Abstract
Cardiac glycosides (CGs) are a class of bioactive organic compounds well-known for their application in treating heart disease despite a narrow therapeutic window. Considerable evidence has demonstrated the potential to repurpose CGs for cancer treatment. Chemical modification of these CGs has been utilized in attempts to increase their anti-cancer properties; however, this has met limited success as their mechanism of action is still speculative. Recent studies have identified the DNA damage response (DDR) pathway as a target of CGs. DDR serves to coordinate numerous cellular pathways to initiate cell cycle arrest, promote DNA repair, regulate replication fork firing and protection, or induce apoptosis to avoid the survival of cells with DNA damage or cells carrying mutations. Understanding the modus operandi of cardiac glycosides will provide critical information to better address improvements in potency, reduced toxicity, and the potential to overcome drug resistance. This review summarizes recent scientific findings of the molecular mechanisms of cardiac glycosides affecting the DDR signaling pathway in cancer therapeutics from 2010 to 2022. We focus on the structural and functional differences of CGs toward identifying the critical features for DDR targeting of these agents.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiac glycosides (CGs) have traditionally been used to treat congestive heart failure and arrythmia; however, their pharmacological applications have been extended to other diseases including cancer, viral infection, inflammation, neurological, and autoimmune diseases [2,3,4,5]. The first therapeutic utility of CGs in cancer was reported in 1967 [6]. A decade later, Stenkvist et al. observed tumor reduction in breast cancer patients that had taken digoxin [7]. The study also noted that these patients had a lower risk of recurrence. Since then, the anti-cancer properties of CGs have generated considerable interest [8,9,10,11,12]. This includes a dramatic increase in the number of in vitro and in vivo studies evaluating the effects of cardiac glycosides on the inhibition of various types of cancer, demonstrating the ability to block cancer cell proliferation and subsequently cause cell death [13,14,15,16,17].
CGs belong to a class of diverse, naturally occurring bioactive compounds that are structurally comprised of a steroid core bound to a lactone ring at C17 and a sugar group at C2 (Fig. 1a). These structural motifs serve a critical purpose in the function of the compound by influencing the binding affinity, pharmacokinetics, and pharmacodynamics of the molecule [18,19,20]. The development of novel structural modifications and assessing their impact on function is essential in designing more potent anti-cancer CGs.
However, as important as investigating the structure–activity relationships (SARs) is in advancing CGs as potential anti-cancer drugs, understanding their molecular mechanism in biological systems is equally important. Unfortunately, the mechanism of cytotoxicity in cancer cells upon treatment with CGs has not yet been fully elucidated. Furthermore, while numerous studies have shown that CGs increase the sensitivity of cancerous cells when used in combination with current cancer therapies [14, 21, 22], the mechanisms of these drug–drug interactions are still not known. While these studies have provided treatment regimens to address drug resistance to first-line therapeutic drugs like cisplatin, how they achieve this synergy is just beginning to be elucidated. Therefore, there is a critical need to understand the anti-cancer mechanism of CGs both as single agents and in combination with existing therapies.
There have been several anti-cancer mechanisms of CG action reported in different cancer models. Prassas and Diamandis showed that the CGs inhibit Na+/K+ ATPase or activate the oncogenic Ras pathway which results in the generation of reactive oxygen species (ROS) and subsequent cell death [23]. Other modes of action explored include inhibiting the phosphatidylinositol 3-kinase (PI3K) pathway [24], activating endoplasmic reticulum stress, inhibiting hypoxia inducible factor 1 alpha (HIF-1α), and extracellular signal-regulated kinase 1/2 (ERK1/2) signaling pathway [25]. Growth signaling pathways have also been shown to be modulated by CG treatment with inhibition of the STAT-3 pathway [15, 26], increasing forkhead box O1 (FOXO1) expression [27], inhibiting NF-κB [16] OBJ, and activating MAPK-Nu77 signaling pathway [28]. Finally, effects on transcription, splicing, and translation have also been reported [29]. Multiple studies implicate the DNA damage response (DDR), and reduced expression of DNA repair proteins and kinases has been reported with GC treatment [30, 31], and interactions with the ubiquitin-like with PHD and RING finger domains protein 1 (UHRF1) [32]. More recently, Zhou et al. reported that a synthetic CG induces parthanatos via overexpression of poly-ADP ribose polymerase (PARP) and poly-ADP ribose (PAR) which are triggered by DNA damaging agents [33]. Our particular interest is in understanding their mode of action in the DDR signaling space as this is a common pathway dysregulated in cancer cells which holds considerable potential for therapeutic intervention [34,35,36].
The efficacy of many existing cancer therapeutics relies on the induction of DNA damage to kill cancer cells. DNA damage repair is activated to maintain genomic stability after DNA damage occurs. The DDR pathway is a signaling network that mediates DNA repair, damage tolerance processes, and cell cycle checkpoint pathways [37]. Hence, targeting and inhibiting the DDR pathway is a viable strategy in cancer therapy due to the reliance of cancer cells on DDR to mitigate the effects of replication stress. The anti-cancer activity of CGs has been demonstrated in some studies to target the DDR by regulating the expression and activity of certain proteins and kinases in the pathway to drive cancer cells into cell cycle arrest, apoptosis, or autophagy-dependent cell death [32, 38].
There is no record of a detailed summary featuring the mechanistic activity of CGs solely focusing on the DDR in the number of review publications outlining the progress of the anti-cancer mechanism of CGs [12, 39,40,41,42,43,44,45,46]. Therefore, this review will highlight the possible anti-cancer mechanisms affecting the DDR pathway that have been reported for different cardiac glycosides from 2010 to date in different cancers. We will focus on CG-induced DDR or DNA repair. Current advances and perspectives on the structural function in different CGs driving this activity will also be discussed. The scope of these molecules will be limited to glycosides with any backbone, including cardenolide or bufadienolide (Fig. 1b), as these have been the most well studied. Other steroidal compounds such as k-strophthadithin, antiarigenin, bufalin, and periplogenin will not be discussed as there are recent reviews covering this material [47, 48].
Structural function and physicochemical properties of CGs
The diversity of the structural size and chemical features of the various CGs illustrated in Fig. 2 begs the question: What are the important features that dictate different effects on cellular function? Cardiac activity is largely driven by interactions with the Na+/K+ ATPase, but the specific macromolecular targets for impacting cancer cell proliferation are still unknown.
Oleandrin is a derivative of odoroside A that possesses an acetate group at the C16 position of the aglycone that is absent in odoroside A (Fig. 2, blue highlight). As demonstrated by the activity of the two compounds, oleandrin displays a better cancer proliferation inhibitory activity than odoroside A [13]. The difference in activity of these two compounds can also be attributed to the difference in stereochemistry of the sugar moiety (Fig. 2, orange highlight). Additionally, the presence of the acetate group can increase the lipid solubility of the compound that consequently results in an enhanced chemical penetration through cellular membranes [13].
The structural motif of ouabain, cerberin, reevesioside A, and Antiaris toxicaria 2 (AT2) is similar to that of odoroside A. Ouabain has hydroxyl groups at the C4, C14, and C23 positions in place of protons as in the odoroside A. In addition to the differences in stereochemistry around the carbons in the sugar moiety, ouabain, like AT2, possesses additional hydroxyl groups around the sugar moiety (Fig. 2, green highlight). Conversely, cerberin and reevesioside A are sufficiently hydroxyl deficient. Cerberin has only one hydroxyl group in the monosaccharide with a couple of hydroxyl groups protected, whereas reevesioside A has no hydroxyl functional groups attached on the sugar moiety. However, reevesioside has a heterocyclic acetal bound to the sugar group. Furthermore, reevesioside A is modified at R2 with an aldehyde at position 23, differing from the other glycosides that have a methyl or hydroxyl group in that position. While each of these CGs have been demonstrated to possess anti-cancer activity, the SAR of these different glycosides has not been investigated in a single model. Thus, conclusive statements comparing their activity are difficult. However, we can predict a trend from a purely theoretical structural analysis of these CGs in the increasing order of lipid solubility, i.e., ouabain < AT2 < odoroside A ≤ cerberin < reevesioside A < oleandrin.
