Abstract
Background
Transient Receptor Potential Ankyrin 1 (TRPA1) is a cation channel that mediates pain, itch, cough, and neurogenic inflammation in response to pungent compounds such as acrolein in cigarette smoke. TRPA1 is also activated by endogenous factors and promotes inflammation in asthma models. We have recently shown that TRPA1 is upregulated by inflammatory cytokines in A549 human lung epithelial cells. Here, we explored the effects of Th1 and Th2-type inflammation on TRPA1.
Methods and results
TRPA1 expression and function was studied in A549 human lung epithelial cells. To induce inflammation, the cells were exposed to a combination of cytokines TNF-α and IL-1β; and to model Th1 or Th2-type responses, IFN-γ or IL-4/IL-13 was added, respectively. TRPA1 expression (measured by RT-PCR and Western blot) and function (assessed by Fluo-3AM intracellular calcium measurement) was enhanced under the influence of TNF-α + IL-1β. IFN-γ further enhanced TRPA1 expression and function, whereas IL-4 and IL-13 suppressed them. The effects of IFN-γ and IL-4 on TRPA1 expression were reversed by the Janus kinase (JAK) inhibitors baricitinib and tofacitinib, and those of IL-4 also by the STAT6 inhibitor AS1517499. The glucocorticoid dexamethasone downregulated TRPA1 expression, whereas the PDE4 inhibitor rolipram had no effect. Under all conditions, TRPA1 blockade was found to reduce the production of LCN2 and CXCL6.
Conclusions
TRPA1 expression and function in lung epithelial cells was upregulated under inflammatory conditions. IFN-γ further increased TRPA1 expression while IL-4 and IL-13 suppressed that in a JAK-STAT6 dependent manner which is novel. TRPA1 also modulated the expression of genes relevant to innate immunity and lung disease. We propose that the paradigm of Th1 and Th2 inflammation is a major determinant of TRPA1 expression and function, which should be considered when targeting TRPA1 for pharmacotherapy in inflammatory (lung) disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
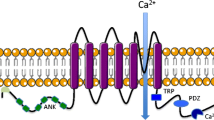
Transient Receptor Potential Ankyrin 1 (TRPA1) is a neuronal cation channel activated by noxious compounds [1, 2]. TRPA1 permeates Na+, Ca2+ and other cations and mediates pain, itch, cough, and neurogenic inflammation [1, 2]. Exogenous TRPA1 activators include, for example, allyl isothiocyanate [3] and acrolein [4], found in mustard oil and cigarette smoke, respectively. Endogenous TRPA1 activators are produced in inflammatory reactions, including reactive oxygen and nitrogen species [5,6,7,8]. More recently, TRPA1 has been found to be expressed also in non-neuronal cells, including chondrocytes [9], keratinocytes [10,11,12] and lung epithelial cells [13,14,15], and to regulate the expression of inflammatory factors such as interleukin 8 (IL-8), interleukin 6 (IL-6) and prostaglandin E2 [9, 13,14,15,16,17,18,19,20,21,22,23].
TRPA1 seems to be important in the pathogenesis of inflammatory lung diseases. TRPA1 is activated by cigarette smoke to cause inflammation and hyperreactivity [4, 17, 19], epithelial cell damage [17, 19] and emphysema [24]. In the ovalbumin model of allergic asthma, TRPA1 has been reported to promote the release of inflammatory factors [25,26,27,28,29], mediate peripheral blood eosinophilia [27, 29], increase leukocyte influx to the lungs [22, 25, 27,28,29] and to increase airway hyperreactivity [25, 26, 28, 29].
We and others have recently found that TRPA1 expression is upregulated by inflammatory factors in human cells. Examples include interleukin 1 beta (IL-1β) [9, 15], interleukin 1 alpha (IL-1α) [30], tumor necrosis factor alpha (TNF-α) [12, 15, 30], interferon gamma (IFN-γ) [15], interleukin 17 (IL-17), lipopolysaccharide (LPS) and resistin [9]. In addition, TRPA1 translocation to the plasma membrane can be induced by inflammatory factors. These include the cytokines TNF-α [31, 32] and IL-1α [33] and the second messengers protein kinase A (PKA) and phospholipase C (PLC) [34]. Inflammatory factors can also modulate TRPA1 channel function. Activation of bradykinin receptors can activate or potentiate TRPA1 in a PKA and PLC-dependent manner [35,36,37]. PLC also mediates protease-activated receptor 2-dependent TRPA1 potentiation [36] and TRPA1 activation by the cytokine thymic stromal lymphopoietin [38]. TRPA1 channel function may also be enhanced by the inflammatory factors TNF-α [21] and nerve growth factor (NGF) [39]. Some anti-inflammatory drugs have been shown to downregulate TRPA1 expression, examples being the glucocorticoid dexamethasone [12, 15, 40], the antirheumatic drug aurothiomalate [40], and calcineurin inhibitors [12].
CD4+ T helper (Th) lymphocytes specialize into different effector subsets. Th1 cells produce IFN-γ and promote cell-mediated immunity–whereas the Th2 cells produce IL-4, promote immunity against parasites and have a role in allergy and humoral immunity. Several other Th subtypes have also been established recently (reviewed in [41, 42]). The Th1-Th2 paradigm is relevant when considering asthma which is divided into phenotypes and endotypes characterized by features of Th2 or non-Th2 type inflammation. [43,44,45].
We have previously found that the signature Th1 cytokine IFN-γ upregulates TRPA1 expression in human A549 lung epithelial cells exposed to inflammatory stimuli (TNF-α and IL-1β) [15]. However, the role of Th2 cytokines on TRPA1 expression remains unknown. As the Th1-Th2 paradigm is essential when considering pathogenesis of inflammatory diseases including asthma, we aimed to study the regulation of TRPA1 expression and function under Th1 and Th2-type inflammation in human A549 lung epithelial cells.
Methods
Cell culture
A549 alveolar epithelial cells (American Type Culture Collection, Manassas, VA, USA) were cultured in Ham’s F–12 K (Kaighn’s modification) medium with 10% heat-inactivated fetal bovine serum, 100 μg/ml streptomycin, 100 U/ml penicillin and 250 ng/ml amphotericin B (all from Gibco/Life Technologies, Carlsbad, CA, USA) at 37 ◦C in 5% CO2. A549 cells were seeded on 24-well plates and grown for 48 h before the experiments. During the experiments the cells were cultured with the following compounds or their combinations as indicated: TNF-α, IL-1β, IFN-γ, IL-4, IL-13 (all from R&D Systems Europe Ltd, Abingdon, UK), the Janus kinase (JAK) inhibitors bariticinib and tofacitinib, the STAT6 inhibitor AS1517499, the TRPA1 agonist allyl isothiocyanate (AITC) and the TRPA1 antagonists HC-030031 and A-967079 (all from Sigma Aldrich, St. Louis, MO, USA).
