different screening patterns, such as opportunistic screening (irregular) or organised (national program with a fixed screening interval within a given age range) screening at different ages and intervals.
The model has a cycle time of 1 year and is run over a maximum of 96 cycles, representing the lifetime of the cohort of 11 years girls modelled. The 1-year cycle time facilitates the use of country specific available statistical data most frequently reported on an annual basis.
Each health state has an associated cost and utility score [between 0 and 1, quality-adjusted life-years (QALY)]. At the end of the model (96 cycles) the total costs and total QALYs over each year are summed to estimate lifetime outcomes (life-years, cervical cancer cases, cervical cancer deaths, and QALYs) for the cohort.
Input data
The model inputs for the base case are summarised in Table 1, together with the values used for the univariate deterministic sensitivity analyses. Input data were obtained from published literature and/or official reports where possible, and were further validated by a panel of four French experts to insure applicability to the French settings especially for data reported for other countries whenever no French data were available (Table 1).
Transition probabilities
The probability for the transition from persistent CIN stage 2/3 to cervical cancer was estimated by calibrating the model to the observed cancer incidence data (see section on Model calibration and validation). Other transition probabilities were based on published literature, national statistics, current guidelines and expert opinion (Table 1).
Costs
The costs associated with events in the model were estimated from a limited societal perspective (all direct healthcare costs) at 2007 values, and are listed in Table 1. Some of the event costs were based on a treatment algorithm supplied by the experts panel, to which unit costs were applied. For positive detected CIN lesion, it was assumed that most treatment costs would fall in the first year, and costs in subsequent years would only consist of follow-up costs such as more frequent pap smear tests.
Disutility values
A utility value of 1 (no disutility) was assigned to the following health states: no HPV, oncogenic HPV, CIN 1 and CIN 2/3, as the model assumes that no disutility occurs from competing illnesses. A utility value of 0 was assigned to death and death from cervical cancer by definition. The disutility values, estimated over a 1 year period, for the other health states (detected CIN, cervical cancer and cured cervical cancer) were taken from published sources (Gold et al. 1998; Institute of Medicine 2000; Goldie et al. 2004; Myers et al. 2004; Insinga et al. 2005) and based both on the disutility experienced by the women and the duration of the disease in order to adjust to the 1 year cycle. They are listed in Table 1.
Vaccine efficacy
Vaccine efficacy data were taken from clinical trials and include cross protection (vaccine efficacy against non vaccine HPV types i.e., non HPV 16 and 18) assuming a reduction only in new infections (from no HPV to HPV) and no effect on existing infections or lesions. Vaccine efficacy was differentiated for females in pre- (HPV naïve) versus post-HPV exposure condition (Total Vaccinated Cohort DNA negative irrespective of HPV sero-status data (TVC DNA neg)). A cut-off date of 17 years of age was selected to differentiate between pre- and post exposure based on the average age of sexual debut in France (Wellings et al. 2006). That info was combined with data on the proportion of HPV due to these HPV types (WHO/ICO 2010) (and data on cross-protection (protection beyond HPV 16/18) to calculate the overall reduction in cervical cancer and CIN cases, corrected for the lower proportion of CIN cases caused by oncogenic HPV (Debicki et al. 2008), The values used are listed in Table 1.
Discount rate
In the base case scenario, costs were discounted at a rate of 3% and outcomes at a rate of 1.5% (Table 1). The discount rate of 1.5% for outcomes was selected for ethical reasons, as a higher discount rate would undervalue clinical benefits felt by future generations and this was considered unacceptable by the authors. This parameter was tested in sensitivity analysis (Table 1). Differential discount for cost and effect is also applicable in other countries such as Belgium and the Netherlands (ISPOR 2010).
Model calibration and validation
The model was calibrated to the cancer incidence rates reported in the French national registry (Exbrayat 2002), by adjusting the transition probability for persistent CIN 2/3 to cervical cancer. This transition probability was selected for calibration as no data are available about this transition probability and therefore had to be assumed.