HTF-1 is a glycosidic molecule extracted and purified from Helleborus thibetanus Franch (HTF) plant [49]. HTF-1 is different from the other glycosides as it is the only bufadienolide. Bufadienolides have a pyrone ring at C17 whereas cardenolides have a furanone. Each of these compounds possesses some degree of anti-cancer activity suggesting that additional modification around C17 could be pursued to optimize this activity.
Catalpol is an iridoid glycoside found in Rehmannia glutinosa. It is comprised of a cyclopentane-pyran bound by a glycosidic bond to a glucose molecule. The activity of this compound, like other more known CGs, spans across multiple biological functions such as neurodegenerative diseases, diabetes, inflammation, and cancer [50]. Structurally, catalpol is drastically different from the conventional cardiac glycosides. Liu et al. [51] demonstrated that catalpol can influence the generation of reactive oxygen species (ROS) just as effectively as odoroside A or oleandrin. Structural analysis of these CGs postulates that the sugar moiety might be more responsible for ROS generation than the steroid core. This induction of ROS as well as DNA damage are common themes that will be discussed below as potential mechanism of CG-induced anti-cancer activity.
Digoxin, digitoxin, and lanatoside C possess n-sugar molecules. The significance of multiple sugar molecules was highlighted by Wang et al. [52]. In this study, the authors showed that cytotoxicity of cancer cells was better achieved by shortening the sugar chain. While multiple sugars would increase the overall solubility of the compound, it would lower its lipid solubility. This would affect the molecule’s membrane transport ability, consequently lowering its bioavailability in the cells/tumors. Compared to digitoxin, digoxin possesses a hydroxyl group at the C13 position instead of a proton (Fig. 2, pink highlight). Lanatoside C possesses four monosaccharides (Fig. 2). Like other glycosides with similar structural features, an examination of this position in digitoxin and digoxin would be worthwhile in understanding its function in CGs structures.
The above discussed glycosides have varying degrees of hydroxylation. Clearly, hydroxylation is an important motif in CGs that also needs to be addressed. As previously noted, lipid solubility has to be taken into account in order to ensure their absorption in cells and the body; therefore, some level of hydrophobicity must also be achieved. So, the questions we ask are: hat is an appropriate amount of hydroxylation? Also, is it relevant if hydroxylation is centered around the steroid frame instead of the sugar moiety? All the CGs except for ouabain (Fig. 2) show minimal hydroxylation on the steroid frame. But, if the vast interests and current applications of ouabain in research are any indication [24, 30, 53,54,55], hydroxylation of the steroid core might be an avenue worth exploring. However, one of the challenges with these bioactive compounds is the limited opportunity for functionalization, especially on the steroid core. Even in publications where a complete construction of the steroid core has been reported, a minimal degree of hydroxylation/oxygenation was achieved [19, 56, 57].
Mechanism of CGs via DNA damage signaling
Activation of DNA damage sensors
DNA discontinuities are sensed by a series of proteins that then signal to regulate downstream effectors and pathways involved in DNA repair, cell cycle, and cell death. Ataxia-telangiectasia mutated (ATM) and DNA-dependent protein kinase (DNA-PK) are the two primary protein kinases that signal the presence of DNA double-strand breaks (DSBs). ATM is recruited by the MRE11-RAD50-NBS1 (MRN) DSB sensor, while DNA-dependent protein kinase catalytic subunits (DNA-PKcs) is recruited by the Ku70/80 heterodimer DSB sensor. Excess single-strand DNA associated with stalled replication forks is sensed by replication protein A (RPA) which signals to the ATM and Rad3-related (ATR) kinase, while single-strand breaks are sensed and signaled by PARP. CGs’ have been shown to impact each of these proteins. The CG ouabain has been studied as a potential anti-cancer agent in a variety of systems. A recent study demonstrated that ouabain can promote cytotoxicity in U2OS osteosarcoma cells via apoptotic cell death [55]. Another study validated this observation and implicated the DDR pathway [30]. Experiments performed using the comet assay and DNA electrophoresis revealed that ouabain induces DNA breaks and DNA fragmentation [30]. The authors also reported increased phosphorylation and expression of several DNA damage proteins such as ATM, ATR, p53, γ-H2A histone family member X (γ-H2AX), mediator of DNA damage checkpoint 1 (MDC-1), PARP, and breast cancer gene 1 (BRCA1) (Fig. 3). Additionally, Ouabain treatment suppressed the levels of DNA-PK and methylguanine methyltransferase (MGMT) gene expression as well as the phosphorylation of mouse double minute 2 (MDM2). The effect of ouabain on the signaling of ATM and ATR pathways is suggestive of CG-induced DSB and single-strand break (SSB) DNA damage. The limitation of this paper is the single time point (48 h after treatment) used in all the studies. Therefore, it is impossible to determine if the breaks measured were the direct effects of ouabain on DNA, an indirect effect on DNA and altered DDR, or simply the DNA fragmentation by the apoptotic nucleases and inconsequential changes in the DDR proteins of dying cells.
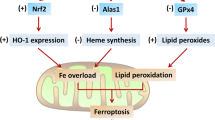
[1] DDR sensors and signaling. DNA damage including DSBs and SSBs, have been found following treatments with different CGs. (yellow = increased expression, pink = decreased expression) As such, upstream DNA repair proteins including PARP, ATM, ATR, and DNA-PK are recruited by DNA damage sensors RPA, MRN and Ku protein which triggers DDR signalling
A more recent study of ouabain on different cancer cells performed time course studies and demonstrated increased ROS and DNA damage at time points before apoptosis [36]. A convincing study for a more direct effect was reported with CG (digitoxin) and HeLa cervical cancer cells, which reported induction of γ-H2AX at times before apoptotic chromosomal degradation [58]. They reported cell cycle alterations in the G2/M phase, and activation of the DDR pathway. This was notably marked by the phosphorylation of ATM and ATR. This study showed activation of the checkpoint kinases (Chk1 and Chk2) in addition to downregulation of cell division cycle 25C (Cdc25C). The evaluation of effector proteins, i.e., cyclin-dependent kinase 1 (CDK1) and cyclin B1 of the G2/M cell cycle phase was performed, and the results showed elevated levels of cyclin B1 while those of CDK1 declined. The investigation of digitoxin activity in this cell model provided evidence for activation of the mitochondrial apoptosis. This demonstration of early and potentially direct induction of DNA damage and activation of the DDR by a CG provides an explanation for the ability to combine with other DNA damaging therapeutics to enhance tumor cell killing.
The CG oleandrin has been shown to induce DNA damage in non-small cell lung cancer (NSCLC) A549 adenocarcinoma cells as measured by surrogate markers including RPA and γ-H2AX foci [31]. To examine what type of DNA damage repair is engaged in this oleandrin-induced apoptosis, the expression of Rad51 and X-ray repair cross-complementing protein 1 (XRCC1) was investigated. Rad51 and XRCC1 are markers of the repair of damaged DSBs and single-strand breaks (SSBs), respectively. Rad51 is a central catalyst in the homologous recombination (HR) pathway that protects stalled replication forks and mediates DSB repair. XRCC1 interacts with DNA ligase III and ligase I to facilitate SSB repair and base excision repair. The suppression of Rad51 was observed when cancer cells were treated with oleandrin, suggesting that the DSBs induced by oleandrin were likely not repaired by HR pathway, thereby resulting in cancer cell death. Conversely, the expression of XRCC1 was elevated which is indicative of activated XRCC1-induced SSB DNA repair.
Activation of DNA repair sensors in combination studies with DNA damaging agents
In addition to single agent CG treatment demonstrating effective anti-cancer activity, combination studies have also been investigated in a few systems combining CGs with DNA damaging therapeutics including cisplatin, mitomycin C, camptothecin, and ionizing radiation (IR) [14, 21, 22, 32, 53, 59]. The targets again remain elusive, though combination treatments show impressive activity in a variety of cancer models.