RNA extraction and RT-PCR
Total RNA was extracted (GenElute Mammalian Total RNA Miniprep kit, Sigma Aldrich) at indicated time points, and was reverse-transcribed to cDNA (TaqManⓇ Reverse Transcription Reagents, Applied Biosystems, Foster City, CA, USA). PCR was carried out by using the Applied Biosystems 7500 Real-Time PCR instrument and Taqman Universal PCR Master Mix reagent. The primer and probe sequences and concentrations for GAPDH were designed and optimized using Primer Express software (Applied Biosystems) and were: 5′-AAGGTCGGAGTCAACGGATTT-3’ (GAPDH, forward, 300 nM), 5′-GCAACAATATCCACTTTACCAGAGTTAA-3’ (GAPDH, reverse, 300 nM), and 5′-CGCCTGGTCACCAGGGCTGC-3’ (GAPDH, probe, 150 nM, containing 6-FAM as 5′-reporter dye and TAMRA as 3′-quencher) (Metabion, Martinsried, Germany). TaqMan Gene Expression assay for TRPA1 (Hs00175798_m1) was obtained from Life Technologies (Life Technologies Europe BV, Bleiswijk, the Netherlands). In data analysis, mRNA expression levels were first normalized against GAPDH mRNA levels, and the ΔΔCt method was used in the calculations.
Western blot
Protein extraction, TRPA1 immunoprecipitation and Western blot analysis were carried out as described previously [9, 12] with slight modifications. In this study, each sample containing 1950 µg of total protein was subjected to immunoprecipitation. As previously, the TRPA1 antibody SAB2105082 (Sigma Aldrich) and Protein A/G PLUS-Agarose (sc-2003, Santa Cruz Biotechnology, Inc., Dallas, TX, USA) were used in TRPA1 immunoprecipitation. In the Western blot analysis, NB110-40,763 (Novus Biologicals, LCC, Littleton, CO, USA) diluted in 1:1000 in 5% non-fat milk was used as the primary antibody. Goat anti-rabbit HRP-linked IgG antibody CST#7074 diluted in 1:10 000 in 5% non-fat milk (Cell Signaling Technology Inc., Beverly, MA, USA) was used as the secondary antibody. HEK293 cells (American Type Culture Collection, Manassas, VA, USA) transfected with TRPA1 plasmid DNA (pCMV6-XL4 by Origene, Rockville, MD, USA) were used as a positive control. HEK293 culturing and transfection were carried out as described previously [9, 12].
Immunoassay
Lipocalin-2 (LCN2) and chemokine (C-X-C motif) ligand 6 (CXCL6) concentrations in A549 medium samples were measured by enzyme-linked immunosorbent assay (ELISA). The reagents were purchased from R&D Systems Europe Ltd, Abingdon, United Kingdom.
Intracellular Ca2+ measurements
TRPA1-dependent changes in intracellular Ca2+ levels were determined using the fluo-3-acetoxymethyl ester assay (Fluo 3-AM, Sigma Aldrich) as described previously [46]. In brief, after culturing the A549 cells in indicated experimental conditions, the cells were loaded in room temperature with 4 μM Fluo 3-AM and 0.08% Pluronic F-127Ⓡ in Hanks’ balanced salt solution (HBSS, Lonza, Verviers, Belgium) containing 1 mg/ml bovine serum albumin, 2.5 mM probenecid and 25 mM HEPES pH 7.2 (all from Sigma Aldrich) for 30 min. The excitation/emission wavelengths of 485/535 nm were analyzed using Victor3 1420 multilabel counter (PerkinElmer, Waltham, MA, USA) as an indicator of free intracellular Ca2+. The cells were first preincubated for 30 min at room temperature with the TRPA1 antagonist HC-030031 (200 μM, Sigma Aldrich) or the vehicle (DMSO). Thereafter, using an injector, the TRPA1 agonist allyl isothiocyanate (AITC, 100 μM, Sigma Aldrich) was applied and the measurements were continued for 30 s.
Statistical analysis
Statistical analysis was performed using Graph-Pad Prism version 5.02 (GraphPad Software, San Diego, CA, USA). The results are presented as mean ± standard error of the mean (SEM). One-way analysis of variance (ANOVA) or repeated measures ANOVA followed by Bonferroni’s multiple comparisons test were used as indicated.
Results
The effect of Th1 and Th2 cytokines on TRPA1 expression in inflammatory conditions
TRPA1 expression was low in dormant A549 lung epithelial cells but it was significantly increased in inflammatory conditions when the cells were cultured with the combination of TNF-α and IL-1β. When the classical Th1 cytokine IFN-γ was added to the culture, it further enhanced TRPA1 expression. The effect of IFN-γ was statistically significant already at 0.3 ng/ml concentration and increased in a dose-dependent manner up to 10 ng/ml concentration. In contrast, the Th2 cytokines IL-4 and IL-13 significantly downregulated TNF-α and IL-1β-induced TRPA1 expression. The effect was dose-dependent and the concentration of 10 ng/ml reduced TRPA1 expression to the control level. (Fig. 1) Based on the concentration curves, we chose to continue experiments with the concentration of 10 ng/ml of IFN-γ, IL-4 and IL-13.
The Th1 cytokine IFN-γ upregulates and the Th2 cytokines IL-4 and IL-13 downregulate TRPA1 expression. In (A), (B) and (C), the dose-dependent effect of the cytokines is shown. A549 cells were cultured for 24 h with the combination of TNF-α (20 ng/ml) and IL-1β (10 ng/ml), and increasing concentrations of IFN-γ A, IL-4 B or IL-13 C. Thereafter, total RNA was extracted and TRPA1 RT-PCR was performed against GAPDH as a housekeeping gene. In all figures, data is presented as mean + SEM, n = 4. Comparisons were carried out using One-way ANOVA with Bonferroni’s post-test. Asterisks on bars indicate comparison against the combination of TNF-α and IL-1β. ** and *** denote p < 0.01 and p < 0.001, respectively; ns = not significant
In Fig. 2, the time curves of the effects of IFN-γ and IL-4 are shown. When the cells were first exposed to the combination of TNF-α and IL-1β, it was found to induce an increase in TRPA1 expression reaching its peak at four and eight hours and thereafter declining. When IFN-γ was added into the culture, it further enhanced TRPA1 expression which was obvious at eight hours and thereafter remained stable up to the 24 h follow-up being at about 12 folds higher level compared to the control expression. Adding IL-4 to the culture significantly downregulated TNF-α and IL-1β-induced TRPA1 expression at all time points, reaching control level at 12–24 h.
