Abstract
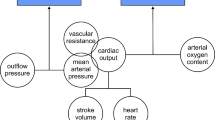
The application of cardiopulmonary bypass (CPB) using a heart-lung machine in open heart surgery is associated with numerous pathophysiological changes in the vascular system and the neurohormonal environment. In this study our purpose was to investigate whether the hormones brain natriuretic peptide (BNP) and ghrelin are involved in changes in the systemic vascular resistance index (SVRI) after CPB, using data from 20 patients who had undergone coronary artery by pass grafting accompanied by CPB. Hemodynamic measurements were obtained using a thermodilution catheter and included cardiac index and systemic vascular resistance index. Blood samples were taken before CPB, after CPB, and at 0 and 24 h postoperatively. The blood levels of total and acylated ghrelin were quantified by radioimmunoassay. Blood levels of BNP were measured by a fluorescence immunoassay kit. The SVRI was significantly higher at the end of CPB and at 0 h postoperatively than before CPB (end of CPB: 4282±1035 dyne·s·cm−5·m−2, 0 h postoperatively: 3239±635 dyne·s·cm−5·m−2 vs. before CPB: 2289±330 dyne·s·cm−5·m−2, p<0.05). Total and acylated ghrelin levels decreased until 0 h postoperatively but the change was not statistically significant. However, at 24 h after surgery, they showed a statistically significant increase over the initial ghrelin values (total before CPB: 1413.71±287.93 pg/ml vs. 24 h postoperatively: 1736.85±236.89 pg/ml; acylated ghrelin before CPB: 55.85±25.53 pg/ml vs. 24 h postoperatively: 106.28±30.86 pg/ml; p<0.05 for both). BNP values were markedly lower after than before CPB (before CPB: 69.07±48 pg/ml vs. after CPB: 21.96±13 pg/ml, p<0.05) and reached a maximum value 24 h postoperatively (before CPB: 56.3±42 vs. after CPB: 454.7±229 pg/ml, p<0.05). There was a weak negative correlation between the changes in SVRI and total and acylated ghrelin levels after the CPB period, but this was not statistically significant. However, there was a statistically significant negative correlation between SVRI and BNP after CPB and at 24 h postoperatively (r:−0.709, p<0.01 and r:−0.649, p<0.03, respectively). Taken together, our results show that the observed initial increases in ghrelin and/or BNP in the postoperative period (at 24 h) might be causally related to the decrease in the SVRI in the same period. However, further investigations are needed to clarify the significance of this observation with respect to that of SVRI.
Resumen
Se investiga si las hormonas ghrelina y péptido natriurético B (BNP) están implicadas en los cambios del índice de resistencia vascular sistémica (SVRI) tras circulación extracorporal (CE). En 20 pacientes a los que se había practicado derivación aortocoronaria con circulación extracorporal, se relaizaron medidas hemodinámicas y determinaciones plasmáticas de ghrelina y BNP antes y después de la CE y 0h y 24h tras la operación. Los valores de SVRI fueron mayores tras CE y 0h tras la cirugía Los niveles de ghrelina y de BNP alcanzaron niveles máximos 24 h tras la cirugía. Los resultados sugieren que los incrementos de ghrelina y de BNP 24 h tras la cirugía podrían estar causalmente relacionados con la disminución de SVRI en el mismo período.
Similar content being viewed by others
References
Avidan, M.S., Meehan, N., Ponte, J., El-Gamel, A., Sherwood, R.A. (2001): Changes in brain natriuretic peptide concentrations following open cardiac surgery with cardioplegic cardac arrest. Clin Chim Acta, 303, 127–132.
Aydin, S. (2007): Discovery of ghrelin hormone, its researches and its clinical applications. Turkish J Biochem, 32, 76–89.
Broglio, F., Gottero, C., Prodam, F., Gauna, C., Muccioli, G., Papotti, M., Abribat, T., Van Der Lely, A.J., Ghigo, E. (2004): Non-acylated ghrelin counteracts the metabolic but not the endocrine response to acylated ghrelin in humans. J Clin Endocrinol Metab, 89, 3062–3065.
