Abstract
Background
Recent trials have shown that high-dose HMG-CoA reductase inhibitor (statin) therapy reduces cardiovascular events in high-risk subjects within weeks of initiating therapy. We investigated the effect of time to titration to maximum dose of statin therapy on cardiovascular events.
Methods
From a list of all patients actively taking simvastatin 80 mg/day as of April 2003 at our hospital, two clinical pharmacists reviewed 213 electronic medical records including pharmacy records from November 1992 to April 2003. Data on cardiovascular risk factors, laboratory results, titration schedules, and outcomes were extracted from the electronic database. Titration period time frames were compared between patient groups using a Student t-test and multiple-variable logistic regression to account for other risk factors.
Results
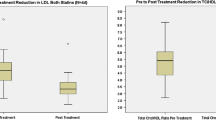
Titration schedules and time frames to attain a regimen of simvastatin 80 mg/day were available for 154 (73%) subjects. Titrations ranged from 1 to 8 and averaged 2.3± 1.3 titrations per patient (median titrations = 2) over 1 month to 8.4 years. On follow-up, 47 patients experienced 80 cardiovascular-related outcomes. The average time to titration to maximum dose of statin therapy was longer for patients who experienced a cardiac event than for those who did not (3.5 ± 2.2 vs 2.1 ± 1.8 years; p = 0.0004). After accounting for other risk factors, the titration period was still significantly related to the presence of a cardiac event (p = 0.0060, odds ratio per month increase in the titration period 1.3, 95% CI 1.08, 1.58).
Conclusions
Despite potential limitations, the results of our study show that an excessive delay in titrating statin therapy to the optimal dose may lead to an increased risk of atherosclerosis-related events in high-risk patients.





Similar content being viewed by others
Notes
Data on patient entry date were not available for 1 patient with cardiovascular events and 13 patients without cardiovascular events.
References
Ridker PM, Cannon CP, Morrow D, et al., On behalf of the Pravastatin or Atorvastatin Evaluation and Infection Therapy-Thrombolysis in Myocardial Infarction 22 (PROVE IT-TIMI 22) Investigators. C-reactive protein levels and outcomes after statin therapy. N Engl J Med 2005; 352: 20–8
MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20536 high-risk individuals: a randomized placebo-controlled trial. Lancet 2002; 360: 7–22
Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III). JAMA 2001; 285: 2486–97
Plenge JK, Hernandez TL, Weil KM, et al. Simvastatin lowers C-reactive protein within 14 days: an effect independent of low-density lipoprotein cholesterol reduction. Circulation 2002; 106: 1447–52
Zocor (simvastatin) [package insert]. Whitehouse Station (NJ): Merck & Co., Inc., 2002 May.
Koren MJ, Smith DG, Hunninghake DB, et al. The cost of reaching National Cholesterol Education Program (NCEP) goals in hypercholestrolemic patients. Pharmacoeconomics 1998; 14: 59–70
Wright RS, Murphy JG, Bybee KA, et al. Statin lipid-lowering therapy for acute myocardial infarction and unstable angina: efficacy and mechanism of benefit. Mayo Clin Proc 2002; 77: 1085–92
Grundy SM, Cleeman JI, Merz NB, et al. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III Guidelines. Circulation 2004; 110: 227–39
Newman CB, Palmer G, Silbershatz H, et al. Safety of atorvastatin derived from analysis of 44 completed trials in 9416 patients. Am J Cardiol 2003; 92: 670–6
Ray KK, Cannon CP, McCabe CH, et al., On behalf of the PROVE IT-TIMI 22 Investigators. Early and late benefits of high-dose atorvastatin in patients with acute coronary syndromes: results from the PROVE IT-TIMI 22 trial. J Am Coll Cardiol 2005; 46: 1405–10
Acknowledgments
Tamara Evans is an employee of Pfizer. The other authors have no conflicts of interest that are directly relevant to the content of this study. No sources of funding were used to assist in the preparation of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Friend, A.S., Kamalesh, M., Schellhase, E. et al. Effect of Time to Titration to Maximum Dose of Statins on Cardiovascular Outcomes. Am J Cardiovasc Drugs 9, 103–107 (2009). https://doi.org/10.1007/BF03256581
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03256581