The model was tested against the criteria published by the International Society for Pharmacoeconomics and Outcomes Research (ISPOR) (Weinstein et al. 2003). External validity was tested by entering the input data for models previously published by Goldie et al. (1999, 2004; Kohli et al. 2007), and Kulasingam and Myers (2003), and comparing the results.
Analysis
The base case analysis compared the costs and outcomes of a girls cohort receiving screening according to current practice in France with those of a cohort receiving screening plus vaccination at age 12 years. We calculated the incremental cost-effectiveness ratio (ICER), expressed as the incremental cost per QALY gained or per life-year gained for the vaccinated cohort compared with the non-vaccinated cohort.
Specific scenarios such as age at vaccination and the effects of implementing a catch-up programme with vaccination of additional cohorts up to 25 years of age were also investigated assuming constant efficacy across ages.
Sensitivity analysis
Univariate deterministic sensitivity analyses were conducted to assess the effect of uncertainty around the input values on the model output. The values used are listed in Table 1. Most parameters were varied by ±20% from the base case values, with the exception of the vaccine cross-protection rate (minimum of 0%), the vaccine efficacy rates (maximum of 100%), and the screening frequency (±2 years). As the vaccine coverage rate does not affect the ICER (for any change in coverage, the changes in costs and outcomes are proportional so the ICER does not change), this parameter was not varied (Suárez et al. 2008).
A probabilistic sensitivity analysis was performed using @Risk version 5.0 (Palisade Corporation, Ithaca, New York, USA). Distributions were assigned to transition probabilities, costs, utility and vaccine-related data using normal distributions (limited between 0 and 1 for transition probabilities) when confidence intervals were available, and beta distributions ranging from 20% below the base case value to 20% above the base case value otherwise. A total of 5,000 replicates were obtained using these distributions and used to derive a confidence interval (CI) around the ICER and to conduct a multivariate stepwise linear regression analysis. This analysis identifies the variables in the probabilistic analysis that have the largest impact on the ICER result. The regression coefficients measured were normalised and a value of 0 corresponds to no significant relationship between the input variable and the output result. A value of +1 or −1 indicates that a change of +1 or −1 standard deviation in the input variable results in an equivalent change in the output result (Suárez et al. 2008).
Results
Model validation
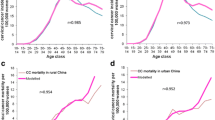
As shown in Fig. 1, the model results closely matched the incidence and mortality data for invasive cervical cancer reported by the French national cancer registry (Exbrayat 2002) for women aged 60–65 years or less, although the model tends to underestimate cancer incidence and mortality at older ages.
Incidence (top) and mortality (bottom) of invasive cervical cancer in France predicted by the model (squares) and observed by the French national cancer registry (Exbrayat 2002) (diamonds)
It fully met all the ISPOR criteria except that the model does not account for the time spent in one health state before transition to another state. The model was also able to replicate the results of a previously published model when run with the input data used for this model, further supporting our model’s validity.
Single cohort analysis
Table 2 shows the base case estimated costs, outcomes and ICER for vaccination of a single cohort of 100,000 girls at age 12 years plus current screening compared with current screening alone. Addition of vaccination at age 12 years to current screening would avoid 749 cases of cervical cancer and 244 deaths from cervical cancer and would gain 5,819 life-years and 6,723 QALYs, compared with screening alone. The estimated discounted ICER was €9,706/QALY. Discounting had a major effect on the results. Without discounting, the estimated ICER would be €309/QALY Table 2.
Effect of age at vaccination
Figure 2 shows the effect of age at vaccination on the ICER and on the numbers of cervical cancer cases avoided and life-years saved. It can be clearly seen that the estimated benefits of adding vaccination to screening were greatest with vaccination at younger ages (before sexual debut), although substantial benefits still accrue even for vaccination at later ages. Approximately 85% of deaths from invasive cervical cancer would be avoided by vaccination at age 12 years, and for vaccination at age 40 years the corresponding value would be approximately 34%. The estimated ICER was also most favourable when vaccination was carried out at age 12, and this was true regardless of discounting (Fig. 2). At a cost-effectiveness threshold of 50,000€/QALY, vaccination would remain cost effective up to the age of 40 years.