Fanconi anemia (FA)/BRCA is a DNA repair pathway that is activated in response to DNA intrastrand crosslinks (ICLs). When the DNA repair process is activated in response to DNA damaging agents, the efficacy of the cancer treatment can be negatively affected, which in the long run could result in the development of drug resistance. This makes inhibition of the DNA repair pathway an attractive approach for enhancing the effectiveness of DNA damaging cancer therapeutics. In studies investigating the impact of CGs on FA/BRCA signaling in U2OS osteosarcoma cells, Jun et al. identified ouabain as a strong candidate for targeting this pathway [53]. The study demonstrated that this CG affected the protein expression of FANCD2 by transcription repression. The factors FANCF and excision repair cross-complementation group 4 (ERCC4) were repressed whereas the messenger ribonucleic acid (mRNA) levels of FANCA, Rad51, XRCC5, and XRCC6 remained constant. Comparable experiments performed with other CGs (digitoxin and digoxin) in this study showed similar activity to ouabain, demonstrating that the inhibition of FA/BRCA can be achieved with other CGs [53]. The mechanistic action of ouabain revealed the activation of p38 in its inhibitory function. The effect of ouabain was found to promote G2/M phase arrest only at high drug concentration. However, no effect was noted on the cycle progression at low concentration unless an ICL-inducing agent was present, at which point the S phase arrest was observed.
Lee et al. showed that digoxin not only enhanced DNA damage following IR treatments, but also reduced the levels of DNA repair proteins [60]. The study reported reduced expression and levels of Rad51, ERCC1, BRCA2, Ku70, Ku86, and DNA-PKcs in A549 cells but not H460 cells. These results suggested that digoxin inhibited the HR and non-homologous end joining (NHEJ) repair pathways in radioresistant A549 cells but not in radiosensitive (H460) cells. More recently, Wang and coworkers probed the anti-cancer activity of digoxin as a single agent and in combination with doxorubicin in NSCLC cell lines A549 and H1299 [59]. In their study, DNA damage and elevated ROS levels were detected after treatment with digoxin. The effect of this treatment on Rad51 and γ-H2AX expression resulted in an increase of γ-H2AX foci while inhibiting Rad51. Digoxin enhanced the expression of RPA and suppressed that of XRCC1. These results suggest that digoxin may inhibit the repair of SSBs and DSBs, though no direct measures of repair were reported. The complexity of the DDR and repair pathway necessitates measurements of repair proteins as expression levels are not an accurate measure of activity with many of the repair components being regulated by post-translational modifications. Tian et al. showed that AT2 was effective in combination with camptothecin, a DNA damaging agent that signals through Chk1 [32]. AT2 was shown to inhibit Chk1 activation and sensitize cells to a wide variety of clinically available chemotherapeutic drugs. The protein target of AT2 was identified as UHRF1 by quantitative mass spectrometry. UHRF1 is a multifunctional protein with roles in epigenetic maintenance and as a DNA damage sensor. Building upon that, we recently reported a series of chemical modifications of AT2 and their effects on impacting chemotherapy sensitivity in a lung cancer model [38], revealing innovative insights into the structure of CGs in inhibiting the DDR and DSB repair.
Stress-activated signaling
The c-Jun N-terminal kinase (JNK) is one of the major DNA damage-activated protein kinases [61, 62]. This signaling pathway is triggered by both DNA damage and oxidative stress. JNK belongs to the mitogen-activated protein kinases (MAPK) family and promotes the phosphorylation of p53 that is also activated in the DDR process [63]. Activation of JNK triggers the upregulation of B-cell lymphoma-2 (Bcl-2) which inhibits the autophagy-inducing Beclin-1/PI3K-complex. Research involving CGs has demonstrated that JNK signaling can be stimulated as a result of treatment with CGs like HTF-1 and ouabain [49, 54]. Du and co-workers also reported the increased generation of ROS with CG treatment [36]. ROS are reactive oxygen species resulting from cellular oxidative metabolism and while they play a crucial role in several cellular signaling pathways, they can also provoke metabolic dysfunction. The mechanism by which ROS is generated is dependent on the specific sub-cellular compartment or organelle. ROS in the cytoplasm is formed using NADPH oxidase (NOX) proteins through nicotinamide adenine dinucleotide phosphate (NADPH) electron exchange [64]. In the mitochondria, ROS are created via oxygen interaction with flavin mononucleotide (FMN) [65] and reverse electron transfer (RET) [66]. ROS in the peroxisome is produced using oxidant scavenger enzymes which transfer electrons to water molecules to form hydrogen peroxide. An in-depth review article of ROS generation and their function in metabolic signaling is presented by Forrester and colleagues [67]. ROS can induce oxidative DNA damage and influence the DDR. Elevated levels of ROS can also increase the permeability of the outer membrane of mitochondria, inducing the release of pro-apoptosis factors.
The increased levels of ROS and the induced DNA damage as an effect of CG treatment resulted in activation of the JNK signaling pathway [36]. In their work, Hu and co-workers demonstrated that CGs (odoroside A and oleandrin) suppress the growth of acute myeloid leukemia (AML) cells by increasing the production of ROS which activates the phosphorylation of JNK [13]. This, consequently, triggered light chain 3B (LC3B) and caspase-9/caspase-3 that induce autophagy and apoptosis, respectively. The implication of caspase activation has also been investigated by other research groups [68]. Furthermore, these CGs inhibited the expression of Bcl-2 and matrix metalloproteinase (MMP) (Fig. 4). Bcl-2 is an anti-apoptotic gene and tumor promoter whose overexpression can inhibit the pro-apoptotic signal in cancer cells [69]. So, by deactivating Bcl-2, CGs can block Bcl-2-mediated DNA repair that is typically associated with genomic instability [70].
[1] CGs and ROS signaling. CGs trigger the production of ROS and DNA damage. A culmination of all or part of these consequences activate different signaling pathways; PI3K (purple), p53 (green) and JNK (blue)
The role of CGs in the ROS formation and activity in apoptosis and autophagy has been extensively reported [13, 71,72,73]. Calderón-Montaño et al. reported that a Nerium oleander extract (NOE)-induced levels of ROS were significantly higher than the basal levels [21]. Additional experiments showed that ROS contributed to the cytotoxicity of NOE in lung cancer, colon cancer, and melanoma cells, albeit a minor role. Furthermore, cell treatment with NOE was shown to trigger DNA damage. A recent work demonstrated that ROS generation also mediated mitochondria apoptosis in breast cancer [51]. The study reported that catalpol not only inhibited the proliferation and growth of MCF-7 cells, but reduced the tumor volume in a xenograft model of breast cancer. The treatment with CG resulted in a decrease in MMP protein and an increase in ROS as well as levels of caspase-3 and cytochrome C (cytC). The upregulated levels of caspase-3 and cytC are indicative of mitochondrial apoptosis. Similar activity by oleandrin was also observed in colorectal cancer [74]. The results reported an upregulation of cytC and Bcl-2-associated X (Bax) protein that subsequently caused a downregulation of Bcl-2.
ROS-mediated DNA damage has also been shown to activate p53 signaling [75]. p53 is a tumor suppressor transcription factor that, when triggered, promotes the expression of kinases involved in apoptosis and cell cycle arrest. In their work, Chen et al. showed that CGs can promote G2/M cell cycle arrest and apoptosis via central events in the p53/ROS pathway. The increased population of cells in the G2/M phase is indicative of DNA damage [76]. Following treatment with odoroside A, an enhanced production of ROS was observed with suppressed expression of mutated p53. The reduced expression of mutated p53 not only caused apoptosis but also incited cell cycle arrest. Apoptosis was evidenced by an increase in expression of Bax, cleaved caspase-3, increase in cytC, and a noticeable decline of Bcl-2 (Fig. 4). The G2/M phase of the cell cycle arrest was shown to be activated by mutated p53 via regulation of p21 and cyclin/CDK complexes.