The time-dependent effects of Th1 and Th2-type cytokines on TRPA1 mRNA expression. A549 cells were cultured with the combination of TNF-α (20 ng/ml) and IL-1β (10 ng/ml), with and without IFN-γ (10 ng/ml) or IL-4 (10 ng/ml). At 0, 4, 8, 12 and 24 h, total RNA was extracted and TRPA1 RT-PCR was performed against GAPDH as a housekeeping gene. Control of each time point is set as 1, and the other values of the same time point are given in relation to that value. Mean ± SEM, n = 4. Comparisons were carried out using one-way ANOVA with Bonferroni’s post-test. Asterisks beside the data points represent comparisons against the control (untreated sample) of the respective time point, and asterisks beside brackets represent comparisons carried out between indicated conditions. *, ** and *** denote p < 0.05, < 0.01 or < 0.001, respectively; ns = not significant
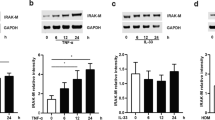
We then studied whether the changes in TRPA1 mRNA also correlate to TRPA1 protein levels. A549 cells were cultured in same conditions as above, protein extraction was carried out and TRPA1 was measured by Western blot after immunoprecipitation. As expected, the combination of TNF-α and IL-1β significantly upregulated TRPA1 protein expression. In accordance with the mRNA data, combining IFN-γ to the treatment further enhanced TRPA1 protein levels; whereas IL-4 significantly downregulated TNF-α and IL-1β-induced TRPA1 protein expression which did not differ from the control level (Fig. 3).
The effects of Th1 and Th2 cytokines on TRPA1 protein expression under inflammatory conditions. A549 cells were cultured with the combination of TNF-α (20 ng/ml) and IL-1β (10 ng/ml), with and without IFN-γ (10 ng/ml) or IL-4 (10 ng/ml) for 12 h. Thereafter TRPA1 protein levels were measured with Western blot after immunoprecipitation. TRPA1-transfected HEK293 cells were used as a positive control. In A is shown a representative immunoblot (a complete gel profile is shown in the Supplementary Figure S1), and in B a densitometric analysis of five independent experiments. In each experiment, the densitometric signal in the control was set as 1 and the other values are given in relation to that value. The data is presented as mean + SEM. Statistical analysis was performed by using repeated measures ANOVA with Bonferroni’s post-test. Asterisks on bars indicate comparison to control, and asterisks on brackets indicate comparison between depicted conditions. *, ** and *** denote p < 0.05, < 0.01 and 0.001, respectively. Ns = not significant
Next, we investigated whether the observed differences in TRPA1 mRNA and protein levels translate into differences in TRPA1 function and utilized the Fluo 3-AM intracellular calcium assay. A549 cells were cultured in the same conditions as above. In all conditions, the TRPA1 agonist allyl isothiocyanate (AITC) induced a fluorescent signal, indicating that intracellular Ca2+ concentration was increased. These effects were reversed by the TRPA1 antagonist HC-030031, indicating the presence of functional TRPA1 channel. In cells cultured in the presence of the combination of TNF-α and IL-1β, the Ca2+ signal was significantly increased as compared to controls. When IFN-γ was added to the culture, the Ca2+ signal further increased, whereas added IL-4 decreased the signal to the control level (Fig. 4). These data indicate that the enhancing effect of the Th1 cytokine IFN-γ and the decreasing effect of the Th2 cytokine IL-4 on TRPA1 is present at mRNA, protein and functional level.
The effects of inflammation as well as Th1 and Th2 conditions on TRPA1 function. Prior to the intracellular Ca2+ measurements, A549 cells were cultured with the combination of TNF-α (20 ng/ml) and IL-1β (10 ng/ml), with or without IFN-γ (10 ng/ml) or IL-4 (10 ng/ml) for 48 h. Thereafter, the cells were loaded with the calcium-responsive fluorescent dye Fluo 3-AM, and the cells were preincubated with the TRPA1 antagonist HC-030031 (200 µM) or vehicle (DMSO) for 30 min. After measuring baseline fluorescence, the TRPA1 agonist allyl isothiocyanate (AITC, 100 µM) was applied and fluorescence was measured for 30 s. In A is shown the averaged trace from 8 wells and in B is shown the area under curve analysis as mean + SEM, n = 8. Statistical analysis was performed using one-way ANOVA with Bonferroni’s post-test. Asterisks on bars indicate comparison against control, asterisks on brackets indicate comparison between depicted conditions; and hashtags on bars indicate comparison against the other bar of the respective condition. **, *** and ### denote p < 0.01, p < 0.001 and p < 0.001, respectively; ns = not significant
The effect of Janus kinase (JAK) inhibitors on IFN-γ and IL-4-induced changes in TRPA1 expression
In their target cells, IFN-γ and IL-4 activate Janus kinase (JAK)—signal transducer and activator of transcription (STAT) signaling pathways which mediate many of their cellular effects [47, 48]. Therefore, we investigated the effects of two JAK inhibitors, baricitinib and tofacitinib, on the IFN-γ and IL-4 induced changes in TRPA1 expression. Baricitinib and tofacitinib at concentrations of 0.1—10 µM significantly reversed the effects of IFN-γ and IL-4 on TRPA1 expression but did not affect TRPA1 expression induced by TNF-α and IL-1β in the absence of IFN-γ and IL-4. (Fig. 5).