Multiple cohort analysis
The effects of a catch-up vaccination programme for women up to the age of 25 years were also explored in a multiple cohort analysis. For a one-year vaccination campaign covering girls and women aged 12–25 years, the ICER for adding vaccination to screening was estimated at €13,079 per QALY. For a 20-year campaign, including all new cohorts of 12-year-old girls over the total campaign, the ICER was estimated at €10,465 across the entire multiple cohort.
Sensitivity analysis
Figure 3 shows the results of the univariate sensitivity analysis as a Tornado plot, with each parameter being varied according to the limits shown in Table 1. The discount rate was the most influential parameter. Most other parameters had only a small effect on the ICER.
The 95% confidence intervals for the ICER, determined from the probabilistic sensitivity analysis, ranged from €2,376/QALY to €33,978/QALY. Figure 4 shows the regression coefficient for all significant results determined from the multivariate stepwise analyses, displaying the level of impact of each on the discounted ICER. These results showed that the most influential parameters were those related to the disease history: progression and regression from HPV, CIN1 and CIN2/3.
Discussion
Healthcare authorities and policymakers need to evaluate the economic impact of healthcare interventions to decide on the allocation of scarce resources. But not all national or regional authorities have access to detailed information on HPV epidemiology, age-specific sexual behaviour or the patterns of cervical cancer screening and treatment, and this lack of data may make it difficult to investigate the potential impact of cervical cancer vaccines. The model presented here has despite several limitations, important advantages. It requires a limited amount of input data that should be readily available in most countries and regions. It represents a generally applicable tool that can help answer key economic questions on cervical cancer vaccination, such as the effects of age at vaccination, catch-up programmes, or different screening practices. These evaluations may be useful when assessing the potential public health impact of different policy options.
The model showed good agreement with cervical cancer incidence and mortality data reported by the French national cancer registry for women aged <60–65 years, but underestimated both parameters for women in older age groups (Fig. 1). This may be because the registry data reflect current incidence and mortality based on past screening practice, whereas the model projects current screening practice into the future. Improvements in screening practice would be expected to reduce the future incidence of cervical cancer, but this may not yet be fully reflected in current observed data in older age groups who would have been screened according to past practice. We were able to replicate the findings of previously published models when our model was run with their input data, and the present model has been shown to produce results similar to those from a more detailed cohort model when tested with data from four countries (Canada, Italy, Taiwan and UK) (Debicki et al. 2008). The findings therefore indicate that the current model is robust and they give confidence in the cost-effectiveness results of HPV vaccination plus screening compared with screening alone.
The model results presented here show that the addition of vaccination with a bivalent HPV vaccine to current cervical screening practice in France would substantially reduce the incidence of and mortality from cervical cancer, at an estimated ICER of €9,706/QALY from a direct healthcare cost perspective. The greatest benefits and most favourable cost-effectiveness would be obtained with vaccination at younger ages (before sexual debut), but substantial benefits would still be obtained with vaccination at older ages. For example, vaccination at age 40 years would still prevent an estimated 35% of cases of invasive cervical cancer, compared with screening alone. These benefits account for a decrease in vaccine efficacy in previously infected women. As expected for a preventive intervention where benefit occurs many years after the intervention, the results are most sensitive to the discount rate and the parameters related to the natural history of the disease.
Our model has a number of limitations. It is not a dynamic transmission model and therefore does not take into account the benefits of herd protection. It would thus underestimate the true benefit of vaccination in that respect. Other published models of cervical cancer have considered this aspect, but these models require much more detailed data than is readily available in France and more computational power. Also, given a succinct model was used, a trade off had to be made between the complexity of the scenarios investigated and their feasibility. For instance our model does not include HPV type specific health states, therefore complex screening pattern such as including HPV DNA testing (Rogoza et al. 2008) or the effect of HPV type specific lesions could not be investigated. Furthermore, we did not account for type replacement or specifically investigate the effect of vaccination on co-infection. One of the uncertainties about HPV vaccination is indeed whether other HPV types will replace the HPV types targeted by the vaccines. To date this question cannot be answered, but available evidence suggests that niche competition is unlikely (Stanley et al. 2006). On the other hand by including only one HPV health state we do not face the problem of increasing susceptibility to non protected HPV types with the vaccine as encountered with other models (Goldie et al. 2004). Finally, our analysis focuses on cost-effectiveness analysis. This, however, does not account for issue of budget impact and therefore affordability that can be assessed by the model but is at the end a decision to be taken by the local health authorities.