PI3K/Akt/mTOR activated by CG-induced DNA damage
As one of the main growth regulatory pathways in both normal and cancerous cells [13], it is not surprising that the PI3K/Akt/(mammalian target of rapamycin) mTOR pathway (referenced as PI3K pathway) is influenced by the activity of CGs. Hyperactivated signaling of PI3K stimulates proliferation and reduces apoptosis in cancer, whereas inhibiting mTOR reduces cellular survival [77]. The cell survival pathways promoted by PI3K signaling is partly a function of impacting DDR [78]. This signaling pathway has also been implicated in DNA replication which suggests that inhibition of PI3K induces replication stress that consequently triggers DDR [79].
Studies showed that digoxin suppressed the cell cycle in the G2/M phase. While a study by Lindholm et al. [80] demonstrated that digitoxin had no effect on the signaling of PI3K/Akt pathway in numerous pancreas cancer cell lines, the majority of studies suggest a negative effect of CGs on the Akt/mTOR pathway. Treatment with digoxin inhibited the phosphorylation and expression of Akt and mTOR proteins in leukemia cell lines [81]. Although no evaluation was performed on the PI3K downstream factors, the observed apoptosis, cell cycle arrest, and subsequent suppressed progression of different cancers [77, 81] imply that mTOR downstream factors that cause apoptosis and cell death must have been activated by treatment with CGs. The downregulation of the PI3K pathway signaling was consistent with the work reported by others using cerberin, reevesioside A, and HTF-1 in different cancer cell lines [49, 82, 83]. The downregulation of components in this signaling pathway by CGs implicate them in triggering replication stress which leads to genomic instability and DNA damage.
In a different study, lanatoside C was shown to promote the upregulation of tumor suppressor genes (PTEN and p53). However, Akt, PI3K, mTOR, c-MYC, p62, LC3, beclin-1, and several cell cycle regulating protein kinases that include Chk1, Chk2, CDK6, and cyclin D1 were downregulated (Fig. 4) [84]. Furthermore, treatment with this CG also activated mitochondria-mediated apoptosis, G2/M cell cycle arrest and inhibited autophagy in breast, liver, and lung cancers. The results from this study also implicated lanatoside C in the activation of other signaling pathways such as JAK-STAT and Wnt/β-catenin that are involved in tumorigenesis.
Activation of c-MYC/E2F
A non-apoptotic cancer cell death via disruption of the structure and function of the cell nucleus, downregulation of c-myc expression, and damage of cyclin-dependent kinases using a commercially available CG, UNBS1450, was an earlier plausible anti-tumor mechanism [85]. Cellular myelocytomatosis (c-MYC) is a transcription factor that plays a crucial role in cell growth, proliferation, and apoptosis. Overexpression of this gene induces oxidative DNA damage by increasing cellular metabolism and mitochondrial biogenesis [86]. Reevesioside A was found to cause mitochondrial damage and block cell proliferation in prostate cancer cell lines [83]. The activity of reevesioside A caused elevated E2F1 expression that is believed to be a result of DNA damage. This is suggestive of a reevesioside A-induced DNA damage. Even more relevant would have been an investigation of the DNA damage and the ROS content as exhibited by the action of this glycoside. The authors showed that reevesioside A downregulated the protein levels of c-myc as well as the expression of c-myc mRNA levels. This study further demonstrated that this CG could stall cell cycle progression at G1 phase by decreasing levels of cyclin D and CDC25A. The downregulation of c-myc using digoxin in triple negative breast cancer (TNBC) cells was also observed by Howard et al. [87]. This work further demonstrated that the inhibition of c-myc would result in reduced levels of eukaryotic initiation factor 4A-1 (eIF4A1).
Perspective and conclusion
There has been a considerable increase in the investigation of the anti-cancer properties of cardiac glycosides, and several reports have provided insight into the anti-cancer mechanism of these compounds. As we have demonstrated above and summarized in Table 1, different signaling mechanisms are triggered when treatments with different CGs are made in different tumor cells. Without a doubt, we believe that the mechanism of anti-cancer action of CGs is likely a coalition of various signal transduction pathways. By analyzing and understanding these signaling pathways, we will be able to develop more targeted CG-mediated cancer therapies.
Some of the most effective existing cancer therapeutics target DNA damage and the DDR pathway. Hence, it is not surprising that many studies of CG’s mechanistic role implicate DNA damage or repair. DNA damage and DDR signaling are promising targets for drug discovery because of their role in the progression and response in cancer therapy. Several studies have recognized the utility of CGs as potential agents that can increase the sensitivity of different cancer cells to other cancer therapies such as IR, doxorubicin, and cisplatin to mention a few [14, 32, 59, 77, 88]. This is an important stride in overcoming drug resistance and increasing the efficacy of these therapeutics. CGs have also been shown to cause various types of DNA damage such as DSBs, SSBs, and ICLs, whereas some forms of damage are exacerbated by the formation of ROS [13, 30, 31, 53]. Once induced, DNA damage activates signaling kinases that trigger responses including transcription, cell cycle arrest, and apoptosis. Additionally, CGs have been implicated in engaging the DNA repair pathways. For these reasons, it is important to closely investigate the activity of CGs in the DNA damage space.
Each of the four structural features (i.e., sugar moiety, glycosidic link, steroid frame, and lactone ring) of CGs have been identified to play a significant role in driving the efficacy of the compound from increasing the lipid solubility to serving a particular function, e.g., initiating apoptosis [52, 89]. However, using the evidence accrued from evaluation of the mechanistic activity of the different CGs discussed above, it is difficult to assign each structural motif to any particular function. What we can discern from this investigation are additional questions that must first be addressed to recommend new structural designs of CGs that are more potent. A degree of lipophilicity is necessary for the lipid solubility of these molecules; Does it matter if the hydroxylation is around the steroid core versus the sugar moiety? What is the role of the lactone? Is the unsaturation of that lactone ring relevant? How does the glycosidic link promote apoptosis? These questions can only be answered following a systematic SAR to identify the suitable features of CGs that enhance their activity. Our groups and several others have published different SAR results [20, 38, 52, 90]. However, a comprehensive investigation would be necessary to not only identify relevant structure moieties, but also discern which signaling pathways are activated and consequently trigger other pathways.
A key challenge in the successful development of glycosides as DDR inhibitors might arguably be their lack of specificity. The inherent complexity of the network of DNA damage signaling kinases and proteins is not the only obstacle. As discussed above, the glycoside-induced DNA damage and repair can trigger other signaling pathways such as growth factors, stress, and transcription [14, 24, 25, 84]. Consequently, we cannot exclude the possibility of an interplay of these signaling kinases as there are numerous studies of crosstalk (direct or indirect) between these pathways [91, 92]. To increase specificity, we must examine the role of these CGs in regulating signaling pathways. Only then can we begin to (1) identify the relevant targets to focus on and (2) design potent CGs for a specific function.
While we have provided a comprehensive analysis of the relevant data from which we can draw conclusions, we have to emphasize that there remain many unanswered questions. Definitive proof of the complete signaling pathways to explain the different mechanisms in the different cancers is lacking. We have explored and discussed the multiple DNA damage and DNA repair regulation proteins influenced by different CGs. However, we need more studies with various CGs to fully comprehend the mechanistic impact of CGs in activating these DDR-related proteins in order to allow the application and our understanding of these basic studies to direct and guide their clinical utility in cancer treatment.
Data availability
Not applicable.