JAK inhibitors reverse the effects of IFN-γ and IL-4 on TRPA1 expression. A549 cells were cultured for 24 h with the combination of TNF-α (20 ng/ml) and IL-1β (10 ng/ml), with or without IFN-γ (10 ng/ml; A and B) or IL-4 (10 ng/ml; C and D) and increasing concentrations of baricitinib (0.01–10 µM; A, C and E) or tofacitinib (0.01-10 µM; B, D and F). Thereafter, total RNA was extracted and TRPA1 mRNA expression was measured by RT-PCR against GAPDH as a housekeeping gene. Data is presented as mean + SEM, n = 4–8. Comparisons were carried out using one-way ANOVA with Bonferroni’s post-test. Asterisks on bars indicate comparison to the treatment with TNF-α + IL-1β + IFN-γ (A,B) or TNF-α + IL-1β + IL-4 (C,D). *** denotes p < 0.001, ns = not significant
JAK signaling activated by IL-4 and IL-13 leads to the phosphorylation and translocation of STAT6 whereas IFN-γ activates primarily STAT1 [47, 48]. Accordingly, the STAT6 inhibitor AS1517499 [49] reversed the downregulation of TRPA1 expression induced by IL-4 and IL-13 (Fig. 6).
STAT6 inhibitor partly reverses the effects of IL-4 and IL-13 on TRPA1 expression. A549 cells were cultured with the combination of TNF-α (20 ng/ml) and IL-1β (10 ng/ml), with or without IL-4 (10 ng/ml, A) or IL-13 (10 ng/ml, B) and the STAT6 inhibitor AS1517499 (1 µM) for 8 h. Thereafter, total RNA was extracted and TRPA1 mRNA was measured by RT-PCR against GAPDH as a housekeeping gene. Data is presented as mean + SEM, n = 4. Comparisons were carried out using one-way ANOVA with Bonferroni’s post-test. Asterisks on bars indicate comparison to the treatment with TNF-α + IL-1β + IL-4 (A) or TNF-α + IL-1β + IL-13 (B). *** denotes p < 0.001
The effects of the anti-inflammatory drugs dexamethasone and rolipram on TRPA1 expression
Glucocorticoids and PDE4 inhibitors are used as anti-inflammatory treatments in lung diseases. Therefore, we investigated the effects of the glucocorticoid dexamethasone and the PDE4 inhibitor rolipram on TRPA1 expression. Dexamethasone downregulated TRPA1 expression in a dose-dependent manner independent on whether the cells were cultured with TNF-α + IL-1β only or in a combination with IFN-γ or IL-4. Full effect was achieved at 0.1 µM drug concentration in the case of TNF-α + IL-1β and TNF-α + IL-1β + IL-4 treated cells, whereas 1 µM was required when the cells were treated with a combination of TNF-α + IL-1β + IFN-γ. In contrast, rolipram had no effect on TRPA1 expression (Fig. 7).
Dexamethasone downregulates TRPA1 but rolipram has no effect. A549 cells were cultured for 24 h with the combination of TNF-α (20 ng/ml) and IL-1β (10 ng/ml, A), with or without IFN-γ (10 ng/ml, B) or IL-4 (10 ng/ml, C), and rolipram (10 µM) or increasing concentrations of dexamethasone (0.01–1 µM). Thereafter, total RNA was extracted and TRPA1 mRNA was measured using RT-PCR against GAPDH as a housekeeping gene. Data is presented as mean + SEM, n = 4. Comparisons were carried out using one-way ANOVA with Bonferroni’s post-test. Asterisks on bars indicate comparison to the treatment with TNF-α + IL-1β (A), TNF-α + IL-1β + IFN-γ (B) or TNF-α + IL-1β + IL-4 (C). *** denotes p < 0.001, ns = not significant
The effect of TRPA1 on lipocalin-2 (LCN2) and chemokine (C-X-C motif) ligand 6 (CXCL6) expression
We were interested in investigating if TRPA1 regulates the expression of inflammatory genes in lung epithelial cells. Based on our preliminary RNA-sequencing data, we chose to focus on lipocalin-2 (LCN2) and chemokine (C-X-C motif) ligand 6 (CXCL6). The production of LCN2 and CXCL6 was increased when A549 cells were cultured in the presence of the combination of TNF-α and IL-1β, with or without IFN-γ or IL-4. TRPA1 inhibitors HC-030031 and A-967079 significantly reduced the production of LCN2 and CXCL6 in all conditions, indicating that TRPA1 enhances the production of these factors in A549 cells (Fig. 8).
TRPA1 regulates lipocalin-2 (LCN2) and chemokine (C-X-C motif) ligand 6 (CXCL6) production. Left: LCN2; right: CXCL6. A549 cells were cultured with the combination of TNF-α (20 ng/ml) and IL-1β (10 ng/ml) (A,B), with IFN-γ (10 ng/ml; C,D) or IL-4 (10 ng/ml; E,F); and the TRPA1 antagonists HC-030031 (10 and 100 µM) and A-967079 (10 and 100 µM) for 24 h. Thereafter, culture medium was collected and enzyme-linked immunosorbent assay (ELISA) was applied. The data is presented as mean + SEM, n = 3–4. Statistical analysis was performed using one-way ANOVA with Bonferroni’s post-test. Asterisks on bars indicate comparison against the stimulated condition without inhibitors. *, ** and *** denote p < 0.05, < 0.01 and 0.001, respectively. ns = not significant
Discussion
The present study shows that TRPA1 expression and function in human lung epithelial cells is regulated by inflammation and Th1 and Th2-type cytokines and that TRPA1 modulates gene expression relevant in innate immunity and inflammation. We demonstrate that inflammatory conditions (depicted by adding TNF-α and IL-1β into the culture) enhance TRPA1 expression and function, and that the Th1 cytokine IFN-γ further upregulates TRPA1. For the first time, we show that the Th2-type cytokines IL-4 and IL-13 significantly downregulate TRPA1 expression and function. Additionally, IFN-γ and IL-4 effects were shown to be reversed by JAK inhibitors; and the effects of IL-4 and IL-13 to be at least partially dependent on the transcription factor STAT6. Moreover, the expression of LCN2 and CXCL6 was suppressed by pharmacological TRPA1 blockade, which is also novel.
Early work showed that in the human airways, TRPA1 is expressed in epithelial cells, smooth muscle cells and fibroblasts, and promotes inflammatory responses [13, 14]. Thereafter, inflammatory stimuli have been shown to upregulate TRPA1. In A549 lung epithelial cells, IL-1α was reported to sensitize TRPA1 function by increasing TRPA1 translocation to the plasma membrane [33]. In lung fibroblasts, TNF-α has been shown to sensitize TRPA1 function [21]. Our recent work [15] showed that in A549 cells, combinations of inflammatory cytokines upregulate TRPA1 expression. The present study strengthens the view of TRPA1 as an inflammation-increased factor, as we show that the combination of TNF-α and IL-1β enhances TRPA1 expression on mRNA and protein levels and significantly increases TRPA1 function.