A recently published study also investigated the cost-effectiveness of HPV vaccination in France, using a quadrivalent HPV vaccine (Bergeron et al. 2008). This study was an adaptation of the model previously published by Kulasingam and Myers (2003), and compared screening plus vaccination at age 14 years with screening alone. The ICER for the addition of vaccination to screening was €13,809/QALY when considering all direct healthcare costs (Bergeron et al. 2008). This is somewhat higher than our finding of €9,706/QALY for the bivalent vaccine, although it should be noted that no study undertook a direct head-to-head comparison of the two products and the results may therefore not be directly comparable.
This paper describes a succinct cohort model that can be used to investigate key economic issues in HPV vaccination for the prevention of cervical cancer. The model results agreed well with observed data in France, as shown here, and indicate that HPV vaccination would be a cost-effective policy option. As the model uses data that are readily available in most countries and regions, it should be generally applicable to the evaluation of the cost effectiveness of HPV vaccination in a variety of settings.
References
Arveux P, Benard S, Bouee S, Lafuma A, Martin L, Cravello L, Remy V, Breugelmans JG (2007) Invasive cervical cancer treatment costs in France. Bull Cancer 94(2):219–224
Beby-Defaux A, Bourgoin A, Ragot S, Battandier D, Lemasson JM, Renaud O, Bouguermouh S, Vienne Md ML, Agius G (2004) Human papillomavirus infection of the cervix uteri in women attending a Health Examination Center of the French social security. J Med Virol 73(2):262–268
Bergeron C, Breugelmans JG, Bouee S, Lorans C, Benard S, Remy V (2006) Coût du depistage et de la prise en charge des lesions precancereuses du col uterin en France. Gynecologie Obstetrique Fertilite 34(11):1036–1042
Bergeron C, Largeron N, McAllister R, Mathevet P, Remy V (2008) Cost-effectiveness analysis of the introduction of a quadrivalent human papillomavirus vaccine in France. Int J Technol Assess Health Care 24(1):10–19
Bosch FX, Lorincz A, Munoz N, Meijer CJ, Shah KV (2002) The causal relation between human papillomavirus and cervical cancer. J Clin Pathol 55(4):244–265
Boulanger JC, Sevestre H, Bauville E, Ghighi C, Harlicot JP, Gondry J (2004) Epidemiology of HPV infection. Gynecol Obstet Fertil 32(3):218–223
Clavel C, Masure M, Bory JP, Putaud I, Mangeonjean C, Lorenzato M, Nazeyrollas P, Gabriel R, Quereux C, Birembaut P (2001) Human papillomavirus testing in primary screening for the detection of high-grade cervical lesions: a study of 7932 women. Br J Cancer 84(12):1616–1623
Clifford GM, Smith JS, Plummer M, Munoz N, Franceschi S (2003) Human papillomavirus types in invasive cervical cancer worldwide: a meta-analysis. Br J Cancer 88(1):63–73
Cochand-Priollet B, Vincent S, Vielh P (2004) Cytopathology in France. Cytopathology 15(3):163–166
Coleman MP, Gatta G, Verdecchia A, Esteve J, Sant M, Storm H, Allemani C, Ciccolallo L, Santaquilani M, Berrino F (2003) EUROCARE-3 summary: cancer survival in Europe at the end of the 20th century. Ann Oncol 14(Suppl 5):v128–v149
Dalstein V, Riethmuller D, Sautiere JL, Pretet JL, Kantelip B, Schaal JP, Mougin C (2004) Detection of cervical precancer and cancer in a hospital population; benefits of testing for human papillomavirus. Eur J Cancer 40(8):1225–1232
