Abstract
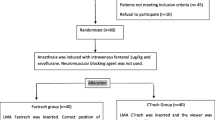
The efficacy of the triple airway manoeuvre (mouth opening, head extension and jaw thrust) for insertion of the laryngeal mask airway (LMA) was compared with the standard insertion method. One hundred paralyzed patients were allocated randomly into two groups: in the control group (n = 50) the LMA was inserted by the standard method, and in the other (TAM group, n = 50) by the triple airway manoeuvre. In ten patients of each group, the position of the LMA and the epiglottis was assessed radiographically before insertion, after insertion but before cuff inflation, and after cuff inflation. In all patients the position was examined using fibrescopy before and after cuff inflation. The mean distance between the epiglottis and the posterior pharyngeal wall, measured radiographically before LMA insertion, was greater in the TAM group (16.3 (SD 4.3) mm) than in the control group (7.0 (2.8) mm) (P < 0.001). Before cuff inflation, radiography and fibrescopy showed that the LMA compressed the epiglottis downwards more frequently in the control group. After cuff inflation the glottis was completely visible fibreoptically in 66% in the TAM group, compared with 14% in the control group (P < 0.001). Complete downfolding of the epiglottis was seen in 10% in the control group and none in the TAM group (P < 0.05). We conclude that in paralyzed patients LMA insertion with the triple airway manoeuvre provides wider pharyngeal space and decreases the incidence of epiglottic downfolding by the LMA compared with the standard method.
Résumé
Cette étude compare avec la méthode d’insertion standard, l’efficacité de la triple manoeuvre de libération des votes aériennes (ouverture de la bouche, extension de la tête et élévation du mandibule) pour l’insertion du masque laryngé (ML). Cent patients paralysés sont répartis au hasard entre deux groupes: dans le groupe contrôle (n = 50), le ML est inséré suivant la méthode standard, et dans l’autre (le groupe TM = 50) suivant la triple manoeuvre. Chez dix patients de chaque groupe, la position du ML et de l’épiglotte est évaluée par radiographie, avant l’insertion, après l’insertion et avant l’insufflation de la manchette, et après celleci. Chez tons les patients, la position a été vérifiée par fibroscopie avant et après l’insufflation. La distance moyenne entre l’épiglotte et la paroi pharyngée postérieure, mesurée par radiographie avant l’insertion du ML, est plus grande dans le groupe TM (16,3 ± ET 4,3 mm) que dans le groupe contrôle (7,0 ± 2,8 mm) (P < 0,001). Avant l’insufflation de la manchette, la radiographie et la fibroscopie montrent que le ML comprime l’épiglotte vers le bas plus fréquemment dans le groupe contrôle. Après l’insufflation de la manchette, la glotte est visualisée dans son entier par fibroscopie chez 66% du groupe TM comparativement à 14% du groupe contrôle (P < 0,001). Un affaissement complet de l’épiglotte est constaté chez 10% du groupe contrôle et chez aucun patient du groupe TM (P < 0,05). Les auteurs concluent que pour l’insertion du ML chez les patients paralysés, la triple manoeuvre procure un espace pharyngé plus vaste et diminue l’incidence de l’affaissement de l’épiglotte par le ML comparativement à la méthode standard.
Article PDF
Similar content being viewed by others
References
Brain AIJ, McGhee TD, McAteer EJ, Thomas A, Abu-Saad MAW, Bushman JA. The laryngeal mask airway. Development and preliminary trials of a new type of airway. Anaesthesia 1985; 40: 356–61.
Brodrick PM, Webster NR, Nunn JF. The laryngeal mask airway. A study of 100 patients during spontaneous breathing. Anaesthesia 1989; 44: 238–41.
Maltby JR, Loken RG, Watson NC. The laryngeal mask airway: clinical appraisal in 250 patients. Can J Anaesth 1990; 37: 509–13.
Asai T, Morris S. The laryngeal mask airway: its features, effects and role. Can J Anaesth 1994; 41: 930–60.
Nandi PR, Nunn JF, Charlesworth CH, Taylor SJ. Radiological study of the laryngeal mask. Eur J Anaesthesiol Suppl 1991; 4: 33–9.
Goudsouzian NG, Denman W, Cleveland R, Shorten G. Radiologic localization of the laryngeal mask airway in children. Anesthesiology 1992; 77: 1085–9.
Payne J. The use of the fibreoptic laryngoscope to confirm the position of the laryngeal mask (Letter). Anaesthesia 1989; 44: 865.
Boidin MP. Airway patency in the unconscious patient. Br J Anaesth 1985; 57: 306–10.
Benumof JL. Management of the difficult adult airway. With special emphasis on awake tracheal intubation. Anesthesiology 1991; 75: 1087–110.
Pennant JH, White PF. The laryngeal mask airway. Its uses in anesthesiology. Anesthesiology 1993; 79: 144–63.
Benumof JL. Use of the larygeal mask airway to facilitate fiberscope-aided tracheal intubation (Letter). Anesth Analg 1992; 74: 313–5.
Safar P, Bircher NG. Cardiopulmonary Cerebral Resuscitation, 3rd ed. London: W.B. Saunders, 1988.
Safer P, Escarraga LA, Chang F. Upper airway obstruction in the unconscious patient. J Appl Physiol 1959; 14: 760–4.
Brain AIJ. The Intavent Laryngeal Mask Instruction Manual, 2nd ed. England: Intavent, 1993.
Brain AIJ. Laryngeal mask misplacement — causes, consequences and solutions (Letter). Anaesthesia 1992; 47: 531–2.
Cass L. Inserting the laryngeal mask (Letter). Anaesth Intensive Care 1991; 19: 615.
Asai T, Latto IP, Vaughan RS. The distance between the grille of the laryngeal mask airway and the vocal cords. Is conventional intubation through the laryngeal mask safe? Anaesthesia 1993; 48: 667–9.
Füllekrug B, Pothmann W, Werner C, Schulte AM Esch J. The laryngeal mask airway: anesthetic gas leakage and fiberoptic control of positioning. J Clin Anesth 1993; 5: 357–63.
Asai T, Barclay K, Power I, Vaughan RS. Cricoid pressure impedes placement of the laryngeal mask airway and subsequent tracheal intubation through the mask. Br J Anaesth 1994; 72: 47–51.
Brimacombe J, Berry A. Laryngeal mask airway insertion. A comparison of the standard versus neutral position in normal patients with a view to its use in cervical spine instability. Anaesthesia 1993; 48: 670–1.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Aoyama, K., Takenaka, I., Sata, T. et al. The triple airway manoeuvre for insertion of the laryngeal mask airway in paralyzed patients. Can J Anaesth 42, 1010–1016 (1995). https://doi.org/10.1007/BF03011074
Accepted:
Issue Date:
DOI: https://doi.org/10.1007/BF03011074