In our view, however, the most significant novel finding of this study is the striking difference between the effects of Th1 and Th2-type cytokines on TRPA1 expression and function in the lung epithelial cells: the Th1 type cytokine IFN-γ upregulated, while the Th2 type cytokine IL-4 downregulated TRPA1 expression and function. In support to this, we confirmed that the effects of IFN-γ and IL-4 are JAK-dependent as they were reversed by the JAK inhibitors baricitinib and tofacitinib. In addition, the effects of IL-4 and IL-13 seemed to be STAT6-dependent.
Our findings suggest that in lung epithelium TRPA1 is upregulated under inflammation and further enhanced under Th1-type inflammatory conditions while it is downregulated towards normal levels in Th2-type conditions. This may have meaningful implications in inflammatory (lung) diseases. For instance, asthma is expressed in various phenotypes. Allergic asthma is an example of the Th2-related phenotype, whereas non-Th2 asthma includes for example smoking associated and obesity associated asthma [43,44,45]. TRPA1 has been shown to mediate asthmatic inflammation and hyperresponsiveness in models of allergic asthma [25,26,27,28,29]. Therefore, TRPA1 has attracted attention as a potential asthma drug target. Our results show that TRPA1 function in inflamed lung epithelium could be more pronounced in Th1-type inflammation than in Th2-type conditions. This could further influence the feasibility of targeting TRPA1 in lung inflammation. One could expect relatively greater TRPA1 function and therefore a more pronounced response to TRPA1 antagonists in Th1-type conditions, such as in viral infection and perhaps non-Th2 asthma. Conversely, in Th2-type conditions–such as in allergic asthma–response to TRPA1 antagonist therapy might be more limited, as the channel would already be moderately downregulated/desensitized. Considering this, targeting TRPA1 could be more effective in non-Th2 asthma. It is also possible that the suppressive effect of IL-4 on the functional expression of TRPA1 is a compensation mechanism aiming to limit inflammation and symptoms in allergic asthma.
However, in addition to non-Th2 asthma, targeting TRPA1 in Th2 asthma could still be a viable strategy. While in our A549 model TNF-α and IL-1β induced TRPA1 expression was downregulated by IL-4, it remained functional in the Fluo 3-AM assay and was able to regulate CXCL6 and LCN2 expression. This suggests that the remaining TRPA1 function could be sufficient to carry out biologically relevant functions also under IL-4 stimulation and could possibly be involved in the development of asthmatic responses. However, inflammation ultimately is a vastly complex in vivo response and therefore the data from our in vitro model cannot be extrapolated directly to the in vivo scenario. As such, further studies are needed to confirm these effects in vivo.
Glucocorticoids and PDE4 inhibitors are used as anti-inflammatory treatments in lung diseases. In the present study we found that dexamethasone downregulated TRPA1 expression under all conditions tested. This is supported by our previous results showing that dexamethasone downregulated TRPA1 expression in chondrocytes, keratinocytes and lung epithelial cells under inflammatory conditions [12, 15, 40]. The full effect was achieved at rather small concentrations (0.1–1 µM). These results indicate that TRPA1 expression is sensitive to glucocorticoid treatment and that the effect is likely present in different types of inflammation. The results also suggest that TRPA1 downregulation is an additional anti-inflammatory/analgesic mechanism of action of glucocorticoids.
We also examined the effect of the PDE4 inhibitor rolipram [50] on TRPA1 expression. PDE4 is an intracellular enzyme catalyzing the hydrolysis of the major intracellular signaling molecule cyclic AMP (cAMP) to its inactive metabolites [51]. Therefore, inhibiting PDE4 results in increased intracellular cAMP levels following cell activation through various G-protein coupled receptors. This leads to the activation of protein kinase A and CREB transcription factor to modulate gene expression and inflammatory response [50]. The use of PDE4 inhibitors is approved in asthma and COPD [50]. In the present study we used the representative PDE4 inhibitor rolipram and did not observe a significant effect on TRPA1 expression. These data suggest that PDE4 inhibitors–and therefore pathways responsive to cAMP concentration–do not likely control TRPA1 expression in lung epithelial cells. However, we cannot exclude the possibility of an effect in some other conditions.
In the present study, the JAK inhibitors baricitinib and tofacitinib reversed the effects of IFN-γ and IL-4 on TRPA1 expression in a dose-dependent manner. Baricitinib at 1 µM drug concentration was sufficient to produce a maximal effect whereas tofacitinib seems to be somewhat less potent. Binding of IFN-γ to its receptor leads to signaling through JAK1 and JAK2 [47] whereas binding of IL-4 to the type II IL-4 receptor (predominant receptor in the epithelium) leads to JAK1, TYK2 and JAK2 activation [48]. Baricitinib is considered a selective JAK1/2 inhibitor, whereas tofacitinib was originally developed as a JAK3 inhibitor but is also found to inhibit JAK1 [52]. The observed difference in the potency of the inhibitors could be explained by these differences in cytokine signaling and JAK selectivity of the inhibitors. Among other indications, baricitinib is recommended for the treatment of severe COVID-19 infection [53]. Our results imply that in the inflammatory environment in the lung (for example during COVID-19 infection), JAK inhibitor therapy could up- or downregulate TRPA1 expression depending on the Th1-Th2 balance.
TRPA1 has been shown to promote leukocyte infiltration to the lung, including neutrophils in models of airway inflammation [20, 22, 28]. This could be partially explained by the findings that TRPA1 promotes the production of the neutrophil-attracting chemokine interleukin 8 (IL-8) [13,14,15,16, 18,19,20,21,22]. In the present study, we found that TRPA1 antagonists in all tested conditions significantly reduced CXCL6 and LCN2 production as measured by ELISA. CXCL6 is a chemokine and binds the same receptors as IL-8 [54,55,56,57], which leads to neutrophil chemotaxis and activation. CXCL6 is also linked to pulmonary fibrosis and cystic fibrosis; it is upregulated in these conditions [58, 59] and its inhibition could have a beneficial effect on remodeling in asthmatic lungs. LCN2 is a secreted protein, essential in innate immunity [60] and sequesters iron [61]. LCN2 has chemoattractant and immunomodulatory properties, for example promoting neutrophil chemotaxis [62,63,64]. In addition, LCN2 inhibits the growth of certain bacteria [65, 66].