Debicki D, Ferko N, Demarteau N, Gallivan S, Bauch C, Anonychuk A, Mantovani L, Capri S, Chou CY, Standaert B, Annemans L (2008) Comparison of detailed and succinct cohort modelling approaches in a multi-regional evaluation of cervical cancer vaccination. Vaccine 26(Suppl 5):F16–F28
Exbrayat C (2002) Col de l’utérus. In: Remontet L, Buemi A, Velten M, Jougla E, Esteve J (eds) Evolution de l’incidence et de la mortalité par cancer en France de 1978 à 2000. Institut de Veille Sanitaire. Departement Maladies Chroniques et Traumatismes, Saint-Maurice Cédex, pp 107–112
Fahey MT, Irwig L, Macaskill P (1995) Meta-analysis of Pap test accuracy. Am J Epidemiol 141(7):680–689
Ferlay J, Bray F, Pisani P, Parkin DM (2004) Globocan 2002: Cancer incidence, mortality and prevalence worldwide. IARC Press. Available via IARC. Accessed August 2008
Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM (2010) GLOBOCAN 2008: Cancer incidence and mortality worldwide. International agency for research on cancer. Available via http://globocan.iarc.fr. Accessed June 2010
Gold MR, Franks P, McCoy KI, Fryback DG (1998) Toward consistency in cost-utility analyses: using national measures to create condition-specific values. Med Care 36(6):778–792
Goldie SJ, Weinstein MC, Kuntz KM, Freedberg KA (1999) The costs, clinical benefits, and cost-effectiveness of screening for cervical cancer in HIV-infected women. Ann Intern Med 130(2):97–107
Goldie SJ, Kohli M, Grima D, Weinstein MC, Wright TC, Bosch FX, Franco E (2004) Projected clinical benefits and cost-effectiveness of a human papillomavirus 16/18 vaccine. J Natl Cancer Inst 96(8):604–615
Harper DM, Franco EL, Wheeler CM, Moscicki AB, Romanowski B, Roteli-Martins CM, Jenkins D, Schuind A, Costa-Clemens SA, Dubin G (2006) Sustained efficacy up to 4.5 years of a bivalent L1 virus-like particle vaccine against human papillomavirus types 16 and 18: follow-up from a randomized control trial. Lancet 367(9518):1247–1255
Insinga R, Glass A, Rush B. (2005) Health state transitions following an abnormal pap smear: implications for health utility assessment in cost-effectiveness analyses. (Abstract W-02 presented at 22nd International Papillomavirus Conference and Clinical Workshop 2005, Vancouver, Canada, April 30–May 6)
Institut National des Etudes Démographiques (2004) Taux de mortalité par sexe et âge en 2004. http://www.ined.fr. Accessed March 2008
Institute of Medicine (2000) Appendix 11: human papillomavirus. In: Stratton KR, Durch JS, Lawrence S (eds) Vaccines for the 21st century: a tool for decisionmaking. National Academy Press, Washington, p 213
ISPOR (2010) Pharmacoeconomic guidelines around the world. http://www.ispor.org/PEguidelines/index.asp. Accessed September 2010
Kim JJ, Brisson M, Edmunds WJ, Goldie SJ (2008) Modeling cervical cancer prevention in developed countries. Vaccine 26(Suppl 10):K76–K86
Kohli M, Ferko N, Martin A, Franco EL, Jenkins D, Gallivan S, Sherlaw-Johnson C, Drummond M (2007) Estimating the long-term impact of a prophylactic human papillomavirus 16/18 vaccine on the burden of cervical cancer in the UK. Br J Cancer 96(1):143–150
Kulasingam SL, Myers ER (2003) Potential health and economic impact of adding a human papillomavirus vaccine to screening programs. JAMA 290(6):781–789
Marra F, Cloutier K, Oteng B, Marra C, Ogilvie G (2009) Effectiveness and cost effectiveness of human papillomavirus vaccine: a systematic review. Pharmacoeconomics 27(2):127–147
Melnikow J, Nuovo J, Willan AR, Chan BK, Howell LP (1998) Natural history of cervical squamous intraepithelial lesions: a meta-analysis. Obstet Gynecol 92(4 Pt 2):727–735