Abbreviations
- Akt:
-
Protein kinase B
- AML:
-
Acute myeloid leukemia
- AT2:
-
Antiaris toxicaria 2
- ATM:
-
Ataxia-telangiectasia mutated
- ATR:
-
ATM and Rad3-related
- Bax:
-
Bcl-2-associated X-protein
- Bcl-2:
-
B-cell lymphoma-2
- BRCA1:
-
Breast cancer gene 1
- Cdc25C:
-
Cell division cycle 25C
- CDK1:
-
Cyclin-dependent kinase 1
- CG:
-
Cardiac glycoside
- CGs:
-
Cardiac glycosides
- Chk1:
-
Checkpoint kinase 1
- Chk2:
-
Checkpoint kinase 2
- c-MYC:
-
Cellular myelocytomatosis
- cytC:
-
Cytochrome C
- DDR:
-
DNA damage response
- DSBs:
-
Double-strand break
- DNA-PK:
-
DNA-dependent protein kinase
- E2F1:
-
E2F transcription factor 1
- eIF4A:
-
Eukaryotic initiation factor 4A-1
- ERCC4:
-
Excision repair cross-complementation group 4
- ERK1/2:
-
Extracellular signal-regulated kinase ½
- FA:
-
Fanconi anemia
- FANCA:
-
Fanconi anemia group A
- FANCD2:
-
Fanconi anemia group D2
- FANCF:
-
Fanconi anemia group F
- FMN:
-
Flavin mononucleotide
- FOXO1:
-
Forkhead box O1
- γ-H2AX:
-
γ-H2A histone family member X
- HIF-1α:
-
Hypoxia-inducible factor 1 alpha
- HR:
-
Homologous recombination
- HRR:
-
Homologous recombination repair
- JNK:
-
C-Jun N-terminal kinase
- ICLs:
-
Intrastrand crosslinks
- IR:
-
Ionizing radiation
- LC3B:
-
Light chain 3B
- MAPK:
-
Mitogen-activated protein kinases
- MDC-1:
-
Mediator of DNA damage checkpoint 1
- MDM2:
-
Mouse double minute 2
- MGMT:
-
Methylguanine methyltransferase
- MMP:
-
Matrix metalloproteinase
- MRN:
-
MRE11-RAD50-NBS1
- mRNA:
-
Messenger ribonucleic acid
- mTOR:
-
Mammalian target of rapamycin
- NADPH:
-
Nicotinamide adenine dinucleotide phosphate
- NHEJ:
-
Non-homologous end joining
- NOE:
-
Nerium oleander Extract
- NOX:
-
NADPH oxidase
- NSCLC:
-
Non-small cell lung cancer
- PAR:
-
Poly-ADP ribose
- PARP:
-
Poly-ADP ribose polymerase
- PI3K:
-
Phosphatidylinositol 3-kinase
- RET:
-
Reverse electron transfer
- ROS:
-
Reactive oxygen species
- RPA:
-
Replication protein A
- SAR:
-
Structure–activity relationship
- SSBs:
-
Single-strand break
- TNBC:
-
Triple negative breast cancer
- UHRF1:
-
Ubiquitin like with PHD and RING finder domains 1
- UNBS1450:
-
1R,3aS,3bR, 5aS,6aR,7aS,9R,12aR,13aR,15aR] -3a,11a-dihydroxy-13a-(hydroxymethyl)-9,15a-dimethyl-1-(5-oxo-2, 5-dihydrofuran-3-yl)icosahydro-1H,4′H-spiro[cyclopenta [7, 8]phenanthro[2,3-b]pyrano[3,2-e][1,4]dioxine-11,2′-[1, 3] thiazolidin]-4′-one
- XRCC1:
-
X-ray repair cross-complementing protein 1
- XRCC5:
-
X-ray repair cross-complementing protein 5
References
Created with BioRender.com.
Ren J, Gao X, Guo X, Wang N, Wang X (2022) Research progress in pharmacological activities and applications of cardiotonic steroids. Front Pharmacol 13:902459–902459. https://doi.org/10.3389/fphar.2022.902459
Škubník J, Pavlíčková V, Rimpelová S (2021) Cardiac glycosides as immune system modulators. Biomolecules 11:659. https://doi.org/10.3390/biom11050659
Jansson D, Dieriks VB, Rustenhoven J, Smyth LCD, Scotter E, Aalderink M, Feng S, Johnson R, Schweder P, Mee E, Heppner P, Turner C, Curtis M, Faull R, Dragunow M (2021) Cardiac glycosides target barrier inflammation of the vasculature, meninges and choroid plexus. Commun Biol 4:260. https://doi.org/10.1038/s42003-021-01787-x
El-Seedi HR, Khalifa SAM, Taher EA, Farag MA, Saeed A, Gamal M, Hegazy MF, Youssef D, Musharraf SG, Alajlani MM, Xiao J, Efferth T (2019) Cardenolides: insights from chemical structure and pharmacological utility. Pharmacol Res 141:123–175. https://doi.org/10.1016/j.phrs.2018.12.015
Shiratori O (1967) Growth inhibitory effect of cardiac glycosides and aglycones on neoplastic cells: in vitro and in vivo studies. Gan 58:521–528
Stenkvist B, Bengtsson E, Eriksson O, Holmquist J, Nordin B, Westman-Naeser S, Eklund G (1979) Cardiac glycosides and breast cancer. Lancet 313:563. https://doi.org/10.1016/S0140-6736(79)90996-6
Haux J (1999) Digitoxin is a potential anticancer agent for several types of cancer. Med Hypotheses 53:543–548. https://doi.org/10.1054/mehy.1999.0985
Haux J, Klepp O, Spigset O, Tretli S (2001) Digitoxin medication and cancer; case control and internal dose-response studies. BMC Cancer 1:11. https://doi.org/10.1186/1471-2407-1-11
Winnicka K, Bielawski K, Fau - Bielawska A Bielawska A (2006) Cardiac glycosides in cancer research and cancer therapy. Acta Pol Pharm Drug Res 63:6
Newman RA, Yang P, Pawlus AD, Block KI (2008) Cardiac glycosides as novel cancer therapeutic agents. Mol Interv 8:36–49. https://doi.org/10.1124/mi.8.1.8
Diederich M, Muller F, Cerella C (2017) Cardiac glycosides: from molecular targets to immunogenic cell death. Biochem Pharmacol 125:1–11. https://doi.org/10.1016/j.bcp.2016.08.017
Hu X, Chen T, Zhang S, Zhang Q, Li C, Wang X (2022) Antitumour effect of odoroside A and its derivative on human leukaemia cells through the ROS/JNK pathway. Basic Clin Pharmacol Toxicol 130:56–69. https://doi.org/10.1111/bcpt.13673
Yong L, Ma Y, Zhu B, Liu X, Wang P, Liang C, He G, Zhao Z, Liu Z, Liu X (2018) Oleandrin synergizes with cisplatin in human osteosarcoma cells by enhancing cell apoptosis through activation of the p38 MAPK signaling pathway. Cancer Chemother Pharmacol 82:1009–1020. https://doi.org/10.1007/s00280-018-3692-7
Ko YS, Rugira T, Jin H, Park SW, Kim HJ (2018) Oleandrin and Its derivative odoroside A, both cardiac glycosides exhibit anticancer effects by inhibiting invasion via suppressing the STAT-3 signaling pathway. Int J Mol Sci. https://doi.org/10.3390/ijms19113350
Li R-Z, Fan X-X, Duan F-G, Jiang Z-B, Pan H-D, Luo L-X, Zhou Y-L, Li Y, Yao Y-J, Yao X-J, Leung EL-H, Liu L (2018) Proscillaridin A induces apoptosis and suppresses non-small-cell lung cancer tumor growth via calcium-induced DR4 upregulation. Cell Death Dis 9:696–696. https://doi.org/10.1038/s41419-018-0733-4
Francischini CRD, Mendonça CR, Barcelos KA, Silva MAM, Botelho AFM (2022) Antitumor effects of oleandrin in different types of cancers: systematic review. Toxicon 216:15–27. https://doi.org/10.1016/j.toxicon.2022.06.010
Zhou X, Chen L, Jiang Z-H, Chen X, Luo P, Bai L-P (2019) Synthesis of 21-Alkylidenes and 21-Alkylol Analogues of Uscharin and their effects on intracellular calcium in cardiac cells. ChemistrySelect 4:5512–5517. https://doi.org/10.1002/slct.201900108