Our results suggest that TRPA1 in the lung epithelium promotes CXCL6 and LCN2 production and could therefore be important in the innate immunity and neutrophil chemotaxis. This could further have consequences when targeting TRPA1 for pharmacotherapy. Anti-inflammatory effects could be expected through reduced neutrophil infiltration in the lungs when TRPA1 is inhibited and CXCL6 and LCN2 subsequently downregulated. On the other hand, decreased LCN2 levels as well as decreased neutrophilia might increase susceptibility to bacterial infection.
Conclusions
The present study reveals TRPA1 in the A549 model of lung epithelium as a factor regulated by Th1 and Th2-type inflammation: expressed and functioning predominantly under Th1-type inflammation and downregulated under Th2-type inflammation. We demonstrated the novel role of the JAKs and the transcription factor STAT6 in regulating TRPA1 expression and showed TRPA1 to be responsive to glucocorticoid treatment. We also discovered novel functions for TRPA1 in the lung epithelium in innate immunity and inflammation through regulating LCN2 and CXCL6 expression. We propose that the paradigm of Th1 and Th2-type inflammation is a major determinant of TRPA1 expression and function, and this should be considered when targeting TRPA1 for pharmacotherapy in (lung) disease.
Data availability
Data that support the findings and conclusions of this study are included within the article.
References
Talavera K, Startek JB, Alvarez-Collazo J, Boonen B, Alpizar YA, Sanchez A, et al. Mammalian transient receptor potential TRPA1 channels: from structure to disease. Physiol Rev. 2020. https://doi.org/10.1152/physrev.00005.2019.
Koivisto A-P, Belvisi MG, Gaudet R, Szallasi A. Advances in TRP channel drug discovery: from target validation to clinical studies. Nat Rev Drug Discov. 2021. https://doi.org/10.1038/s41573-021-00268-4.
Jordt S-E, Bautista DM, Chuang H, McKemy DD, Zygmunt PM, Högestätt ED, et al. Mustard oils and cannabinoids excite sensory nerve fibres through the TRP channel ANKTM1. Nat Publ Group. 2004;427:260–5.
Andrè E, Campi B, Materazzi S, Trevisani M, Amadesi S, Massi D, et al. Cigarette smoke–induced neurogenic inflammation is mediated by α, β-unsaturated aldehydes and the TRPA1 receptor in rodents. J of Clin Invest. 2008. https://doi.org/10.1172/JCI34886.
Takahashi N, Mizuno Y, Kozai D, Yamamoto S, Kiyonaka S, Shibata T, et al. Molecular characterization of TRPA1 channel activation by cysteine-reactive inflammatory mediators. Channels Taylor & Francis. 2008;2:287–98.
Andersson DA, Gentry C, Moss S, Bevan S. Transient receptor potential A1 is a sensory receptor for multiple products of oxidative stress. J Neurosci Soc Neurosci. 2008;28:2485–94.
Bessac BF, Sivula M, von Hehn CA, Escalera J, Cohn L, Jordt S-E. TRPA1 is a major oxidant sensor in murine airway sensory neurons. J Clin Invest. 2008;118:1899–910.
Taylor-Clark TE, Ghatta S, Bettner W, Undem BJ. Nitrooleic acid, an endogenous product of nitrative stress, activates nociceptive sensory nerves via the direct activation of TRPA1. Mol Pharmacol ASPET. 2009;75:820–9.
Nummenmaa E, Hamalainen M, Moilanen LJ, Paukkeri EL, Nieminen RM, Moilanen T, et al. Transient receptor potential ankyrin 1 (TRPA1) is functionally expressed in primary human osteoarthritic chondrocytes. Arthritis Res Ther England. 2016;18:184–5.
Atoyan R, Shander D, Botchkareva N, v. Non-Neuronal Expression of Transient Receptor Potential Type A1 (TRPA1) in Human Skin. J Investigat Dermatol. 2009;129:2312–5.
Jain A, Brnneke S, Kolbe L, Stb F, Wenck H, Neufang G. TRP-channel-specific cutaneous eicosanoid release patterns. Pain Elsevier. 2011;152:2765–72.
Luostarinen S, Hämäläinen M, Moilanen E. Transient receptor potential ankyrin 1 (TRPA1)-an inflammation-induced factor in human HaCaT Keratinocytes. Int J Mol Sci. 2021;22(7):3322.
Nassini R, Pedretti P, Moretto N, Fusi C, Carnini C, Facchinetti F, et al. Transient receptor potential ankyrin 1 channel localized to non-neuronal airway cells promotes non-neurogenic inflammation. PLoS ONE. 2012;7: e42454.
Mukhopadhyay I, Gomes P, Aranake S, Shetty M, Karnik P, Damle M, et al. Expression of functional TRPA1 receptor on human lung fibroblast and epithelial cells. J Recep Signal Transd. 2011;31:350–8.
Luostarinen S, Hämäläinen M, Hatano N, Muraki K, Moilanen E. The inflammatory regulation of TRPA1 expression in human A549 lung epithelial cells. Pulm Pharmacol Ther. 2021;70:102059.
Wang S, Shi P, Wang Y. TRPA1 ion channels in vagal afferent nerves contribute to ventilator-induced lung injury in a rat model. Gen Physiol Biophys. 2013;32:389–94.
Lin A-H, Liu M-H, Ko H-K, Perng D-W, Lee T-S, Kou YR. Lung Epithelial TRPA1 transduces the extracellular ROS into transcriptional regulation of lung inflammation induced by cigarette smoke: the role of influxed Ca 2+. Mediators Inflamm. 2015;2015:1–16.
Prandini P, de Logu F, Fusi C, Provezza L, Nassini R, Montagner G, et al. Transient receptor potential ankyrin 1 channels modulate inflammatory response in respiratory cells from patients with cystic fibrosis. Am J Respir Cell Mol Biol. 2016;55:645–56.
Wang M, Zhang Y, Xu M, Zhang H, Chen Y, Chung KF, et al. Roles of TRPA1 and TRPV1 in cigarette smoke -induced airway epithelial cell injury model. Free Radic Biol Med. 2019;134:229–38.
Ko H-K, Lin A-H, Perng D-W, Lee T-S, Kou YR. Lung epithelial TRPA1 Mediates lipopolysaccharide-induced lung inflammation in bronchial epithelial cells and mice. Front Physiol. 2020. https://doi.org/10.3389/fphys.2020.596314.