Cao, J.M., Ong, H., Chen, C. (2006): Effects of ghrelin and synthetic GH secretagogues on the cardiovascular system. Trends Endocrinol Metab, 17, 13–18.
Christakis, G.T., Fremes, S.E., Koch, JP, Harwood S, Juhasz S, Sharpe E, Deemar KA, Hamilton C, Chen E, Rao V. (1994): Determinats of low systemic vascular resistance during cardiopulmonary bypass. Ann Thorac Surg, 58, 1040–1049.
Gröschl, M., Uhr, M., Kraus, T. (2004): Evaluation of the comparability of commercial ghrelin assays. Clin Chem, 50, 457–458.
Hosada, H., Doi, K., Nagaya, N., (2004): Optimum collection and storage conditions for ghrelin measurements: octanoyl modification of ghrelin is rapidly hydrolyzed to deacyl ghrelin in blood samples. Clin Chem, 50, 1077–1080.
Iglesias, M.J., Piñeiro, R., Blanco, M., Gallego, R., Diéguez, C., Gualillo, O., González-Juanatey, J.R., Lago, F. (2004): Growth hormone-releasing peptide (ghrelin) is synthesized and secreted by cardiomyocytes. Cardiovasc Res, 62, 481–488.
Kasimay, O., Iseri, S.O., Barlas, A., Bangir, D., Yegen, C., Arbak, S., Yegen, B.C. (2006): Ghrelin ameliorates pancreaticobiliary inflammation and associated remote organ injury in rats. Hepatol Res, 36, 11–19.
Kleinz, M.J., Maguire, J.J., Skepper, J.N. (2006): Functional and immunocytochemical evidence for a role ghrelin and des-octanoyl ghrelin in the regulation of vascular tone in man. Cardiovasc Res, 69, 227–235.
Kojima, M., Hosoda, H., Date, Y., Nakazato, M., Matsuo, H., Kangawa, K. (1999): Ghrelin is a growth-hormone-releasing acylated peptide from stomach. Nature, 402, 656–660.
Kojima, M., Kangawa, K. (2005): Ghrelin: structure and function. Physiol Rev, 85, 495–522.
Lin, Y., Matsumura, K., Fukuhara, M., Kagiyama, S., Fujii, K., Iida, M. (2004): Ghrelin acts at the nucleus of the solitary tract to decrease arterial pressure in rats. Hypertension, 43, 977–982.
Louagie, Y.A.G., Jamart, J., Gonzales, M., (2004): Continuos cold cardioplegia improves myocardial protection: a prospective randomized study. Ann Thorac Surg, 77, 664–671.
Mair, P., Mair, J., Bleir, J. (1997): Augmented release of brain natriuretic peptide during reperfusion of the human heart after cardioplegic cardiac arrest. Clin Chim Acta, 261, 57–68.
Maisel, A.S., Krishnaswamy, P., Nowak, R.M., (2002): Breathing Not Properly Multinational Study Investigators. Rapid measurement of the B-type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med, 347, 161–167.
Morimoto, K., Mori, T., Ishiguro, S. (1998): Perioperative changes in plasma brain natriuretic peptide concentrations in patients undergoing cardiac surgery. Surg Today, 28, 23–29.
Morris, D.C., Clements, S.D. Jr., Bailey, J.M. (2004): Management of the patient after cardiac surgery. In: “The Heart” (Fuster, V., Alexander, R. W. and O’Rourke, R.A., eds.). McGraw Hill, New York, pp. 1509–1516.
Nagaya, N., Kojima, M., Uematsu, M. (2001b): Hemodynamic and hormonal effects of human ghrelin in healty volunteers. Am J Physiol Regul Integr Comp Physiol, 280, R1483-R1487.