Khatri HR, Bhattarai B, Kaplan W, Li Z, Curtis Long MJ, Aye Y, Nagorny P (2019) Modular total synthesis and cell-based anticancer activity evaluation of ouabagenin and other cardiotonic steroids with varying degrees of oxygenation. J Am Chem Soc 141:4849–4860. https://doi.org/10.1021/jacs.8b12870
Surovtseva YV, Jairam V, Salem AF, Sundaram RK, Bindra RS, Herzon SB (2016) Characterization of cardiac glycoside natural products as potent inhibitors of DNA double-strand break repair by a whole-cell double immunofluorescence assay. J Am Chem Soc 138:3844–3855. https://doi.org/10.1021/jacs.6b00162
Calderón-Montaño JM, Burgos-Morón E, Orta ML, Mateos S, López-Lázaro M (2013) A hydroalcoholic extract from the leaves of Nerium oleander inhibits glycolysis and induces selective killing of lung cancer cells. Planta Med 79:1017–1023. https://doi.org/10.1055/s-0032-1328715
Apostolou P, Toloudi M, Chatziioannou M, Ioannou E, Knocke DR, Nester J, Komiotis D, Papasotiriou I (2013) Anvirzel™ in combination with cisplatin in breast, colon, lung, prostate, melanoma and pancreatic cancer cell lines. BMC Pharmacol Toxicol 14:18. https://doi.org/10.1186/2050-6511-14-18
Prassas I, Diamandis EP (2008) Novel therapeutic applications of cardiac glycosides. Nat Rev Drug Discov 7:926–935. https://doi.org/10.1038/nrd2682
Yang XS, Xu ZW, Yi TL, Xu RC, Li J, Zhang WB, Zhang S, Sun HT, Yu ZQ, Xu HX, Tu Y, Cheng SX (2018) Ouabain suppresses the growth and migration abilities of glioma U-87MG cells through inhibiting the Akt/mTOR signaling pathway and downregulating the expression of HIF-1α Corrigendum in /10.3892/mmr.2021.11836. Mol Med Rep 17:5595–5600. https://doi.org/10.3892/mmr.2018.8587
Lee D-H, Cheul OhS, Giles AJ, Jung J, Gilbert MR, Park DM (2017) Cardiac glycosides suppress the maintenance of stemness and malignancy via inhibiting HIF-1α in human glioma stem cells. Oncotarget 8:40233–40245. https://doi.org/10.18632/oncotarget.16714
Li XX, Wang DQ, Sui CG, Meng FD, Sun SL, Zheng J, Jiang YH (2020) Oleandrin induces apoptosis via activating endoplasmic reticulum stress in breast cancer cells. Biomed Pharmacother 124:109852. https://doi.org/10.1016/j.biopha.2020.109852
Zhang L, Liang B, Xu H, Gong Y, Hu W, Jin Z, Wu X, Chen X, Li M, Shi L, Shi Y, Wang Y, Yang L (2022) Cinobufagin induces FOXO1-regulated apoptosis proliferation migration and invasion by inhibiting G9a in non-small-cell lung cancer A549 cells. J Ethnopharmacol 291:115095. https://doi.org/10.1016/j.jep.2022.115095
Hu Q-Y, Zhang X-K, Wang J-N, Chen H-X, He L-P, Tang J-S, Yao X-S, Liu J (2021) Malayoside, a cardenolide glycoside extracted from Antiaris toxicaria Lesch, induces apoptosis in human non-small lung cancer cells via MAPK-Nur77 signaling pathway. Biochem Pharmacol 190:114622. https://doi.org/10.1016/j.bcp.2021.114622
Lu G-Y, Liu S-T, Huang S-M, Chang Y-L, Lin W-S (2014) Multiple effects of digoxin on subsets of cancer-associated genes through the alternative splicing pathway. Biochimie 106:131–139. https://doi.org/10.1016/j.biochi.2014.08.013
Yang J-L, Yang M-D, Chen J-C, Lu K-W, Huang Y-P, Peng S-F, Chueh F-S, Liu K-C, Lin T-S, Chen P-Y, Chen W-J (2021) Ouabain induces DNA damage in human osteosarcoma U-2 OS cells and alters the expression of DNA damage and DNA repair–associated proteins. In Vivo 35:2687. https://doi.org/10.21873/invivo.12552
Bao Z, Tian B, Wang X, Feng H, Liang Y, Chen Z, Li W, Shen H, Ying S (2016) Oleandrin induces DNA damage responses in cancer cells by suppressing the expression of Rad51. Oncotarget 7:59572–59579. https://doi.org/10.18632/oncotarget.10726
Tian D, Tang J, Geng X, Li Q, Wang F, Zhao H, Narla G, Yao X, Zhang Y (2020) Targeting UHRF1-dependent DNA repair selectively sensitizes KRAS mutant lung cancer to chemotherapy. Cancer Lett 493:80–90. https://doi.org/10.1016/j.canlet.2020.08.008
Zhou M, Boulos JC, Klauck SM, Efferth T (2023) The cardiac glycoside ZINC253504760 induces parthanatos-type cell death and G2/M arrest via downregulation of MEK1/2 phosphorylation in leukemia cells. Cell Biol Toxicol. https://doi.org/10.1007/s10565-023-09813-w
Gavande NS, VanderVere-Carozza PS, Hinshaw HD, Jalal SI, Sears CR, Pawelczak KS, Turchi JJ (2016) DNA repair targeted therapy: the past or future of cancer treatment? Pharmacol Therapeut 160:65–83. https://doi.org/10.1016/j.pharmthera.2016.02.003
Huang RX, Zhou PK (2020) DNA damage response signaling pathways and targets for radiotherapy sensitization in cancer. Signal Transduct Target Ther 5:60. https://doi.org/10.1038/s41392-020-0150-x
Liang Y, Lin S-Y, Brunicardi FC, Goss J, Li K (2009) DNA damage response pathways in tumor suppression and cancer treatment. World J Surg 33:661–666. https://doi.org/10.1007/s00268-008-9840-1
Giglia-Mari G, Zotter A, Vermeulen W (2011) DNA damage response. Cold Spring Harb Perspect Biol 3:a000745–a000745. https://doi.org/10.1101/cshperspect.a000745
Ainembabazi D, Geng X, Gavande NS, Turchi JJ, Zhang Y (2022) Synthesis and biological evaluation of cardiac glycosides for cancer therapy by targeting the DNA damage response. Chem Med Chem 17:e202200415. https://doi.org/10.1002/cmdc.202200415
Newman RA, Yang P, Pawlus A, Block K (2008) Cardiac glycosides as novel cancer therapeutic agents. Mol Interv 8: 36–49. Mol Interv 8:36–49. https://doi.org/10.1124/mi.8.1.8
Reddy D, Kumavath R, Barh D, Azevedo V, Ghosh P (2020) Anticancer and antiviral properties of cardiac glycosides: a review to explore the mechanism of actions. Molecules 25:3596. https://doi.org/10.3390/molecules25163596
Škubník J, Svobodová Pavlíčková V, Psotová J, Rimpelová S (2021) Cardiac glycosides as autophagy modulators. Cells. https://doi.org/10.3390/cells10123341
Hou Y, Shang C, Meng T, Lou W (2021) Anticancer potential of cardiac glycosides and steroid-azole hybrids. Steroids 171:108852. https://doi.org/10.1016/j.steroids.2021.108852
Cerella C, Dicato M, Diederich M (2013) Assembling the puzzle of anti-cancer mechanisms triggered by cardiac glycosides. Mitochondrion 13:225–234. https://doi.org/10.1016/j.mito.2012.06.003
Slingerland M, Cerella C, Guchelaar HJ, Diederich M, Gelderblom H (2013) Cardiac glycosides in cancer therapy: from preclinical investigations towards clinical trials. Investig New Drugs 31:1087–1094. https://doi.org/10.1007/s10637-013-9984-1