Yap JMG, Ueda T, Takeda N, Fukumitsu K, Fukuda S, Uemura T, et al. An inflammatory stimulus sensitizes TRPA1 channel to increase cytokine release in human lung fibroblasts. Cytokine. 2020;129: 155027.
Fang Z, Yi F, Peng Y, Zhang J, (Jim), Zhang L, Deng Z, et al. Inhibition of TRPA1 reduces airway inflammation and hyperresponsiveness in mice with allergic rhinitis. FASEB J. 2021. https://doi.org/10.1096/fj.201902627R.
Nummenmaa E, Hämäläinen M, Pemmari A, Moilanen LJ, Tuure L, Nieminen RM, et al. Transient receptor potential ankyrin 1 (TRPA1) Is involved in upregulating interleukin-6 expression in osteoarthritic chondrocyte models. Int J Mol Sci. 2020;22:87.
Hajna Z, Csekő K, Kemény Á, Kereskai L, Kiss T, Perkecz A, et al. Complex regulatory role of the TRPA1 receptor in acute and chronic airway inflammation mouse models. Int J Mol Sci. 2020;21:4109.
Caceres AI, Brackmann M, Elia MD, Bessac BF, del Camino D, D’Amours M, et al. A sensory neuronal ion channel essential for airway inflammation and hyperreactivity in asthma. Proc Natl Acad Sci. 2009;106:9099–104.
Wu Y, You H, Ma P, Li L, Yuan Y, Li J, et al. Role of transient receptor potential ion channels and evoked levels of neuropeptides in a formaldehyde-induced model of asthma in BALB/c mice. PLoS ONE. 2013;8:e62827.
Li M, Fan X, Yue Q, Hu F, Zhang Y, Zhu C. The neuro-immune interaction in airway inflammation through TRPA1 expression in CD4+ T cells of asthmatic mice. Int Immunopharmacol. 2020;86: 106696.
Balestrini A, Joseph V, Dourado M, Reese RM, Shields SD, Rougé L, et al. A TRPA1 inhibitor suppresses neurogenic inflammation and airway contraction for asthma treatment. J Exp Med. 2021. https://doi.org/10.1084/jem.20201637.
Sun Y, Liu M, Fan X, Zhou L, Li M, Hu F, et al. Effects of cigarette smoke on the aggravation of ovalbumin-induced asthma and the expressions of TRPA1 and tight junctions in mice. Mol Immunol. 2021;135:62–72.
Hatano N, Itoh Y, Suzuki H, Muraki Y, Hayashi H, Onozaki K, et al. Hypoxia-inducible factor-1alpha (HIF1alpha) switches on transient receptor potential ankyrin repeat 1 (TRPA1) gene expression via a hypoxia response element-like motif to modulate cytokine release. J Biol Chem United States. 2012;287:31962–72.
Meng J, Wang J, Steinhoff M, Dolly JO. TNFα induces co-trafficking of TRPV1/TRPA1 in VAMP1-containing vesicles to the plasmalemma via Munc18–1/syntaxin1/SNAP-25 mediated fusion. Sci Rep. 2016;6:21226.
Nugent M, Yusef YR, Meng J, Wang J, Dolly JO. A SNAP-25 cleaving chimera of botulinum neurotoxin /A and /E prevents TNFα−induced elevation of the activities of native TRP channels on early postnatal rat dorsal root ganglion neurons. Neuropharmacology. 2018;138:257–66.
Takahashi K, Ohta T. Membrane translocation of transient receptor potential ankyrin 1 induced by inflammatory cytokines in lung cancer cells. Biochem Biophys Res Commun. 2017;490:587–93.
Schmidt M, Dubin AE, Petrus MJ, Earley TJ, Patapoutian A. Nociceptive signals induce trafficking of TRPA1 to the plasma membrane. Neuron Elsevier. 2009;64:498–509.
Bandell M, Story GM, Hwang SW, Viswanath V, Eid SR, Petrus MJ, et al. Noxious cold ion channel TRPA1 is activated by pungent compounds and bradykinin. Neuron Elsevier. 2004;41:849–57.
Dai Y, Wang S, Tominaga M, Yamamoto S, Fukuoka T, Higashi T, et al. Sensitization of TRPA1 by PAR2 contributes to the sensation of inflammatory pain. J Clin Invest United States. 2007;117:1979–87.
Wang S, Dai Y, Fukuoka T, Yamanaka H, Kobayashi K, Obata K, et al. Phospholipase C and protein kinase A mediate bradykinin sensitization of TRPA1: a molecular mechanism of inflammatory pain. Brain. 2008;131:1241–51.
Wilson SR, Th L, Batia LM, Beattie K, Katibah GE, McClain SP, et al. The epithelial cell-derived atopic dermatitis cytokine TSLP activates neurons to induce itch. Cell. 2013;155:285–95.
Malin S, Molliver D, Christianson JA, Schwartz ES, Cornuet P, Albers KM, et al. TRPV1 and TRPA1 function and modulation are target tissue dependent. J Neurosci Soc Neurosci. 2011;31:10516–28.
Nummenmaa E, Hämäläinen M, Moilanen LJ, Moilanen T, Vuolteenaho K, Moilanen E. TRPA1 expression is downregulated by dexamethasone and aurothiomalate in human chondrocytes: TRPA1 as a novel factor and drug target in arthritis. RMD Open. 2017;3:e000556.
Wan YY. Multi-tasking of helper T cells. Immunology. 2010;130:166–71.
Geginat J, Paroni M, Maglie S, Alfen JS, Kastirr I, Gruarin P, et al. Plasticity of human CD4 T cell subsets. Front Immunol. 2014. https://doi.org/10.3389/fimmu.2014.00630.
Holgate ST, Wenzel S, Postma DS, Weiss ST, Renz H, Sly PD. Asthma. Nat Rev Dis Primers. 2015;1:15025.
Papi A, Brightling C, Pedersen SE, Reddel HK. Asthma. The Lancet. 2018;391:783–800.
Kuruvilla ME, Lee FE-H, Lee GB. Understanding asthma phenotypes, endotypes, and mechanisms of disease. Clin Rev Allergy Immunol. 2019;56:219–33.
Moilanen LJ, Hamalainen M, Lehtimaki L, Nieminen RM, Muraki K, Moilanen E. Pinosylvin Inhibits TRPA1-induced calcium influx in vitro and trpa1-mediated acute paw inflammation in vivo. Basic Clin Pharmacol Toxicol England. 2016;118:238–42.