Moscicki AB, Hills N, Shiboski S, Powell K, Jay N, Hanson E, Miller S, Clayton L, Farhat S, Broering J, Darragh T, Palefsky J (2001) Risks for incident human papillomavirus infection and low-grade squamous intraepithelial lesion development in young females. JAMA 285(23):2995–3002
Munoz N, Castellsague X, Gonzalez ABd, Gissmann L (2006) Chapter 1. Human papillomavirus in the etiology of human cancer. Vaccine 24(Suppl 3):S1–S10
Myers ER, GreenS, Lipkus I (2004) Patient preferences for health states related to HPV infection: visual analog scale versus time trade-off elicitation. (Abstract n° 542 presented at the Twenty-first International Papillomavirus Conference, Mexico City, Mexico. February 20–27)
Nobbenhuis MA, Helmerhorst TJ, van den Brule AJ, Rozendaal L, Voorhorst FJ, Bezemer PD, Verheijen RH, Meijer CJ (2001) Cytological regression and clearance of high-risk human papillomavirus in women with an abnormal cervical smear. Lancet 358(9295):1782–1783
Paavonen J, Naud P, Salmerón J, Wheeler CM, Chow SN, Apter D, Kitchener H, Castellsague X, Teixeira JC, Skinner SR, Hedrick J, Jaisamrarn U, Limson G, Garland S, Szarewski A, Romanowski B, Aoki FY, Schwarz TF, Poppe WAJ, Bosch FX, Jenkins D, Hardt K, Zahaf T, Descamps D, Struyf F, Lehtinen M, Dubin G (2009) Efficacy of human papillomavirus (HPV)-16/18 AS04-adjuvanted vaccine against cervical infection and precancer caused by oncogenic HPV types (PATRICIA): final analysis of a double-blind, randomised study in young women. Lancet 374(9686):301–314
Riethmuller D, Gay C, Bertrand X, Bettinger D, Schaal JP, Carbillet JP, Lassabe C, Arveux P, Seilles E, Mougin C (1999) Genital human papillomavirus infection among women recruited for routine cervical cancer screening or for colposcopy determined by Hybrid Capture II and polymerase chain reaction. Diagn Mol Pathol 8(3):157–164
Rogoza RM, Ferko N, Bentley J, Meijer CJLM, Berkhof J, Wang KL, Downs L, Smith JS, Franco EL (2008) Optimization of primary and secondary cervical cancer prevention strategies in an era of cervical cancer vaccination: A multi-regional health economic analysis. Vaccine 26(Suppl 5):F46–F58
Romanowski B, de Borba PC, Naud PS, Roteli-Martins CM, De Carvalho NS, Teixeira JC, Aoki F, Ramjattan B, Shier RM, Somani R, Barbier S, Blatter MM, Chambers C, Ferris D, Gall SA, Guerra FA, Harper DM, Hedrick JA, Henry DC, Korn AP, Kroll R, Moscicki AB, Rosenfeld WD, Sullivan BJ, Thoming CS, Tyring SK, Wheeler CM, Dubin G, Schuind A, Zahaf T, Greenacre M, Sgriobhadair A (2009) Sustained efficacy and immunogenicity of the human papillomavirus (HPV)-16/18 AS04-adjuvanted vaccine: analysis of a randomised placebo-controlled trial up to 6.4 years. Lancet 374(9706):1975–1985
Sanders GD, Taira AV (2003) Cost-effectiveness of a potential vaccine for human papillomavirus. Emerg Infect Dis 9(1):37–48
Schaffer P, Sancho-Garnier H, Fender M, Dellenbach P, Carbillet JP, Monnet E, Gauthier GP, Garnier A (2000) Cervical cancer screening in France. Eur J Cancer 36(17):2215–2220
Skinner R, Apter D, Chow SN, Wheeler C, Dubin G (2009) Cross-protection efficacy of Cervarix(tm) against oncogenic HPV types beyond HPV-16/18. (Abstract n° O-29.01 presented at the 25th International Papillomavirus Conference, Malmö, Sweden, May 8–14)
Stanley M, Lowy DR, Frazer I (2006) Chapter 12: Prophylactic HPV vaccines: underlying mechanisms. Vaccine 24(Suppl 3):S106–S113