Kumavath R, Paul S, Pavithran H, Paul MK, Ghosh P, Barh D, Azevedo V (2021) Emergence of cardiac glycosides as potential drugs: current and future scope for cancer therapeutics. Biomolecules. https://doi.org/10.3390/biom11091275
Ayogu JI, Odoh AS (2020) Prospects and therapeutic applications of cardiac glycosides in cancer remediation. ACS Comb Sci 22:543–553. https://doi.org/10.1021/acscombsci.0c00082
Soumoy L, Ghanem GE, Saussez S, Journe F (2022) Bufalin for an innovative therapeutic approach against cancer. Pharmacol Res 184:106442. https://doi.org/10.1016/j.phrs.2022.106442
Deng L-J, Li Y, Qi M, Liu J-S, Wang S, Hu L-J, Lei Y-H, Jiang R-W, Chen W-M, Qi Q, Tian H-Y, Han W-L, Wu B-J, Chen J-X, Ye W-C, Zhang D-M (2020) Molecular mechanisms of bufadienolides and their novel strategies for cancer treatment. Eur J Pharmacol 887:173379. https://doi.org/10.1016/j.ejphar.2020.173379
Ma L, Meng Y, Tu C, Cao X, Wang H, Li Y, Man S, Zhou J, Li M, Liu Z, Su Y (2018) A cardiac glycoside HTF-1 isolated from helleborus thibetanus Franch displays potent in vitro anti-cancer activity via caspase-9, MAPK and PI3K-Akt-mTOR pathways. Eur J Med Chem 158:743–752. https://doi.org/10.1016/j.ejmech.2018.09.019
Bhattamisra SK, Yap KH, Rao V, Choudhury H (2020) Multiple biological effects of an iridoid glucoside, catalpol, and its underlying molecular mechanisms. Biomolecules 10:32. https://doi.org/10.3390/biom10010032
Liu J, Du J, Li Y, Wang F, Song D, Lin J, Li B, Li L (2022) Catalpol induces apoptosis in breast cancer in vitro and in vivo: Involvement of mitochondria apoptosis pathway and post-translational modifications. Toxicol Appl Pharmacol 454:116215. https://doi.org/10.1016/j.taap.2022.116215
Wang H-YL, Rojanasakul Y, O’Doherty GA (2011) Synthesis and evaluation of the α-D-/α-L-rhamnosyl and Amicetosyl digitoxigenin oligomers as anti-tumor agents. ACS Med Chem Lett 2:264–269. https://doi.org/10.1021/ml100290d
Wha Jun D, Hwang M, Kim HJ, Hwang SK, Kim S, Lee C-H (2013) Ouabain, a cardiac glycoside, inhibits the fanconi anemia/BRCA pathway activated by DNA interstrand cross-linking agents. PLoS One 8:e75905. https://doi.org/10.1371/journal.pone.0075905
Du J, Jiang L, Chen F, Hu H, Zhou M (2021) Cardiac glycoside ouabain exerts anticancer activity via downregulation of STAT3. Front Oncol. https://doi.org/10.3389/fonc.2021.684316
Chou W-H, Liu K-L, Shih Y-L, Chuang Y-Y, Chou J, Lu H-F, Jair H-W, Lee M-Z, Au M-K, Chung J-G (2018) Ouabain induces apoptotic cell death through caspase- and mitochondria-dependent pathways in human osteosarcoma U-2 OS cells. Anticancer Res 38:169. https://doi.org/10.21873/anticanres.12205
Bhattarai B, Nagorny P (2018) Enantioselective total synthesis of cannogenol-3-O-α-l-rhamnoside via sequential Cu(II)-catalyzed michael addition/intramolecular aldol cyclization reactions. Org Lett 20:154–157. https://doi.org/10.1021/acs.orglett.7b03513
Carney N, Perry N, Garabedian J, Nagorny P (2023) Development of α-selective glycosylation with l-Oleandral and its application to the total synthesis of oleandrin. Org Lett 25:966–971. https://doi.org/10.1021/acs.orglett.2c04358
Gan H, Qi M, Chan C, Leung P, Ye G, Lei Y, Liu A, Xue F, Liu D, Ye W, Zhang D, Deng L, Chen J, Gan H, Qi M, Chan C, Leung P, Ye G, Lei Y, Liu A, Xue F, Liu D, Ye W, Zhang D, Deng L, Chen J, Gan H, Qi M, Chan C, Leung P, Ye G, Lei Y, Liu A, Xue F, Liu D, Ye W, Zhang D, Deng L, Chen J (2020) Digitoxin inhibits HeLa cell growth through the induction of G2/M cell cycle arrest and apoptosis in vitro and in vivo. Int J Oncol 57:562–573. https://doi.org/10.3892/ijo.2020.5070
Wang Y, Ma Q, Zhang S, Liu H, Zhao B, Du B, Wang W, Lin P, Zhang Z, Zhong Y, Kong D (2020) Digoxin enhances the anticancer effect on non-small cell lung cancer while reducing the cardiotoxicity of adriamycin. Front Pharmacol. https://doi.org/10.3389/fphar.2020.00186
Lee Ji Y, Kim M-S, Lee Mi S, Ju Jae E, Chung N, Jeong Youn K (2017) Digoxin enhances radiation response in radioresistant A549 cells by reducing protein phosphatase 2A. Biosci Rep 37:BSR20171257. https://doi.org/10.1042/BSR20171257
Picco V, Pagès G (2013) Linking JNK activity to the DNA damage response. Genes Cancer 4:360–368. https://doi.org/10.1177/1947601913486347
Park S-J, Oh E-J, Yoo M-A, Lee S-H (2001) Involvement of DNA-dependent protein kinase in regulation of stress-induced JNK Activation. DNA Cell Biol 20:637–645. https://doi.org/10.1089/104454901753340622
Yogosawa S, Yoshida K (2018) Tumor suppressive role for kinases phosphorylating p53 in DNA damage-induced apoptosis. Cancer Sci 109:3376–3382. https://doi.org/10.1111/cas.13792
Paik JY, Jung KH, Lee JH, Park JW, Lee KH (2017) Reactive oxygen species-driven HIF1alpha triggers accelerated glycolysis in endothelial cells exposed to low oxygen tension. Nucl Med Biol 45:8–14. https://doi.org/10.1016/j.nucmedbio.2016.10.006
Kussmaul L, Hirst J (2006) The mechanism of superoxide production by NADH:ubiquinone oxidoreductase (complex I) from bovine heart mitochondria. Proc Natl Acad Sci USA 103:7607–7612. https://doi.org/10.1073/pnas.0510977103
Murphy Michael P (2008) How mitochondria produce reactive oxygen species. Biochem J 417:1–13. https://doi.org/10.1042/BJ20081386
Forrester SJ, Kikuchi DS, Hernandes MS, Xu Q, Griendling KK (2018) Reactive oxygen species in metabolic and inflammatory signaling. Circ Res 122:877–902. https://doi.org/10.1161/CIRCRESAHA.117.311401
Iyer AK, Zhou M, Azad N, Elbaz H, Wang L, Rogalsky DK, Rojanasakul Y, O’Doherty GA, Langenhan JM (2010) A direct comparison of the anticancer activities of digitoxin MeON-Neoglycosides and O-Glycosides: oligosaccharide chain length-dependent induction of caspase-9-mediated apoptosis. ACS Med Chem Lett 1:326–330. https://doi.org/10.1021/ml1000933
Zinkel S, Gross A, Yang E (2006) BCL2 family in DNA damage and cell cycle control. Cell Death Differ 13:1351–1359. https://doi.org/10.1038/sj.cdd.4401987
Wang Q, Gao F, May WS, Zhang Y, Flagg T, Deng X (2008) Bcl2 negatively regulates DNA double-strand-break repair through a nonhomologous end-joining pathway. Mol Cell 29:488–498. https://doi.org/10.1016/j.molcel.2007.12.029