Ivashkiv LB. IFNγ: signalling, epigenetics and roles in immunity, metabolism, disease and cancer immunotherapy. Nat Rev Immunol. 2018;18:545–58.
Junttila IS. Tuning the cytokine responses: an update on interleukin (IL)-4 and IL-13 receptor complexes. Front Immunol. 2018;9:888.
Nagashima S, Yokota M, Nakai E, Kuromitsu S, Ohga K, Takeuchi M, et al. Synthesis and evaluation of 2-{[2-(4-hydroxyphenyl)-ethyl]amino}pyrimidine-5-carboxamide derivatives as novel STAT6 inhibitors. Bioorg Med Chem. 2007;15:1044–55.
Li H, Zuo J, Tang W. Phosphodiesterase-4 Inhibitors for the treatment of inflammatory diseases. Front Pharmacol. 2018. https://doi.org/10.3389/fphar.2018.01048.
Maurice DH, Ke H, Ahmad F, Wang Y, Chung J, Manganiello VC. Advances in targeting cyclic nucleotide phosphodiesterases. Nat Rev Drug Discov. 2014;13:290–314.
Tanaka Y, Luo Y, O’Shea JJ, Nakayamada S. Janus kinase-targeting therapies in rheumatology: a mechanisms-based approach. Nat Rev Rheumatol. 2022;18:133–45.
Agarwal A, Rochwerg B, Lamontagne F, Siemieniuk RA, Agoritsas T, Askie L, et al. A living WHO guideline on drugs for covid-19. BMJ. 2020;M3379.
Proost P, de Wolf-Peeters C, Conings R, Opdenakker G, Billiau A, van Damme J. Identification of a novel granulocyte chemotactic protein (GCP-2) from human tumor cells. In vitro and in vivo comparison with natural forms of GRO IP-10 and IL-8. J Immunol. 1993;150:1000–10.
Proost P, Wuyts A, Conings R, Lenaerts JP, Billiau A, Opdenakker G, et al. Human and bovine granulocyte chemotactic protein-2: complete amino acid sequence and functional characterization as chemokines. Biochemistry. 1993;32:10170–7.
Wuyts A, van Osselaer N, Haelens A, Samson I, Herdewijn P, Ben-Baruch A, et al. Characterization of synthetic human granulocyte chemotactic protein 2: usage of chemokine receptors cxcr1 and cxcr2 and in vivo inflammatory properties. Biochemistry. 1997;36:2716–23.
Russo RC, Garcia CC, Teixeira MM, Amaral FA. The CXCL8/IL-8 chemokine family and its receptors in inflammatory diseases. Expert Rev Clin Immunol. 2014;10:593–619.
Jovic S, Linge HM, Shikhagaie MM, Olin AI, Lannefors L, Erjefält JS, et al. The neutrophil-recruiting chemokine GCP-2/CXCL6 is expressed in cystic fibrosis airways and retains its functional properties after binding to extracellular DNA. Mucosal Immunol. 2016;9:112–23.
Besnard A-G, Struyf S, Guabiraba R, Fauconnier L, Rouxel N, Proost P, et al. CXCL6 antibody neutralization prevents lung inflammation and fibrosis in mice in the bleomycin model. J Leukoc Biol. 2013;94:1317–23.
Guardado S, Ojeda-Juárez D, Kaul M, Nordgren TM. Comprehensive review of lipocalin 2-mediated effects in lung inflammation. Am J Physiol-Lung Cell Mole Physiol. 2021;321:L726–33.
Flo TH, Smith KD, Sato S, Rodriguez DJ, Holmes MA, Strong RK, et al. Lipocalin 2 mediates an innate immune response to bacterial infection by sequestrating iron. Nature. 2004;432:917–21.
Schroll A, Eller K, Feistritzer C, Nairz M, Sonnweber T, Moser PA, et al. Lipocalin-2 ameliorates granulocyte functionality. Eur J Immunol. 2012;42:3346–57.
Shao S, Cao T, Jin L, Li B, Fang H, Zhang J, et al. Increased Lipocalin-2 contributes to the pathogenesis of psoriasis by modulating neutrophil chemotaxis and cytokine secretion. J Invest Dermatol. 2016;136:1418–28.
Wang Q, Li S, Tang X, Liang L, Wang F, Du H. Lipocalin 2 protects against escherichia coli infection by modulating neutrophil and macrophage function. Front Immunol. 2019. https://doi.org/10.3389/fimmu.2019.02594.
Saiga H, Nishimura J, Kuwata H, Okuyama M, Matsumoto S, Sato S, et al. Lipocalin 2-dependent inhibition of mycobacterial growth in alveolar epithelium. J Immunol. 2008;181:8521–7.
Dahl SL, Woodworth JS, Lerche CJ, Cramer EP, Nielsen PR, Moser C, et al. Lipocalin-2 Functions as Inhibitor of Innate Resistance to Mycobacterium tuberculosis. Front Immunol. 2018. https://doi.org/10.3389/fimmu.2018.02717.
Acknowledgements
We wish to thank Ms Meiju Kukkonen and Ms Niina Ikonen for their excellent technical assistance.
Funding
Open access funding provided by Tampere University including Tampere University Hospital, Tampere University of Applied Sciences (TUNI). The study was supported by grants by the Research Foundation of Rheumatic Diseases, Finland; Tampere Tuberculosis Foundation, Finland; The Finnish Cultural Foundation; The Finnish Medical Foundation; The Academy of Finland; and the Competitive research funding (VTR funding) of Tampere University Hospital. Open access funding was provided by Tampere University. The funding bodies had no role in the study design, or in data collection, analysis or interpretation, or in the writing of the manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conceptualization and design. SL performed the experiments and the statistical analysis. All authors contributed to the analysis and interpretation of the data. SL wrote the draft of the manuscript, and all authors were involved in the reviewing and editing of the submitted article. EM supervised the study and had a major role in the project administration and funding acquisition.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Responsible Editor: John Di Battista.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Luostarinen, S., Hämäläinen, M., Pemmari, A. et al. The regulation of TRPA1 expression and function by Th1 and Th2-type inflammation in human A549 lung epithelial cells. Inflamm. Res. 72, 1327–1339 (2023). https://doi.org/10.1007/s00011-023-01750-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00011-023-01750-y