Suárez E, Smith JS, Bosch FX, Nieminen P, Chen CJ, Torvinen S, Demarteau N, Standaert B (2008) Cost-effectiveness of vaccination against cervical cancer: a multi-regional analysis assessing the impact of vaccine characteristics and alternative vaccination scenarios. Vaccine 26(Suppl 5):F29–F45
Szarewski A (2010) HPV vaccine: Cervarix. Expert Opin Biol Ther 10(3):477–487
Tjalma W, Paavonen J, Naud P, Wheeler CM, Chow SN, Apter D, Kitchener H, Castellsague X, Teixeira JC, Skinner SR, Hedrick J, Jaisamrarn U, Garland S, Szarewski A, Romanowski B, Aoki D, Schwarz TF, Poppe WAJ, Bosch FX, Jenkins D, Hardt K, Zahaf T, Descamps D, Struyf F, Lehtinen M, Dubin G (2009) Efficacy of the HPV-16/18 AS04-adjuvanted vaccine against abnormal cytology and low-grade histopathological lesions in an oncogenic HPV-naïve population. (Abstract n° A-171-0004-01446 presented at the 16th International Meeting of the European Society for Gynaecological Oncology (ESGO), Belgrade, Serbia, October 11–14 )
Trottier H, Franco EL (2006) The epidemiology of genital human papillomavirus infection. Vaccine 24(Suppl 1):S1–S15
Van De Velde N, Brisson M, Boily MC (2007) Modeling human papillomavirus vaccine effectiveness: quantifying the impact of parameter uncertainty. Am J Epidemiol 165(7):762–775
Walboomers JM, Jacobs MV, Manos MM, Bosch FX, Kummer JA, Shah KV, Snijders PJ, Peto J, Meijer CJ, Munoz N (1999) Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J Pathol 189(1):12–19
Weinstein MC, O’Brien B, Hornberger J, Jackson J, Johannesson M, McCabe C, Luce BR (2003) Principles of good practice for decision analytic modeling in health-care evaluation: report of the ISPOR task force on good research practices–modeling studies. Value Health 6(1):9–17
Wellings K, Collumbien M, Slaymaker E, Singh S, Hodges Z, Patel D, Bajos N (2006) Sexual behaviour in context: a global perspective. Lancet 368(9548):1706–1728
Wheeler C, HPV Patricia Study Group (2010) Efficacy of the AS04-adjuvanted HPV-16/18 vaccine in reducing abnormal cytology and against lesions associated with vaccine and non-vaccine oncogenic types: an analysis of women negative for specific HPV types at baseline. (Abstract presented at THE European Research Organisation on Genital Infection and Neoplasia (EUROGIN), Monte Carlo, Monaco, February 17–20)
WHO/ICO (2010) Information centre on HPV and cervical cancer. http://www.who.int/hpvcentre/statistics/dynamic/ico/DataQuerySelect.cfm. Accessed February 2010
zur Hausen H (1996) Roots and perspectives of contemporary papillomavirus research. J Cancer Res Clin Oncol 122(1):3–13
Acknowledgments
The authors thank Professor Lucien Abenhaim (Paris), Pierre-Jean Lancry (Paris), Dr Didier Guillemot (Paris) and Dr Christine Bergeron (Saint Ouen l’Aumône) for providing expert advice on the input data, and Carole Nadin and Rachel Emerson for medical writing services. This study was conducted on behalf of GlaxoSmithKline Biologicals, Rixensart, Belgium.
Conflict of interest
Nadia Demarteau, Bertrand Tehard, Abdelkader El Hasnaoui and Baudouin Standaert are employees of GlaxoSmithKline. Bruno Detournay has performed consultancy work for GlaxoSmithKline. This study was funded by GSK Biologicals SA, Rixensart, Belgium.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Demarteau, N., Detournay, B., Tehard, B. et al. A generally applicable cost-effectiveness model for the evaluation of vaccines against cervical cancer. Int J Public Health 56, 153–162 (2011). https://doi.org/10.1007/s00038-010-0216-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00038-010-0216-6