Abstract
Background
Deep vein thrombosis (DVT) and pulmonary embolism (PE) are manifestations of venous thromboembolic events (VTEs). Patients undergoing major surgical procedures such as total hip replacement (THR), total knee replacement (TKR), and hip fracture surgery (HFS) are at an elevated risk for VTEs. The American College of Chest Physicians’ (ACCP) guidelines recommend that such patients receive thromboprophylaxis for at least 10 days. In patients undergoing THR or HFS, extended prophylaxis for up to 28–35 days is the recommended approach for those at high risk of thromboembolic events. The NAFT (North American Fragmin Trial) compared the prophylactic efficacy of dalteparin with that of warfarin during the in-hospital period, and with that of placebo during the period of hospital discharge until day 35 postsurgery, in patients who underwent total hip arthroplasty. During both the in-hospital and the post-discharge time periods, dalteparin significantly reduced the occurrence of DVT. Given the clinical relevance of these results, the low specificity of the ACCP recommendations regarding optimal prophylaxis duration, and the importance of optimizing the efficiency of DVT prophylaxis in the practice setting, a cost-utility analysis was conducted comparing dalteparin 10-day and 35-day (extended) with a warfarin 10-day protocol, in patients undergoing major orthopedic surgeries such as THR, TKR, or HFS.
Design and setting
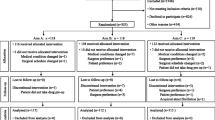
A three-arm decision model was developed using the prevalence of symptomatic DVT from NAFT publications, epidemiologic studies, and published meta-analyses. Healthcare resource use was abstracted from a survey of clinicians and from the economic literature. Utility estimates were obtained by interviewing a sample of 24 people from the general public using the time trade-off technique. The clinical, economic and utility data were then used to estimate the cost per quality-adjusted life-year (QALY) gained with dalteparin for 10 or 35 days relative to 10 days of warfarin.
Study perspective
Canadian provincial healthcare system.
Main outcome measures and results
The cost per QALY gained with 10 days of dalteparin was below $Can1000 for all the surgeries evaluated (all costs are reported in 2007 Canadian dollars [$Can1 = $US1, as of December 2007]). In the case of extended prophylaxis, the incremental cost per QALY gained with 35 days of dalteparin over warfarin was $Can40 100, $Can46 500, and $Can31 200 for patients undergoing THR, TKR, and HFS, respectively. Reducing the duration of prophylaxis from 35 to 28 days generated ratios that were below $Can35 000 for all three surgeries evaluated.
Conclusions
Ten days of dalteparin following major orthopedic surgery is a clinically and economically attractive alternative to warfarin for DVT prophylaxis. In the case of the 35-day dalteparin protocol, the results also indicated acceptable economic value to a publicly funded healthcare system, particularly in the settings of HFS and THR. In addition, reducing the duration of prophylaxis to 28 days postsurgery would be associated with a more favorable return on public healthcare expenditures.








Similar content being viewed by others
References
Pineo GF. New developments in the prevention and treatment of venous thromboembolism. Pharmacotherapy 2001; 21: S51–6
Weinmann EE, Salzman EW. Deep vein thrombosis. N Engl J Med 1994; 331: 1630–41
Landefeld CS, Ilanus P. Economic burden of venous thromboembolism. In: Jones J, editor. Prevention of venous thrombosis. New York: Marcel Dekker, 1993: 69–85
Kearon C. Duration of thromboembolism prophylaxis after surgery. Chest 2003; 124: 386S–2S
Colwell Jr CW, Spiro TE, Trowbridge AA, et al. Efficacy and safety of enoxaparin versus unfractionated heparin for prevention of deep venous thrombosis after elective knee arthroplasty. Clin Orthop 1995; 321: 19–27
Colwell Jr CW, Spiro TE, Trowbridge AA, et al. Use of enoxaparin, a low-molecular-weight heparin, and unfractionated heparin for the prevention of deep venous thrombosis after elective hip replacement: a clinical trial comparing efficacy and safety. J Bone Joint Surg Am 1994; 76: 3–14
Drummond MF, Aristides M, Davies L, et al. Economic evaluation of standard heparin and enoxaparin for prophylaxis against deep vein thrombosis in elective hip surgery. Br J Surg 1994; 81: 1742–6