Nagaya, N., Miyatake, K., Uematsu, M., Oya, H., Shimizu, W., Hosoda, H., Kojima, M., Nakanishi, N., Mori, H., Kangawa, K. (2001a): Hemodynamic, renal, and hormonal effects of ghrelin infusion in patients with chronic heart failure. J Clin Endocrinol Metab, 86, 5854–5859.
Nakamura, K., Ueno, T., Yamamoto, H., (2005): Relationship between cerebral injury and inflammatory responses in patients undergoing cardiac surgey with cardiopulmonary bypass. Cytokine, 29, 95–104.
Ohata, T., Sawa, Y., Kadoba, K., Kagisaki, K., Suzuki, K., Matsuda, H. (2000): Role of nitrix oxide in atemparature dependent regulation of systemic vascular resistance in cardiopulmonary bypass. Eur J Cardiothorac Surg, 18, 342–347.
Palazzuoli, A., Carrera, A., Calabria, P., (2004): Brain natriuretic peptide levels during cardiac reperfusion: comparison between percutaneous coronary angioplasty and aorto-coronaric bypass. Clin Chim Acta, 342, 87–92.
Pemberton, C.J., Tokola, H., Bagi, Z. (2004): Ghrelin induces vasoconstriction in the rat coronary vasculature without altering without altering cardiac peptide secretion. Am J Physiol Heart Circ Physiol, 287, H1522-H1529.
Protter, A.A., Wallace, A.M., Ferraris, V.A., Weishaar, R.E. (1996): Relaxant effect of human brain natriuretic peptide on human artery and vein tissue. Am J Hypertens, 9, 432–436.
Rastan, A.J., Bittner, H.B., Gummert, J.F., (2005): On-pump beating heart versus off-pump coronary artery bypass surgery-evidence of pump-induced myocardial injury. Eur J Cardiothorac Surg, 27, 1057–1064.
Sehirli, O., Sener, E., Sener, G., (2008): Ghrelin improves burn-induced multiple organ injury by depressing neutrophil infiltration and the release of pro-inflammatory cytokines. Peptides, 29, 1231–1240.
Shimizu, Y., Nagaya, N., Teranishi, Y., Imazu, M., Yamamoto, H., Shokawa, T., Kangawa, K., Kohno, N., Yoshizumi, M. (2003): Ghrelin improves endothelial dysfunction through growth hormone-independent mechanism in rats. Biochem Biophys Res Commun, 310, 830–835.
Stein, B.C., Levin, R.I. (1998): Natriuretic peptides: physiology, therapeutic potential, and risk stratification in ischemic heart disease. Am Heart J, 135, 914–923.
Thomson, N.M., Gill, D.A., Davies, R., Loveridge, N., Houston, P.A., Robinson, I.C., Wells, T. (2004): Ghrelin and des-octanoyl ghrelin promote adipogenesis directly in vivo by a mechanism independent of type 1a growth hormone secretagogue receptor. Endocrinology, 145, 234–242.
Van der Zander, K., Houben, A.J., Kroon, A.A., De Mey, J.G., Smits, P.A., de Leeuw, P.W. (2002): Nitric oxide and potassium channels are involved in brain natriuretic peptide induced vasodilatation in man. J Hypertens, 20, 493–439.
Wiley, K., Davenport, A. (2002): Comparision of vasodilators in human internal mammary artery. Ghrelin is a potent physiological antagonist of endothelin-1. Br J Pharmacol, 136, 1146–1152.
Yasue, H., Yoshimura, M. (1996): Natriuretic peptides in the treatment of heart failure. J Card Fail, 2, S277-S285.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rahman, A., Aydin, S., Bayar, M.K. et al. Changes of ghrelin and brain natriuretic peptide levels in systemic vascular resistance after cardiopulmonary bypass. J. Physiol. Biochem. 64, 221–230 (2008). https://doi.org/10.1007/BF03178845
Received:
Issue Date:
DOI: https://doi.org/10.1007/BF03178845