Abstract
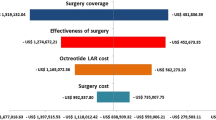
Background: At the time of diagnosis, macroadenomas represent 60–80% of GH secreting adenomas, of which 25–30% are invasive macroadenomas. These aggressive tumors have the worst surgical success rates in terms of cure, and often need several therapeutic approaches in order to control disease status. Acromegalic patients are subject to increased mortality and important health resource consumption related to their associated co-morbidities, in addition to the costs that are related to diagnosis itself and initial treatment of the disease. Objective: Assessment of the cost of initial management and outcome of acromegalic patients with invasive pituitary adenomas. Study design: Retrospective and observational study of review of records. Setting: Two tertiary hospitals. Patients: 11 consecutive patients between 18 and 80 yr old diagnosed with acromegaly due to an invasive pituitary macroadenoma. Intervention: Collection of data of biochemical and radiological tests, specialist visits, hospitalisation, surgery, pharmacological and radiotherapy treatment at diagnosis and over 4 yr of follow-up after initial treatment. Costs were evaluated using the data of the Centre for Health Economics and Social Policy Studies and the Official College of Pharmacists of Spain. Main outcome measure: Global and patient/yr follow-up costs of illness. Results: The mean costs for acromegaly for the period of follow-up ranged from 7,072 to 9,874 €/patient/yr, for biochemically non-controlled (no.=6) and controlled patients (no.=5) respectively. The most important cost in the perioperative period was for admission in the intensive care unit. After surgery, SS analogues were the principal contributors to the economic burden. Conclusion: In this paper we have for the first time presented a pharmacoeconomic study of GH secreting invasive macroadenoma. The poor prognosis of our cohort of patients and the higher rate of controlled patients and normal IGF-I levels warrant the employment of multiple therapeutic options. The cost associated with this treatment in this complex disease of low prevalence is not excessive and can be supported by healthcare services.
Similar content being viewed by others
References
Etxabe J, Gaztambide J, Latorre P, Vazquez JA. Acromegaly: an epidemiological study. J Endocrinol Invest 1993, 16: 181–7.
Mestrón A, Webb SM, Astorga R, et al. Epidemiology, clinical characteristics, outcome, morbidity and mortality in acromegaly based on the Spanish Acromegaly Registry (Registro Español de Acromegalia, REA). Eur J Endocrinol 2004, 151: 439–46.
Melmed S. Acromegaly. N Engl J Med 1990, 322: 966–77.
Minniti G, Jaffrain-Rea M-L, Esposito V, Santoro A, Tamburrano G, Cantore G. Evolving criteria for post-operative biochemical remission of acromegaly: can we achieve a definitive cure? An audit of surgical results on a large series and a review of the literature. Endocr RelatCancer 2003, 10: 611–9.
Beauregard C, Truong U, Hardy J, Serri O. Long-term outcome and mortality after transsphenoidal adenomectomy for acromegaly. Clin Endocrinol (Oxf) 2003, 58: 86–91.
Besser GM, Burman P, Daly AF. Predictors and rates of treatment-resistant tumor growth in acromegaly. Eur J Endocrinol 2005, 1 53: 187–93.
Orme SM, McNally RJ, Cartwright RA, Belchetz PE. Mortality and cancer incidence in acromegaly: a retrospective cohort study. United Kingdom Acromegaly Study Group. J Clin Endocrinol Metab 1998, 83: 2730–4.
Colao A, Ferone D, Marzullo P, Lombardi G. Systemic complications of acromegaly: epidemiology, pathogenesis and management. Endocr Rev 2004, 25: 102–52.
Weekes LM, Ho KK, Seale JP. Treatment options in acromegaly. Benefits and costs. Pharmacoeconomics 1996, 10: 453–9.
Abosch A, Tyrell JB, Lamborn KR, Hannegan LT, Applebury CB, Wilson CB. Transsphenoidal microsurgery for growth hormone-secreting pituitary adenomas: initial outcome and long-term results. J Clin Endocrinol Metab 1998, 83: 3411–8.
Swearingen B, Barker II FG, Katznelson L, et al. Long-term mortality after transsphenoidal surgery and adjunctive therapy for acromegaly. J Clin Endocrinol Metab 1998, 83: 3419–26.
Ayuk J, Clayton RN, Holder G, Sheppard MC, Stewart PM, Bates AS. Growth hormone and pituitary radiotherapy, but notserum insulin-like growth factor-1 concentrations predict excess mortality in patients with acromegaly. J Clin Endocrinol Metab 2004, 89: 1613–7.
Giustina A, Barkan A, Casanueva FF, et al. Criteria for cure of acromegaly: a consensus statement. J Clin Endocrinol Metab 2000, 85: 526–9.
Holdaway IM, Rajasoorya RC, Gamble GD. Factors influencing mortality in acromegaly. J Clin Endocrinol Metab 2004, 89: 667–74.
Melmed S, Casanueva FF, Cavagnini F, et al. Guidelines for acromegaly management. J Clin Endocrinol Metab 2002, 87: 4054–8.
Freda PU, Katznelson L, van der Lely AJ, Reyes CM, Zhao S, Rabinowitz D. Long-acting somatostatin analog therapy of acromegaly: a meta-analysis. J Clin Endocrinol Metab 2005, 90: 4465–73.
Barrande G, Pittino-Lungo M, Coste J, et al. Hormonal and metabolic effects of radiotherapy in acromegaly: long-term results in 128 patients followed in a single center. J Clin Endocrinol Metab 2000, 85: 3779–85.
Castinetti F, Taieb D, Kuhn JM, et al. Outcome of gamma knife radiosurgery in 82 patients with acromegaly: correlation with initial hypersecretion. J Clin Endocrinol Metab 2005, 90: 4483–8.
Wilson LS, Shin JL, Ezzat S. Longitudinal assessment of economic burden and clinical outcomes in acromegaly. Endocr Pract 2001, 7: 170–80.
Didoni G, Grottol S, Gasco V, et al. Cost-of-illness study in acromegalic patients in Italy. J Endocrinol Invest 2004, 27: 1034–9.
Melmed S, Casanueva F, Cavagnini F, et al. Consensus statement: medical treatment of acromegaly. Eur J Endocrinol 2005, 153: 737–40.
Ehrnborg C, Hakkaart-Van Roijen L, Jonsson B, Rutten FF, Bengtsson BA, Rosén T. Cost of illness in adult patients with hypopituitarism. Pharmacoeconomics 2000, 17: 621–8.
Author information
Authors and Affiliations
Corresponding author
Additional information
M. L-R. and C. V. have contributed equally to this manuscript.
Rights and permissions
About this article
Cite this article
Luque-Ramirez, M., Paramo, C., Varela da Costa, C. et al. Cost of management of invasive growth hormone-secreting macroadenoma. J Endocrinol Invest 30, 541–545 (2007). https://doi.org/10.1007/BF03346346
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03346346