Rodger M, Bredeson C, Wells PS, et al. Cost effectiveness of low molecular weight heparin and unfractionated heparin in the treatment of deep vein thrombosis. CMAJ 1998; 159: 931–8
Boccalon H, Elias A, Chale JJ, et al. Clinical outcome and cost of hospital vs. home treatment of proximal deep vein thrombosis with a low-molecular-weight heparin: the Vascular Midi-Pyrenees study. Arch Intern Med 2000; 160: 1769–73
Hull RD, Pineo GF, Francis C, et al. Low-molecular-weight heparin prophylaxis using dalteparin in close proximity to surgery vs. warfarin in hip arthroplasty patients: a double-blind, randomized comparison. Arch Intern Med 2000; 160: 2199–207
Hull RD, Pineo GF, Francis C, et al. Low-molecular-weight heparin prophylaxis using dalteparin extended out of hospital vs. in-hospital warfarin/out of hospital placebo in hip arthroplasty patients: a double-blind, randomized comparison. Arch Intern Med 2000; 160: 2208–15
Geerts WH, Pinei GF, Heit JA, et al. Prevention of venous thromboembolism: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest 2004; 126 (3 Suppl. 3): 338S–400S
Hip and knee replacements in Canada. The Canadian Joint Replacement Registry Report. Ottawa (ON): Canadian Institute for Health Information, 2006
Buller HR, Agnelli G, Hull RD, et al. Antithrombotic therapy for venous thromboembolic disease: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest 2004 Sep; 126 (3 Suppl.): 401S–28S
McCart GM, Kayser SR. Therapeutic equivalency of low-molecular-weight heparins. Ann Pharmacother 2002; 36: 1042–57
Torrance GW. Utility approach to measuring health-related quality of life. J Chron Dis 1987; 40: 593–600
Gafni A. Alternatives to the QALY measure for economic evaluations. Support Care Cancer 1997; 5: 105–11
Schedule of benefits: physician services under the Health Insurance Act. Toronto (ON): Ontario Ministry of Health and Long-Term Care, 2005
Canadian Agency for Drugs and Technology in Health. Guidelines for the economic evaluation of health technologies. 3rd ed. Ottawa (ON): CADTH, 2006 [online]. Available from URL: http://www.cadth.ca/media/pdf/186_EconomicGuidelines_e.pdf [Accessed 2007 Apr 20]
Russell LB, Gold MR, Siegel JE, et al. The role of cost-effectiveness analysis in health and medicine. JAMA 1996; 276: 1172–77
Skedgel C, Goeree R, Pleasance S, et al. The cost effectiveness of extended duration antithrombotic prophylaxis after total hip arthroplasty. J Bone Joint Surg Am 2007; 89: 819–28
Eikelboom JW, Quinlan DJ, Douketis JD. Extended duration prophylaxis against venous thromboembolism after total hip or knee replacement: a meta analysis of the randomized trials. Lancet 2001; 358: 9–15
Hull RD, Pineo GF, Stein PD, et al. Extended out of hospital low molecular weight heparin prophylaxis against deep vein thrombosis in patients after elective hip arthroplasty: a systematic review. Ann Intern Med 2001; 135: 858–69
Prevention of pulmonary embolism and deep vein thrombosis with low dose aspirin: Pulmonary Embolism Prevention Trial. Lancet 2000; 355: 1295–302
Statistics Canada. Annual report, 2007. Ottawa (ON): Statistics Canada, 2007
Hull RD, Pineo GF, Raskob GE. The economic impact of treating deep vein thrombosis with low molecular weight heparin: outcome of therapy and health economic aspects. Haemostasis 1998; 28 Suppl. 3: 8–16
Canadian Agency for Drugs and Technology in Health. Recommendations and status on drug subsmissions [online]. Available from URL: http://www.cadth.ca/index.php/en/cdr/recommendations [Accessed 2007 Sep 13]
Friesen E, Lier D, Bachynsky J, et al. An economic comparison of enoxaparin and warfarin in the prevention of deep vein thrombosis after hip and knee replacement. Can J Hosp Pharm 2002; 55: 128–35
Acknowledgments
This study was funded by Pfizer Canada Inc. George Dranitsaris has acted as a consultant to Pfizer Canada Inc. Carmine Stumpo, Reginald Smith, and William Bartle received honoraria from Pfizer Canada Inc. for providing clinical expertise throughout this study. The corresponding author had full access to all the data in the study and had the final responsibility for the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
For cost data for hospital healthcare resources obtained from Canadian sources, see table AI.
Rights and permissions
About this article
Cite this article
Dranitsaris, G., Stumpo, C., Smith, R. et al. Extended Dalteparin Prophylaxis for Venous Thromboembolic Events. Am J Cardiovasc Drugs 9, 44–58 (2009). https://doi.org/10.1007/BF03256594
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03256594