Liu X, Zhao P, Wang X, Wang L, Zhu Y, Song Y, Gao W (2019) Celastrol mediates autophagy and apoptosis via the ROS/JNK and Akt/mTOR signaling pathways in glioma cells. J Exp Clin Cancer Res 38:184. https://doi.org/10.1186/s13046-019-1173-4
Li M-y, Zhu X-l, Zhao B-x, Shi L, Wang W, Hu W, Qin S-l, Chen B-h, Zhou P-h, Qiu B, Gao Y, Liu B-l (2019) Adrenomedullin alleviates the pyroptosis of Leydig cells by promoting autophagy via the ROS–AMPK–mTOR axis. Cell Death Dis 10:489. https://doi.org/10.1038/s41419-019-1728-5
Wu JJ, Wang DJ, Zhou JY, Li JT, Xie RX, Li YY, Huang JY, Liu BH, Qiu JG (2022) Gambogenic acid induces apoptosis and autophagy through ROS-mediated endoplasmic reticulum stress via JNK pathway in prostate cancer cells. Phytother Res. https://doi.org/10.1002/ptr.7614
Pan L, Zhang Y, Zhao W, Zhou X, Wang C, Deng F (2017) The cardiac glycoside oleandrin induces apoptosis in human colon cancer cells via the mitochondrial pathway. Cancer Chemother Pharmacol 80:91–100. https://doi.org/10.1007/s00280-017-3337-2
Chen Y-Y, Wen S-Y, Deng C-M, Yin X-F, Sun Z-H, Jiang M-M, He Q-Y (2019) Proteomic analysis reveals that odoroside a triggers G2/M arrest and apoptosis in colorectal carcinoma through ROS-p53 pathway. Proteomics 19:1900092. https://doi.org/10.1002/pmic.201900092
Kastan MB, Bartek J (2004) Cell-cycle checkpoints and cancer. Nature 432:316–323. https://doi.org/10.1038/nature03097
Zhang X-H, Wang X-Y, Zhou Z-W, Bai H, Shi L, Yang Y-X, Zhou S-F, Zhang X-C (2017) The combination of digoxin and GSK2606414 exerts synergistic anticancer activity against leukemia in vitro and in vivo. BioFactors 43:812–820. https://doi.org/10.1002/biof.1380
Ma Y, Vassetzky Y, Dokudovskaya S (2018) mTORC1 pathway in DNA damage response. Biochim Biophys Acta - Mol Cell Res 1865:1293–1311. https://doi.org/10.1016/j.bbamcr.2018.06.011
Huang T-T, Lampert EJ, Coots C, Lee J-M (2020) Targeting the PI3K pathway and DNA damage response as a therapeutic strategy in ovarian cancer. Cancer Treat Rev 86:102021. https://doi.org/10.1016/j.ctrv.2020.102021
Lindholm H, Ejeskär K, Szekeres F (2022) Digitoxin affects metabolism, ROS production and proliferation in pancreatic cancer cells differently depending on the cell phenotype. Int J Mol Sci 23:8237. https://doi.org/10.3390/ijms23158237
Lin S-Y, Chang H-H, Lai Y-H, Lin C-H, Chen M-H, Chang G-C, Tsai M-F, Chen JJW (2015) Digoxin suppresses tumor malignancy through inhibiting multiple Src-related signaling pathways in non-small cell lung cancer. PLoS ONE 10:e0123305–e0123305. https://doi.org/10.1371/journal.pone.0123305
Hossan MS, Chan Z-Y, Collins HM, Shipton FN, Butler MS, Rahmatullah M, Lee JB, Gershkovich P, Kagan L, Khoo T-J, Wiart C, Bradshaw TD (2019) Cardiac glycoside cerberin exerts anticancer activity through PI3K/AKT/mTOR signal transduction inhibition. Cancer Lett 453:57–73. https://doi.org/10.1016/j.canlet.2019.03.034
Leu W-J, Chang H-S, Chan S-H, Hsu J-L, Yu C-C, Hsu L-C, Chen I-S, Guh J-H (2014) Reevesioside A, a cardenolide glycoside, induces anticancer activity against human hormone-refractory prostate cancers through suppression of c-myc expression and induction of G1 arrest of the cell cycle. PLoS One 9:e87323. https://doi.org/10.1371/journal.pone.0087323
Reddy D, Kumavath R, Ghosh P, Barh D (2019) Lanatoside C induces G2/M cell cycle arrest and suppresses cancer cell growth by attenuating mapk, Wnt, JAK-STAT, and PI3K/AKT/mTOR signaling pathways. Biomolecules 9:792. https://doi.org/10.3390/biom9120792
Mijatovic T, De Nève N, Gailly P, Mathieu V, Haibe-Kains B, Bontempi G, Lapeira J, Decaestecker C, Facchini V, Kiss R (2008) Nucleolus and c-Myc: potential targets of cardenolide-mediated antitumor activity. Mol Cancer Ther 7:1285–1296. https://doi.org/10.1158/1535-7163.MCT-07-2241
Rohban S, Campaner S (2015) Myc induced replicative stress response: how to cope with it and exploit it. Biochim Biophys Acta - Gene Regul Mech 1849:517–524. https://doi.org/10.1016/j.bbagrm.2014.04.008
Howard CM, Estrada M, Terrero D, Tiwari AK, Raman D (2020) Identification of cardiac glycosides as novel inhibitors of eIF4A1-mediated translation in triple-negative breast cancer cells. Cancers. https://doi.org/10.3390/cancers12082169
Zhang Z, Wang Y, Ma Q, Zhang S, Liu H, Zhao B, Liu R, Wang W, Du B, Zhong Y, Kong D (2021) Biomimetic carrier-free nanoparticle delivers digoxin and doxorubicin to exhibit synergetic antitumor activity in vitro and in vivo. Chem Eng J 406:126801. https://doi.org/10.1016/j.cej.2020.126801
Iyer AKV, Zhou M, Azad N, Elbaz H, Wang L, Rogalsky DK, Rojanasakul Y, O’Doherty GA, Langenhan JM (2010) A direct comparison of the anticancer activities of digitoxin MeON-neoglycosides and O-glycosides. ACS Med Chem Lett 1:326–330. https://doi.org/10.1021/ml1000933
Li XS, Ren YC, Bao YZ, Liu J, Zhang XK, Zhang YW, Sun XL, Yao XS, Tang JS (2018) Synthesis of C(3)-neoglycosides of digoxigenin and their anticancer activities. Eur J Med Chem 145:252–262
Mahajan K, Mahajan NP (2015) Cross talk of tyrosine kinases with the DNA damage signaling pathways. Nucleic Acids Res 43:10588–10601. https://doi.org/10.1093/nar/gkv1166
Kawanishi S, Ohnishi S, Ma N, Hiraku Y, Murata M (2017) Crosstalk between DNA damage and inflammation in the multiple steps of carcinogenesis. Int J Mol Sci. https://doi.org/10.3390/ijms18081808
Acknowledgements
We would like to thank Pamela VanderVere-Carozza, Katherine Pawelczak, Pamela Lorena Mendoza-Munoz, Maria Casiano and Matthew Jordan who assisted in proofreading this manuscript and Navnath Gavande for his helpful discussions on CG chemistry.
Funding
National Institute of Health award CA230453 to YZ.
Author information
Authors and Affiliations
Contributions
DA wrote the initial draft and DA, JT, and YZ edited the manuscript. JT and DA prepared the figures.
Corresponding author
Ethics declarations
Conflict of interest
Not applicable.
Ethical approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ainembabazi, D., Zhang, Y. & Turchi, J.J. The mechanistic role of cardiac glycosides in DNA damage response and repair signaling. Cell. Mol. Life Sci. 80, 250 (2023). https://doi.org/10.1007/s00018-023-04910-9
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00018-023-04910-9